Abstract
Background: Chronic low-back pain (LBP) is a frequent cause of work absence and disability, and is frequently associated with long-term use of opioids.
Objective: To describe military readiness-related outcomes at follow-up in soldiers with LBP grouped by the type of early treatment received for their LBP. Treatment groups were based on receipt of opioid or tramadol prescription and receipt of nonpharmacologic treatment modalities (NPT).
Design, Subjects, Measures: A retrospective longitudinal analysis of U.S. soldiers with new LBP episodes persisting more than 90 days between October 2012 and September 2014. Early treatment groups were constructed based on utilization of services within 30 days of the first LBP claim. Outcomes were measured 91–365 days after the first LBP claim. Outcomes were constructed to measure five indicators of limitations of military readiness: military duty limitations, pain-related hospitalization, emergency room visit for LBP, pain score of moderate/severe, and prescription for opioid/tramadol.
Results: Among soldiers with no opioid receipt in the prior 90 days, there were 30,612 new episodes of LBP, which persisted more than 90 days. Multivariable logistic regression models found that compared to the reference group (no NPT, no opioids/tramadol receipt), soldiers who received early NPT-only had lower likelihoods for military duty limitations, pain-related hospitalization, and opioid/tramadol prescription at follow-up, while soldiers' that started with opioid receipt (at alone or follow-up in conjunction with NPT) exhibited higher likelihoods on many of these negative outcomes.
Conclusion: This observational study of soldiers with a new episode of LBP and no opioid receipt in the prior 90 days suggests that early receipt of NPT may be associated with small, significant gains in ability to function as a soldier and reduced reliance on opioid/tramadol medication. While further research is warranted, increased access to NPT at the beginning of LBP episodes should be considered.
Keywords: : complementary services, integrative healthcare, low-back pain, opioids, military
Introduction
Low-back pain (LBP) is a significant cause of adult disability and economic burden in the United States (US).1 LBP is also of particular concern for the Department of Defense (DoD) and the health and readiness of its military population,2,3 with an overall incidence of LBP among active duty service members of 40.5 per 1000 person-years, with Army soldiers at greater risk.3,4 Even though military members are on average in better physical condition than the average U.S. citizen, they endure greater physical challenges and must meet rigorous standards for force readiness, which make them more susceptible to LBP injuries.5,6
Opioids are commonly prescribed for moderate and severe acute pain, yet long-term opioid use is associated with an increased drug tolerance, risk of opioid use disorder, and overdose.7,8 Furthermore, the effectiveness of long-term opioid therapy is limited.7,9–15 A study of active duty members serving in 2010 revealed that 26.4% received at least one opioid prescription.16 In 2017, the VA/DoD Clinical Practice Guideline for Opioid Therapy for Chronic Pain was updated and included a specific recommendation against initiation of long-term opioid therapy.9,17 The Army's Pain Management Task Force set an objective to reduce reliance on opioids and incorporate NPT modalities into a patient-centered plan of care, which includes training for clinicians on acupuncture and establishment, in some locations, of interdisciplinary pain management centers, which make available nonpharmacologic treatments (NPT).18
NPT for LBP include exercise therapy, often supervised by physical therapists, and a variety of complementary and integrative therapies, including chiropractic, massage, and acupuncture.18–23,24 Studies of acute LPB have shown efficacy for exercise therapy25 and spinal manipulation.26,27 Acupuncture has been shown to be beneficial for addressing acute pain in the emergency department28 and in a military setting.29 This study seeks to address gaps in the evidence base for NPT by evaluating the outcomes associated with choice of early treatment (first 30 days) in a new episode of LBP in the Military Health System (MHS). Treatments examined include NPT, opioids, and tramadol. The MHS provides an ideal setting because it has adopted a broad variety of nonpharmacologic modalities, and when NPT are ordered by clinicians, it is recorded in the MHS records. To evaluate outcomes, the authors focus on five indicators that are related to military readiness, the soldier's ability to deploy on a mission or perform their usual military duties. Military readiness outcomes are measured 91–365 days after the first LBP encounter, and include the following: use of prescription opioids, ability to carry on military functions, utilization of inpatient hospitalizations and emergency department visits, and self-reported moderate or severe pain.
Methods
Setting and data
For this retrospective study, the authors examined DoD MHS healthcare utilization data to identify all active duty soldiers with new episodes of LBP between October 2012 to September 2014. The authors identified all treatment services provided at military treatment facilities (MTFs) or purchased through the military's TRICARE health plan. MHS medical records have complete diagnosis and procedure codes of all MTF encounters and from claims submitted by civilian providers. Pharmacy files capture all prescription medications dispensed by MTFs, retail pharmacies, and mail order. Because healthcare provided by the military on operational missions (e.g., combat) is not recorded in the MHS database, LBP care in this environment was excluded.
Sample and episode construction
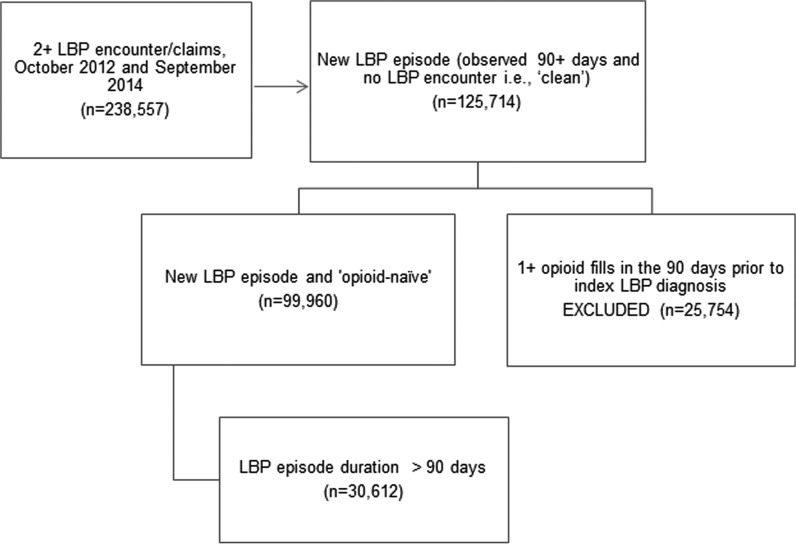
The sample consisted of soldiers on active duty, who experienced a new episode of LBP. The start of a new LBP episode was defined as the first (index) encounter with an LBP diagnosis in the primary diagnostic position, with no LBP diagnoses in the preceding 90 days (Flow Diagram Fig. 1). The authors searched all ambulatory medical encounters for LBP diagnosis codes 720–724, (except 720.0, 723.4, and 723.8) and 756.130,31 among soldiers who met the criterion of two separate LBP encounters during the study observation window. Excluded as index episodes were those in which the observation days before the first LBP encounter was less than 90 (to establish a clean period), and LBP encounters associated with a pregnancy and childbirth. After exclusions, there were 125,447 soldiers with new LBP episodes. The analysis sample was then restricted to opioid-naive soldiers, defined as no prescription opioid or tramadol fill for the preceding 90 days (n = 99,960). For outcomes' analyses reported in this article, the analyses were restricted to soldiers with episodes that lasted longer than 90 days (n = 30,612).
FIG. 1.
Selection of opioid-naive sample with new low-back pain episode duration greater than 90 days. LBP, low-back pain.
Utilization during the LBP episode included all subsequent LBP records with an LBP diagnosis code in the primary or secondary position, inclusive of physical therapy (ICD9 diagnosis V57.1), as well as opioid prescription records with fill dates on or between the dates of the first and last LBP encounters.32 The episode end was defined by the beginning of 90 days with no subsequent LBP diagnosis. For prescription users, the episode end was extended to the day the opioid supply ran out based on date of fill and days supply.
Follow-up status outcome measures
Study outcomes consisted of five dichotomous indicators of reduced military readiness during the sample subject's follow-up window, which started at 91 days after the first LBP encounter and ended at 365 days or the end of the soldier's MHS data if that occurred earlier. Military duty limitation was identified by an LBP encounter record with a disposition code of temporary duty limitation or assignment to quarters. Pain-related hospitalization was identified by an overnight stay with a principal diagnosis within eight major diagnostic categories plausibly related to chronic pain or its treatment (Table available upon request). An LBP emergency department (ED) encounter was identified as an encounter with any LBP diagnosis and ED place of service. Moderate or severe pain score was defined as 4 or greater for any pain score reported during follow-up on MHS standard vital records.33 Self-report pain scores were based on the 0–10 Numeric Rating Scale with cut points for moderate pain scores (4–6) and severe pain scores (7–10).34 A final follow-up outcome was created for any prescription opioid or tramadol fill.
Early treatment groups for LBP—key independent variables
Five mutually exclusive “early treatment” groups were created based on the services and medications the soldiers received during the first 30 days of their LBP episodes: NPT only, opioid only, NPT and opioid, tramadol only, and NPT and tramadol. The reference group for the logistic models consisted of soldiers who received neither NPT nor a prescription opioid or tramadol fill during the first 30 days of their LBP episode. NPT modalities used in this study include exercise-related therapies, chiropractic procedures, massage and manual therapies, traction, superficial heat, acupuncture, biofeedback, and other physical therapy procedures (e.g., [whirlpool baths], TENS, and other electrical modulation [further definition and procedure codes found in Table 1]), and were based on the Chou et al.,23,24 review of evidence of nonpharmacologic modalities for LBP for the American Pain Society/American College of Physicians Clinical Practice Guideline. Any use of these 14 modalities in the first 30 days of the episode identified the soldier as receiving early NPT.
Table 1.
Percent with Early Receipt and Any Receipt of Nonpharmacologic Treatments, and Mean Encounters (n = 30,612)
| Mean NPT encounters during total episode | ||||
|---|---|---|---|---|
| Modality received | Percent with early receipt (first 30 days of the LBP episode) | Percent with receipt any time during episode | Meana | ± SD |
| Total | 44.0 | 84.4 | 14.4 | 15.1 |
| Exercise therapy | 26.0 | 63.0 | 7.4 | 8.0 |
| Superficial heat | 14.1 | 42.3 | 6.3 | 6.5 |
| Other physical therapy | 13.9 | 44.5 | 7.4 | 7.2 |
| TENS | 13.6 | 41.9 | 5.7 | 6.4 |
| Chiropractic | 11.6 | 29.3 | 7.3 | 7.2 |
| Massage | 11.0 | 33.2 | 5.6 | 7.0 |
| Spinal Manipulation | 8.1 | 20.4 | 2.4 | 2.9 |
| Traction | 5.8 | 21.3 | 6.2 | 6.0 |
| Self-Care | 4.7 | 17.6 | 2.2 | 2.8 |
| Acupuncture | 2.4 | 11.9 | 3.4 | 4.2 |
| Ultrasonography | 1.1 | 3.8 | 5.3 | 7.1 |
| Lumbar supports | 0.5 | 3.6 | 1.1 | 0.4 |
| Biofeedback | 0.4 | 2.6 | 2.1 | 1.9 |
| Cold laser | 0.0 | 0.1 | 3.9 | 3.5 |
Multiple procedures could be contained on one encounter; mean of all NPT procedures represent unduplicated number of encounters
Definition of procedures and procedure codes:
Exercise therapy (pilates, yoga, and therapeutic exercise; neuromuscular re-education; therapeutic activities): ICD9 Diagnosis Codes V65.41, CPT Procedure Codes 97110, 97112, 97113, 97116, 97150, and 97530, HCPCS Codes 4242F and S9451
Superficial heat (infrared and shortwave diathermy): CPT Procedure Codes 97010, 97018, 97024, and 97026
Other physical therapy (hot or cold packs, whirlpool bath, and contrast baths): ICD9 Diagnosis Codes V57.1, CPT Procedure Codes 97016, 97022, and 97036
TENS and Other Electrical Modulation: CPT Procedure Codes 97014 and 97032, HCPCS Codes 0278T, A4595, E0720, E0730, E0770, and G0281 - G0283
Chiropractic: CPT Procedure Codes 98940–98943
Massage hot and cold packs, manual therapy techniques (e.g., mobilization/manipulation, manual lymphatic drainage, and manual traction): CPT Procedure Codes 97010, 97124, and 97140
Spinal Manipulation (physical or manipulative therapy): CPT Procedure Codes 98925-98929 and S9090
Traction: CPT Procedure Codes 97012, HCPCS Codes E0941 and E0944
Self-Care/management: CPT Procedure Codes 96152-96155, 97535, 98960-98962, 99071, 99078, and 99605-99607, HCPCS Codes 4450F, G8780, S9445, and S9446
Acupuncture/dry needling: CPT Procedure Codes 97810-97814, HCPCS Codes S8930 and S8990
Ultrasonography (Ultrasound therapy): CPT Procedure Codes 97033 and 97035
Lumbar supports (back braces): HCPCS Codes L0621, L0623, L0625-L0628, L0630, L0631, L0633, L0634, L0637, L0638, L0972, L0976, and L1005
Biofeedback: CPT Procedure Codes 90875-90876 and 90901-90910
Cold laser (low level laser): CPT Procedure Codes 97039, HCPCS Codes S8948
CPT, current procedure terminology; HCPCS, healthcare common procedure coding system; ICD9, international classification of diseases, ninth revision; LBP, low back-pain; NPT, nonpharmacologic treatment; TENS, transcutaneous electrical nerve stimulation.
Early opioid treatment was defined as at least one fill of an opioid prescription other than tramadol in the first 30 days of the episode. Opioids were identified based on the prescription drug classification of the Centers for Disease Control and Prevention.35 Certain partial opioids used to treat addiction were excluded (e.g., buprenorphine). While tramadol is a synthetic weak opioid analgesic and now classified as an opioid, it was not a controlled substance until the end of the study period. Thus, the authors established a separate early tramadol treatment group, which was defined as at least one fill of a tramadol prescription during the first 30 days when there was no opioid fill.
Also, a treatment intensity indicator for more than 7 days supply of opioids or tramadol within the first 30 days of the episode was included because current research suggests it is an added risk factor for long-term opioid use.36
Covariates
Covariates for the logistic regressions included soldier characteristics, treatment facility, and soldier status at treatment start. Soldier characteristics were derived from MHS demographic and enrollment records and included age category, gender, military rank group, race/ethnicity, and deployment status. Covariates for the practices and resources of the treating provider and care setting included the index encounter's MTF clinic location (primary care, orthopedic/physical therapy or other rehabilitation, urgent care, other MTF, or purchased care), treatment region, type of setting as a proxy for MTF size, and provider type (physician, physician assistant/advanced practice nurse, and other). To control for baseline status, covariates also were included for the soldier's status within the first 30 days of the episode regarding any pain score moderate, any pain score severe, or military duty limitation/hospitalization.
Statistical analyses
Univariate and bivariate analyses describe the receipt of NPT modalities, estimates of the mean NPT encounters by modality, and associations of the demographic, deployment, and clinical characteristics of soldiers with LBP episodes with early treatment group. Following these preliminary analyses, five separate multivariable logistic regression models were estimated to examine the association of early treatment group with each follow-up status dichotomous outcome adjusted for covariates. These models included all demographic characteristics, type of clinic, MTF type, provider type, and patient status covariates, including pain score moderate, pain score severe, and military duty limitation/hospitalization measured during the 30 days after index LBP encounter, although the coefficients are not presented in the tables. Odds ratios (ORs), significance tests using two-sided alternatives and p ≤ 0.05, and 95% confidence intervals (CI) were reported for each treatment group. Statistical analyses were performed with SPSS version 19.0.0.
This study was approved by Brandeis University's Committee for Protection of Human Subjects and the Human Research Protection Program at the Office of the Assistant Secretary of Defense Health Affairs.
Results
Treatment of new LBP episodes had varying duration. Less than one-third (30.6%) of new LBP episodes were chronic (longer than 90 days), with 15.5% lasting between 91 and 180 days and 15.1% lasting longer than 6 months.
Table 1 describes the receipt of NPT modalities, the mean number of NPT encounters, and receipt of NPT during the first 30 days, among episodes of LBP with 90 days of duration or longer (n = 30,612). The majority (66.3%) received exercise therapy sometime during their treatment. Other modalities with utilization by one-third or more of the sample included superficial heat, other physical therapy, and transcutaneous electrical nerve stimulation. Acupuncture, biofeedback, and cold laser, modalities commonly considered alternative, were infrequently received; chiropractic care exceeded one-quarter of episodes. The mean encounters over the episode for exercise therapy, other physical therapy, and chiropractic care exceeded 7.
Also, shown is the distribution of treatment receipt during the first 30 days (early treatment).
Regarding distribution of early treatment groups: 36% received NPT alone, and 8% received NPT in combination with an opioid or tramadol; 10% received an opioid prescription alone and 6% received tramadol alone. About 40% did not receive any of these treatments and thus formed the reference group. Comparisons of characteristics of soldiers in each early treatment group versus soldiers in the reference group found only small differences. The exception was that the opioid and tramadol early treatment groups had more soldiers with severe pain scores than the reference group and NPT group (Table 2).
Table 2.
Characteristics of Soldiers with Low-Back Pain Episodes By Early Treatment Group
| Percent distribution by LBP early treatment receipta | |||||||
|---|---|---|---|---|---|---|---|
| Reference group | NPT only | Opioid only | Opioid and NPT | Tramadol only | Tramadol and NPT | Total | |
| Total N | 12,072 | 11,000 | 3,143 | 1,523 | 1,931 | 943 | 30,612 |
| Age group | |||||||
| ≤24 years | 15.6% | 19.2% | 15.6% | 16.5% | 19.1% | 19.1% | 18.4% |
| 25–34 | 40.5% | 42.2% | 40.5% | 42.1% | 42.2% | 45.7% | 40.1% |
| 35–44 | 35.3% | 30.9% | 35.3% | 32.2% | 30.9% | 28.8% | 33.0% |
| ≥45 | 8.6% | 7.8% | 8.6% | 9.3% | 7.8% | 6.4% | 8.5% |
| Gender | |||||||
| Female | 15.6% | 18.5% | 14.6% | 17.3% | 14.4% | 14.6% | 16.5% |
| Male | 84.4% | 81.5% | 85.4% | 82.7% | 85.6% | 85.4% | 83.5% |
| Rank group | |||||||
| Junior enlisted | 33.8% | 33.0% | 30.2% | 30.9% | 33.7% | 39.1% | 33.2% |
| Senior enlistedb | 47.0% | 44.6% | 52.2% | 50.0% | 51.7% | 47.3% | 47.1% |
| Junior officer | 5.8% | 7.3% | 5.0% | 5.6% | 5.4% | 5.1% | 6.2% |
| Senior officer | 11.1% | 13.2% | 9.8% | 12.0% | 8.1% | 8.0% | 11.5% |
| Race/ethnicity | |||||||
| White, Non-Hispanic | 57.4% | 59.0% | 61.5% | 60.5% | 57.5% | 59.9% | 58.6% |
| Black, Non-Hispanic | 22.4% | 20.3% | 20.9% | 20.7% | 23.0% | 19.8% | 21.4% |
| Hispanic | 11.9% | 12.0% | 10.2% | 11.2% | 11.8% | 12.9% | 11.8% |
| Other or unknownc | 8.2% | 8.7% | 7.4% | 7.7% | 7.7% | 7.3% | 8.2% |
| Deployment status | |||||||
| Never deployed | 21.2% | 20.4% | 18.5% | 20.5% | 20.0% | 22.5% | 20.6% |
| 1 or more prior FY12 | 61.8% | 61.1% | 65.9% | 64.3% | 63.7% | 62.0% | 62.2% |
| 1 or more after FY12 but before index | 17.0% | 18.5% | 15.6% | 15.2% | 16.3% | 15.5% | 17.2% |
| Pain scored | |||||||
| Mild, othere | 53.3% | 55.1% | 41.9% | 31.3% | 43.5% | 37.0% | 55.1% |
| Moderate (4–6) | 29.3% | 29.7% | 24.9% | 31.5% | 28.2% | 32.8% | 29.1% |
| Severe (7–10) | 17.4% | 15.1% | 33.2% | 37.3% | 28.3% | 30.2% | 20.3% |
| Duty limitationd | |||||||
| None | 68.4% | 68.9% | 55.6% | 49.6% | 56.6% | 64.9% | 64.9% |
| Some | 31.6% | 31.1% | 43.4% | 50.4% | 43.4% | 35.1% | 35.1% |
| Provider typef | |||||||
| Physician | 37.0% | 20.7% | 48.8% | 36.7% | 32.6% | 24.8% | 31.7% |
| PA/APRN | 54.6% | 30.7% | 45.8% | 38.2% | 63.6% | 56.5% | 44.9% |
| All othersg | 8.4% | 48.6% | 5.3% | 25.1% | 3.8% | 18.7% | 23.4% |
All treatment indicators measured during first 30 days of LBP episode. For each treatment, the reference group is soldiers without NPT or opioids or tramadol.
Includes other/unknown (n = 128).
Includes Asian, Native American, Other, unknown.
Measured in first 30 days after index LBP encounter.
Includes none, 1–3, not reported.
Based on first LBP encounter.
Includes urgent care, other locations, and purchased care.
Note: chi-square statistic for each bivariate association with early treatment group was significant at p ≤ 0.001
APRN, advanced practice registered nurse; LBP, low-back pain; NPT, nonpharmacologic treatment; PA, physician assistant.
The Appendix Table A1 presents the distribution on each follow-up outcome for each early treatment group. Relative to the reference group, the group with early NPT receipt had a lower percent of patients with duty limitation (ref = 37.5%, NPT = 33.4%), pain-related inpatient stay (ref = 4.7%, NPT = 3.2%), emergency department visit (ref = 5.4%, NPT = 4.6%), and opioid/tramadol use (ref = 31.6%, NPT = 28.7%) at follow-up; and it had a higher percent of patients with moderate/severe pain (ref = 53.4%, NPT = 51.9%). By contrast, the groups with early opioid or tramadol receipt had a higher percent of patients with these negative outcomes than the reference group.
Table 3 presents the estimated effects of early treatment on each outcome from the logistic modeling. Only the odds ratios for the early treatment group indicators are provided, but the logistic models included all covariates described in the methods. The table notes that, compared with the reference group, the NPT group had reduced odds for two of the four functional status outcomes: military duty limitations (OR 0.86, CI 0.81–0.91, p-value ≤0.001) and an inpatient stay for a pain-related condition (OR 0.68, CI 0.58–0.79, p-value ≤0.001) (Table 3). In addition, early NPT significantly reduced the odds, relative to the reference group, of opioid or tramadol use during follow-up (OR 0.91, CI 0.85–0.96, p ≤ 0.001).
Table 3.
Logistic Regression Models of 5 Follow-up Military Readiness Outcomes (n = 30,612)
|
LBP early treatment groupsb Adjusted odds ratios and 95% confidence interval |
||||||
|---|---|---|---|---|---|---|
| Follow-up Outcome Modela | NPT only | Opioid onlyc | Opioid and NPTc | Tramadol only | Tramadol and NPT | Treatment intensityc: Opioid days supply >7 days |
| Military Duty Limitation | 0.86*** [0.81–0.91] | 1.14*** [1.04–1.26] | 1.06 [0.94–1.20] | 1.09 [0.97–1.23] | 1.08 [0.93–1.26] | 1.04 [0.94–1.14] |
| Pain-related inpatient stay | 0.68*** [0.58–0.79] | 1.15 [0.94–1.41] | 1.08 [0.84–1.33] | 0.97 [0.75–1.24] | 0.80 [0.57–1.11] | 1.36*** [1.12–1.64] |
| ED visit for LBP | 0.90 [0.79–1.03] | 1.73*** [1.46–2.04] | 1.42*** [1.15–1.76] | 0.99 [0.79–1.24] | 1.04 [0.78–1.38] | 1.13 [0.96–1.32] |
| Moderate or Severe pain | 1.06 [0.99–1.12] | 1.20*** [1.09–1.33] | 1.25*** [1.11–1.42] | 1.26*** [1.12–142] | 1.28*** [1.10–1.49] | 0.96 [0.87–1.05] |
| Opioid or tramadol use | 0.91*** [0.85–0.96] | 1.67*** [1.52–1.84] | 1.46*** [1.29–1.65] | 1.66*** [1.48–1.86] | 1.42*** [1.23–1.65] | 1.60*** [1.46–1.76] |
Each regression model included covariates for gender, age group, race/ethnicity group, rank group, deployment status, region, and provider type, MTF clinic, MTF size, and patient status covariates measured in first 30 days of the LBP episode (moderate pain score, severe pain score, and military duty limitation/hospitalization). The table in the appendix displays the results of the full model for a single outcome measure, military duty limitation.
Follow-up window was 91–365 days after index LBP encounter.
All treatment indicators measured during first 30 days of LBP episode. For each treatment, the reference group is soldiers without NPT or opioids or tramadol.
The full impact of opioid treatment is the sum of the opioid treatment coefficient and treatment intensity coefficient.
p ≤ 0.001.
ED, emergency department; LBP, low-back pain; MTF, military treatment facility; NPT, nonpharmacologic treatment included in the study.
Table 3 also shows that early opioid treatment and early tramadol treatment were associated with greater odds of opioid/tramadol use during follow-up (OR 1.67, CI 1.52–1.84, p ≤ 0.001, and OR 1.66, CI 1.48–1.86, p ≤ 0.001, respectively). Early opioid treatment was also associated with greater odds of military duty limitation and ED visit for LBP during follow-up, and both early opioid and early tramadol treatments predicted greater likelihood of moderate or severe pain during follow-up. Finally, as an ancillary issue regarding early opioid treatment, the logistic models determined that among soldiers with an opioid/tramadol fill during the first 30 days, a supply for more than 7 days rather than 7 days or less was associated with greater likelihood for a pain-related inpatient stay and for opioid/tramadol receipt during the follow-up window.
To provide an idea of the effects of other covariates on military functional status, full logistic model results for one outcome, military duty limitation, are reported in Table 4. Other covariates that increased the odds of military duty limitation after 90 days were severe pain or military duty limitation during the first 30 days of the LBP episode and characteristics of the first encounter (seeing a physician assistant or advanced practice nurse practitioner relative to a physician and presenting to urgent care relative to primary care). Covariates that reduced the odds were serving in the west region (relative to the north), treatment at the largest-sized MTF or a military hospital (relative to an ambulatory clinic), being older than 45 years old (relative age 24 or under), having race identification of American Indian or Alaskan Native (relative to white), being in any rank group other than junior enlisted, and having a very recent deployment (relative to no prior deployment).
Table 4.
Full Logistic Regression Model on Military Duty Limitation Outcome (n = 30,612)
| 95% CI | ||||
|---|---|---|---|---|
| Variables | Odds ratio | p value | Lower | Upper |
| Early treatment groupa (ref = otherb) | ||||
| NPT only | 0.86 | 0.000 | 0.805 | 0.914 |
| Opioid only | 1.14 | 0.009 | 1.035 | 1.261 |
| Tramadol only | 1.09 | 0.150 | 0.969 | 1.225 |
| NPT and opioid | 1.06 | 0.360 | 0.936 | 1.200 |
| NPT and tramadol | 1.08 | 0.316 | 0.929 | 1.255 |
| Treatment Intensity, opioid days >7, yes (ref = 1–7) | 1.03 | 0.482 | 0.94 | 1.139 |
| Clinical covariatesa | ||||
| Moderate Pain (4–6), yes (ref = 0–3 or missing) | 0.99 | 0.753 | 0.936 | 1.049 |
| Severe Pain (7–10), yes (ref = 0–3 or missing) | 1.09 | 0.007 | 1.025 | 1.167 |
| Duty limitation, yes (ref = no) | 2.05 | 0.000 | 1.945 | 2.157 |
| Region (ref = TRICARE North) | ||||
| TRICARE South | 0.98 | 0.556 | 0.918 | 1.047 |
| TRICARE West | 0.88 | 0.000 | 0.819 | 0.939 |
| OCONUS | 1.04 | 0.406 | 0.946 | 1.147 |
| Provider type (ref = physician) | 0.006 | |||
| PA/APRN | 1.10 | 0.002 | 1.034 | 1.168 |
| All others | 1.09 | 0.072 | 0.992 | 1.202 |
| Care location (ref = primary care) | ||||
| Orthopedic/PT/OT/Chiropractor | 0.98 | 0.723 | 0.88 | 1.092 |
| Urgent care | 1.21 | 0.006 | 1.057 | 1.395 |
| All other locations | 1.10 | 0.066 | 0.994 | 1.211 |
| Not available | 1.14 | 0.879 | 0.207 | 6.285 |
| Facility type (ref = Mil. Ambulatory Clinic) | ||||
| Military Hospital | 0.90 | 0.003 | 0.842 | 0.966 |
| Military Medical Center | 0.94 | 0.159 | 0.855 | 1.026 |
| VHA or civilian facility | 0.82 | 0.823 | 0.15 | 4.526 |
| Female (ref = male) | 1.02 | 0.510 | 0.956 | 1.095 |
| Age in years (ref = 24 & under) | 0.004 | |||
| 25–34 | 1.01 | 0.879 | 0.933 | 1.084 |
| 35–44 | 0.94 | 0.161 | 0.861 | 1.025 |
| ≥45 | 0.83 | 0.004 | 0.738 | 0.943 |
| Race (ref = white) | 0.017 | |||
| Black | 0.97 | 0.429 | 0.916 | 1.038 |
| Hispanic | 1.01 | 0.760 | 0.937 | 1.093 |
| Asian | 0.91 | 0.109 | 0.806 | 1.022 |
| American Indian/Alaskan Native/Other | 0.59 | 0.002 | 0.428 | 0.824 |
| Other/unknown | 0.92 | 0.240 | 0.795 | 1.059 |
| Rank (ref = Junior enlisted) | 0.000 | |||
| Senior enlisted | 0.74 | 0.000 | 0.692 | 0.794 |
| Junior officer | 0.49 | 0.000 | 0.438 | 0.553 |
| Senior officer | 0.40 | 0.000 | 0.363 | 0.452 |
| Other/unknown | 0.04 | 0.000 | 0.025 | 0.071 |
| Deployment (ref = no deployment) | 0.051 | |||
| 1 or more before October 2013 | 0.96 | 0.282 | 0.896 | 1.033 |
| 1 or more after October 2013 but before index encounter | 0.90 | 0.017 | 0.834 | 0.982 |
| Constant | 0.67 | 0.000 | ||
The results are for one dependent variable, military duty limitation, during the follow-up window. The follow-up window was 91–365 days after index LBP encounter.
Early treatment measured in first 30 days after index LBP encounter.
Reference group is no nonpharmacologic treatment modalities (NPT) and no opioid or tramadol prescription.
APRN, advanced practice registered nurse; CI, confidence interval (associated with the Odds Ratio); PA, physician assistant; PT, physical therapy; OT, occupational therapy; VHA, Veterans Health Administration.
Discussion
The authors establish in this observational study that, receipt of NPT services in the first 30 days of an LBP episode was associated with modest improvements on many important military readiness outcomes.23,24,37 The finding that opioid use was lessened in the early NPT group is potentially of great significance and would be important to replicate in future clinical trial studies.
A particular strength of this study is that the authors were able to evaluate a relatively comprehensive set of NPT modalities used as early treatment for LBP and examined the association of NPT with longer term outcomes related to military readiness, including indicators of healthcare utilization, long-term opioid use, and ability to carry out military duties. The Army has consciously decided to include acupuncture, chiropractic care, and interdisciplinary pain centers within some MTFs,38–40 thus NPT use among military members may be higher than among civilians.41
Biopsychological services and interdisciplinary pain management have been proven effective for individuals with many types of chronic pain.42,43 Understanding that early moderate-severe pain is a significant warning signal for refractory pain may prod health systems to add a psychosocial approach for some individuals with acute pain. Such an approach might include cognitive behavioral therapy44,45 or a mind–body program,46 and might involve treatment in a group setting.47 Posttraumatic stress disorder, depression, and history of smoking have been linked in prior research to increased likelihood of opioid receipt and increased experiences of pain.48–51 It would appear important for clinicians to identify whether or not the warning signal of moderate–severe pain is identifying individuals with these complex histories and to consider augmenting early treatment with NPT and psychosocial services.
These findings also indicate the importance of further investigation of the long-term status of patients receiving opioids as part of their treatment. They reinforce the importance that providers attend to the current opioid prescription guidelines that call for limiting opioid exposure, when possible as first-line treatment in LBP, and promoting early introduction of nonpharmacological treatment.7,9,52
This study has several limitations. First, these findings are specific to the relatively young, Army active duty population that the authors studied, and the associations found in this study may differ in non-military, older individuals and individuals treated in private or public healthcare settings. Although the authors controlled for a broad range of clinical factors at the beginning of treatment (age, gender, pain score, duty limitations, new episode, and no prior opioid prescription in past 90 days), there may be important unobserved differences between the reference group and those that started either NPT service or opioid/tramadol that contributes to these results. One might, for example, postulate that soldiers with lower motivation declined NPT. The authors used a broad definition of early NPT and did not capture the skill of provider, effectiveness of care, or quantity of NPT received. However, if the methods combined effective and ineffective early NPT, the effect would be to reduce the ability to find positive follow-up status associations with NPT treatment. Furthermore, the NPT definition does not include self-initiated NPT activities such as yoga53 that were not delivered as part of formal treatment and not recorded in medical records. Again, if reference group members engaged in these activities, it would have suppressed the ability to detect positive associations with NPT. Finally, the measure of pain was limited to a single score (0–10) rather than a multidimensional assessment inclusive of pain location and interference with personal functioning.54,55 Better assessment of pain interference using the Defense and Veterans Pain Rating54,55 could guide treatment choices as well as contribute to a more nuanced assessment of outcomes of pain management approaches.
These system-wide findings, combined with findings from other clinical trials of certain NPT modalities, lead us to suggest some implications to healthcare systems of increased access to NPT early in treatment. A study of early physical therapy found significant reduction in healthcare utilization,56 a randomized control trial found that brief psychosocial education about LBP among soldiers with no history of LBP was effective in reducing future LBP-related healthcare costs,57 and a nationally representative sample of individuals with neck and back problems found that uses of chiropractic and other integrative treatment services had lower spine-related annual medical costs.58 This study and these prior findings combined should encourage further exploration and research of possible favorable outcomes to systems that expand availability and utilization of NPT early in treatment.
The military continues to investigate strategies to reorganize aspects of pain management care and in many ways is at the frontier in its approach.21,59–62 To promote early use of integrative health services, the MHS expanded availability of chiropractic services, acupuncture, and interdisciplinary centers with close linkage to primary care.39 The study findings suggest that this model should be evaluated by other medical systems. Early NPT use, rather than delayed, may require further research into clinicians' attitudes, given they have been more resistant to NPT than their patients.38 No doubt that there will be challenges ahead to effective implementation of early NPT and integrative care modalities into health systems, including the military environment.63,64 It may be advisable to reconsider payment or benefit restrictions that limit access to modalities such as short-term acupuncture and chiropractic care, as mechanisms to enhance availability of effective NPT modalities.
In conclusion, provisions of NPT services in the first 30 days to opioid-naive soldiers presenting with low-back pain was associated with small, but significant long-term improvements in military readiness in this large observational study. These findings support the adoption of early NPT services to soldiers with low-back pain that is likely to become chronic.
Appendix Table A1.
Outcome Measured at Follow-Up by Early Treatment Group (n = 30,612)
| LBP early treatment groupb | ||||||
|---|---|---|---|---|---|---|
| Reference group | NPT only | Opioid only | Opioid and NPT | Tramadol only | Tramadol and NPT | |
| Follow-up outcomea | Percent of patients with outcome | |||||
| Duty Limitation | 37.5 | 33.4 | 43.1 | 42.4 | 43.2 | 45.1 |
| Pain-related inpatient stay | 4.7 | 3.2 | 7.2 | 6.8 | 5.6 | 4.9 |
| ED visit for LBP | 5.4 | 4.6 | 11.6 | 9.6 | 6.3 | 6.8 |
| Moderate or Severe pain | 51.9 | 53.4 | 58.9 | 62.6 | 59.7 | 62.5 |
| Opioid or tramadol use | 31.6 | 28.7 | 51.5 | 47.5 | 51.5 | 48.5 |
Chi-square statistic of each early treatment modality with each outcome was significant at p ≤ 0.001.
Follow-up window was 91–365 days after index LBP encounter.
All treatment indicators measured during first 30 days of LBP episode. For each treatment, the reference group is soldiers without NPT or opioids or tramadol.
ED, emergency department; LBP, low-back pain; NPT, non-pharmaceutical treatments included in the study.
Acknowledgments
The authors acknowledge Dr. Richard Gromadzki of Axiom Resource Management, Inc., for compiling the data files used in these analyses, as well as Dr. Thomas V. Williams, the Defense Health Agency's (DHA) Department of Defense (DoD) data sponsor. The DHA's Privacy and Civil Liberties Office provided access to DoD data. The opinions and assertions herein are those of the authors and do not necessarily reflect the official views of the DoD, NIDA, or the National Institutes of Health. Research completed with grant funding from the National Center on Complementary and Integrative Health (#R01 AT008404).
Authors' Contribution
Dr. Larson has full access to all data in the study and takes responsibility for the integrity and accuracy of the data analysis.
Study concept and design: Larson, Adams, Ritter, Bauer, and Williams.
Acquisition, analysis, and interpretation of data: Williams, Larson, Adams, Ritter, and Linton.
Drafting the article: Larson, Adams, Bauer, Ritter, Linton, and Saadoun.
Critical revision of the article for important intellectual content: Williams, Ritter, and Saadoun.
Study supervision and management: Larson and Adams.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Pai S, Sundaram LJ. Low back pain: An economic assessment in the United States. Orthop Clin North Am 2004;35:1–5 [DOI] [PubMed] [Google Scholar]
- 2.Eilat-Tsanani S, Tabenkin H, Lavie I, et al. The effect of low back pain on work absenteeism among soldiers on active service. Spine 2010;35:E995–E999 [DOI] [PubMed] [Google Scholar]
- 3.Jonas WB, Schoomaker EB. Pain and opioids in the military: We must do better. JAMA Intern Med 2014;174:1402–1403 [DOI] [PubMed] [Google Scholar]
- 4.Knox J, Orchowski J, Scher DL, et al. The incidence of low back pain in active duty United States military service members. Spine 2011;36:1492–1500 [DOI] [PubMed] [Google Scholar]
- 5.Clark ME, Bair MJ, Buckenmaier CC 3rd, et al. Pain and combat injuries in soldiers returning from Operations Enduring Freedom and Iraqi Freedom: Implications for research and practice. J Rehabil Res Dev 2007;44:179–194 [DOI] [PubMed] [Google Scholar]
- 6.Cohen SP, Nguyen C, Kapoor SG, et al. Back pain during war: An analysis of factors affecting outcome. Arch Intern Med 2009;169:1916–1923 [DOI] [PubMed] [Google Scholar]
- 7.Dowell D, Haegerich TM, Chou R. CDC Guideline for Prescribing Opioids for Chronic Pain-United States, 2016. JAMA 2016:E1–E22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vowles KE, McEntee ML, Julnes PS, et al. Rates of opioid misuse, abuse, and addiction in chronic pain: A systematic review and data synthesis. PAIN 2015;156:569–576 [DOI] [PubMed] [Google Scholar]
- 9.Department of Veterans Affairs - Department of Defense. VA/DoD Clinical Practice Guideline for the Management of Opioid Therapy for Chronic Pain - Clinician Summary. 2017. Online document at: www.healthquality.va.gov/guidelines/Pain/cot/, accessed April14, 2017
- 10.Kissin I. Long-term opioid treatment of chronic nonmalignant pain: Unproven efficacy and neglected safety? J Pain Res 2013;6:513–529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chou R, Turner JA, Devine EB, et al. The effectiveness and risks of long-term opioid therapy for chronic pain: A systematic review for a National Institutes of Health Pathways to Prevention Workshop. Ann Intern Med 2015;162:276–286 [DOI] [PubMed] [Google Scholar]
- 12.Darnall BD, Stacey BR, Chou R. Medical and psychological risks and consequences of long-term opioid therapy in women. Pain Med 2012;13:1181–1211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Martell BA, O'Connor PG, Kerns RD, et al. Systematic review: Opioid treatment for chronic back pain: Prevalence, efficacy, and association with addiction. Ann Intern Med 2007;146:116–127 [DOI] [PubMed] [Google Scholar]
- 14.Noble M, Treadwell JR, Tregear SJ, et al. Long-term opioid management for chronic noncancer pain. Cochrane Database Syst Rev 2010;1:CD006605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nelson LS, Juurlink DN, Perrone J. Addressing the Opioid Epidemic. JAMA 2015;314:1453–1454 [DOI] [PubMed] [Google Scholar]
- 16.Jeffery DD, May L, Luckey B, et al. Use and abuse of prescribed opioids, central nervous system depressants, and stimulants among U.S. active duty military personnel in FY 2010. Mil Med 2014;179:1141–1148 [DOI] [PubMed] [Google Scholar]
- 17.Department of Veterans Affairs - Department of Defense. VA/DoD Clinical Practice Guideline for the Management of Opioid Therapy for Chronic Pain - Qualifying Statements. 2017. Online document at: www.healthquality.va.gov/guidelines/Pain/cot/, accessed April14, 2017
- 18.Office of The Army Surgeon General. Pain Management Task Force: Providing a Standardized DoD and VHA Vision and Approach to Pain Management to Optimize the Care for Warriors and their Families. Final Report. 2010. Online document at: www.dvcipm.org/files/reports/pain-task-force-final-report-may-2010.pdf, accessed July14, 2017
- 19.Abbasi J. As Opioid Epidemic Rages, Complementary Health Approaches to Pain Gain Traction. JAMA 2016;316. [DOI] [PubMed] [Google Scholar]
- 20.Interagency Pain Research Coordinating Committee. National Pain Strategy: A Comprehensive Population Health-Level Strategy for Pain. 2015. Online document at: https://iprcc.nih.gov/docs/DraftHHSNationalPainStrategy.pdf, accessed April5, 2017
- 21.Buckenmaier CC, 3rd, Griffith S. Military pain management in 21st century war. Mil Med 2010;175(7 Suppl):7–12 [DOI] [PubMed] [Google Scholar]
- 22.Chou R, Atlas SJ, Stanos SP, Rosenquist RW. Nonsurgical interventional therapies for low back pain: A review of the evidence for an American Pain Society clinical practice guideline. Spine (Phila Pa 1976) 2009;34:1078–1093 [DOI] [PubMed] [Google Scholar]
- 23.Chou R, Huffman LH, American Pain S, American College of P. Nonpharmacologic therapies for acute and chronic low back pain: A review of the evidence for an American Pain Society/American College of Physicians clinical practice guideline. Ann Intern Med 2007;147:493–505 [DOI] [PubMed] [Google Scholar]
- 24.Chou R, Deyo R, Friedly J, et al. Nonpharmacologic therapies for low back pain: A systematic review for an American College of Physicians Clinical Practice Guideline. Ann Intern Med 2017;166:493–505 [DOI] [PubMed] [Google Scholar]
- 25.Fritz JM, Magel JS, McFadden M, et al. Early Physical Therapy vs Usual Care in Patients With Recent-Onset Low Back Pain: A Randomized Clinical Trial. JAMA 2015;314:1459–1467 [DOI] [PubMed] [Google Scholar]
- 26.Hagen EM, Odelien KH, Lie SA, Eriksen HR. Adding a physical exercise programme to brief intervention for low back pain patients did not increase return to work. Scand J Public Health 2010;38:731–738 [DOI] [PubMed] [Google Scholar]
- 27.Cicero TJ, Wong G, Tian Y, et al. Co-morbidity and utilization of medical services by pain patients receiving opioid medications: Data from an insurance claims database. PAIN 2009;144:20–27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cohen MM, Smit V, Andrianopoulos N, et al. Acupuncture for analgesia in the emergency department: A multicentre, randomised, equivalence and non-inferiority trial. Med J Aust 2017;206:494–499 [DOI] [PubMed] [Google Scholar]
- 29.Niemtzow RC, Burns SM, Cooper J, et al. Acupuncture clinical pain trail in a military medical center: Outcomes. Med Acupunct 2008;20:255–261 [Google Scholar]
- 30.Department of Veterans Affairs - Office of Inspector General. Healthcare Inspection - VA Patterns of Dispensing Take-Home Opioids and Monitoring Patients on Opioid Therapy. 2014. Online document at: www.va.gov/oig/pubs/VAOIG-14-00895-163.pdf, accessed July14, 2017
- 31.Seal KH, Shi Y, Cohen G, et al. Association of mental health disorders with prescription opioids and high-risk opioid use in US veterans of Iraq and Afghanistan. JAMA 2012;307:940–947 [DOI] [PubMed] [Google Scholar]
- 32.de Vet HC, Heymans MW, Dunn KM, et al. Episodes of low back pain: A proposal for uniform definitions to be used in research. Spine (Phila Pa 1976) 2002;27:2409–2416 [DOI] [PubMed] [Google Scholar]
- 33.Goulet JL, Brandt C, Crystal S, et al. Agreement between electronic medical record-based and self-administered pain numeric rating scale: Clinical and research implications. Med Care 2013;51:245–250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dobscha SK, Morasco BJ, Duckart JP, et al. Correlates of prescription opioid initiation and long-term opioid use in veterans with persistent pain. Clin J Pain 2013;29:102–108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.National Center for Injury Prevention and Control CfDCaP. CDC Compilation of Opioid Analgesic Formulations with Morphine Milligram Equivalent Conversion Factors, 2015 Version. Atlanta, GA, 2015 [Google Scholar]
- 36.Frieden TR, Houry D. Reducing the risks of relief—The CDC opioid-prescribing guideline. N Engl J Med 2016;374:1501–1504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Patrick N, Emanski E, Knaub MA. Acute and chronic low back pain. Med Clin North Am 2016;100:169–181 [DOI] [PubMed] [Google Scholar]
- 38.Deyo RA. The role of spinal manipulation in the treatment of low back pain. JAMA 2017;317:1418–1419 [DOI] [PubMed] [Google Scholar]
- 39.Jaditz T, Schaefer E, Hill C. Evaluation of Chiropractic Services - Impact on MHS. Alexandria, VA: The CNA Corporation;2008. CRM D0017761.A2/Final [Google Scholar]
- 40.Herman PM, Sorbero ME, Sims-Columbia AC. Complementary and Alternative Medicine in the Miltiary Health System. Santa Monica, CA: RAND Corporation, 2017 [DOI] [PubMed] [Google Scholar]
- 41.Jonas WB, Welton RC, Delgado RE, et al. CAM in the United States military: Too little of a good thing? Med Care 2014;52(12 Suppl 5):S9–12 [DOI] [PubMed] [Google Scholar]
- 42.Gatchel RJ, McGeary DD, McGeary CA, Lippe B. Interdisciplinary chronic pain management: Past, present, and future. Am Psychol 2014;69:119–130 [DOI] [PubMed] [Google Scholar]
- 43.Cheatle MD. Biopsychosocial approach to assessing and managing patients with chronic pain. Med Clin North Am 2016;100:43–53 [DOI] [PubMed] [Google Scholar]
- 44.Bair MJ, Ang D, Wu J, et al. Evaluation of stepped care for chronic pain (ESCAPE) in veterans of the Iraq and Afghanistan conflicts: A randomized clinical trial. JAMA Intern Med 2015;175:682–689 [DOI] [PubMed] [Google Scholar]
- 45.Linton SJ, Nordin E. A 5-year follow-up evaluation of the health and economic consequences of an early cognitive behavioral intervention for back pain: A randomized, controlled trial. Spine (Phila Pa 1976) 2006;31:853–858 [DOI] [PubMed] [Google Scholar]
- 46.Morone NE, Greco CM, Moore CG, et al. A Mind-Body Program for Older Adults With Chronic Low Back Pain: A Randomized Clinical Trial. JAMA Intern Med 2016;176:329–337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lamb SE, Hansen Z, Lall R, et al. Group cognitive behavioural treatment for low-back pain in primary care: A randomised controlled trial and cost-effectiveness analysis. Lancet 2010;375:916–923 [DOI] [PubMed] [Google Scholar]
- 48.Sun EC, Darnall B, Baker LC, Mackey S. Incidence of and risk factors for chronic opioid use among opioid-naive patients in the postoperative period. JAMA Intern Med 2016;176:1286–1293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bair MJ, Robinson RL, Katon W, Kroenke K. Depression and pain comorbidity: A literature review. Arch Intern Med 2003;163:2433–2445 [DOI] [PubMed] [Google Scholar]
- 50.Macey TA, Morasco BJ, Duckart JP, Dobscha SK. Patterns and correlates of prescription opioid use in OEF/OIF veterans with chronic noncancer pain. Pain Med 2011;12:1502–1509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ciesielski T, Iyengar R, Bothra A, et al. A tool to assess risk of de novo opioid abuse or dependence. Am J Med 2016;129:699–705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Alford DP. Chronic back pain with possible prescription opioid misuse. JAMA 2013;309:919–925 [DOI] [PubMed] [Google Scholar]
- 53.Groessl EJ, Weingart KR, Aschbacher K, et al. Yoga for veterans with chronic low-back pain. J Altern Complement Med 2008;14:1123–1129 [DOI] [PubMed] [Google Scholar]
- 54.Cook KF, Buckenmaier C, 3rd, Gershon RC. PASTOR/PROMIS (R) pain outcomes system: What does it mean to pain specialists? Pain Manag 2014;4:277–283 [DOI] [PubMed] [Google Scholar]
- 55.Buckenmaier CC, 3rd, Galloway KT, Polomano RC, et al. Preliminary validation of the Defense and Veterans Pain Rating Scale (DVPRS) in a military population. Pain Med 2013;14:110–123 [DOI] [PubMed] [Google Scholar]
- 56.Childs JD, Fritz JM, Wu SS, et al. Implications of early and guideline adherent physical therapy for low back pain on utilization and costs. BMC Health Serv Res 2015;15:150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Childs JD, Wu SS, Teyhen DS, et al. Prevention of low back pain in the military cluster randomized trial: Effects of brief psychosocial education on total and low back pain-related health care costs. Spine J 2014;14:571–583 [DOI] [PubMed] [Google Scholar]
- 58.Martin BI, Gerkovich MM, Deyo RA, et al. The association of complementary and alternative medicine use and health care expenditures for back and neck problems. Med Care 2012;50:1029–1036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Buckenmaier CC, 3rd, Gallagher RM, et al. War on Pain—New Strategies in Pain Management for Military Personnel and Veterans. A Supplement to Federal Practitioner; 2011;28:1–16 [Google Scholar]
- 60.Crawford C, Lee C, Buckenmaier C, 3rd, et al. The current state of the science for active self-care complementary and integrative medicine therapies in the management of chronic pain symptoms: Lessons learned, directions for the future. Pain Med 2014;15 Suppl 1:S104–S113 [DOI] [PubMed] [Google Scholar]
- 61.Delgado R, York A, Lee C, et al. Assessing the quality, efficacy, and effectiveness of the current evidence base of active self-care complementary and integrative medicine therapies for the management of chronic pain: A rapid evidence assessment of the literature. Pain Med 2014;15 Suppl 1:S9–20 [DOI] [PubMed] [Google Scholar]
- 62.Kent ML, Buckenmaier CC. Battlefield regional anesthesia: Evolution and future concepts. Tech Reg Anesth Pain Manage 2012;16:184–189 [Google Scholar]
- 63.Coulter ID, Hilton L, Walter J, Brown KS. Integrative pain management centers in the military: The challenges. Mil Med 2016;181:1033–1039 [DOI] [PubMed] [Google Scholar]
- 64.Eisenberg DM, Buring JE, Hrbek AL, et al. A model of integrative care for low-back pain. J Altern Complement Med 2012;18:354–362 [DOI] [PMC free article] [PubMed] [Google Scholar]