Evolution of Modern Accelerometry Research in Aging
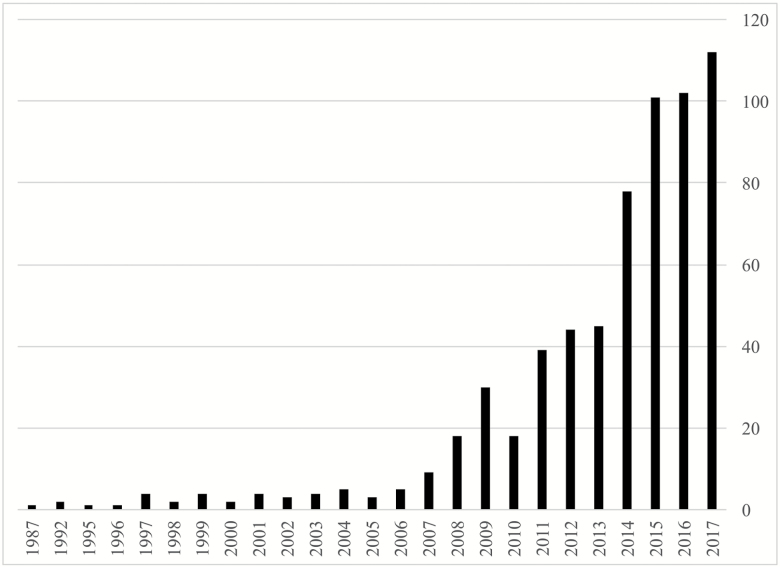
Physical activity has consistently been associated with health benefits, including for older adults (1). As technology has evolved, physical activity research has begun to include more objective measures of physical activity and function (2). As a result, the literature has recorded an explosion in the use of accelerometers, small, wearable devices that continuously assess movement in at least three dimensions. A PubMed search for research studies using accelerometers in older adults shows a rapid increase over the past 20 years, with an average of about two articles per year in the 1990s and 112 articles in 2017 (Figure 1).
Figure 1.
Frequency of PubMed manuscripts with keywords “accelerometer” and “older adults” from 1987 to 2017.
Because accelerometer-based technology is still fairly new, the majority of aging research studies have been cross-sectional or focused on shorter duration interventions, but as follow-up time increases, we have begun to see longitudinal and intervention studies with longer durations related to aging-related conditions. However, with new technology and opportunity comes new challenges, as discussed by recent reviews (3,4). In this short communication, we highlight how current research is addressing these challenges and future directions in accelerometer research among older adults.
New Technology, New Opportunities, and New Challenges
Physical Activity Assessment Among Older Adults
Physical activity assessment among older adults faces unique challenges compared with assessment in younger adults (4). For instance, older adults have a wider range of activity, from very active to quite inactive, with key differences in both the type and the intensity of activities. Unlike younger populations, older populations with low activity often have diminished physiological capacity or multimorbidity. These factors present important differences for researchers using accelerometers in older study populations, as these differences must be accounted for in the analyses to avoid substantial threats to validity.
Moving Beyond a Single Physical Activity Metric
The majority of physical activity research has centered around summarizing activity into a few simple metrics: the minutes of moderate- to vigorous-intensity physical activity per day or week and, more recently, sedentary time (1,5,6). Accelerometers provide an opportunity, with minimal additional participant burden, to examine physical activity beyond these simple metrics. In this issue, researchers used accelerometers to examine physical activity patterns, looking closely at “how” physical activity is accrued over the course of the day (7,8), gait and balance (9), and how the mechanical forces of activity such as vertical impacts experienced during activity (10,11).
Accelerometers assess activity continuously, providing not only the activity volume but also a time stamp, allowing for the calculation of a rate of activity accrual. Surprisingly, in most older nonworking populations, activity appears diurnal with a peak in activity in mid-morning and a gradual decline in activity in late afternoon. This has led to a body of literature examining the shape of activity patterns and how they differ by age and health status (12). Building on this, Huisingh-Scheetz and colleagues looked at the association of hourly activity levels and frailty (7) and Wanigatunga and colleagues investigated activity and perceived fatigability (8). Although several studies have shown that total volume of activity is lower among those who are older, more frail, or have chronic health conditions, the timing of when activity is accrued may provide additional information that may identify modifiable targets for intervention. Investigators therefore describe not only the differences in activity volume but also when the activity occurs. Wanigatunga and colleagues looked at physical activity and perceived fatigability and observed that those with greater fatigability tended to reduce their activity earlier in the day (8). Moreover, a relatively small change in fatigability was reflected in significant differences in daily activity volume and patterns. Further research is needed to include within- and between-day variability. The strongest utility may be to use these patterns as part of a circadian rhythm assessment or to establish individualized activity prescriptions based on accelerometry.
Focusing on Aging Outcomes
Gait and balance are established, important markers of healthy aging, particularly as determinants of physical activity and physical and cognitive functioning (13–16). Using accelerometers and gyroscopes, researchers can assess not only detailed physical activity measures but also gait and balance with minimal additional burden (17). Dawe and colleagues used a wrist-worn accelerometer and an accelerometer/gyroscope device on the lower back to objectively assess physical activity, gait, and balance, in one of the first studies to characterize the interdependent associations (9). The authors found that gait and balance account for up to 16% of the variability in total physical activity levels, highlighting the importance of viewing physical activity among older adults as beyond a simple “exercise more” recommendation.
Expanding on previous literature showing that vertical impact (the force applied in the upward or downward direction due to activity) is positively associated with bone mineral density (18,19), two studies, one by Hartley and colleagues and the other by Elhakeem and colleagues, used a hip-worn accelerometer to measure vertical impacts over 7 days among community-dwelling older women to examine the association of vertical impact intensity with sarcopenia and body composition (10,11). Both Elhakeem and colleagues and Hartley and colleagues observed that high-intensity impacts, but not lower- or moderate-intensity impacts, were associated with sarcopenia and body composition (10,11). Measuring impacts in a free-living environment during usual activities may provide a more complete picture of a participants’ activity than a laboratory-based physical function test such as jumping force. Studies such as these are integral in determining how physical activity affects various aging-specific outcomes in both free-living environments and intervention studies, as well as prove that accelerometry can be used for translational studies of function.
Relative Versus Absolute Cut points for Older People
Accelerometers assess movement, but as currently configured, they are unable to measure the amount of effort or energy needed to perform specific movements. In this issue, researchers explore how to translate accelerometer output into metrics of physical activity intensity that are appropriate for older populations (20,21). As part of the LIFE study, a physical activity intervention of 1,635 older adults, Rejeski and colleagues examined the ability of several standard accelerometer moderate-to-vigorous activity thresholds to identify changes in activity level (20). Although several studies have shown that accelerometer thresholds for adults may not be applicable in older adults, the LIFE study provides an opportunity to look at changes in activity thresholds over time by intervention status (eg, structured physical activity vs. health education) and to assess the appropriateness of thresholds in this context. Rejeski and colleagues also furthered the conversation by looking at differences by physical function status, showing that among participants with low physical function, accelerometers may not be solely sufficient to detect changes in activity level (20).
Using a combined heart rate and accelerometer device, Schrack and colleagues compared relative versus absolute intensity of daily physical activity in 440 older adults participating in the Baltimore Longitudinal Study of Aging (21). Using traditional absolute intensity thresholds, older adults registered lower levels of daily activity and more sedentary time. However, using individualized relative intensity thresholds as defined by heart rate reserve, the results reversed, with older adults spending more time each day engaged in moderate- to vigorous-intensity activities. These findings suggest that the amount of time spent in higher-intensity activities may not be lower with age after considering changes in physiologic reserve, functional ability, and subclinical disease burden, and further emphasize the need for careful consideration of application of universal accelerometer thresholds to older populations.
Future Directions
Physical activity and aging research will continue to advance with the increased use of accelerometers, but we wish to highlight two challenges and opportunities: (i) expanding usage in clinical and intervention studies and (ii) identifying which of the new activity metrics or combination of metrics are relevant to predicting health outcomes in older adults. Building on the existing clinical and intervention studies such as the LIFE study, the expansion of accelerometer deployment within clinical and intervention populations will allow researchers to quantify and monitor changes in activity (or its characteristics) with greater precision over time. If this change is associated with longitudinal clinical outcomes, it will provide evidence to treat changes in objectively measured activity as a surrogate marker and end point in its own for future studies. Thus, accelerometry is also a translational tool, ranging from measurement of movement to physiological intermediates such as impact force.
Accelerometers provide the opportunity to push past evaluating physical activity through a single metric; however, researchers now face the challenge of identifying which physical activity characteristics and patterns are most important to aging-related outcomes, obtained through longitudinal health data. This is not meant to discount the importance of other activity assessment methods, such as questionnaires, but more to leverage the complementary potential of using multiple assessment methods to understand the underlying biological relationship of activity and healthy aging. We encourage researchers also to examine a combination of activity metrics from multiple sources to more fully characterize individuals and identify potential intervention targets for increasing activity.
Funding
This research is supported in part by the Intramural Research Program at the National Institute on Aging, National Institutes of Health (Shiroma, Harris). Dr. Schrack is supported by R21AG053198, P30AG021334, and U01AG057545.
Conflict of Interest
None reported.
References
- 1. Physical Activity Guidelines Committee. Physical Activity Guidelines Advisory Committee Report 2008. http://health.gov/paguidelines/guidelines/report.aspx. Accessed February 26, 2018.
- 2. Troiano RP, Berrigan D, Dodd KW, Mâsse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40:181–188. doi:10.1249/mss.0b013e31815a51b3 [DOI] [PubMed] [Google Scholar]
- 3. Schrack JA, Cooper R, Koster A, et al. Assessing daily physical activity in older adults: unraveling the complexity of monitors, measures, and methods. J Gerontol A Biol Sci Med Sci. 2016;71:1039–1048. doi:10.1093/gerona/glw026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Murphy SL. Review of physical activity measurement using accelerometers in older adults: considerations for research design and conduct. Prev Med. 2009;48:108–114. doi:10.1016/j.ypmed.2008.12.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ekelund U, Steene-Johannessen J, Brown WJ, et al. ; Lancet Physical Activity Series 2 Executive Committee; Lancet Sedentary Behaviour Working Group Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonised meta-analysis of data from more than 1 million men and women. Lancet. 2016;388:1302–1310. doi:10.1016/S0140-6736(16)30370-1 [DOI] [PubMed] [Google Scholar]
- 6. Lee IM, Shiroma EJ, Lobelo F, Puska P, Blair SN, Katzmarzyk PT; Lancet Physical Activity Series Working Group Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet. 2012;380:219–229. doi:10.1016/S0140-6736(12)61031-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Huisingh-Scheetz M, Wroblewski K, Kocherginsky M, et al. Physical activity and frailty among older adults in the U.S. based on hourly accelerometry data. J Gerontol A Biol Sci Med Sci. 2017. doi:10.1093/gerona/glx208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Wanigatunga AA, Simonsick EM, Zipunnikov V, et al. Perceived fatigability and objective physical activity in mid- to late-life. J Gerontol A Biol Sci Med Sci. 2017. doi:10.1093/gerona/glx181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Dawe RJ, Leurgans SE, Yang J, et al. Association between quantitative gait and balance measures and total daily physical activity in community-dwelling older adults. J Gerontol A Biol Sci Med Sci. 2017. doi:10.1093/gerona/glx167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Elhakeem A, Hannam K, Deere KC, et al. Physical activity producing low, but not medium or higher, vertical impacts is inversely related to BMI in older adults: findings from a multi cohort study. J Gerontol A Biol Sci Med Sci. 2017. doi:10.1093/gerona/glx176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hartley A, Gregson CL, Hannam K, Deere KC, Clark EM, Tobias JH. Sarcopenia is negatively related to high gravitational impacts achieved from day-to-day physical activity. J Gerontol A Biol Sci Med Sci. 2017. doi:10.1093/gerona/glx223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Schrack JA, Zipunnikov V, Goldsmith J, et al. Assessing the “physical cliff”: detailed quantification of age-related differences in daily patterns of physical activity. J Gerontol A Biol Sci Med Sci. 2014;69:973–979. doi:10.1093/gerona/glt199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Verghese J, Lipton RB, Hall CB, Kuslansky G, Katz MJ, Buschke H. Abnormality of gait as a predictor of non-Alzheimer’s dementia. N Engl J Med. 2002;347:1761–1768. doi:10.1056/NEJMoa020441 [DOI] [PubMed] [Google Scholar]
- 14. Best JR, Liu-Ambrose T, Boudreau RM, et al. ; Health, Aging and Body Composition Study An evaluation of the longitudinal, bidirectional associations between gait speed and cognition in older women and men. J Gerontol A Biol Sci Med Sci. 2016;71:1616–1623. doi:10.1093/gerona/glw066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Mielke MM, Roberts RO, Savica R, et al. Assessing the temporal relationship between cognition and gait: slow gait predicts cognitive decline in the Mayo Clinic Study of Aging. J Gerontol A Biol Sci Med Sci. 2013;68:929–937. doi:10.1093/gerona/gls256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Guralnik JM, Ferrucci L, Simonsick EM, Salive ME, Wallace RB. Lower-extremity function in persons over the age of 70 years as a predictor of subsequent disability. N Engl J Med. 1995;332:556–561. doi:10.1056/NEJM199503023320902 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Buchman AS, Leurgans SE, Weiss A, et al. Associations between quantitative mobility measures derived from components of conventional mobility testing and Parkinsonian gait in older adults. PLoS One. 2014;9:e86262. doi:10.1371/journal.pone.0086262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Deere KC, Hannam K, Coulson J, et al. Quantifying habitual levels of physical activity according to impact in older people: accelerometry protocol for the VIBE study. J Aging Phys Act. 2016;24:290–295. doi:10.1123/japa.2015-0066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Hannam K, Deere KC, Hartley A, et al. Habitual levels of higher, but not medium or low, impact physical activity are positively related to lower limb bone strength in older women: findings from a population-based study using accelerometers to classify impact magnitude. Osteoporos Int. 2017;28:2813–2822. doi:10.1007/s00198-016-3863-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Rejeski WJ, Walkup MP, Fielding RA, et al. Evaluating accelerometry thresholds for detecting changes in levels of moderate physical activity and resulting major mobility disability. J Gerontol A Biol Sci Med Sci. 2017. doi:10.1093/gerona/glx132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Schrack JA, Leroux A, Fleg JL, et al. Using heart and accelerometry to define quantity and intensity of daily physical activity in older adults. J Gerontol A Biol Sci Med Sci. 2018. doi:10.1093/gerona/gly029 [DOI] [PMC free article] [PubMed] [Google Scholar]