Abstract
Background
To determine the validity of the lactate threshold (LT) and maximal oxygen uptake () determined during graded exercise test (GXT) of different durations and using different LT calculations. Trained male cyclists (n = 17) completed five GXTs of varying stage length (1, 3, 4, 7 and 10 min) to establish the LT, and a series of 30-min constant power bouts to establish the maximal lactate steady state (MLSS). was assessed during each GXT and a subsequent verification exhaustive bout (VEB), and 14 different LTs were calculated from four of the GXTs (3, 4, 7 and 10 min)—yielding a total 56 LTs. Agreement was assessed between the highest measured during each GXT () as well as between each LT and MLSS. and LT data were analysed using mean difference (MD) and intraclass correlation (ICC).
Results
The value from GXT1 was 61.0 ± 5.3 mL.kg-1.min-1 and the peak power 420 ± 55 W (mean ± SD). The power at the MLSS was 264 ± 39 W. from GXT3, 4, 7, 10 underestimated by ~1–5 mL.kg-1.min-1. Many of the traditional LT methods were not valid and a newly developed Modified Dmax method derived from GXT4 provided the most valid estimate of the MLSS (MD = 1.1 W; ICC = 0.96).
Conclusion
The data highlight how GXT protocol design and data analysis influence the determination of both and LT. It is also apparent that and LT cannot be determined in a single GXT, even with the inclusion of a VEB.
Introduction
Sampling of expired gas and blood data during a graded exercise test (GXT) to exhaustion permits identification of the gas exchange threshold (GET), the respiratory compensation point (RCP), the lactate threshold (LT), and maximal oxygen uptake (). These indices can distinguish cardiorespiratory fitness, and demarcate the domains of exercise [1, 2] that can be used to prescribe exercise and to optimize training stimuli [3–6]. However, despite the popularity of these indices, the methods used to determine them can differ substantially and there has been little systematic investigation of their validity [7–9].
The recommended duration of a GXT to assess is 8 to 12 minutes [10–13]. However, there is little consensus on an appropriate GXT protocol design, including duration, stage length, or number of stages, needed to establish the LT. A stage length of at least 3 minutes has been recommended [13], although an 8-minute stage length has also been suggested for blood lactate concentrations to stabilize [14]. The number of stages and GXT duration will depend on the starting intensity and power increments. Power is typically increased identically [15], regardless of sex or fitness, leading to a heterogenous GXT duration and number of stages completed [16]. A customized approach to LT testing has been recommended to ensure a more homogenous GXT duration [17].
More than 25 methods have been proposed to calculate the LT [18]; these include the power preceding a rise in blood lactate concentration of more than 0.5, 1.0 or 1.5 mmol.L-1 from baseline [19], the onset of a fixed blood lactate accumulation (OBLA) ranging from 2.0 to 4.0 mmol.L-1 [20, 21], or the use of curve fitting procedures such as the Dmax or modified Dmax methods (ModDmax) [22, 23]. However, many of these ‘accepted’ methods are influenced by GXT protocol design [8, 24] and their underlying validity has not been reported.
Assessing the validity of a measurement requires comparison with a criterion measure. The maximal lactate steady state (MLSS) represents the highest intensity where blood lactate appearance and disappearance is in equilibrium and where energy demand is adequately met by oxidative phosphorylation [25]. Exercise performed above the MLSS results in accelerated blood lactate appearance and it has therefore been suggested as an appropriate criterion measure for the LT [25, 26]. The primary advantages of the MLSS test include its independence of participant effort, it’s submaximal and is reliable [27]. However, the disadvantage is the necessity of multiple laboratory visits and that it yields only one index of performance.
is considered the “gold standard” for assessing cardiorespiratory fitness [28] and the highest recorded from a GXT is often accepted as the [10]. Establishing the LT requires a GXT that typically exceeds 20 minutes [13]; however, in these instances the highest may underestimate the [12] and is termed . Recently, the use of a verification exhaustive bout (VEB) has been recommended to confirm the . However, it is unknown if a VEB performed after a longer duration GXT provides a valid estimate of .
The aim of this study was to determine the validity of the LT and derived from a single visit GXT. We hypothesized that our results would yield one or more GXT stage length and LT calculation method combination that provides a valid estimation of the criterion measure of the LT (i.e., MLSS). We also hypothesized the highest measured during longer duration GXTs would underestimate and that the highest value measured during each VEB would be similar to the measured during the 8- to 12-minute GXT.
Materials and methods
Ethical approval
All procedures were performed in accordance with the ethical standards of the institutional and/or national research committee, and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Participants/Experimental design
Seventeen trained male cyclists ( 62.1 ± 5.8 mL.kg-1.min-1, age 36.2 ± 7.4 years, body mass index (BMI): 24.1 ± 2.0 kg.m-2) volunteered for this study which required 7 to 10 visits to the laboratory. Informed consent was obtained from all individual participants included in the study.
Visit one included risk stratification using the American College of Sports Medicine Risk Stratification guidelines [29], written informed consent, self-reported physical activity rating (PA-R) [30], measurement of height and body mass, and completion of a cycling GXT with 1-minute stages (GXT1) followed by a VEB. The remaining visits consisted of four cycling GXTs with varying stage length (3-, 4-, 7- and 10-min stages) and a series of 30-min constant power bouts to establish the MLSS. The GXTs and constant power bouts were performed in an alternating order and the order of the GXTs was randomised. Prior to each GXT and the constant power bouts a 5-min warm up was administered at a self-selected power followed by 5 min of passive rest. Participants performed each test at their preferred cadence determined during the initial visit. Antecubital venous blood (1.0 mL) was sampled during all visits (excluding GXT1) at rest, and at the end of every stage during the GXTs or every 5 min during the constant power exercise bouts. All participants self-reported abstaining from the consumption of alcohol and caffeine or engaging in heavy exercise 24 h prior to each visit. Participants were given at least 48 h between visits and all tests were completed within 6 weeks. The Victoria University Human Research Ethics Committee approved all procedures (HRE 017–035).
Equipment/Instruments
All exercise testing was conducted using an electronically-braked cycle ergometer (Lode Excalibur v2.0, The Netherlands). A metabolic analyser (Quark Cardiopulmonary Exercise Testing, Cosmed, Italy) was used to assess oxygen uptake () on a breath-by-breath basis, and heart rate was measured throughout all tests. Antecubital venous blood was analysed using a blood lactate analyser (YSI 2300 STAT Plus, YSI, USA).
GXTs with verification exhaustive bout
Demographic data, PA-R, and measurements of height and body mass were used to estimate [31] and maximum power output [30, 32].
| Eq 1 |
| Eq 2 |
Where is expressed in millilitres per kilogram per minute, BMI is in kg.m-2, and is in Watts.
A custom GXT protocol with a desired time limit of 10 min was then designed for each particpant using: min = 1-min intensities (W.min-1). Additional customized protocols were designed for each of the remaining GXTs based on a percentage of the measured from GXT1. The predicted was 80%, 77%, 72% and 70% for GXT3, GXT4, GXT7, and GXT10, respectively. The target number of stages for each participant was nine; the initial stage and subsequent stages of the remaining GXTs were determined using the following equations:
| Eq 3 |
| Eq 4 |
where stage 1 power and predicted subsequent power increments are expressed in Watts.
A 5-min recovery was administered after each GXT, followed by a VEB performed at 90% of measured from GXT1 to measure the highest measured measure () [17].
Constant power exercise bouts to establish the maximal lactate steady state
The power associated with the respiratory compensation point (RCP) from GXT1 was used in a regression equation (Eq 5) to estimate the MLSS (RCPMLSS) and the first constant power exercise [33]. The RCP was determined as the average of the power output associated with: 1) the break point in ventilation relative to expired carbon dioxide (), 2) second break point in and 3) the fall in end-tidal carbon dioxide (PETCO2) after an apparent steady state [34–36].
| Eq 5 |
where the RCPMLSS and RCP are expressed in Watts
Participants performed 3 min of baseline cycling at 20 W prior to each constant power bout. The MLSS was established as the highest intensity where blood lactate increased <1.0 mmol.L-1 from the 10th to the 30th minute [26]. If the blood lactate concentration increased >1.0 mmol.L-1 the power was decreased by 3%, otherwise the power was increased by 3% [27]. This process continued until the MLSS was obtained.
LT and respiratory compensation point calculations
The LTs were calculated from GXT3,4,7 and 10 using 14 methods (4 GXTs * 14 LTs = 56 LTs in total), and the RCP and the RCPMLSS were also calculated from GXT1 (56 LTs + RCP and RCPMLSS = 58 total estimates) (Fig 1):
Fig 1. Representative blood lactate curve with 14 LTs calculated from GXT4 (participant #9).
The power of the MLSS was 302 W and the blood lactate concentration was 2.85 mmol.L-1. Log-log = power at the intersection of two linear lines with the lowest residual sum of squares; log = using the log-log method as the point of the initial data point when calculating the Dmax or Modified Dmax; poly = Modified Dmax method calculated using a third order polynomial regression equation; exp = Modified Dmax method calculated using a constant plus exponential regression equation; OBLA = onset of blood lactate accumulation; B + absolute value = the intensity where blood lactate increases above baseline.
Log-log: The lactate curve was divided into two segments and the intersection point of the two lines with the lowest residuals sum of squares was taken as the LT [37].
OBLA value of 2.0, 2.5, 3.0, 3.5, or 4.0 mmol.L-1 [1, 24, 38].
Baseline + absolute value(s) (B + mmol.L-1): The intensity at which blood lactate concentration increased 0.5, 1.0 or 1.5 mmol.L-1 above baseline value(s) [39, 40].
Dmax: The point on the third order polynomial regression curve that yielded the maximum perpendicular distance to the straight line formed by the two end points of the curve [23].
Modified Dmax (ModDmax): The intensity at the point on the third order polynomial regression curve that yielded the maximal perpendicular distance to the straight line formed by the point preceding the first rise in blood lactate concentration of >0.4 mmol.L-1 lactate and the final lactate point [22].
Exponential Dmax (Exp-Dmax): The point on the exponential plus-constant regression curve that yielded the maximum perpendicular distance to the straight line formed by the two end points of the curve [41, 42].
Log-log Modified Dmax (Log-Poly-ModDmax): The intensity at the point on the third order polynomial regression curve that yielded the maximal perpendicular distance to the straight line formed by the intensity associated with the log-log LT and the final lactate point.
Log-log Exponential Modified Dmax method (Log-Exp-ModDmax): The intensity at the point on the exponential plus-constant regression curve that yielded the maximal perpendicular distance to the straight line formed by the intensity associated with the log-log LT and the final lactate point.
RCP: refer to Constant Power Exercise Bouts to Establish the Maximal Lactate Steady State method section.
The estimated MLSS was based on a regression equation based on the RCP from GXT1 (RCPMLSS) (Eq 5).
Data analysis
Breath-by-breath data were edited individually with values greater than three standard deviations from the mean excluded [43]. The data was interpolated on a second-by-second basis and averaged into 5- and 30-s bins [44, 45]. The highest measured value from every GXT and VEB was determined as the highest 20-s rolling average. The was computed as the highest measured from any GXT or VEB. The for each GXT was defined as the highest measured from either the GXT or the subsequent VEB.
The for every GXT was determined as the power from the last completed stage plus the time completed in the subsequent stage multiplied by the slope (Eq 6). The response at the MLSS was determined by the average value during the last two minutes of the 30-minute constant power bout.
| Eq 6 |
Calculated LTs were excluded if the mean difference between the MLSS and calculated LT was greater than the error of the measurement of the MLSS [coefficient of the variation (CV%) = 3%, 7.9 W] [27], the effect size (ES) was greater than 0.2, or the Pearson Product moment correlation coefficient (r) was less than 0.90. Using these criteria, 10 of the 56 LTs and the RCPMLSS (Eq 5) were included in the analysis (Table 1).
Table 1. The mean ± standard deviation (SD) of the 14 lactate thresholds calculated from the 4 prolonged graded exercise tests (i.e., GXT3, GXT4, GXT7 and GXT10), and the respiratory compensation point (RCP) and the maximal lactate steady state (MLSS) estimated from the RCP (RCPMLSS) calculated from GXT1.
| GXT3 | GXT4 | GXT7 | GXT10 | ||
|---|---|---|---|---|---|
| Log-log LT | Mean SD (W) | 211 ± 43 | 202 ± 38 | 200 ± 40 | 196 ± 41 |
| MD (W) | 53.1 | 62.8 | 64.8 | 68.3 | |
| r | 0.84 | 0.89 | 0.87 | 0.78 | |
| ES | 1.28 | 1.63 | 1.62 | 1.70 | |
| OBLA 2.0 | Mean SD (W) | 262 ± 40 | 249 ± 39 | 247 ± 39 | 245 ± 37 |
| MD (W) | 2.1 | 15.1 | 17.3 | 19.6 | |
| r | 0.86 | 0.94 | 0.94 | 0.93 | |
| ES | -0.05 | -0.38 | -0.44 | -0.50 | |
| OBLA 2.5 | Mean SD (W) | 276 ± 42 | 262 ± 40 | 258 ± 40 | 255 ± 38 |
| MD (W) | -11.9 | 2.0 | 6.7 | 9.2 | |
| r | 0.89 | 0.95 | 0.94 | 0.93 | |
| ES | 0.30 | -0.05 | -0.17 | -0.23 | |
| OBLA 3.0 | Mean SD (W) | 288 ± 43 | 273 ± 41 | 267 ± 41 | 264 ± 39 |
| MD (W) | -23.2 | -8.8 | -2.2 | 0.4 | |
| r | 0.90 | 0.96 | 0.95 | 0.93 | |
| ES | 0.59 | 0.22 | 0.06 | -0.01 | |
| OBLA 3.5 | Mean SD (W) | 297 ± 45 | 282 ± 41 | 274 ± 41 | 272 ± 40 |
| MD (W) | -32.8 | -18.1 | -10.0 | -7.3 | |
| r | 0.91 | 0.96 | 0.95 | 0.93 | |
| ES | 0.83 | 0.46 | 0.25 | 0.19 | |
| OBLA 4.0 | Mean SD (W) | 306 ± 46 | 291 ± 42 | 281 ± 42 | 279 ± 41 |
| MD (W) | -41.3 | -26.3 | -16.8 | -14.2 | |
| r | 0.91 | 0.97 | 0.95 | 0.93 | |
| ES | 1.05 | 0.67 | 0.43 | 0.36 | |
| Baseline + 0.5 | Mean SD (W) | 235 ± 38 | 229 ± 40 | 228 ± 41 | 225 ± 37 |
| MD (W) | 29.4 | 35.6 | 36.6 | 39.5 | |
| r | 0.74 | 0.81 | 0.83 | 0.82 | |
| ES | -0.75 | -0.90 | -0.93 | -1.00 | |
| Baseline + 1.0 | Mean SD (W) | 255 ± 39 | 239 ± 40 | 236 ± 39 | 235 ± 39 |
| MD (W) | 9.5 | 25.3 | 27.9 | 29.1 | |
| r | 0.88 | 0.92 | 0.93 | 0.91 | |
| ES | -0.24 | -0.64 | -0.71 | -0.74 | |
| Baseline + 1.5 | Mean SD (W) | 270 ± 41 | 254 ± 41 | 250 ± 39 | 248 ± 39 |
| MD (W) | -6.0 | 10.1 | 14.7 | 16.8 | |
| r | 0.90 | 0.94 | 0.94 | 0.92 | |
| ES | 0.15 | -0.26 | -0.37 | -0.43 | |
| Dmax | Mean SD (W) | 246 ± 34 | 232 ± 36 | 223 ± 31 | 216 ± 33 |
| MD (W) | 18.6 | 31.9 | 41.6 | 48.8 | |
| r | 0.94 | 0.97 | 0.96 | 0.95 | |
| ES | -0.47 | -0.81 | -1.06 | -1.24 | |
| Modified Dmax | Mean SD (W) | 278 ± 37 | 267 ± 39 | 255 ± 40 | 248 ± 37 |
| MD (W) | -13.2 | -2.9 | 9.7 | 15.9 | |
| r | 0.90 | 0.91 | 0.93 | 0.92 | |
| ES | 0.33 | 0.07 | -0.25 | -0.40 | |
| Log-Poly-MDmax | Mean SD (W) | 280 ± 42 | 265 ± 42 | 255 ± 39 | 248 ± 40 |
| MD (W) | -15.5 | -1.1 | 9.5 | 16.5 | |
| r | 0.94 | 0.96 | 0.96 | 0.92 | |
| ES | 0.39 | 0.03 | -0.24 | -0.42 | |
| Exp-Dmax | Mean SD (W) | 256 ± 35 | 243 ± 36 | 234 ± 34 | 228 ± 35 |
| MD (W) | 8.0 | 21.8 | 30.8 | 36.8 | |
| r | 0.92 | 0.97 | 0.96 | 0.94 | |
| ES | -0.20 | -0.55 | -0.78 | -0.93 | |
| Log-Exp-MDmax | Mean SD (W) | 286 ± 42 | 271 ± 42 | 260 ± 39 | 253 ± 40 |
| MD (W) | -21.7 | -7.0 | 4.3 | 11.1 | |
| r | 0.94 | 0.97 | 0.96 | 0.93 | |
| ES | 0.55 | 0.18 | -0.11 | -0.28 | |
| GXT1 | |||||
| RCPMLSS | Mean SD (W) | 271 ± 39 | |||
| MD (W) | -6.71 | ||||
| r | 0.92 | ||||
| ES | -0.17 | ||||
| RCP | Mean SD (W) | 315 ± 40 | |||
| MD (W) | -50.4 | ||||
| r | 0.91 | ||||
| ES | 1.27 |
Also shown is the mean difference (MD), the Pearson product moment correlation (r) and effect size (ES) of the difference when compared with the MLSS. (log = using the log-log method as the point of the initial data point when calculating the Dmax or Modified Dmax; poly = Modified Dmax method calculated using a third order polynomial regression equation; exp = Modified Dmax method calculated using a constant plus exponential regression equation; OBLA = onset of blood lactate accumulation, B + = baseline lactate value plus an absolute lactate value). Bold represents the LT that met the three criteria for inclusion in our final analysis: mean difference less than 7.9 Watts, Pearson moment product correlation >0.90, and a less than trivial ES difference from the MLSS (ES <0.2)
Statistical analysis
A one-way analysis of variance with repeated measures was used to assess significant differences between the MLSS and the calculated LTs. Agreement between the MLSS and the calculated LTs was evaluated using a two-way mixed intraclass correlation coefficient (ICC), standard error of the measurement (SEM), Lin’s concordance correlation coefficient (pc) [46], Bland-Altman plots [47], (r), CV% [48, 49] and a magnitude-based inference approach involving standardised differences (ED) [50, 51]. Differences between values measured during each GXT were assessed using ES, p-values, and the CV%. Agreement between measured during each GXT and subsequent VEB was evaluated using intraclass calculation coefficient (ICC), SEM, and CV% [49]. Descriptive statistics are reported as the mean ± SD. Alpha was set to P ≤ 0.05.
Results
MLSS
The power associated with the MLSS was 264 ± 39 W, and the blood lactate concentrations at the 10th and 30th min were 2.8 ± 0.8 and 3.3 ± 0.8 mmol.L-1, respectively. The blood lactate values at 3% above the MLSS (272 ± 41 W) at the 10th and 30th min were 3.6 ± 0.8 and 5.0 ± 0.9 mmol.L-1, respectively. The at the MLSS was 81.4 ± 4.7% of (3892 ± 441 mL.min-1; 50.5 ± 4.0 mL.kg-1.min-1). For each GXT the at the MLSS and the power at the MLSS are shown in Table 2.
Table 2. Mean, standard deviation, and range of the and power associated with the maximal lactate steady state (MLSS) expressed as a percentage of the maximal power () and measured during each GXT.
Note: The at the MLSS was 81.4 ± 4.7% of the . (Defined as the highest measured during any GXT).
| GXT1 | GXT3 | GXT4 | GXT7 | GXT10 | |
|---|---|---|---|---|---|
|
at MLSS (% of ) |
83.0 ± 4.5 [75.5–90.7] |
84.7 ± 4.7 [76.6–91.9] |
86.1 ± 5.9 [73.9–94.2] |
88.4 ± 6.0 [77.4–103.2] |
90.2 ± 5.3 [78.7–99.9] |
|
Power at MLSS (% of ) |
62.9 ± 3.9 [56.8–71.7] |
78.4 ± 4.3 [69.8–84.4] |
82.4 ± 3.6 [73.7–88.8] |
87.3 ± 4.4 [79.8–96.0] |
89.6 ± 4.7 [81.6–98.1] |
Validity of LT estimates
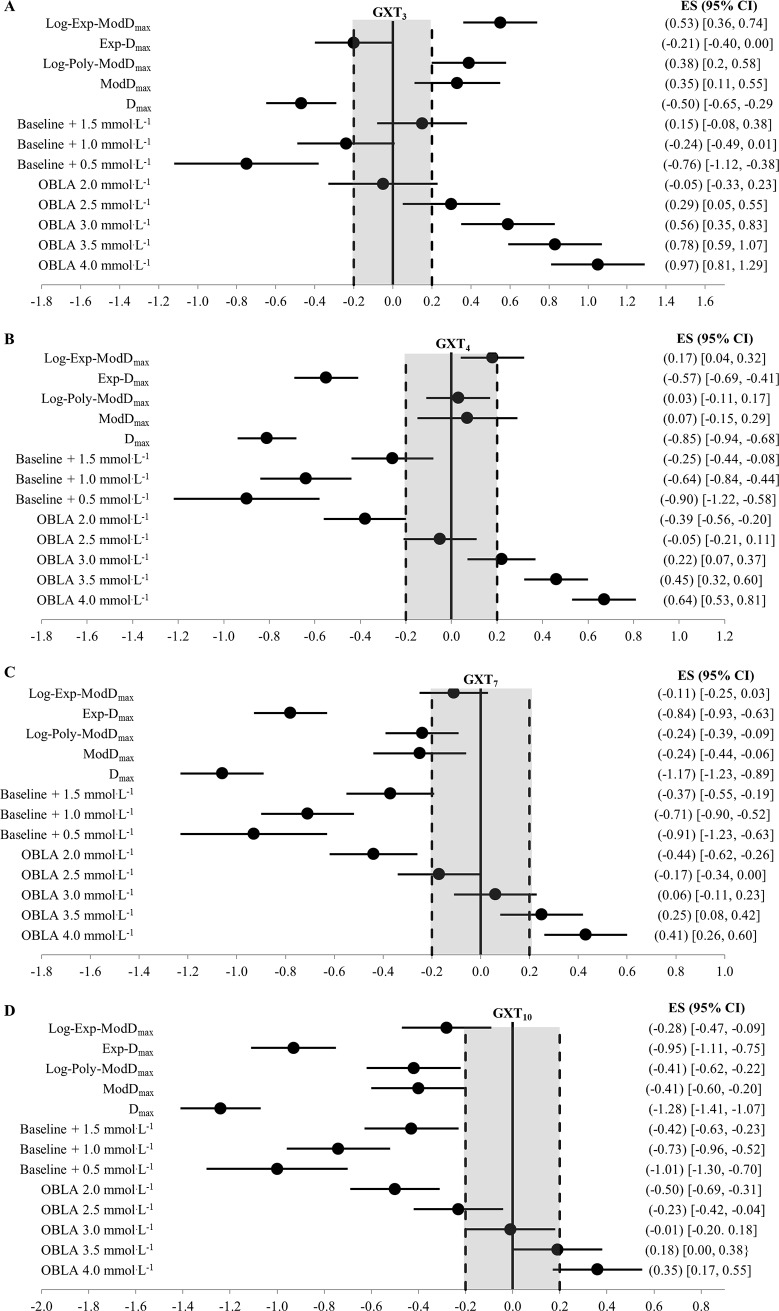
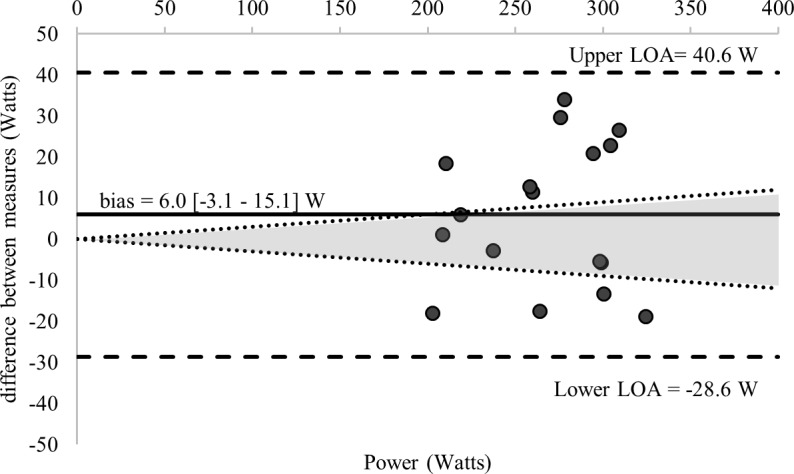
Comparisons of the 58 estimations of the MLSS and the calculated MLSS are detailed in Table 1. Fig 2 displays the standardized difference of the 13 LTs calculated for each GXT (52 in total) and the MLSS (all log-log methods were excluded given an ES > 1.0). Ten of the calculated LTs and the RCPMLSS met our inclusion criteria for final analysis—detailed comparisons with the MLSS are provided in Table 3 and Fig 3. Figs 3–7 shows Bland-Altman plots of the 11 estimations included in our analysis; the newly developed ModDmax LT calculations (Fig 5 Panel C and D; Fig 6 Panel C) had the lowest limits of agreement with the MLSS. The log-log polynomial modified Dmax (Log-Poly-ModDmax) method derived from GXT4 provided the best estimation of the MLSS (Fig 5 Panel C). There was an inverse relationship between the power calculated for each of the 14 LTs and stage length (Tables 1 and 4).
Fig 2.
(A-D) Forrest Plots of the difference (ES ± 95% CI) between the MLSS and the power calculated from the 13 lactate thresholds derived from (A) GXT3, (B) GXT4, (C) GXT7 and (D) GXT10 (52 in total and excluding log-log). The solid vertical bar represents no difference from the MLSS and the dashed vertical bars represents the threshold between a trivial and small difference (ES = 0.2) established by Cohen (50) and Hopkins (49). log = using the log-log method as the initial data point when calculating the Dmax or Modified Dmax; poly = Modified Dmax method calculated using a third order polynomial regression equation; exp = Modified Dmax method calculated using a constant plus exponential regression equation; OBLA = onset of blood lactate accumulation.
Table 3. Mean ± standard deviation, mean difference (MD), intraclass correlation coefficient (ICC), Lin’s concordance correlation coefficient (ρc), standard error of the measurement (SEM), effect size (ES) with 95% confidence limits, and coefficient of the variation (%CV) between the maximal lactate steady state (MLSS) and the eleven thresholds included in our analysis.
(RCPMLSS = MLSS estimate based on the respiratory compensation point; log = Modified Dmax method using the log-log method as the point of the initial lactate point; poly = Modified Dmax method calculated using a third order polynomial regression equation; exp = Modified Dmax method calculated using a constant plus exponential regression equation; OBLA = onset of blood lactate accumulation).
| Mean ± SD (W) |
MD (W) |
ICC [95% CI] | ρc | SEM [95% CI] (W) |
ES [95% CI] | CV [95% CI] (%) | ||
|---|---|---|---|---|---|---|---|---|
| MLSS | 264 ± 39 | |||||||
| GXT1 | RCPMLSS | 271 ± 39 | 6.7 | 0.92 [0.78–0.97] | 0.90 | 11.2 [8.3–17.0] | 0.17 [-0.04–0.38] | 6.0 [4.4–9.4] |
| GXT3 | Baseline + 1.5 mmol.L-1 | 270 ± 41 | 6.0 | 0.90 [0.75–0.97] | 0.90 | 12.5 [9.3–19.0] | 0.15 [-0.08–0.38] | 6.6 [4.9–10.4] |
| GXT4 | OBLA 2.5 mmol.L-1 | 262 ± 40 | -2.0 | 0.95 [0.87–0.98] | 0.95 | 8.7 [6.5–13.2] | -0.05 [-0.21–0.11] | 5.3 [3.9–8.4] |
| Modified Dmax | 267 ± 39 | 2.9 | 0.91 [0.76–0.98] | 0.90 | 11.7 [8.7–17.9] | 0.07 [-0.15–0.29] | 7.0 [5.1–11.0] | |
| Log-Poly-MDmax | 265 ± 42 | 1.1 | 0.96 [0.90–0.99] | 0.96 | 7.9 [5.8–12.0] | 0.03 [-0.11–0.17] | 4.4 [3.2–6.9] | |
| Log-Exp-MDmax | 271 ± 42 | 7.0 | 0.97 [0.91–0.99] | 0.95 | 7.5 [5.6–11.4] | 0.18 [0.04–0.32] | 4.1 [3.0–6.3] | |
| GXT7 | OBLA 2.5 mmol.L-1 | 258 ± 41 | -6.7 | 0.94 [0.85–0.98] | 0.93 | 9.4 [7.0–14.3] | -0.17 [-0.34–0.00] | 4.9 [3.6–7.7] |
| OBLA 3.0 mmol.L-1 | 267 ± 41 | 2.2 | 0.95 [0.86–0.98[ | 0.95 | 9.2 [6.9–14.1] | 0.06 [-0.11–0.23] | 5.1 [3.7–8.0] | |
| Log-Exp-MDmax | 260 ± 39 | -4.3 | 0.96 [0.89–0.99] | 0.95 | 7.8 [5.8–11.9] | -0.11 [-0.25–0.03] | 4.1 [3.0–6.4] | |
| GXT10 | OBLA 3.0 mmol.L-1 | 264 ± 39 | -0.4 | 0.93 [0.82–0.98] | 0.93 | 10.2 [7.6–15.5] | -0.01 [-0.20–0.18] | 5.5 [4.0–8.6] |
| OBLA 3.5 mmol.L-1 (n = 16) | 275 ± 39 | 6.9 | 0.93 [0.82–0.98] | 0.91 | 10.3 [7.7–15.7] | 0.19 [0.00–0.38] | 5.5 [4.0–8.7] |
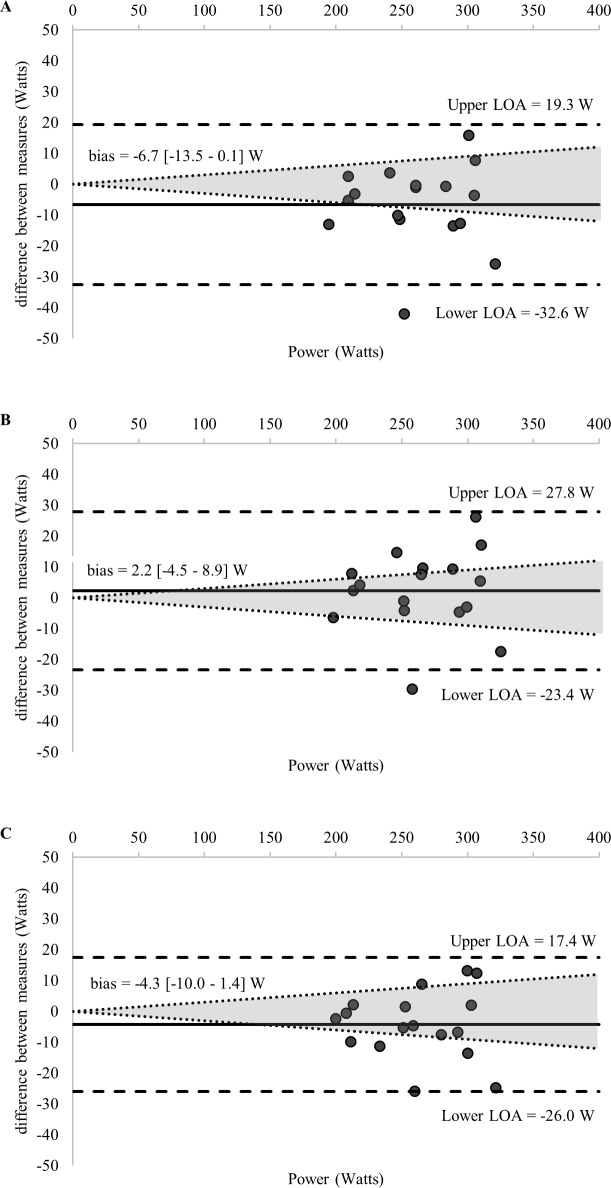
Fig 3. Bland-Altman plots displaying agreement between measures of the power associated with the RCP regression equation (RCPMLSS) calculated from GXT1 and the MLSS.

The differences between measures (y-axis) are plotted as a function of the mean of the two measures (x-axis) in power (Watts). The horizontal solid line represents the mean difference between the two measures (i.e., bias). The two horizontal dashed lines represent the limits of agreement (1.96 x standard deviation of the mean difference between the estimated lactate threshold via the RCPMLSS and the maximal lactate steady state). The dotted diagonal lines represent the boundaries of the 95% CI for MLSS reliability (CV = 3.0%; 95%; CI = 3.8%) calculated from Hauser et al., 2014) (RCP = respiratory compensation point).
Fig 7.
(A-B) Bland-Altman plots displaying agreement between measures of the power associated with the (A) OBLA 3.0 mmol.L-1, (B) OBLA 3.5 mmol.L-1 calculated from GXT10 and the MLSS. The differences between measures (y-axis) are plotted as a function of the mean of the two measures (x-axis) in power (Watts). The horizontal solid line represents the mean difference between the two measures (i.e., bias). The two horizontal dashed lines represent the limits of agreement (1.96 x standard deviation of the mean difference between the lactate threshold and the maximal lactate steady state). The dotted diagonal lines represent the boundaries of the 95% CI for MLSS reliability (CV = 3.0%; 95%; CI = 3.8%) calculated from Hauser et al., 2014) (OBLA = onset of blood lactate accumulation.).
Fig 5.
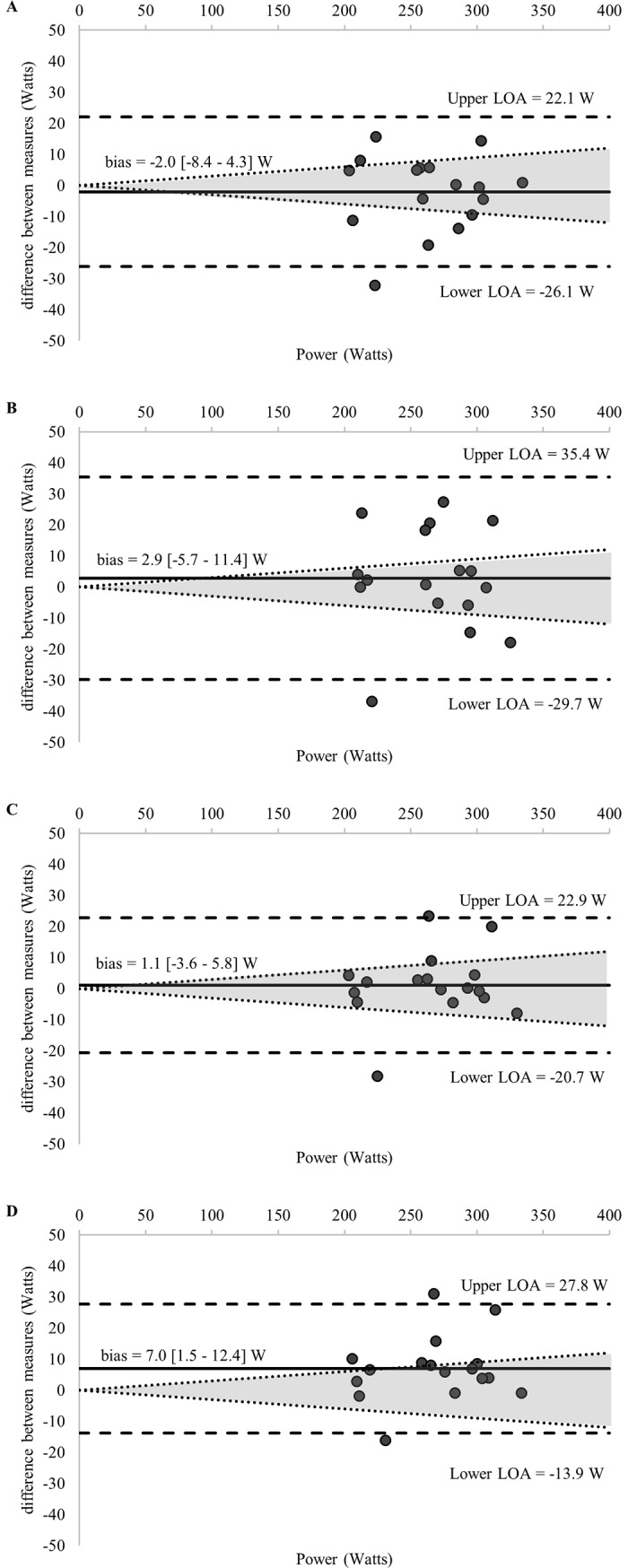
(A-D) Bland-Altman plots displaying agreement between measures of the power associated with the (A) OBLA 2.5 mmol.L-1, (B) Modified Dmax, (C) Log-Poly-Modified Dmax, (D) Log-Exp-Modified Dmax calculated from GXT4 and the MLSS. The differences between measures (y-axis) are plotted as a function of the mean of the two measures (x-axis) in power (Watts). The horizontal solid line represents the mean difference between the two measures (i.e., bias). The two horizontal dashed lines represent the limits of agreement (1.96 x standard deviation of the mean difference between the lactate threshold and the maximal lactate steady state). The dotted diagonal lines represent the boundaries of the 95% CI for MLSS reliability (CV = 3.0%; 95%; CI = 3.8%) calculated from Hauser et al., 2014) (log = Modified Dmax method using the log-log method as the point of the initial lactate point; poly = Modified Dmax method calculated using a third order polynomial regression equation; exp = Modified Dmax method calculated using a constant plus exponential regression equation; OBLA = onset of blood lactate accumulation.).
Fig 6.
(A-C) Bland-Altman plots displaying agreement between measures of the power associated with the (A) OBLA 2.5 mmol.L-1 (GXT7), (B) OBLA 3.0 mmol.L-1 (GXT7), (C) Log-Exp-Modified Dmax calculated from GXT7 and the MLSS. The differences between measures (y-axis) are plotted as a function of the mean of the two measures (x-axis) in power (Watts). The horizontal solid line represents the mean difference between the two measures (i.e., bias). The two horizontal dashed lines represent the limits of agreement (1.96 x standard deviation of the mean difference between the lactate threshold and the maximal lactate steady state). The dotted diagonal lines represent the boundaries of the 95% CI for MLSS reliability (CV = 3.0%; 95%; CI = 3.8%) calculated from Hauser et al., 2014) (log = Modified Dmax method using the log-log method as the point of the initial lactate point; exp = Modified Dmax method calculated using a constant plus exponential regression equation; OBLA = onset of blood lactate accumulation.).
Table 4. Mean difference (MD), effect size (ES), and p-value comparing the influence of graded exercise test stage length on all 14 lactate threshold methods.
| 3 vs. 4 | 3 vs. 7 | 3 vs. 10 | 4 vs. 7 | 4 vs. 10 | 7 vs. 10 | ||
|---|---|---|---|---|---|---|---|
| Log-log LT | MD (W) | 10 | 12 | 15 | 2 | 6 | 3 |
| ES | 0.24 | 0.28 | 0.36 | 0.05 | 0.14 | 0.08 | |
| p-value | 0.09 | 0.02 | 0.02 | 0.63 | 0.15 | 0.47 | |
| OBLA 4.0 mmol.L-1 | MD (W) | 15 | 24 | 27 | 9 | 12 | 3 |
| ES | 0.34 | 0.56 | 0.63 | 0.22 | 0.29 | 0.06 | |
| p-value | 0.00 | 0.00 | 0.00 | 0.05 | 0.01 | 0.35 | |
| OBLA 3.5 mmol.L-1 | MD (W) | 15 | 23 | 25 | 8 | 11 | 3 |
| ES | 0.34 | 0.53 | 0.60 | 0.20 | 0.26 | 0.06 | |
| p-value | 0.00 | 0.00 | 0.00 | 0.09 | 0.02 | 0.35 | |
| OBLA 3.0 mmol.L-1 | MD (W) | 14 | 21 | 24 | 7 | 9 | 3 |
| ES | 0.34 | 0.50 | 0.57 | 0.16 | 0.23 | 0.06 | |
| p-value | 0.00 | 0.00 | 0.00 | 0.16 | 0.05 | 0.36 | |
| OBLA 2.5 mmol.L-1 | MD (W) | 14 | 19 | 21 | 5 | 7 | 2 |
| ES | 0.34 | 0.46 | 0.53 | 0.12 | 0.18 | 0.06 | |
| p-value | 0.00 | 0.00 | 0.00 | 0.30 | 0.13 | 0.39 | |
| OBLA 2.0 mmol.L-1 | MD (W) | 13 | 15 | 18 | 2 | 4 | 2 |
| ES | 0.33 | 0.38 | 0.45 | 0.06 | 0.12 | 0.06 | |
| p-value | 0.01 | 0.01 | 0.00 | 0.63 | 0.36 | 0.45 | |
| Baseline + 0.5 mmol.L-1 | MD (W) | 6 | 7 | 10 | 1 | 4 | 3 |
| ES | 0.16 | 0.18 | 0.27 | 0.03 | 0.10 | 0.07 | |
| p-value | 0.25 | 0.27 | 0.10 | 0.85 | 0.46 | 0.50 | |
| Baseline + 1.0 mmol.L-1 | MD (W) | 16 | 18 | 20 | 3 | 4 | 1 |
| ES | 0.40 | 0.47 | 0.51 | 0.07 | 0.10 | 0.03 | |
| p-value | 0.01 | 0.00 | 0.00 | 0.53 | 0.41 | 0.71 | |
| Baseline + 1.5 mmol.L-1 | MD (W) | 16 | 21 | 23 | 5 | 7 | 2 |
| ES | 0.39 | 0.52 | 0.57 | 0.12 | 0.17 | 0.05 | |
| p-value | 0.00 | 0.00 | 0.00 | 0.27 | 0.14 | 0.49 | |
| Dmax | MD (W) | 13 | 23 | 30 | 10 | 17 | 7 |
| ES | 0.38 | 0.71 | 0.90 | 0.29 | 0.49 | 0.22 | |
| p-value | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | |
| Modified Dmax | MD (W) | 10 | 23 | 29 | 13 | 19 | 6 |
| ES | 0.27 | 0.59 | 0.79 | 0.32 | 0.50 | 0.16 | |
| p-value | 0.01 | 0.00 | 0.00 | 0.01 | 0.00 | 0.06 | |
| Log-Poly-ModDmax | MD (W) | 14 | 25 | 32 | 11 | 18 | 7 |
| ES | 0.35 | 0.62 | 0.78 | 0.26 | 0.43 | 0.18 | |
| p-value | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.02 | |
| Exp-Dmax | MD (W) | 14 | 23 | 29 | 9 | 15 | 6 |
| ES | 0.38 | 0.66 | 0.82 | 0.26 | 0.42 | 0.17 | |
| p-value | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.02 | |
| Log-Exp-ModDmax | MD (W) | 15 | 26 | 33 | 11 | 18 | 7 |
| ES | 0.35 | 0.64 | 0.80 | 0.28 | 0.44 | 0.17 | |
| p-value | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.01 |
Fig 4. Bland-Altman plots displaying agreement between measures of the power associated with the baseline plus 1.5 mmol.L-1 calculated from GXT3 and the MLSS.
The differences between measures (y-axis) are plotted as a function of the mean of the two measures (x-axis) in power (Watts). The horizontal solid line represents the mean difference between the two measures (i.e., bias). The two horizontal dashed lines represent the limits of agreement (1.96 x standard deviation of the mean difference between the lactate threshold and the maximal lactate steady state). The dotted diagonal lines represent the boundaries of the 95% CI for MLSS reliability (CV = 3.0%; 95%; CI = 3.8%) calculated from Hauser et al., 2014).
and
There was an inverse relationship between GXT duration and both and (Table 5). The values derived from GXT3 and GXT4 were similar to the measured during GXT1 (Table 6); however, the values were outside the variability of the measurement (CV > 3%) [27]. values from GXT1 and the corresponding VEB had the highest agreement (MD = 0.5 mL.kg-1.min-1, ICC = 0.96, SEM = 1.1 mL.kg-1.min-1 and CV = 2.0%) compared with any GXT and corresponding VEB. The remaining GXTs and corresponding VEB had a CV of 3.3, 2.0, 3.5 and 5.2%, for GXT3, GXT4, GXT7 and GXT10, respectively. The VEB performed following the longer duration GXTs (GXT3-10) underestimated the from GXT1 (Table 6).
Table 5. Mean and standard deviation of —highest measured during any graded exercise test (GXT); GXT -highest measured during each GXT; VEB highest measured during each verification exhaustive bout (VEB); , highest measured during either the GXT or corresponding VEB.
Mean and standard deviation of GXT duration, max power (Watts) from each GXT, percentage of maximum power from the prolonged GXT expressed as a percentage of W maximum power from GXT1 and power of each VEB (Watts) from the GXTs. Relative power of the verification exhaustive bout expressed as a percentage (%) of the maximal power measured during the GXT. The subscript (i.e., 1, 3, 4, 7 or 10) refers to the stage duration (minutes) for each test.
| GXT1 | GXT3 | GXT4 | GXT7 | GXT10 | |
|---|---|---|---|---|---|
| (mL.kg-1.min-1) | 62.1 ± 5.8 | ||||
| GXT (mL.kg-1.min-1) | 60.6 ± 5.4 | 58.2 ± 5.3 | 57.3 ± 5.7 | 56.4 ± 5.2 | 54.9 ± 4.9 |
| VEB (mL.kg-1.min-1) | 60.1 ± 5.8 | 58.9 ± 5.9 | 58.8 ± 6.1 | 56.4 ± 5.9 | 54.7 ± 6.6 |
| (mL.kg-1.min-1) | 61.0 ± 5.3 | 59.7 ± 5.4 | 58.9 ± 6.0 | 57.3 ± 5.4 | 56.2 ± 5.5 |
| GXT Duration (min) | 11.3 ± 0.9 | 26.8 ± 1.4 | 34.9 ± 1.9 | 59.2 ± 3.3 | 81.6 ± 4.6 |
| Maximum Power (Watts) | 420 ± 55 | 337 ± 46 | 321 ± 47 | 303 ± 43 | 295 ± 43 |
| Percent of GXT1 (%) | 100 | 80.3 ± 2.9 | 76.4 ± 3.1 | 72.1 ± 3.6 | 70.3 ± 4.0 |
| VEB (Watts) | 378 ± 50 | ||||
| VEB (% of GXT ) | 90 | 109.7 ± 3.8 | 118.4 ± 18.7 | 125.4 ± 19.3 | 128.8 ± 20.4 |
Table 6. Mean difference (MD) and standard deviation, effect size (ES), coefficient of the variation (CV) and p-value (p) for the measured values from GXT1 compared with the values from GXT3, GXT4, GXT7, and GXT10 and for the values from GXT1 compared with the values from the VEB following GXT3, GXT4, GXT7, and GXT10.
The subscript (i.e., 1, 3, 4, 7 or 10) refers to the stage duration (minutes) for each test.
| GXT1 vs. GXT3 | GXT1 vs. GXT4 | GXT1 vs. GXT7 | GXT1 vs. GXT10 | |
| MD (mL.kg-1.min-1) | -1.2 ± 3.3 | -2.1 ± 4.2 | -3.7 ± 4.7 | -4.8 ± 3.7 |
| ES | 0.23 | 0.36 | 0.69 | 0.88 |
| CV (%) | 3.8 | 4.9 | 5.6 | 4.6 |
| p | 0.13 | 0.06 | < 0.01 | < 0.01 |
| GXT1 vs. VEB GXT3 | GXT1 vs. VEB GXT4 | GXT1 vs. VEB GXT7 | GXT1 vs. VEB GXT10 | |
| MD (mL.kg-1.min-1) | -2.1 ± 5.9 | -2.1 ± 6.1 | -4.6 ± 5.9 | -6.2 ± 6.6 |
| ES | 0.37 | 0.37 | 0.81 | 1.04 |
| CV (%) | 4.2 | 4.9 | 6.1 | 5.9 |
| p | 0.02 | 0.98 | 0.03 | 0.03 |
Discussion
The main findings of the present study are as follows. Only 11 of the 58 threshold values met our inclusion criteria as valid estimates of the MLSS. Of the 11 methods included in our analysis, three of the ModDmax methods yielded the most favourable estimations of the MLSS, and the Log-Poly-ModDmax derived from GXT4 provided the best estimation of the MLSS. There was an inverse relationship between stage length and LT, and this effect was larger in all Dmax methods compared with the OBLA and baseline plus absolute lactate value methods. The values measured during the longer duration GXTs (GXT3-10) underestimated the and the values obtained from GXT1 (MD = 1.2 to 4.8 mL.kg-1.min-1). Finally, contrary to our hypothesis, the VEB after the longer duration GXTs did not yield values comparable to the derived from GXT1.
The use of five GXT protocols, 14 common LT methods, the RCP and RCPMLSS resulted in 58 unique thresholds. However, despite their common use, we observed that only 11 of these values met our criteria for inclusion (MD < 7.9 W; ES < 0.2; r > 0.90). Of the four Dmax methods included in our analysis, one consisted of the traditional ModDmax method [22]. This had the poorest agreement relative to the other ModDmax methods included in our analysis. The remaining three Dmax methods are new variations of the ModDmax method, and the Log-Poly-ModDmax derived from GXT4 had the highest correlation and lowest mean difference with the MLSS. These variations of the ModDmax method use the power at the log-log LT as the initial intensity to calculate the ModDmax and then either the traditional third-order polynomial or exponential plus-constant regression curve to fit the lactate curve [23, 41]. Although the validity of these three methods has not previously been assessed, the favourable estimations of the MLSS may be related to the greater objectivity with which they determine the intensity that corresponds with the initial rise in blood lactate concentration [37].
Although the original Dmax method is a commonly cited method for determining the LT [23], we observed large mean differences (19 to 49 W) between the Dmax and MLSS. Three previous studies have purported to investigate the validity of this method to estimate the MLSS in trained male cyclists [15, 52, 53]. One concluded that the Dmax method derived from GXT3 was a valid estimation of the MLSS (r = 0.97) [54]. We also observed a high correlation between Dmax and the MLSS (r = 0.94 to 0.97) (Table 1), but, as indicated by the MD and other measures, a high correlation is not sufficient to establish validity [55]. Another study examined Dmax derived from two GXTs with similar durations (36 vs. 39 min), but with different stage lengths (30-s vs. 6-min) [15]. The Dmax derived from GXT30s was not correlated (r = 0.51) with the MLSS, even though the MD was 5 W, whilst the Dmax derived from GXT6 was correlated (r = 0.85); however, it underestimated the MLSS (MD = 22 W). The third study concluded the Dmax derived from GXT1 yielded poor estimates of the MLSS (r = 0.56; bias = -1.8 ± 38.1 W) [53]. Thus, although some studies [15, 54] have used correlation analysis to suggest the Dmax provides a valid estimate of the MLSS, this is not supported by the more comprehensive assessment of validity performed in the present and other studies [53].
There were five fixed blood LT methods and one baseline plus an absolute value that met our inclusion criteria, and, as previously reported [15, 24], these varied with the GXT protocol used. The baseline + 1.5 mmol.L-1 was the only LT derived from GXT3 included in our analysis (bias = -6 ± 35 W). This is consistent with the results of one previous study (bias = 0.5 ± 24 W), which also recruited trained male cyclists and had a similar GXT protocol design [56]. Consistent with our findings, this study also reported that an OBLA of 3.5 mmol.L-1 derived from GXT3 did not provide a valid estimation of the MLSS. In contrast, another study confirmed the validity of the OBLA of 3.5 mmol.L-1 [52], despite recruiting trained cyclists and using an identical GXT protocol. These conflicting results are likely attributable to the low reproducibility of the OBLA methods [16].
While none of the OBLAs from GXT3 met our inclusion criteria, the OBLA methods of 2.5 mmol.L-1 derived from GXT4 and GXT7 provided valid estimations of the MLSS, as did the OBLA of 3.0 mmol.L-1 derived from GXT7 and GXT10. The OBLA of 3.5 mmol.L-1 from GXT10 was the highest fixed blood LT that identified the MLSS. There is no previous data investigating the validity of these OBLA methods. However, it is worth noting that these five methods provided superior estimations of the MLSS compared with the original ModDmax, but were less favourable than the newly-developed ModDmax methods.
An OBLA of 4.0 mmol.L-1 is the most commonly-accepted fixed blood lactate value for estimating the LT or MLSS. Three previous studies have attempted to validate use of an OBLA of 4.0 mmol.L-1 with cycle ergometry [15, 53, 57]. One study found that it overestimated the MLSS (MD = 49 W) when derived from GXT1 [53]. The other study reported poor agreement (bias 7 ± 49 W) when OBLA of 4.0 mmol.L-1 was derived from GXT4 [57]. The final study observed a poor correlation between an OBLA of 4.0 mmol.L-1 and the MLSS (r = 0.71) [15]. Our results indicated the OBLA of 4.0 mmol.L-1 overestimated the MLSS across all GXTs. Thus, in agreement with previous research, our results indicate; the OBLA of 4.0 mmol.L-1 does not accurately estimate the MLSS. It is also worth noting that the original authors cautioned the use of this OBLA method, given the lack of a significant correlation when comparing OBLA methods from a GXT and the MLSS [24].
The RCP derived from an 8- to 12-minute GXT consistently overestimates the MLSS [44, 53], and this was confirmed in our study (Table 1). Therefore, we used a regression equation based on the RCP (RCPMLSS) (Eq 5) to estimate the starting intensity for establishing the MLSS [33]. Our results indicate there was good agreement between the MLSS and RCPMLSS (Table 3). Nonetheless, for many participants the difference between MLSS and RCPMLSS exceeded the CV% for the MLSS (Fig 3). Therefore, although the RCPMLSS can be used as a convenient ‘starting point’ when establishing the MLSS, we recommend methods based on blood sampling from the current study and assessing blood lactate kinetics in real time as recommended by Hering et al. [58] for a more accurate estimation of the MLSS.
Although a single GXT can be used to estimate both and LT, the optimal test duration for each measure is different [11, 13]. To address this challenge, we added a supramaximal VEB after each GXT, equivalent to that performed following GXT1, expecting all VEBs would yield similar values. However, the values from the VEB after the longer duration GXTs underestimated the from GXT1. Although the values from GXT3 and GXT4 were similar to GXT1, the differences were larger than the typical coefficient of variability for (CV < 3%) [59]. Our results are consistent with previous recommendations that longer duration GXTs are not optimal for establishing [10, 60]. Furthermore, while a VEB can be used to verify that was achieved, it appears that a VEB following a prolonged GXT cannot be used to establish .
Extending the duration of the GXT stages results in a lower [61]. This has implications for exercise prescription, as it is common in sport and exercise science research to prescribe exercise intensity as a percentage of . For example, in the present study the MLSS ranged from 63 ± 4% (range = 52 to 72%) of from GXT1 to 82 ± 4% (range = 74 to 88%) of from GXT4. Prescribing exercise in the current study cohort at a fixed percentage of (e.g., 73% of ), would result in all participants exercising above or below the MLSS, GXT1 and GXT4, respectively. This is important as it has previously been reported that prescribing exercise relative to LT results in a more homogenous physiological response than when exercise performed relative to [62]. This also highlights why it is important to consider the GXT protocol and the method used to determine relative exercise intensity when comparing results between studies.
The wide range of for each GXT is also note-worthy, the range for GXT1 was 320 to 517 W and the duration ranged from 9 to 12 minutes. Had we employed a standardized GXT (e.g., 35 W increments), and assuming stayed constant, the range would have been 9- to 15 min. Applying this to our longer duration GXTs resulted in a homogenous duration (GXT4: 32- to 39 min), whereas a standardised approach (e.g., 35 W increments) would have resulted in a range of 27- to 46 min [57]. Thus, individualizing GXT protocol design is a useful approach to ensure homogenous test duration [17].
Conclusion
In conclusion, the traditional Dmax and OBLA of 4.0 mmol.L-1 did not provide valid estimates of the MLSS. The best estimation of the MLSS was the Log-Poly-ModDmax derived from GXT4. The validity of our newly-developed ModDmax model may relate to the objectivity for determining the initial rise in blood lactate concentration. However, we must advise caution with the use of our newly-developed method until future research investigates the reliability and reproducibility. It is apparent that both and LT cannot be determined in a single GXT, even if the GXT is followed by a VEB. Therefore, to appropriately determine the optimum duration of a GXT is 8–12 minutes and the values measured during the GXT and VEB be within 3% = CV [63]. Our data also highlight how differences in GXT protocol design and methods used to calculate the relative exercise intensity may contribute to the conflicting findings reported in the literature.
Abbreviations
- LT
lactate threshold
- GXT
graded exercise testing
maximal oxygen uptake
- OBLA
onset of fixed blood lactate accumulation
- MLSS
maximal lactate steady state
- VEB
verification exhaustive bout
- BMI
body mass index
maximum power output
highest measured oxygen uptake value
- RCP
respiratory compensation point
- RCPMLSS
estimate of the maximal lactate steady state via respiratory compensation point
- B + mmol.L-1
blood lactate concentration increases above baseline value(s)
- ModDmax
modified Dmax
- Exp-Dmax
exponential Dmax
- Log-Poly-ModDmax
Log-log Modified Dmax
- Log-Exp-ModDmax
Log-log Exponential Modified Dmax
- CV
coefficient of the variation
- ES
effect size
- r
Pearson product moment correlation
- ICC
intraclass correlation
- SEM
standard error of the measurement
Data Availability
The data underlying this study have been uploaded to the Open Science Framework and are accessible using the following link: https://osf.io/293ns/.
Funding Statement
Funding was provided by the Graduate Research Office (PhD Student Budget) at Victoria University. The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Skinner JS, McLellan TH. The transition from aerobic to anaerobic metabolism. Research Quarterly for Exercise and Sport. 1980;51(1):234–48. 10.1080/02701367.1980.10609285 [DOI] [PubMed] [Google Scholar]
- 2.Londeree BR. Effect of training on lactate/ventilatory thresholds: a meta-analysis. Medicine and Science in Sport and Exercise. 1997;29(6):837–43. [DOI] [PubMed] [Google Scholar]
- 3.Wenger HA, Bell GJ. The interactions of intensity, frequency and duration of exercise training in altering cardiorespiratory fitness. Sports Medicine. 1986;3(5):346–56. [DOI] [PubMed] [Google Scholar]
- 4.Mann T, Lamberts RP, Lambert MI. Methods of prescribing relative exercise intensity: physiological and practical considerations. Sports Medicine. 2013;43(7):613–25. 10.1007/s40279-013-0045-x [DOI] [PubMed] [Google Scholar]
- 5.Coen B, Schwarz L, Urhausen A, Kindermann W. Control of training in middle-and long-distance running by means of the individual anaerobic threshold. International Journal of Sports Medicine. 1991;12(06):519–24. [DOI] [PubMed] [Google Scholar]
- 6.Granata C, Jamnick NA, Bishop DJ. Principles of Exercise Prescription, and How They Influence Exercise-Induced Changes of Transcription Factors and Other Regulators of Mitochondrial Biogenesis. Sports Medicine. 2018:1–19. [DOI] [PubMed] [Google Scholar]
- 7.González-Haro C. Differences in Physiological Responses Between Short-vs. Long-Graded Laboratory Tests in Road Cyclists. Journal of Strength and Conditioning Research. 2015;29(4):1040–8. 10.1519/JSC.0000000000000741 [DOI] [PubMed] [Google Scholar]
- 8.McNaughton LR, Roberts S, Bentley DJ. The relationship among peak power output, lactate threshold, and short-distance cycling performance: effects of incremental exercise test design. Journal of Strength and Conditioning Research. 2006;20(1):157 10.1519/R-15914.1 [DOI] [PubMed] [Google Scholar]
- 9.Bentley D, McNaughton L, Batterham A. Prolonged stage duration during incremental cycle exercise: effects on the lactate threshold and onset of blood lactate accumulation. European Journal of Applied Physiology. 2001;85(3–4):351–7. 10.1007/s004210100452 [DOI] [PubMed] [Google Scholar]
- 10.Poole DC, Jones AM. Measurement of the maximum oxygen uptake is no longer acceptable. Journal of Applied Physiology. 2017;122(4):997–1002. 10.1152/japplphysiol.01063.2016 [DOI] [PubMed] [Google Scholar]
- 11.Buchfuhrer MJ, Hansen JE, Robinson TE, Sue DY, Wasserman K, Whipp BJ. Optimizing the exercise protocol for cardiopulmonary assessment. Journal of Applied Physiology. 1983;55(5):1558–64. 10.1152/jappl.1983.55.5.1558 [DOI] [PubMed] [Google Scholar]
- 12.Yoon B-K, Kravitz L, Robergs R. VO2max, Protocol Duration, and the VO2 Plateau. Medicine and Science in Sport and Exercise. 2007;39(7):1186–92. 10.1249/mss.0b13e318054e304 [DOI] [PubMed] [Google Scholar]
- 13.Bentley DJ, Newell J, Bishop D. Incremental exercise test design and analysis. Sports Medicine. 2007;37(7):575–86. [DOI] [PubMed] [Google Scholar]
- 14.Foxdal P, Sjödin A, Sjödin B. Comparison of blood lactate concentrations obtained during incremental and constant intensity exercise. International Journal of Sports Medicine. 1996;17(05):360–5. [DOI] [PubMed] [Google Scholar]
- 15.Van Schuylenbergh R, Vanden EB, Hespel P. Correlations between lactate and ventilatory thresholds and the maximal lactate steady state in elite cyclists. International Journal of Sports Medicine. 2004;25(6):403–8. 10.1055/s-2004-819942 [DOI] [PubMed] [Google Scholar]
- 16.Morton RH, Stannard SR, Kay B. Low reproducibility of many lactate markers during incremental cycle exercise. British Journal of Sports Medicine. 2012;46(1):64–9. 10.1136/bjsm.2010.076380 [DOI] [PubMed] [Google Scholar]
- 17.Pettitt R, Clark I, Ebner S, Sedgeman D, Murray S. Gas Exchange Threshold and VO2max Testing for Athletes: An Update. Journal of Strength and Conditioning Research. 2013;27(2):549–55. 10.1519/JSC.0b013e31825770d7 [DOI] [PubMed] [Google Scholar]
- 18.Faude O, Kindermann W, Meyer T. Lactate threshold concepts. Sports Medicine. 2009;39(6):469–90. 10.2165/00007256-200939060-00003 [DOI] [PubMed] [Google Scholar]
- 19.Ivy JL, Withers RT, Vanhandel PJ, Elger DH, Costill DL. Muscle respiratory capacity and fiber type as determinants of the lactate threshold. Journal of Applied Physiology. 1980;48(3):523–7. PubMed PMID: WOS:A1980JJ95100018. 10.1152/jappl.1980.48.3.523 [DOI] [PubMed] [Google Scholar]
- 20.Kindermann W, Simon G, Keul J. Significance of the aerobic-anaerobic transition for the determination of work load intensities during endurance training. European Journal of Applied Physiology and Occupational Physiology. 1979;42(1):25–34. 10.1007/bf00421101 PubMed PMID: WOS:A1979HN15900003. [DOI] [PubMed] [Google Scholar]
- 21.Heck H, Mader A, Hess G, Mucke S, Muller R, Hollmann W. Justification of the 4-mmol/L lactate threshold. International Journal of Sports Medicine. 1985;6(3):117–30. 10.1055/s-2008-1025824 PubMed PMID: WOS:A1985ALS1800002. [DOI] [PubMed] [Google Scholar]
- 22.Bishop D, Jenkins DG, Mackinnon LT. The relationship between plasma lactate parameters, Wpeak and 1-h cycling performance in women. Medicine and Science in Sports and Exercise. 1998;30(8):1270–5. [DOI] [PubMed] [Google Scholar]
- 23.Cheng B, Kuipers H, Snyder A, Keizer H, Jeukendrup A, Hesselink M. A new approach for the determination of ventilatory and lactate thresholds. International Journal of Sports Medicine. 1992;13(7):518–22. 10.1055/s-2007-1021309 [DOI] [PubMed] [Google Scholar]
- 24.Heck H, Mader A, Hess G, Mücke S, Müller R, Hollmann W. Justification of the 4-mmol/l lactate threshold. International Journal of Sports Medicine. 1985;(6):117–30. [DOI] [PubMed] [Google Scholar]
- 25.Billat VL, Sirvent P, Py G, Koralsztein J-P, Mercier J. The concept of maximal lactate steady state. Sports Medicine. 2003;33(6):407–26. [DOI] [PubMed] [Google Scholar]
- 26.Beneke R. Methodological aspects of maximal lactate steady state—implications for performance testing. European Journal of Applied Physiology. 2003;89(1):95–9. 10.1007/s00421-002-0783-1 [DOI] [PubMed] [Google Scholar]
- 27.Hauser T, Bartsch D, Baumgärtel L, Schulz H. Reliability of maximal lactate-steady-state. International Journal of Sports Medicine. 2013;34(3):196–9. 10.1055/s-0032-1321719 [DOI] [PubMed] [Google Scholar]
- 28.Hill AV, Long C, Lupton H. Muscular exercise, lactic acid, and the supply and utilisation of oxygen. Proceedings of the Royal Society of London Series B, Containing Papers of a Biological Character. 1924;97(681):84–138. [Google Scholar]
- 29.Riebe D, Franklin BA, Thompson PD, Garber CE, Whitfield GP, Magal M, et al. Updating ACSM’s recommendations for exercise preparticipation health screening. Medicine and Science in Sport and Exercise. 2015;47(11):2473–9. 10.1249/MSS.0000000000000664 [DOI] [PubMed] [Google Scholar]
- 30.Jamnick NA, By S, Pettitt CD, Pettitt RW. Comparison of the YMCA and a Custom Submaximal Exercise Test for Determining VO2max. Medicine and Science in Sport and Exercise. 2016;48(2):254–9. 10.1249/MSS.0000000000000763 [DOI] [PubMed] [Google Scholar]
- 31.Jackson AS, Blair SN, Mahar MT, Wier LT, Ross RM, Stuteville JE. Prediction of functional aerobic capacity without exercise testing. Medicine and Science in Sports and Exercise. 1990;22(6):863–70. Epub 1990/12/01. . [DOI] [PubMed] [Google Scholar]
- 32.Medicine ACoS. ACSM's guidelines for exercise testing and prescription: Lippincott Williams & Wilkins; 2013. [DOI] [PubMed] [Google Scholar]
- 33.Smekal G, von Duvillard SP, Pokan R, Hofmann P, Braun WA, Arciero PJ, et al. Blood lactate concentration at the maximal lactate steady state is not dependent on endurance capacity in healthy recreationally trained individuals. European Journal of Applied Physiology. 2012;112(8):3079–86. 10.1007/s00421-011-2283-7 [DOI] [PubMed] [Google Scholar]
- 34.Beaver W, Wasserman K, Whipp B. A new method for detecting anaerobic threshold by gas exchange. Journal of Applied Physiology. 1986;60(6):2020–7. 10.1152/jappl.1986.60.6.2020 [DOI] [PubMed] [Google Scholar]
- 35.Whipp BJ, Davis JA, Wasserman K. Ventilatory control of the ‘isocapnic buffering’region in rapidly-incremental exercise. Respiration Physiology. 1989;76(3):357–67. [DOI] [PubMed] [Google Scholar]
- 36.Caiozzo VJ, Davis JA, Ellis JF, Azus JL, Vandagriff R, Prietto C, et al. A comparison of gas exchange indices used to detect the anaerobic threshold. Journal of Applied Physiology. 1982;53(5):1184–9. 10.1152/jappl.1982.53.5.1184 [DOI] [PubMed] [Google Scholar]
- 37.Beaver W, Wasserman K, Whipp B. Improved detection of lactate threshold during exercise using a log-log transformation. Journal of Applied Physiology. 1985;59(6):1936–40. 10.1152/jappl.1985.59.6.1936 [DOI] [PubMed] [Google Scholar]
- 38.Kindermann W, Simon G, Keul J. The significance of the aerobic-anaerobic transition for the determination of work load intensities during endurance training. European Journal of Applied Physiology and Occupational Physiology. 1979;42(1):25–34. [DOI] [PubMed] [Google Scholar]
- 39.Zoladz JA, Rademaker A, Sargeant AJ. Non-linear relationship between O2 uptake and power output at high intensities of exercise in humans. Journal of Physiology. 1995;488(Pt 1):211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Berg A, Jakob E, Lehmann M, Dickhuth H, Huber G, Keul J. Current aspects of modern ergometry. Pneumologie (Stuttgart, Germany). 1990;44(1):2. [PubMed] [Google Scholar]
- 41.Machado FA, Nakamura FY, Moraes SMFD. Influence of regression model and incremental test protocol on the relationship between lactate threshold using the maximal-deviation method and performance in female runners. Journal of Sports Sciences. 2012;30(12):1267–74. 10.1080/02640414.2012.702424 [DOI] [PubMed] [Google Scholar]
- 42.Hughson RL, Weisiger KH, Swanson GD. Blood lactate concentration increases as a continuous function in progressive exercise. Journal of Applied Physiology. 1987;62(5):1975–81. 10.1152/jappl.1987.62.5.1975 [DOI] [PubMed] [Google Scholar]
- 43.Lamarra N, Whipp BJ, Ward SA, Wasserman K. Effect of interbreath fluctuations on characterizing exercise gas exchange kinetics. Journal of Applied Physiology. 1987;62(5):2003–12. 10.1152/jappl.1987.62.5.2003 [DOI] [PubMed] [Google Scholar]
- 44.Keir DA, Fontana FY, Robertson TC, Murias JM, Paterson DH, Kowalchuk JM, et al. Exercise Intensity Thresholds: Identifying the Boundaries of Sustainable Performance. Medicine and Science in Sport and Exercise. 2015;47(9):1932–40. 10.1249/MSS.0000000000000613 [DOI] [PubMed] [Google Scholar]
- 45.Keir DA, Murias JM, Paterson DH, Kowalchuk JM. Breath‐by‐breath pulmonary O2 uptake kinetics: effect of data processing on confidence in estimating model parameters. Experimental Physiology. 2014;99(11):1511–22. 10.1113/expphysiol.2014.080812 [DOI] [PubMed] [Google Scholar]
- 46.Lawrence I, Lin K. A concordance correlation coefficient to evaluate reproducibility. Biometrics. 1989:255–68. [PubMed] [Google Scholar]
- 47.Bland JM, Altman D. Statistical methods for assessing agreement between two methods of clinical measurement. The Lancet. 1986;327(8476):307–10. [PubMed] [Google Scholar]
- 48.Hopkins W. Analysis of validity by linear regression (Excel spreadsheet). 2015;19:36–44. [Google Scholar]
- 49.Hopkins W. Measures of reliability in sports medicine and science. Sports Medicine. 2000;30(1):1–15. [DOI] [PubMed] [Google Scholar]
- 50.Hopkins W, Marshall S, Batterham A, Hanin J. Progressive statistics for studies in sports medicine and exercise science. Medicine and Science in Sports and Exercise. 2009;41(1):3 10.1249/MSS.0b013e31818cb278 [DOI] [PubMed] [Google Scholar]
- 51.Cohen J. A power primer. Psychological Bulletin. 1992;112(1):155 [DOI] [PubMed] [Google Scholar]
- 52.Denadai B, Figueira T, Favaro O, Gonçalves M. Effect of the aerobic capacity on the validity of the anaerobic threshold for determination of the maximal lactate steady state in cycling. Brazilian Journal of Medical and Biological Research. 2004;37(10):1551–6. doi: /S0100-879X2004001000015 [DOI] [PubMed] [Google Scholar]
- 53.Pallarés JG, Morán-Navarro R, Ortega JF, Fernández-Elías VE, Mora-Rodriguez R. Validity and Reliability of Ventilatory and Blood Lactate Thresholds in Well-Trained Cyclists. PloS one. 2016;11(9):e0163389 10.1371/journal.pone.0163389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Czuba M, Zając A, Cholewa J, Poprzęcki S, Waśkiewicz Z, Mikołajec K. Lactate threshold (D-max method) and maximal lactate steady state in cyclists. Journal of Human Kinetics. 2009;21:49–56. [Google Scholar]
- 55.Aldrich J. Correlations genuine and spurious in Pearson and Yule. Statistical Science. 1995:364–76. [Google Scholar]
- 56.Grossl T, De Lucas RD, De Souza KM, Antonacci Guglielmo LG. Maximal lactate steady-state and anaerobic thresholds from different methods in cyclists. European Journal of Sport Science. 2012;12(2):161–7. [Google Scholar]
- 57.Hauser T, Adam J, Schulz H. Comparison of selected lactate threshold parameters with maximal lactate steady state in cycling. International Journal of Sports Medicine. 2014;35(6):517–21. 10.1055/s-0033-1353176 [DOI] [PubMed] [Google Scholar]
- 58.Hering GO, Hennig EM, Riehle HJ, Stepan J. A Lactate Kinetics Method for Assessing the Maximal Lactate Steady State Workload. Frontiers in Physiology. 2018;9(310). 10.3389/fphys.2018.00310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kirkeberg J, Dalleck L, Kamphoff C, Pettitt R. Validity of 3 protocols for verifying VO2max. International Journal of Sports Medicine. 2011;32(04):266–70. [DOI] [PubMed] [Google Scholar]
- 60.Bishop D, Jenkins DG, Mackinnon LT. The effect of stage duration on the calculation of peak VO2 during cycle ergometry. Journal of Science and Medicine in Sport. 1998;1(3):171–8. [DOI] [PubMed] [Google Scholar]
- 61.Adami A, Sivieri A, Moia C, Perini R, Ferretti G. Effects of step duration in incremental ramp protocols on peak power and maximal oxygen consumption. European Journal of Applied Physiology. 2013;113(10):2647–53. 10.1007/s00421-013-2705-9 [DOI] [PubMed] [Google Scholar]
- 62.Baldwin J, Snow RJ, Febbraio MA. Effect of training status and relative exercise intensity on physiological responses in men. Medicine and Science in Sport and Exercise. 2000;32(9):1648–54. [DOI] [PubMed] [Google Scholar]
- 63.Pettitt RW, Jamnick NA. Commentary on “Measurement of the maximum oxygen uptake is no longer acceptable”. Journal of Applied Physiology. 2017;123(3):696–. 10.1152/japplphysiol.00338.2017 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data underlying this study have been uploaded to the Open Science Framework and are accessible using the following link: https://osf.io/293ns/.