Abstract
Antiretroviral therapy (ART) is a lifelong treatment. To date, ART adherence is suboptimal for most patients in resource-poor settings. Previous research indicates that medication side effects are perceived to be a significant barrier of high ART adherence. Data regarding the role of adherence self-efficacy in mediating the relationship between side effects from ART and adherence to ART are limited; thus, this study examines this potential mediational role of self-efficacy. A cross-sectional survey of 2,987 people living with HIV aged ≥ 18 years was conducted in 2012–2013 in Guangxi Autonomous Region (Guangxi) which has one of the fastest-growing HIV rates in China. Of the total sample, 2,146 (72.1%) participants had initiated ART. Participants reported the number of days of completing the daily dose of ART in the past month; adherence was defined as completing the daily dose at least 28 days in the last month (≥ 90%). Side effects were significantly negatively related to adherence to ART. Mediation analyses indicated that adherence self-efficacy significantly mediated the side effects–adherence relationship. Future interventions to increase adherence self-efficacy and effective coping with side effects among HIV patients are needed in order to improve their ART adherence.
Keywords: Adherence, Adherence self-efficacy, Antiretroviral therapy (ART), Side effects, HIV infection, China
Introduction
Globally, approximately 35.3 million people were living with human immunodeficiency virus (HIV) at the end of 2012, according to the Joint United Nations Programme on HIV and AIDS (UNAIDS) report on the global AIDS epidemic (UNAIDS, 2013). In China, the estimated number of HIV patients was 780,000 by 2011 (Zheng et al., 2014). Guangxi is one of the provinces besides Yunnan and Henan in China with the most severe HIV epidemic (Li et al., 2013). The survival of patients infected with HIV relies on a high level of adherence to antiretroviral therapy (ART) (Mills et al., 2006). Medication adherence is defined as the extent to which a patient’s medication-taking behavior follows their healthcare provider’s recommendations (World Health Organization, 2003). A high level of adherence (e.g., ≥90%) is critical for treatment success among patients with HIV (Friedland & Williams, 1999). Good ART adherence is associated with the reduction of viral load; whereas, poor adherence to ART undermines viral suppression and increases the risk of drug resistance, onward transmission of the virus, and the progression of AIDS (Hailasillassie, Etana, Alemayehu, & Fisseha, 2014; Sherr et al., 2010). Adherence research among PLHIV in the United States has been conducted for the last two decades (Chesney et al., 2000); however, we are not aware any previous studies in this field among people living with HIV (PLHIV) in China.
ART has been widely available in China since 2003 when ART drugs became generically produced (Chen et al., 2013). National data indicated that the coverage rate of ART was 63.4% in 2009 (F. Zhang et al., 2011). Since 2008, the combination of zidovudine (AZT) or stavudine (d4T) with nevirapine (NVP) has been used as the first-line treatment (Chen et al., 2013). With the utilization of ART, the mortality of PLHIV has declined dramatically from 39.3 per 100 person-years in 2002 to 14.2 per 100 person-years in 2009 (F. Zhang et al., 2011). Although the mortality rate has improved, ART adherence is still suboptimal in China. A recent study conducted in Guangzhou (a large city in southern China) indicated that 18.9% of HIV patients reported nonadherence to ART (Muessig et al., 2014).
ART is lifelong and ART adherence is suboptimal for many patients in resource-poor settings (Mills et al., 2006). Adherence level is potentially influenced by many facilitators and barriers (Starks et al., 2008). Reda and Biadgilign’s (2012) review of studies conducted in Africa suggests that determinants of ART adherence might include patient-related factors (e.g., sociodemographic characteristics, substance use, knowledge and perceptions about ART, psychological factors), medication-related factors (e.g., medication regimens, side effects, accessibility of drugs), health care delivery systems-related factors (e.g., healthcare providers’ experience, patient-provider relationship), and social factors (e.g., HIV stigma, social support) (Reda & Biadgilign, 2012). Poverty and access to ART are additional barriers to maintaining high levels of adherence (Mills et al., 2006). Studies conducted in sub-Saharan Africa report that cost, perceived HIV stigma, alcohol abuse, complexity of drug regimens, and forgetfulness were negatively associated with adherence (Mills et al., 2006). Depressive symptoms are consistently associated with poor adherence to ART (Magidson, Blashill, Safren, & Wagner, 2015). In a UK study, Sherr et al. (2010) indicated that race and age were associated with nonadherence. Further, a study in the US indicated that stigma was strongly associated with poor access to care, and mental health mediated the relationships between stigma and access to care and adherence (Sayles, Wong, Kinsler, Martins, & Cunningham, 2009). In one of the few studies conducted in China, nonadherence was associated with lower education, living alone, alcohol use, and years on ART (Muessig et al., 2014).
Experiencing severe side effects of ART have been identified as another significant barrier of poor adherence to ART (Ammassari et al., 2001; Rao, Kekwaletswe, Hosek, Martinez, & Rodriguez, 2007). The most common side effects from ART include gastrointestinal problems, dermatological problems, systematic discomforts, and metabolic dysfunctions (F. Zhang et al., 2011). People’s response to side effects vary from individual to individual (Rao et al., 2007). In a focus group study of 25 PLHIV, Rao et al. (2007) reported that most participants experienced side effects and some participants stopped their medication because of side effects. Overcoming and managing ART side effects is critical not only for maintaining high adherence, but also for maintaining high quality of life. Interventions on side effect management skills have demonstrated positive effects on ART adherence levels (Johnson, Dilworth, Taylor, & Neilands, 2011).
Another critical factor associated with medication adherence is adherence self-efficacy (Johnson et al., 2006). A wealth of research guided by social-cognitive theory demonstrates self-efficacy’s key role in successfully engaging in a variety of health behaviors, including taking medications as prescribed (Bandura, 1989). Adherence self-efficacy is one’s confidence in his/her ability to take the medication as recommended by medical providers (Johnson et al., 2007). Previous studies have demonstrated a positive correlation between self-efficacy and adherence (Chesney et al., 2000; Johnson et al., 2003). For instance, with a sample of racial and/or ethnic minority youth from 20 sites across the US, higher medication self-efficacy predicted higher ART adherence (MacDonell, Jacques-Tiura, Naar, Fernandez, & ATN 086/106 Protocol Team, 2015).
Severe side effects of ART have significant impact on adherence. As of now, ART side effects may be unavoidable. Despite previous studies indicating the negative relationship between side effects and adherence, data regarding the potential mediation effect of self-efficacy on the relationship between side effects and adherence are limited overall and nonexistent in Chinese samples. It is critical to understand factors that could increase ART adherence in order to develop targeted interventions to improve adherence. Therefore, we conducted this study to examine adherence self-efficacy as a mediator of the ART side effects–adherence relationship with a sample of PLHIV in southern China.
Method
Study site
This study was conducted in 2012–2013 in Guangxi Autonomous Region (Guangxi) in China. Guangxi is located in southern China and has a population of 46 million (National Bureau of Statistics of China, 2012). Guangxi has the second largest number of reported HIV cases among 31 provinces in China (China Ministry of Health, 2012).
Sampling and survey procedure
A total of 17 cities and 75 counties in Guangxi were ranked in terms of number of reported HIV/AIDS cases. The 2 cities and 10 counties with the largest number, accounting for 43% of the reported cases, were selected as the sampling frame. From the list of known HIV cases in local Center for Disease Control and Prevention (CDC), 10% were randomly drawn in each of the 12 selected study sites. We recruited those who were at least 18 years of age and physically and mentally able to complete a survey. Local CDC staff contacted selected cases by telephone and invited them to participate in the survey. Approximately 90% of selected participants agreed to participate and provide written informed consent. Participants completed the survey in local community health centers where they received medical care. Nineteen percent of participants completed the questionnaire in Mandarin by themselves; the remaining 81.2% participants completed the questionnaire through one-on-one interview because of reading difficulties and/or personal preference. Interviewers received intensive 2-day training on research ethics and interview skills prior to the study. The entire survey took about 75–100 minutes to complete. Each participant received a gift valued at US$5 when they completed the survey as a token of appreciation for their time. A total of 3,002 PLHIV consented and participated. Fifteen surveys with extensive missing data were removed from the data analysis, thus giving the final study sample of 2,987. Seventy-two percent (n=2,146) of participants were prescribed ART and were included in the current analyses. The research protocol was approved by the Institutional Review Boards at both Wayne State University in the United States and Guangxi CDC in China.
Measures
Adherence to ART
Information about adhering to ART regimen schedules was collected directly from patients. Adherence was measured by the number of days that patients completed their medication in the last month prior to the survey. Participants were asked, “How many days did you take daily-dose HIV medication in the last month?” Consistent with recent research ((MacDonell et al., 2015; Viswanathan et al., 2015) that maintaining at least 90% adherence is critical for treatment success, if a patient completed their daily-dose medication at least 28 days in the past month, they were considered to be adherent to ART (adherence=1). If the number of days that a patient completed daily-dose medication was less than 28, they were considered nonadherent to ART (adherence=0).
Side effects
The occurrence of side effects and how they affected patients’ daily lives was measured using one item: “In the past two weeks, have you experienced medication-related side effects and how did those influence you?” There were five response options (0=had no side effects, 1=had side effects with no influence on me, 2=had side effects with little influence on me, 3=had side effects with large influence on me, 4=had side effects with severe influence).
Adherence self-efficacy
Adherence self-efficacy was assessed with a 12-item scale. This scale was developed based on our qualitative interviews with participants in the formative phase of the study (English translation of items are shown in Table 1). These items reflect patients’ confidence to carry out behaviors related to adhering to their ART regimen, being able to manage side effects, and dealing with ART-related health problems. Each item had five response options (1=completely not sure, 2=mostly not sure, 3=it is hard to say, 4=mostly sure, and 5=completely sure). A composite score of adherence self-efficacy was calculated by summing the item scores. Scores ranged from 12 to 60, with a higher score indicating a higher level of adherence self-efficacy. Internal consistency was high (Cronbach’s α=0.92).
Table 1.
Items of adherence self-efficacy scale
| To what degree can you do the following things (completely not sure=1, mostly not sure=2, it is hard to say=3, mostly sure=4, and completely sure=5): |
Mean (S.D.) | Corrected item- total correlation |
|---|---|---|
| 1. I can follow the recommendation of using a high dose of ART. |
3.62 (0.91) | 0.51 |
| 2. I can take my medicine at the appropriate time. | 4.01 (0.71) | 0.67 |
| 3. I can follow my doctor’s recommendation and use ART or other preventive methods. |
4.05 (0.67) | 0.70 |
| 4. Despite the side-effects, I can follow the recommendation to use drugs on time and in the appropriate dose for all/almost of my medications. |
3.76 (0.79) | 0.61 |
| 5. If there are any side-effects, I can follow the recommendation to use drugs on time and in the appropriate dose for all/almost of my medications. |
3.88 (0.71) | 0.65 |
| 6. I can follow my doctor’s recommendation and use ART everyday. |
4.11 (0.64) | 0.68 |
| 7. I can discuss with doctors to take the drugs that are best for me. |
4.03 (0.69) | 0.67 |
| 8. Overall, I can use drugs to control my symptoms. | 3.97 (0.68) | 0.70 |
| 9. I can minimize the influence of sleep problems caused by the disease on my life. |
3.63 (0.80) | 0.70 |
| 10. I can minimize the influence of physical problems caused by the disease on my life. |
3.58 (0.81) | 0.71 |
| 11. I can minimize the influence of other problems caused by the disease on my life. |
3.57 (0.81) | 0.70 |
| 12. I can manage the symptoms or other health problems to continue my daily activities. |
3.64 (0.81) | 0.70 |
| Scale score (Cronbach’s alpha=0.92) | 45.80 (6.58) | NA |
Depressive symptoms
Depressive symptoms were assessed using the short version (10 items) of the Center for Epidemiological Studies Depression scale (Kohout, Berkman, Evans, & Cornoni-Huntley, 1993). Each item had a 4-point response reflecting symptom frequency (0=never, 1=sometime, 2=often, 3=always). A composite score (ranging from 0 to 28) was obtained by summing item responses, with higher scores indicating higher frequency of depressive symptoms. Cronbach’s alpha was 0.88.
Perceived HIV stigma
Perceived HIV stigma was measured using six items adapted from a previous study (Lin et al., 2010). A sample item states, “Other people are prejudiced against HIV patients.” Items had a 4-point Likert-type response scale (1=strongly disagree, 2=disagree, 3=agree, and 4=strongly agree). A composite score was calculated by summing the item scores. Scores ranged from 6 to 24, with higher scores indicating higher levels of perceived HIV stigma. Internal consistency was high (Cronbach’s α=0.91).
Demographic and health related factors
Self-reported relevant demographic factors were obtained and included in the analysis. These factors included age, gender, ethnicity (1=Han ethnicity [ethnic majority in China], 0=minority), education (years of formal schooling), residence (0=rural, 1=urban), lifetime illicit drug use (1=yes, 0=no), and family income. Monthly family income was a categorical variable with the unit of Renminbi yuan (1 yuan=US$ 0.16), the Chinese currency (1=0–999 yuan, 2=1000–1999 yuan, 3=2000–2999 yuan, 4=3000–3999 yuan, 5=4000–4999 yuan, 6=5000 yuan and above).
Statistical analyses
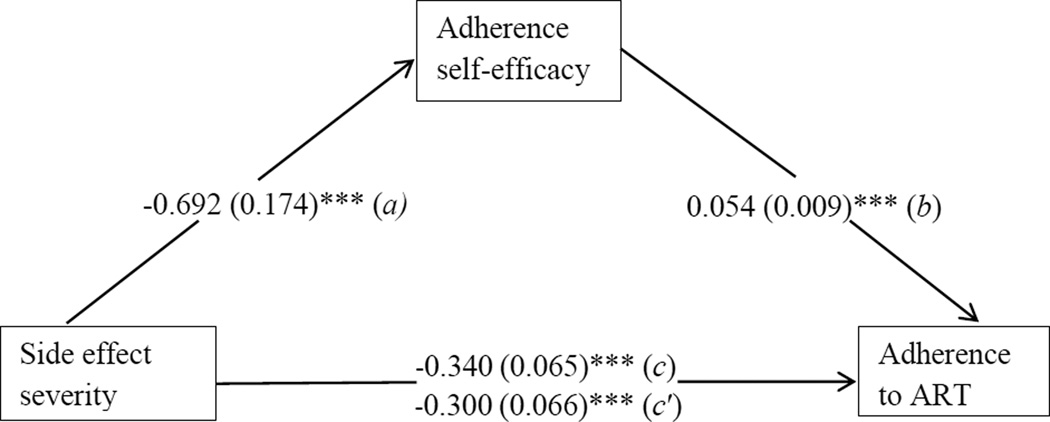
First, we computed descriptive statistics of demographic characteristics. Statistically significant differences of socio-demographic factors between two groups (adherent and nonadherent) were tested using ANOVA for continuous variables and the Chi-square test for categorical variables. Second, bivariate association analyses were performed between adherence and psychosocial factors (i.e., drug use, depressive symptoms, perceived HIV stigma, side effects, and adherence self-efficacy). Third, mediation analysis was employed following the guidelines by Baron and Kenny (Baron & Kenny, 1986). Multivariate linear regression analysis (adherence self-efficacy as the continuous dependent variable) and multivariate logistic regression analysis (adherence as the dichotomized dependent variable) were performed to examine the role of adherence self-efficacy in mediating the effect of side effects on adherence (Figure. 1). One multivariate linear regression model (model 1) and two multivariate logistic regression models (model 2 and model 3) were used to test the effect of mediator (adherence self-efficacy, M). In the first model, the mediation variable (adherence self-efficacy, M) was regressed on the independent variable (side effects, X) with a regression coefficient a. In the second model, the dependent variable (adherence, Y) was regressed on the independent variable (side effects, X) with a regression coefficient c. In the third model, the dependent variable (Y) was simultaneously regressed on the independent variable (X) and the mediation variable (M) with regression coefficients c′ (Y on X) and b (Y on M). The Sobel z-test was used to confirm the mediation effect (Sobel, 1982). All statistical analyses were performed using SPSS 18.0 for Windows.
Figure 1. Mediation analysis.
Note: Numbers are unstandardized coefficients and standard errors are given inside the brackets.
Sobel test statistics=−3.315 (0.011)***.
*p<0.05; **p<0.01; *** p<0.001.
Results
Demographic characteristics
Table 2 shows demographic characteristics of the sample. Participants’ mean age was 42.4 years (SD=12.5). About 61% (n=1,316) were male.. About 69% (n=1,479) of participants were Han ethnicity, and 81% (n=1,727) were from rural areas. The average years of formal schooling was 7 years and about 52.0% (n=1,107) had monthly family income less than 1,000 Yuan (about $165). In bivariate analysis, age, ethnicity, residence, and household monthly income were significantly associated with ART adherence (Table 2). Older patients were more likely to adhere to ART compared to their younger counterparts (p<0.01). Patients who were ethnic minorities and who lived in rural areas were more likely to adhere to ART than their Han counterparts (p<0.01) and urban residents (p<0.05), respectively. We also examined differences based on survey administration mode. Compared with those who completed the survey with an interviewer, those who self-administered the survey were age, ethnicity, and residence (p<0.01).
Table 2.
Demographic characteristics of the sample
| Variables | Total number of patients using ART (%) |
Adherence to ART, n (%) | |
|---|---|---|---|
| Nonadherent | Adherent | ||
| N | 2,146 | 365 (17.6) | 1713 (82.4) |
| Age, mean (SD) | 42.37 (12.47) | 40.57 (12.43) | 42.71 (12.45)** |
| 18–29 | 199 (10.1) | 48 (25.0) | 144 (75.0) |
| 30–39 | 826 (41.8) | 154 (19.1) | 651 (80.9) |
| 40–49 | 446 (22.6) | 65 (15.0) | 367 (85.0) |
| ≥50 | 506 (25.6) | 74 (15.2) | 413 (84.8) |
| Gender | |||
| Male | 1316 (61.3) | 225 (17.7) | 1049 (82.3) |
| Female | 830 (38.7) | 140 (17.4) | 664 (82.6) |
| Ethnicity | |||
| Minorities | 664 (31.0) | 83 (12.7) | 572 (87.3)*** |
| Han ethnicity | 1479 (69.0) | 282 (19.9) | 1138 (80.1) |
| Residence | |||
| Rural | 1727 (80.6) | 278 (16.6) | 1393 (83.4)* |
| Urban | 416 (19.4) | 87 (21.5) | 317 (78.5) |
| Years of formal schooling, mean (SD) | 7.01 (3.02) | 6.91 (2.98) | 7.02 (3.01) |
|
Monthly household income (in Chinese currency, Renminbi yuan) |
|||
| < 1000 | 1107 (52.0) | 169 (15.8) | 900 (84.2) |
| 1000–1999 | 653 (30.7) | 112 (17.6) | 523 (82.4) |
| 2000–2999 | 237 (11.1) | 51 (22.3) | 178 (77.7) |
| ≥ 3000 | 131 (6.2) | 27 (20.9) | 102 (79.1) |
Note:
p<0.05;
p<0.01;
p<0.001.
Association between psychosocial factors and adherence
Bivariate associations between psychosocial factors and adherence are presented in Table 3. Seventeen percent (n=356) had ever used drugs in the past. Drug use was negatively associated with adherence to ART (p<0.01). Compared with their nonadherent counterparts, adherent PLHIV reported significantly lower perceived HIV stigma and side effects, and significantly higher adherence self-efficacy.
Table 3.
Associations between adherence to ART and psychosocial factors
| Variables | Total number of patients using ART (%) |
Adherence to ART, n (%) | |
|---|---|---|---|
| Nonadherent | Adherent | ||
| N | 2,146 | 365 (17.6) | 1713 (82.4) |
| Drug use | |||
| No | 1783 (83.4) | 280 (16.2) | 1451 (83.8)** |
| Ever used | 356 (16.6) | 81 (23.8) | 259 (76.2) |
| Depressive symptoms scale, mean (SD) | 7.18 (5.75) | 7.58 (6.09) | 7.03 (5.67) |
| Perceived HIV stigma scale, mean (SD) | 15.55 (3.51) | 16.10 (3.31) | 15.43 (3.53)** |
| Side effect severity | |||
| 0=Had no side effect | 1620 (77.5) | 248 (15.4) | 1362 (84.6)*** |
| 1=Had side effect with no influence on me | 159 (7.6) | 33 (21.0) | 124 (79.0) |
| 2=Had side effect with little influence on me | 253 (12.1) | 60 (24.0) | 190 (76.0) |
| 3=Had side effect with large/severe influence on me | 58 (2.8) | 22 (39.3) | 34 (60.7) |
| Adherence self-efficacy scale, mean (SD) | 45.80 (6.58) | 43.94 (7.44) | 46.22 (6.26)*** |
Note:
p<0.05;
p<0.01;
p<0.001.
Mediation analysis
Mediation analysis indicated that adherence self-efficacy significantly mediated the effect of side effects on adherence (Table 4 and Figure 1). In Model 1, adherence self-efficacy was negatively associated with side effect severity (regression coefficient=−0.692, SE=0.174, p<0.001), after controlling for key demographic and psychosocial factors (age, gender, ethnicity, residence, education, income, drug use, depressive symptoms, perceived HIV stigma). Model 2 showed that adherence was negatively associated with side effects (regression coefficient=−0.340, SE=0.065, p<0.001). In Model 3, when both side effects and adherence self-efficacy were included in the model, adherence was positively associated with adherence self-efficacy (regression coefficient=0.054, SE=0.009, p<0.001) while the significant direct effect of side effects on adherence was reduced (regression coefficient decreased from 0.340 to 0.300). The Sobel test indicated that the association between influence of side effect and adherence was significantly mediated by adherence self-efficacy (z=3.315, SE=0.011, p<0.001). In addition, Model 3 also showed that ART adherence was significantly associated with age, ethnicity, residence, household income, and perceived stigma.
Table 4.
Mediation analysis of the effect of adherence self-efficacy on the relationship of influence of side effect and adherence to ART
| Model 1: (X → M) | Model 2: (X → Y) | Model 3: (X, M → Y) | |
|---|---|---|---|
| DV=Self-efficacy (a) |
DV=Adherence (c) |
DV=Adherence (c′) (b) |
|
| Age | −0.027 (0.013)* | 0.016 (0.006)* | 0.017 (0.006)** |
| Gender | −0.112 (0.322) | 0.038 (0.138) | 0.048 (0.140) |
| Ethnicity | −0.103 (0.307) | −0.537 (0.140) | −0.566 (0.143)*** |
| Residence | 0.770 (0.381)* | −0.347 (0.154)* | −0.380 (0.158)* |
| Year of formal schooling | 0.178 (0.052)** | 0.053 (0.022)** | 0.044 (0.023) |
| Monthly household income | 0.298 (0.136)* | −0.134 (0.053)* | −0.157 (0.054)** |
| Drug use | −0.793 (0.429) | −0.303 (0.169) | −0.262 (0.171) |
| Depressive symptoms | −0.194 (0.026)*** | 0.000 (0.011)*** | 0.011 (0.012) |
| Perceived HIV stigma | 0.158 (0.042)*** | −0.048 (0.019)*** | −0.063 (0.019)** |
| Side effect severity | −0.692 (0.174)*** | −0.340 (0.065)*** | −0.300 (0.066)*** |
| Adherence self-efficacy | - | - | 0.054 (0.009)*** |
| Sobel test, z-value | −3.315 (0.011)*** |
Note: Numbers in the cells are unstandardized coefficients (SE).
X: Influence of side effect; M: Adherence self-efficacy; Y: Adherence to ART.
p<0.05;
p<0.01;
p<0.001.
Discussion
ART adherence is critical to achieve viral suppression and avoid drug resistance for PLHIV. In addition, optimal adherence can prevent HIV transmission to others who are at risk for infection and survival (Palella et al., 2003; Robbins, Spector, Mellins, & Remien, 2014). This study found that side effects from ART were negatively associated with adherence to ART, and adherence self-efficacy mediated the relationship between side effects and adherence. In addition, our results also indicated that HIV stigma was positively associated with adherence self-efficacy while stigma was negatively associated with medication adherence.
Social cognitive theory suggests that self-efficacy is an important factor on motivation, affect, and behaviors (Bandura, 1989). Self-efficacy enhances people’s task performances (Themanson & Rosen, 2015). People with strong self-efficacy may be more active and persistent in making efforts to follow their medical providers’ instructions (Buchmann, 1997). Although medication side effects may influence ART adherence, adherence self-efficacy, which includes the ability to overcome side effects, appears to channel the influence of side effects and enhance patients’ willingness to follow the instructions and thus remain adherent to ART. Adherence self-efficacy reflects patients’ confidence to carry out behaviors related to adhering to the ART regimen, being able to manage side effects, and dealing with ART related health problems.
The National Free Antiretroviral Treatment Program (NFATP) was put into effect in 2003 in China (Wu, Wang, Detels, & Rotheram-Borus, 2010). Guangxi is one of the successful examples of NFATP implementation (Leng et al., 2014). As showed in one study, CD4 cell count testing within 6 months of HIV diagnosis was 62% in 2009 in Yunan and Guangxi (Y. Zhang et al., 2011). When medication shortage is not the problem, increasing patients’ confidence to follow their health care provider’s recommendation seems to be a very important factor that may contribute to improving adherence. More research is needed to explore how to improve adherence self-efficacy.
Data in this study also indicated that several other factors were related to ART adherence. Adherence was higher among older patients, ethnic minorities, rural residents, and those with lower monthly income. Perceived HIV stigma was also negatively associated with adherence. HIV stigma in health care settings may interfere with PLHIV’s access to health care services including ART (Kinsler, Wong, Sayles, Davis, & Cunningham, 2007). HIV stigma may also prevent HIV serostatus disclosure.
There are several limitations in the current study. First, the causal interpretations need to be precluded because of the cross-sectional data. Future studies with a longitudinal design are needed to confirm the findings in the current study. Second, our findings were based on self-reported data which may be subject to various biases (e.g., social desirability bias and recall bias). Third,, we measured ART adherence using the number of days completing the medication in the last month since there are no optimal measures for adherence to date. Validation studies that combine patient self-reported adherence with the information of adherence from providers are needed in future studies.
Despite these limitations, this study provides important implications for developing future targeted interventions on optimal adherence to ART and other medication adherence as well. Because of a wide array of adherence barriers and facilitators, it has been challenging to develop effective interventions to improve long-term medication adherence. Future interventions to increase adherence self-efficacy and cope more effectively with side effects through education and counseling by medical providers are needed. Since some health providers may lack psychosocial intervention skills, theory-driven cognitive-behavioral interventions for both patients and medical providers may be needed to increase patients’ adherence self-efficacy, thus ART adherence.
Acknowledgments
The study was supported by National Institutes of Health (NIH) research grants R01HD074221 and R01AA018090 and National Natural Science Foundation of China (NSFC) (Grant # 71203098). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or NSFC. The authors want to thank local team members at Guangxi CDC for their efforts in instrument development and data collection.
References
- Ammassari A, Murri R, Pezzotti P, Trotta MP, Ravasio L, De Longis P, Antinori A. Self-reported symptoms and medication side effects influence adherence to highly active antiretroviral therapy in persons with HIV infection. J Acquir Immune Defic Syndr. 2001;28(5):445–449. doi: 10.1097/00042560-200112150-00006. [DOI] [PubMed] [Google Scholar]
- Bandura A. Human agency in social cognitive theory. American Psychologist. 1989;44(9):1175–1184. doi: 10.1037/0003-066x.44.9.1175. [DOI] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51(6):1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Buchmann WF. Adherence: A matter of self-efficacy and power. Journal of Advanced Nursing. 1997;26(1):132–137. doi: 10.1046/j.1365-2648.1997.1997026132.x. doi: [DOI] [PubMed] [Google Scholar]
- Chen WT, Shiu CS, Yang JP, Simoni JM, Fredriksen-Goldsen KI, Lee TS, Zhao H. Antiretroviral therapy (ART) side effect impacted on quality of life, and depressive symptomatology: a mixed-method study. J AIDS Clin Res. 2013;4:218. doi: 10.4172/2155-6113.1000218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chesney MA, Ickovics JR, Chambers DB, Gifford AL, Neidig J, Zwickl B, Wu AW. Self-reported adherence to antiretroviral medications among participants in HIV clinical trials: the AACTG Adherence Instruments. AIDS Care. 2000;12(3):255–266. doi: 10.1080/09540120050042891. [DOI] [PubMed] [Google Scholar]
- China Ministry of Health. 2012 China AIDS Response Progress Report. Beijing: China Ministry of Health; 2012. [Google Scholar]
- Friedland GH, Williams A. Attaining higher goals in HIV treatment: the central importance of adherence. AIDS. 1999;13(Suppl 1):S61–S72. [PubMed] [Google Scholar]
- Hailasillassie K, Etana B, Alemayehu M, Fisseha G. Factors associated with adherence of highly active antiretroviral therapy among adult HIV/AIDS patients in Mekelle Hospital Northern Ethiopia. Sci J Public Health. 2014;2(4):367–372. [Google Scholar]
- Johnson MO, Catz SL, Remien RH, Rotheram-Borus MJ, Morin SF, Charlebois E, Chesney MA. Theory-guided, empirically supported avenues for intervention on HIV medication nonadherence: findings from the Healthy Living Project. AIDS Patient Care STDS. 2003;17(12):645–656. doi: 10.1089/108729103771928708. [DOI] [PubMed] [Google Scholar]
- Johnson MO, Chesney MA, Goldstein RB, Remien RH, Catz S, Gore-Felton C, Morin SF. Positive provider interactions, adherence self-efficacy, and adherence to antiretroviral medications among HIV-infected adults: A mediation model. AIDS Patient Care STDS. 2006;20(4):258–268. doi: 10.1089/apc.2006.20.258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson MO, Dilworth SE, Taylor JM, Neilands TB. Improving coping skills for self-management of treatment side effects can reduce antiretroviral medication nonadherence among people living with HIV. Ann Behav Med. 2011;41(1):83–91. doi: 10.1007/s12160-010-9230-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson MO, Neilands TB, Dilworth SE, Morin SF, Remien RH, Chesney MA. The role of self-efficacy in HIV treatment adherence: Validation of the HIV treatment adherence self-efficacy scale (HIV-ASES) J Behav Med. 2007;30(5):359–370. doi: 10.1007/s10865-007-9118-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinsler JJ, Wong MD, Sayles JN, Davis C, Cunningham WE. The effect of perceived stigma from a health care provider on access to care among a low-income HIV-positive population. AIDS Patient Care STDS. 2007;21(8):584–592. doi: 10.1089/apc.2006.0202. [DOI] [PubMed] [Google Scholar]
- Kohout FJ, Berkman LF, Evans DA, Cornoni-Huntley J. Two shorter forms of the CES-D (Center for Epidemiological Studies Depression) depression symptoms index. J Aging Health. 1993;5(2):179–193. doi: 10.1177/089826439300500202. [DOI] [PubMed] [Google Scholar]
- Leng XB, Liang SJ, Ma YL, Dong YH, Kan W, Goan D, Shao YM. HIV virological failure and drug resistance among injecting drug users receiving first-line ART in China. Bmj Open. 2014;4(10):e005886. doi: 10.1136/bmjopen-2014-005886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li L, Sun GQ, Liang SJ, Li JJ, Li TY, Wang Z, Li JY. Different Distribution of HIV-1 Subtype and Drug Resistance Were Found among Treatment Naive Individuals in Henan, Guangxi, and Yunnan Province of China. PLoS One. 2013;8(10):e75777. doi: 10.1371/journal.pone.0075777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin XY, Zhao GX, Li XM, Stanton B, Zhang LY, Hong Y, Fang XY. Perceived HIV stigma among children in a high HIV-prevalence area in central China: beyond the parental HIV-related illness and death. AIDS Care. 2010;22(5):545–555. doi: 10.1080/09540120903253999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacDonell K, Jacques-Tiura JA, Naar S, Fernandez M ATN 086/106 Protocol Team. Predictors of self-reported adherence to antiretroviral medication in a multisite study of ethnic and racial minority HIV-positive youth. J Pediatr Psychol Online. 2015:1–10. doi: 10.1093/jpepsy/jsv097. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magidson JF, Blashill AJ, Safren SA, Wagner GJ. Depressive symptoms, lifestyle structure, and ART adherence among HIV-infected individuals: a longitudinal mediation analysis. AIDS Behav. 2015;19(1):34–40. doi: 10.1007/s10461-014-0802-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mills EJ, Nachega JB, Buchan I, Orbinski J, Attaran A, Singh S, Bangsberg DR. Adherence to antiretroviral therapy in sub-Saharan Africa and North America: a meta-analysis. JAMA. 2006;296(6):679–690. doi: 10.1001/jama.296.6.679. [DOI] [PubMed] [Google Scholar]
- Muessig KE, McLaughlin MM, Nie JM, Cai W, Zheng H, Yang L, Tucker JD. Suboptimal antiretroviral therapy adherence among HIV-infected adults in Guangzhou, China. AIDS Care. 2014;26(8):988–995. doi: 10.1080/09540121.2014.897912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Bureau of Statistics of China. Sixth national census data released. Beijing: National Bureau of Statistics of China; 2012. [access on September 12, 2012]. Avaible on http://www.stats.gov.cn/was40/gjtjj_detail.jsp?searchword=%C8%CB%BF%DA&channelid=6697&record=18. [Google Scholar]
- Palella FJ, Jr, Deloria-Knoll M, Chmiel JS, Moorman AC, Wood KC, Greenberg AE, Holmberg SD. Survival benefit of initiating antiretroviral therapy in HIV-infected persons in different CD4+ cell strata. Ann Intern Med. 2003;138(8):620–626. doi: 10.7326/0003-4819-138-8-200304150-00007. [DOI] [PubMed] [Google Scholar]
- Rao D, Kekwaletswe TC, Hosek S, Martinez J, Rodriguez F. Stigma and social barriers to medication adherence with urban youth living with HIV. AIDS Care. 2007;19(1):28–33. doi: 10.1080/09540120600652303. [DOI] [PubMed] [Google Scholar]
- Reda AA, Biadgilign S. Determinants of adherence to antiretroviral therapy among HIV-infected patients in Africa. AIDS Res Treat. 2012;2012:574656. doi: 10.1155/2012/574656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robbins RN, Spector AY, Mellins CA, Remien RH. Optimizing ART adherence: Update for HIV treatment and prevention. Curr HIV/AIDS Rep. 2014;11(4):423–433. doi: 10.1007/s11904-014-0229-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sayles JN, Wong MD, Kinsler JJ, Martins D, Cunningham WE. The association of stigma with self-reported access to medical care and antiretroviral therapy adherence in persons living with HIV/AIDS. J Gen Intern Med. 2009;24(10):1101–1108. doi: 10.1007/s11606-009-1068-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherr L, Lampe FC, Clucas C, Johnson M, Fisher M, Date HL, Harding R. Self-reported non-adherence to ART and virological outcome in a multiclinic UK study. AIDS Care. 2010;22(8):939–945. doi: 10.1080/09540121.2010.482126. [DOI] [PubMed] [Google Scholar]
- Sobel ME. Asymptotic intervals for indirect effects in structural equations models. In: Leinhart S, editor. Sociological methodology. San Francisco: Jossey-Bass; 1982. pp. 290–312. [Google Scholar]
- Starks H, Simoni J, Zhao H, Huang B, Fredriksen-Goldsen K, Pearson C, Zhang F. Conceptualizing antiretroviral adherence in Beijing, China. AIDS Care. 2008;20(6):607–614. doi: 10.1080/09540120701660379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Themanson J, Rosen P. Examining the relationships between self-efficacy, task-relevant attentional control, and task performance: Evidence from event-related brain potentials. British Journal of Psychology. 2015;106(2):253–271. doi: 10.1111/bjop.12091. [DOI] [PubMed] [Google Scholar]
- UNAIDS. Global report: UNAIDS report on the global AIDS epidemic 2013. Geneva: UNAIDS; 2013. [Google Scholar]
- Viswanathan S, Detels R, Mehta SH, Macatangay BJC, Kirk GD, Jacobson LP. Level of adherence and HIV RNA suppression in the current era of highly active antiretroviral therapy (HAART) AIDS Behav. 2015;19(4):601–611. doi: 10.1007/s10461-014-0927-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. Adherence to long-term therapies: Eevidence for action. Geneva, Switzerland: World Health Organization; 2003. [Access on Novermber 15, 2014]. http://www.who.int/chp/knowledge/publications/adherence_full_report.pdf?ua=1. [Google Scholar]
- Wu ZY, Wang Y, Detels R, Rotheram-Borus MJ. China AIDS policy implementation: reversing the HIV/AIDS epidemic by 2015. International Journal of Epidemiology. 2010;39:Ii1–Ii3. doi: 10.1093/ije/dyq220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang F, Dou Z, Ma Y, Zhang Y, Zhao Y, Zhao D, Chen RY. Effect of earlier initiation of antiretroviral treatment and increased treatment coverage on HIV-related mortality in China: a national observational cohort study. Lancet Infect Dis. 2011;11(7):516–524. doi: 10.1016/S1473-3099(11)70097-4. [DOI] [PubMed] [Google Scholar]
- Zhang Y, Lu L, Li HQ, Liu W, Tang ZR, Fang H, Zhang FJ. Engaging HIV-infected patients in antiretroviral therapy services: CD4 cell count testing after HIV diagnosis from 2005 to 2009 in Yunnan and Guangxi, China. Chinese Medical Journal. 2011;124(10):1488–1492. [PubMed] [Google Scholar]
- Zheng H, Wang L, Huang P, Norris J, Wang Q, Guo W, Wang N. Incidence and risk factors for AIDS-related mortality in HIV patients in China: a cross-sectional study. BMC Public Health. 2014;14:831–839. doi: 10.1186/1471-2458-14-831. [DOI] [PMC free article] [PubMed] [Google Scholar]