Summary
Vocal cord palsy (VCP) is one of the most frequent complications following thyroidectomy. We evaluated the outcomes of intraoperative reconstruction of the recurrent laryngeal nerve (RLN). Of 917 patients who underwent thyroid surgery in a single high-volume general surgery ward between 2000 and 2015, 12 (1.3%) were diagnosed with RLN injury and were retrospectively categorized into 2 groups: group A (n = 5), with intraoperative evidence of iatrogenic transection or cancer invasion of the RLN, and group B (n = 7), with postoperative confirmation of VCP. In group A, immediate microsurgical primary repair of the RLN was performed. Postoperative assessment included subjective ratings (aspiration and voice quality improvement) and objective ratings (perceptual voice quality according to the grade, roughness, breathiness, asthenia and strain [GRBAS] scale, and direct laryngoscopy). In group A, roughness, breathiness and strain were significantly lower at 9 months than at 3 months (p < 0.05). Although larger, multicentre studies are needed, the results suggest potentially excellent postoperative phonatory function after immediate RLN reconstruction.
Recurrent laryngeal nerve (RLN) palsy is one of the most common complications following total thyroidectomy. It is caused by iatrogenic lesions or by adhesion to thyroid cancer. Recurrent laryngeal nerve palsy has a detrimental impact on patients’ outcomes,1 and it often leads to accusations of malpractice.2 Postoperative vocal cord palsy (VCP) is rarely asymptomatic: it causes hoarseness and swallowing difficulties; when bilateral, emergency tracheotomy is needed. This complication can be recognized intraoperatively or diagnosed postoperatively by laryngoscopy.
We analyzed the outcomes of patients who underwent intraoperative reconstruction of the transected RLN compared to a control group of patients in whom no reconstruction was performed.
Approach
Between 2000 and 2015, 917 patients (582 women and 335 men with a mean age of 49.3 yr) underwent total thyroidectomy performed by the same surgeon in a single high-volume (> 100 thyroidectomy procedures per year over the last 5 yr) general surgery ward. In 73 cases (8.0%), minimally invasive video-assisted thyroidectomy was performed. Preoperative fibre-optic laryngoscopy was performed in all patients, and preoperative evidence of VCP represented an exclusion criterion. Written informed consent was obtained before surgery in all cases.
The standardized capsular dissection approach was used. The parathyroid glands and RLNs were meticulously dissected with the use of 3× surgical magnifying glasses and microsurgical instruments, and hemostasis was achieved close to these structures by means of conventional ligature improved with biosurgical agents. With the exception of cases of minimally invasive video-assisted thyroidectomy, a drainage was placed.
Definitive unilateral VCP was diagnosed in 12 patients (1.3%), and they were considered eligible for the study. The 12 patients were retrospectively categorized into 2 groups: group A (n = 5), in which a therapeutic sacrifice for cancer invasion or iatrogenic transection (Fig. 1) was recognized during thyroidectomy, and group B (n = 7), in which unilateral VCP was confirmed by fibreoptic laryngoscopy.
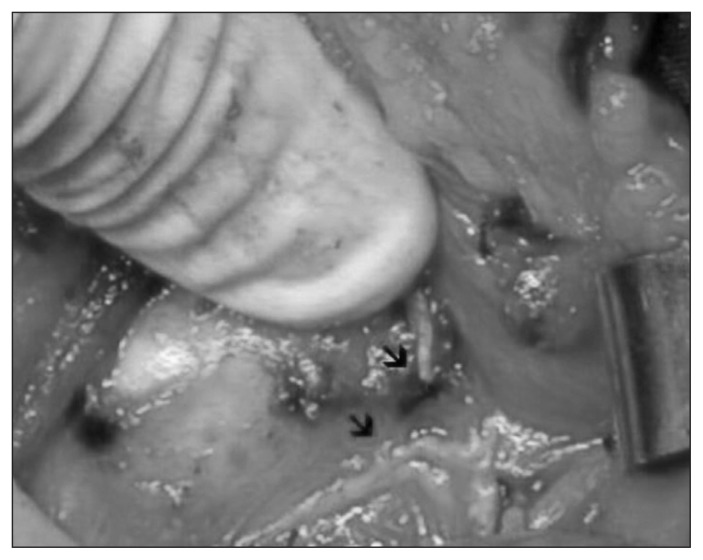
Fig. 1.
Intraoperative image of an iatrogenic lesion of the recurrent laryngeal nerve. The arrows indicate the 2 nerve stumps.
In group A, an intraoperative RLN primary repair (endto- end epineural repair) was made with three to five 7-0 nylon sutures (Ethicon) with the use of microsurgical instruments and 3× magnifying glasses. The defect was 5 mm or less in all cases, and the stumps of the RLNs could be approximated without tension. In group B, the unilateral injury to the RLN was suspected because of immediate or late voice change, dyspnea and dysphagia, and was confirmed by laryngoscopy.
Patients with VCP were seen in weekly/monthly follow-up and received speech therapy and steroid medication for at least 9 months. Assessment was performed 3 and 9 months after the VCP diagnosis by means of subjective ratings of aspiration and voice quality improvement, objective ratings of perceptual voice quality and laryngeal video-stroboscopy examinations. Aspiration was rated on a 4-point scale where 0 = normal (occasional choking with or without the need for dietary modifications), 1 = mild (occasional choking with or without the need for dietary modifications), 2 = moderate and 3 = severe (feeding tube placement for alimentation). Voice quality improvement was rated on a 4-point scale where 0 = markedly improved, 1 = improved, 2 = unchanged and 3 = worse. Perceptual voice quality was evaluated by a laryngologist and a speech pathologist according to the grade, roughness, breathiness, asthenia and strain (GRBAS) scale (0 = normal, 1 = mild dysphonia, 2 = moderate dysphonia, 3 = severe dysphonia, 4 = aphonia).3 Direct laryngoscopy was performed, evaluating the sustained phonation of vowels and making a grading scale of the glottal gap (0 = normal, 1 = minimal gap, 2 = moderate gap, 3 = severe gap, 4 = complete glottal incompetence).
This study was approved by the local ethics committee.
Comparisons
We made comparisons using the Student t test for independent samples for continuous variables, the χ2 test or Fisher exact test for frequencies, and the Wilcoxon signed-rank test for paired observations of ordinal variables. A p value < 0.05 was considered statistically significant. Analysis was performed with Stata 14 (StataCorp).
Outcome
No patient had preoperative evidence of VCP. No significant differences between groups were observed in demographic characteristics or histological findings (Table 1). In 3 patients (60%) in group A, the RLN lesion was iatrogenic, and in 2 (40%), the nerve was sacrificed for cancer invasion without preoperative VCP. Subjective ratings of aspiration and voice quality improvement are summarized in Table 2, objective ratings of perceptual voice quality in Table 3 and results of laryngeal videostroboscopy in Table 4. In group B, the subjective rating of aspiration was significantly improved at 9 months (p = 0.02). There were significant improvements in the GRBAS scale of perceptual voice quality in both groups at 9 months (p < 0.05). In group A, roughness, breathiness and strain were significantly lower at 9 months than at 3 months (p = 0.04). Laryngoscopy in this group showed that fixed vocal cords in the median position were not atrophic, had good tension and showed a narrow gap during phonation.
Table 1.
Demographic characteristics and histological diagnosis of patients with definitive unilateral vocal cord palsy after thyroidectomy
| Variable | No. (%) of patients* | p value† | |
|---|---|---|---|
| Group A n = 5 |
Group B n = 7 |
||
| Age, yr, mean ± SD | 57.4 ± 21.7 | 56.8 ± 19.9 | 1.0 |
| Sex | 0.7 | ||
| Male | 2 (40) | 2 (29) | |
| Female | 3 (60) | 5 (71) | |
| Histological diagnosis | 0.6 | ||
| Benign | 2 (40) | 4 (57) | |
| Malignant | 3 (60) | 3 (43) | |
SD = standard deviation.
Except where noted otherwise.
Student t test for independent samples or χ2 test.
Table 2.
Subjective ratings of aspiration and voice quality improvement at 3 and 9 months postoperatively
| Variable; score | Group A, no. of patients | Group B, no. of patients | ||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| 3 mo | 9 mo | p value* | 3 mo | 9 mo | p value* | |
| Aspiration† | ||||||
|
| ||||||
| 2 | 3 | 0 | 0.05 | 5 | 2 | 0.02 |
|
| ||||||
| 1 | 1 | 0 | 2 | 3 | ||
|
| ||||||
| 0 | 1 | 5 | 0 | 2 | ||
|
| ||||||
| Voice quality improvement‡ | ||||||
|
| ||||||
| 2 | 0 | 0 | 0.2 | 5 | 2 | 0.08 |
|
| ||||||
| 1 | 3 | 1 | 2 | 5 | ||
|
| ||||||
| 0 | 2 | 4 | 0 | 0 | ||
Wilcoxon signed-rank test for paired observations applied to values measured at 3 and 9 months.
0 = normal, 1 = mild, 2 = moderate.
0 = markedly improved, 1 = improved, 2 = unchanged.
Table 3.
Perceptual voice quality according to the grade, roughness, breathiness, asthenia and strain (GRBAS) scale3
| Item; score* | Group A, no. of patients | Group B, no. of patients | ||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| 3 mo | 9 mo | p value† | 3 mo | 9 mo | p value† | |
| Grade | ||||||
|
| ||||||
| 4 | 0 | 0 | 0.03 | 1 | 0 | 0.01 |
|
| ||||||
| 3 | 0 | 0 | 4 | 2 | ||
|
| ||||||
| 2 | 3 | 0 | 2 | 3 | ||
|
| ||||||
| 1 | 2 | 2 | 0 | 2 | ||
|
| ||||||
| 0 | 0 | 3 | 0 | 0 | ||
|
| ||||||
| Roughness | ||||||
|
| ||||||
| 3 | 0 | 0 | 0.04 | 5 | 4 | 0.3 |
|
| ||||||
| 2 | 2 | 0 | 1 | 2 | ||
|
| ||||||
| 1 | 3 | 3 | 1 | 1 | ||
|
| ||||||
| 0 | 0 | 2 | 0 | 0 | ||
|
| ||||||
| Breathiness | ||||||
|
| ||||||
| 4 | 0 | 0 | 0.04 | 2 | 1 | 0.08 |
|
| ||||||
| 3 | 0 | 0 | 4 | 3 | ||
|
| ||||||
| 2 | 3 | 0 | 1 | 3 | ||
|
| ||||||
| 1 | 2 | 1 | 0 | 0 | ||
|
| ||||||
| 0 | 0 | 4 | 0 | 0 | ||
|
| ||||||
| Asthenia | ||||||
|
| ||||||
| 4 | 0 | 0 | 0.05 | 1 | 0 | 0.2 |
|
| ||||||
| 3 | 0 | 0 | 4 | 5 | ||
|
| ||||||
| 2 | 1 | 0 | 2 | 2 | ||
|
| ||||||
| 1 | 4 | 1 | 0 | 0 | ||
|
| ||||||
| 0 | 0 | 4 | 0 | 0 | ||
|
| ||||||
| Strain | ||||||
|
| ||||||
| 4 | 0 | 0 | 0.04 | 3 | 1 | 0.08 |
|
| ||||||
| 3 | 0 | 0 | 4 | 5 | ||
|
| ||||||
| 2 | 4 | 0 | 0 | 1 | ||
|
| ||||||
| 1 | 1 | 1 | 0 | 0 | ||
|
| ||||||
| 0 | 0 | 4 | 0 | 0 | ||
0 = normal, 1 = mild dysphonia, 2 = moderate dysphonia, 3 = severe dysphonia, 4 = aphonia.
Wilcoxon signed-rank test for paired observations applied to values measured at 3 and 9 months.
Table 4.
Glottal gap rating on direct laryngoscopy
| Score* | Group A, no. of patients | Group B, no. of patients | ||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| 3 mo | 9 mo | p value† | 3 mo | 9 mo | p value† | |
| 4 | 0 | 0 | 0.08 | 1 | 1 | 0.3 |
|
| ||||||
| 3 | 0 | 0 | 2 | 1 | ||
|
| ||||||
| 2 | 3 | 0 | 3 | 4 | ||
|
| ||||||
| 1 | 2 | 5 | 1 | 1 | ||
1 = minimal gap, 2 = moderate gap, 3 = severe gap, 4 = complete glottal incompetence.
Wilcoxon signed-rank test for paired observations applied to values measured at 3 and 9 months.
Discussion
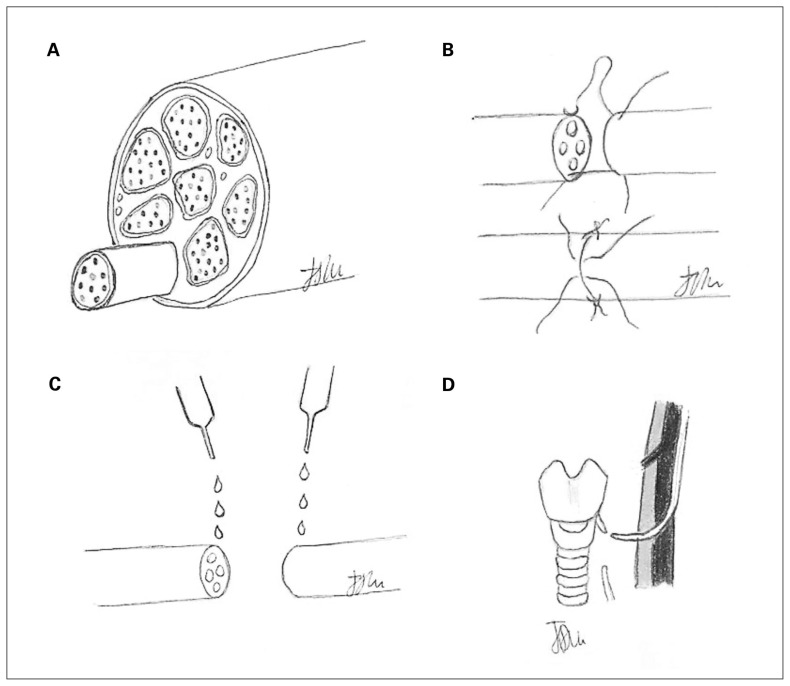
The RLN contains both adductor and abductor fibres, without special segregation.4 After primary repair, regeneration of the nerve occurs in a random way, mixing adductor and abductors fibres, a phenomenon called “misdirected regeneration.”4 Because there are many more adductor fibres than abductor fibres (Fig. 2, A), the reinnervated cords are usually fixed at the median position. For this reason, although normal cord movements are not restored, the reinnervated cord recovers from atrophy, restoring tension during phonation and reducing aspiration. Different methods of peripheral nerve repair such as microsuturing (Fig. 2, B), gluing and grafting have been proposed.4,5 Direct microsuture is preferable when the defect is no longer than 5 mm and the primary repair can be completed without tension.6 Cyanoacrylate glue has also been proposed for nerve repair5,7 (Fig. 2, C) but has been criticized for its toxicity, excessively slow resorption and risk of inflammatory reaction in the perineural tissues.5 When the proximal stump of the RLN cannot be used, grafting should be done using the transverse cervical nerve, supraclavicular nerve or ansa cervicalis (Fig. 2, D).
Fig. 2.
(A) Section of a recurrent laryngeal nerve; the adductors fibres are shown in dark grey, and the abductors fibres, in light grey. (B) Direct microsuture of a transected recurrent laryngeal nerve. (C) Repair of the recurrent laryngeal nerve using cyanoacrylate. (D) Repair of the recurrent laryngeal nerve using the ansa cervicalis.
Limitations
Our study was not randomized. This limitation was unavoidable, as it was ethically impossible to randomly allocate patients to the transected and nontransected RLN groups. In addition, owing to the single-centre design and the low incidence of definitive palsy, the sample was small.
Conclusion
Our results indicate potentially excellent postoperative phonatory function after immediate reconstruction of the transected RLN during thyroid surgery. Larger, multicentre studies are needed to draw reliable conclusions. Endocrine and general surgeons performing thyroid surgery in high-volume centres should know microsurgical techniques.
Acknowledgement
The authors thank Claudia Ventrelli for English revision of the manuscript.
Footnotes
Presented as a poster at the American Head and Neck Society 9th International Conference on Head and Neck Cancer, Seattle, Wash., July 16–20, 2016.
Competing interests: None declared.
Contributors: All authors contributed substantially to the conception, writing and revision of this article and approved the final version for publication.
References
- 1.Spector BC, Netterville JL, Billante C, et al. Quality-of-life assessment in patients with unilateral vocal cord paralysis. Otolaryngol Head Neck Surg. 2001;125:176–82. doi: 10.1067/mhn.2001.117714. [DOI] [PubMed] [Google Scholar]
- 2.Kern KA. Medicolegal analysis of errors in diagnosis and treatment of surgical endocrine disease. Surgery. 1993;114:1167–73. [PubMed] [Google Scholar]
- 3.Koufman JA. Laryngoplasty for vocal cord medialization: an alternative to Teflon. Laryngoscope. 1986;96:726–31. doi: 10.1288/00005537-198607000-00004. [DOI] [PubMed] [Google Scholar]
- 4.Miyauchi A, Inoue H, Tomoda C, et al. Improvement in phonation after reconstruction of the recurrent laryngeal nerve in patients with thyroid cancer invading the nerve. Surgery. 2009;146:1056–62. doi: 10.1016/j.surg.2009.09.018. [DOI] [PubMed] [Google Scholar]
- 5.Wieken K, Angioi-Duprez K, Lim A, et al. Nerve anastomosis with glue: comparative histologic study of fibrin and cyanoacrylate glue. J Reconstr Microsurg. 2003;19:17–20. doi: 10.1055/s-2003-37186. [DOI] [PubMed] [Google Scholar]
- 6.Sanuki T, Yumoto E, Minoda R, et al. The role of immediate recurrent laryngeal nerve reconstruction for thyroid cancer surgery. J Oncol. 2010;2010:846235. doi: 10.1155/2010/846235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Choi BH, Kim BY, Huh JY, et al. Microneural anastomosis using cyanoacrylate adhesives. Int J Oral Maxillofac Surg. 2004;33:777–80. doi: 10.1016/j.ijom.2004.03.006. [DOI] [PubMed] [Google Scholar]