Abstract
Background
Community violence may affect a broad range of health outcomes through physiologic stress responses and changes in health behaviors among residents. However, existing research on the health impacts of community violence suffers from problems with bias.
Methods
We examined the relations of acute changes in community violence with hospital visits and deaths due to stress-responsive diseases (mental, respiratory, and cardiac conditions) in statewide data from California 2005–2013. The community violence exposure was measured as both binary spikes and continuous acute changes. We applied a combined fixed-effects and time-series design that separates the effects of violence from those of community- and individual-level confounders more effectively than past research. Temporal patterning was removed from community violence rates and disease rates in each place using a Kalman smoother, resulting in residual rates. We used linear regression with place fixed-effects to examine within-place associations of acute changes in community violence with residual rates of each outcome, controlling for local time-varying covariates.
Results
We found acute increases in hospital visits and deaths due to anxiety disorders (0.31 per 100,000; 95% Confidence Interval (CI) 0.02,0.59), substance use (0.47 per 100,000; 95%CI 0.14,0.80), asthma (0.56 per 100,000; 95%CI 0.16,0.95), and fatal acute myocardial infarction (0.09 per 100,000; 95%CI 0.00,0.18) co-occurring with violence spikes. The pattern of findings was similar for the exposure of continuous acute violence changes.
Conclusions
Although the associations were small, the identified increases in stress-responsive conditions suggest the possibility of health impacts of acute changes in community violence.
Keywords: Anxiety Disorders, Asthma, California, Hospital Visit, Myocardial Infarction, Residence Characteristics, Violence, Vital Statistics
Introduction
Community violence, which includes injuries due to assault and deaths due to homicide, is a major public health concern.1–3 Research suggests that community violence may affect a broad range of health outcomes. Thus, the scope of public health concern around community violence may extend beyond injury.
Theory and research support an important role of the contextual environment in shaping the health of residents.4–7 Community violence is recognized globally as an important aspect of the contextual environment.2 Residents can experience community violence as direct injury, injury of friends or family, witnessing violence, hearing gunshots, and learning about violence through neighbors or media.8,9 Research indicates that the rate of violence in a community strongly correlates with the frequency of experiences of direct injury and witnessing violence reported by residents.10,11
Furthermore, community violence can lead to stress for residents due to worry about harm to self, family, and friends; it can also lead to alterations in behavior that aim to keep the individual and family safe (e.g., staying inside, closer monitoring of youth, or avoiding parts of communities).12–14 Community violence may affect residents’ health through changes in behaviors such as physical inactivity, unhealthy diets, and substance use, in an effort to stay safe or cope with stress.15,16 Physiologic aspects of the stress response, such as the activation and disruption of the hypothalamic–pituitary–adrenal axis and the alteration or increase in systemic inflammatory response, may also impact the health of residents.17–20
Based on established links between community violence and both physiological and behavioral stress responses, it is reasonable to consider the potential for health impacts of community violence on stress-responsive diseases. Indeed, a variety of studies have found associations between community violence exposure and mental health.21–35 There is also evidence that community violence may exacerbate asthma and increase the risk of heart conditions.36–45 Across conditions, there are behavioral and biologic mechanisms through which exposure to community violence would increase both incidence of disease and acute exacerbations among those with existing disease.
There are major methodologic limitations in research to date on the health effects of community violence. Same-source bias occurs when self-report of both exposure and outcome leads to spurious association due to correlated measurement error in the report (for example, due to optimistic or pessimistic outlook of the respondent). Same-source bias is a concern in studies that rely on self-report of community violence exposure and associate it with self-reported health outcomes.46 In studies that limit same-source bias by using a separate data source for violence exposure, the strong correlation of community violence with other important determinants of health, such as economic, social, and physical features of communities, creates problems with structural confounding.47 Structural confounding occurs when the correlation between the exposure and covariates is too strong to separate the effects. Thus, disentangling the effects of community violence from other determinants of health has posed a major challenge.
Violence varies substantially within communities over short time-frames. These acute changes in community violence offer an opportunity to overcome structural confounding challenges. A comparison of health outcomes at times with higher and lower levels of acute violence in the same geographic area allows each place to serve as its own control. This approach separates the effects of violence from other economic, social, and physical characteristics of places and individuals that remain constant within places over the study period.
In this study, we examined the associations of two forms of acute community violence, specifically binary spikes and continuous acute changes, with hospital visits and deaths due to stress-responsive diseases throughout California, using a combined fixed-effects and time-series design. The diseases included a range of mental, respiratory, and cardiovascular disorders that previous research suggests may be exacerbated by stress. We hypothesized that acute increases in community violence would increase these health outcomes.
METHODS
Data
To capture both fatal and non-fatal occurrences of community violence and of the outcome diseases of interest, we used two statewide data sources for California between 2005 and 2013. For fatal outcomes, we used all mortality records from the California Department of Public Health Office of Vital Statistics. For non-fatal outcomes, we used all emergency department and inpatient hospitalization discharge records from California’s Office of Statewide Health Planning and Development (OSHPD). Events that resulted in fatality in the OSHPD data were removed to avoid double counting. The research was reviewed and approved by the Committees for the Protection of Human Subjects at the University of California, Berkeley and OSHPD. We used US Census Bureau population estimates as denominators, and calculated monthly rates at the census-designated place level (hereafter “place”). Places are single, locally recognized, settled concentrations of residents that are named, but do not have to be legally incorporated.48 We selected places because, as the named cities and towns in which people reside, information about an unusually high level of violence in a month would be expected to be known within the area. These units are also large enough for stable estimation of monthly rates of community violence and the outcomes of interest. Consistent with other research, we examined places with at least 5000 residents to ensure stable rates of both community violence and the outcomes of interest;49 based on this restriction, 91% of California residents (~34 of ~37 million people) residing in 42% of places (631/1,516 places) were included.
Acute Changes in Community Violence
Monthly rates of community violence were calculated as the rate of homicides and assaults, identified by ICD codes as detailed in Table 1. We applied a Kalman smoother to each place-level 108-month series, resulting in residual rates, which retain variability in community violence that was not predictable based on the temporal patterning of the time-series.50 Temporal patterns removed include secular trends, cycles, and seasonality. Residuals from the Kalman smoother model fit constituted the exposure of continuous acute changes in community violence. Binary spikes in community violence were operationalized as place–months with residuals from the Kalman smoother that were greater than two standard deviations above the series. In a simulation study of time-series methods for spike identification, the Kalman smoother performed best in correctly identifying spikes while minimizing false positives (for example: 90.0% sensitivity and 99.4% specificity for spikes of 50% above the average rate; 84.6% sensitivity and 99.1% specificity for spikes of 40% above the average rate).50,51
Table 1.
International Classification of Diseases (ICD) Codes Used to Classify Hospital Discharge and Mortality Records for Measures of Violence and Health Outcomes
| Measure | ICD-9 (hospital discharge records) | ICD-10 (mortality records) |
|---|---|---|
| Homicides and assaults | E960–E969, E970–E977 | X85–X99, Y00–Y09, Y35, U01, U02, Y871 |
| Anxiety disorders | 300 and all 300 subtypes, 308–309 and all 308–309 subtypes | F40–F45 and all F40–F45 subtypes, F48 and all F48 subtypes, F93.0–F93.2 |
| Episodic mood disorders | 296 and all 296 subtypes | F30–F34 and all F30–F34 subtypes, F38–F39 and all F38–F39 subtypes |
| Substance use | 291–292 and all 291–292 subtypes, 303–305 and all 303–305 subtypes | F10–F19 and all F10–F19 subtypes |
| Asthma | 493 and all 493 subtypes | J45 and all J45 subtypes, J46 |
| Chronic obstructive pulmonary disease | 490–492 and all 490–492 subtypes, 494 and all 494 subtypes, 496 | J40–J44 and all J40–J44 subtypes, J47 and all J47 subtypes |
| Acute myocardial infarction | 410 and all 410 subtypes | I21–I22 and all I21–I22 subtypes |
| Heart failure | 428 and all 428 subtypes | I50 and all I50 subtypes |
Health Outcomes
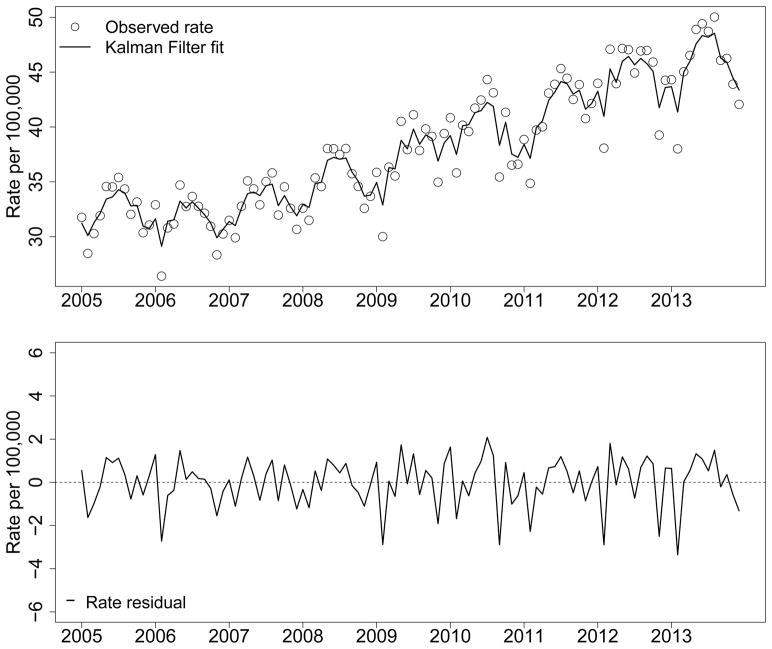
Monthly rates of the health outcomes of anxiety disorders, episodic mood disorders, substance use, asthma, chronic obstructive pulmonary disease (COPD), acute myocardial infarction (MI), and heart failure were calculated based on International Classification of Diseases (ICD) codes as detailed in Table 1. For each outcome group, we examined all events (fatal and non-fatal combined) and fatal events alone when sufficient numbers of fatal outcomes occurred for model convergence. As with the community violence exposure, predictable temporal patterning was removed from disease rates in each place with a Kalman smoother.50 Figure 1 presents an example of substance use rates with the Kalman smoother fit and the residual rates after processing.
Figure 1.
Rates of Hospital Visits and Deaths Due to Substance Use to Illustrate Kalman Smoother Fit and Residuals, Los Angeles 2005 – 2013
Design
In a combined fixed-effects and time-series design,52,53 within each place we compared a) outcomes in months with a violence spike to the outcomes in months without a spike, and b) outcome changes associated with continuous acute violence changes across months. Comparing outcomes in the same geographic area allowed us to separate the effects of the acute violence from the effects of other economic, social and physical characteristics of places and individuals that are constant over this time period within a place. However, shared temporal patterning in the acute violence and outcomes remains a concern. Thus, for all analyses dependent variables were Kalman smoother residuals of the outcome rates, so that we only examine variability in the outcomes that was not predictable based on the temporal patterning of the time-series.50 This approach removes local temporal patterning specific to each place, and thus provides control for confounding by local variables with predictable patterning.54
Analysis
Analyses were conducted with linear regression models with fixed-effects on place and robust sandwich standard errors.55 We adjusted for local monthly average precipitation, average temperature, unemployment, and civil unrest events to control for confounding by covariates with unpredictable temporal patterning that change over short time frames and are determinants of both community violence and health outcomes.56,57 Additionally, we controlled for local annual measures of poverty, unemployment, marital status, racial/ethnic composition, and educational attainment that are strongly predictive of violence (see eAppendix 1 for covariate details). We also conducted a sensitivity analysis in which we identified and omitted places from the analysis for a given outcome if there was evidence of persistent autocorrelation in the time-series. (See eTable 2, eAppendix 2 for sensitivity analysis results). All analyses were conducted in R version 3.2.1 (see eAppendix 4 for code).
RESULTS
Across the 631 places over 108 months (68,148 place-months of observation), there were 2,401 violence spikes, and all but 6 places experienced at least one spike. For the continuous violence measure and each outcome, the distribution of the total cases, average monthly rates and monthly rate residuals after Kalman smoother processing across the place–months of analysis can be found in Table 2.
Table 2.
Description of Health Outcomes Across All Place-Months of Analysis, California 2005–2013
| Condition | Outcome | Total cases | Rate b | Rate residualsc | |
|---|---|---|---|---|---|
| Mean | IQR | IQR | |||
| Community violence | Combined fatal and non-fatal | 1,124,382 | 27.2 | 13.08, 37.08 | −3.68, 3.00 |
| Anxiety disordersa | Combined fatal and non-fatal | 922,064 | 25.5 | 14.40, 33.38 | −3.65, 3.02 |
| Episodic mood disordersa | Combined fatal and non-fatal | 973,049 | 23.85 | 12.93, 32.35 | −3.64, 2.85 |
| Substance use | Combined fatal and non-fatal | 1,255,735 | 32.32 | 18.432, 42.114 | −4.21, 3.49 |
| Fatal only | 8,338 | 0.247 | 0, 0 | −0.14, −0.03 | |
| Asthma | Combined fatal and non-fatal | 1,494,217 | 38.06 | 18.73, 51.30 | −5.06, 4.08 |
| Fatal only | 3,409 | 0.09 | 0, 0 | −0.06, 0.00 | |
| Chronic obstructive pulmonary disease | Combined fatal and non-fatal | 1,299,122 | 38.08 | 18.38, 49.16 | −4.99, 3.82 |
| Fatal only | 99,232 | 3.23 | 0, 4.50 | −1.30, 0.66 | |
| Acute myocardial infarction | Combined fatal and non-fatal | 538,233 | 15.86 | 7.96, 20.80 | −3.15, 2.35 |
| Fatal only | 92,961 | 2.68 | 0, 3.79 | −1.15, 0.53 | |
| Heart failure | Combined fatal and non-fatal | 828,778 | 22.63 | 12.72, 29.84 | −3.49, 2.85 |
| Fatal only | 37,283 | 1.15 | 0, 0.98 | −0.58, 0.00 | |
IQR: interquartile range
There were too few cases of these fatal outcomes to examine them separately (fatal anxiety disorder cases: 46, fatal episodic mood disorder cases: 322)
Rates are per 100,000 population
Rate residuals all have a mean of zero
In the main analysis models that examined binary violence spikes in relation to residual outcome rates, including fixed-effects on place and control for time varying local covariates (Table 3), we found acute increases in deaths and hospital visits due to anxiety disorders (0.31 per 100,000 increase (95% Confidence Interval (CI) 0.02, 0.59)), substance use (0.47 per 100,000 increase (95% CI 0.14, 0.80)), asthma (0.56 per 100,000 increase (95% CI 0.16, 0.95)), and fatal acute MI (0.09 per 100,000 increase (95% CI 0.00, 0.18)) co-occurring with violence spikes. In the models that examined continuous acute violence in relation to residual outcome rates (Table 3), there was a similar pattern of results with acute increases in deaths and hospital visits due to anxiety disorders (0.14 per 100,000 increase (95% CI 0.04, 0.24)), substance use (0.35 per 100,000 increase (95% CI 0.24, 0.46)), and asthma (0.16 per 100,000 increase (95% CI 0.03, 0.30)) for a 10 per 100,000 difference in acute violence. Continuous acute violence was not associated with fatal acute MI. Overall, there were no indications of changes in deaths and hospital visits due to episodic mood disorders, COPD, or heart failure associated with acute community violence.
Table 3.
Relationships of Acute Violence Changes with Health Outcomes, Estimated With Linear Regression Analysis of Monthly Residual Outcome Rates With Fixed-effects on Place, California 2005–2013
| Residual rate differences associated with violence spikes b | Residual rate differences associated with acute violence increases b, c | ||||
|---|---|---|---|---|---|
|
| |||||
| Condition | Outcome | RD d | 95% CI | RD d | 95% CI |
| Anxiety disorders a | Combined fatal and non-fatal | 0.31 | 0.02, 0.59 | 0.14 | 0.04, 0.24 |
| Episodic mood disorders a | Combined fatal and non-fatal | 0.07 | −0.2, 0.35 | 0.07 | −0.02, 0.17 |
| Substance use | Combined fatal and non-fatal | 0.47 | 0.14, 0.80 | 0.35 | 0.24, 0.46 |
| Fatal only | 0.00 | −0.02, 0.03 | 0.00 | −0.01, 0.01 | |
| Asthma | Combined fatal and non-fatal | 0.56 | 0.16, 0.95 | 0.16 | 0.03, 0.30 |
| Fatal only | 0.00 | −0.02, 0.01 | 0.00 | 0.00, 0.01 | |
| Chronic obstructive pulmonary disease | Combined fatal and non-fatal | 0.02 | −0.35, 0.38 | −0.10 | −0.25, 0.04 |
| Fatal only | 0.00 | −0.10, 0.10 | −0.02 | −0.05, 0.02 | |
| Acute myocardial infarction | Combined fatal and non-fatal | 0.08 | −0.16, 0.31 | 0.03 | −0.05, 0.11 |
| Fatal only | 0.09 | 0.00, 0.18 | 0.01 | −0.02, 0.04 | |
| Heart failure | Combined fatal and non-fatal | 0.23 | −0.04, 0.49 | 0.00 | −0.10, 0.09 |
| Fatal only | −0.01 | −0.07, 0.04 | −0.01 | −0.03, 0.01 | |
RD: Rate Difference; 95%CI: 95% Confidence Interval
There were too few cases of these fatal outcomes to examine them separately (fatal anxiety disorder cases: 46, fatal episodic mood disorder cases: 322)
Residuals based on fitting a Kalman smoother to the outcome rates in each place to remove predictable temporal patterning
RD corresponding to 10 per 100,000 increase in acute violence residual
Controlled for local monthly average precipitation, average temperature, unemployment, and civil unrest events; controlled for local annual measures of poverty, unemployment, marital status, racial/ethnic composition, and educational attainment
In the sensitivity analysis, we first examined residual autocorrelation by outcome and for the exposure of community violence (eAppendix 2, eTable 1). In general, the degree of residual autocorrelation was low; however, autocorrelation tended to persist in the fatal asthma (20.9% of places) and fatal substance use (9.2% of places) time-series. For all other outcomes and the community violence exposure autocorrelation was minimal, with a few places for some outcomes in which autocorrelation persisted (range from 0% to 1.3% of places). In models that omitted places from the analysis for a given outcome if there was evidence of persistent autocorrelation in the time-series the results were unchanged (eAppendix 2, eTable 2).
DISCUSSION
Overall, we found acute relations of community violence with anxiety disorders, substance use, asthma, and fatal acute MI. Although studies have documented correlations of community violence with mental health and substance use outcomes,21–35 our design provides stronger evidence by avoiding same-source bias and minimizing structural confounding. The findings are also consistent with the small set of studies that has examined the relations of community violence with asthma and cardiac events.36–45
Our exposures were acute changes in community violence and thus, do not capture any effects of chronic exposure to community violence on the outcomes. The combined time-series and fixed-effects approach removes any effect of the average rate of violence and isolates the effect of acute violence changes. Chronic exposure to violence is also a stressor and expected to have important impacts on health, but these effects are more challenging to separate analytically from other community characteristics.58 Thus, differences between our results and studies of violence rates may be due to our examination of only acute forms of violence.
There are several considerations for interpretation of the results with respect to the outcomes. Increases in cause-specific hospital visits and deaths may be composed more of exacerbations in underlying conditions than of incident outcomes. Furthermore, the outcomes include only events that are sufficiently serious to result in an emergency department visit, hospitalization, or death. Thus, we do not have data on less severe events or exacerbations of symptoms that influence health and wellbeing, but do not necessitate a visit to the hospital or result in a death and may underestimate the overall burden associated with acute violence. However, we have captured the most severe and costly events – a subgroup of interest and concern. While health care coverage varies and may affect use of the hospital system,59 this would only affect our results if temporal, within-place changes in health care coverage coincide with the acute violence changes during the study period.
We examined cities and towns as the geographical units of interest in this study. While we expect that residents would be aware of violent events within this geography, it is possible that smaller areas would better capture the geographical scope in which violent events would generate concern or impact residents, particularly in larger cities. In general, results of geographic analyses may be sensitive to the choice of geographic unit, a problem that has been discussed as the modifiable areal unit problem.60
Among the substance use and mental disorders, acute violence was related to increases in deaths and hospital visits due to anxiety disorders and substance use, but not mood disorders. One explanation may be that exposure to traumas is more important for anxiety disorders, such as post-traumatic stress disorder, whereas determinants of mood disorders such a depression relate more to personal loss and supports available in the aftermath of the loss.61,62 It is conceivable that an acute increase in violence could cause traumatic exposure for a broader population within a city or town, manifesting in increased hospital visits for anxiety and substance use. In contrast, acute violence would lead to personal loss for a much smaller subset of the population and thus increase in mood disorder-related hospital visits would be expected to be smaller and more challenging to detect at the population level.
The relationship of acute violence with cardiopulmonary outcomes was consistent for asthma, but varied by form of acute violence for fatal MI. Research supports a clear role for chronic stress in the development and progression of cardiovascular diseases.42 Acute stressors may induce acute cardiac events in those already physiologically vulnerable.42,43 Although any explanation of inconsistency in findings is post hoc, it is worth noting that in research on population stressors that has found increases in acute cardiac events, the stressors have generally been of larger magnitude and/or of broader impact, specifically earthquakes, wars, and terrorist attacks.43 Thus, it is plausible that acute changes in community violence had insufficient breadth, duration, and/or strength of impact to generate large enough effects on acute cardiac events for consistent detection in our analyses. Exacerbations of asthma, in contrast, are more frequent, and occurrence has been related to far less extreme acute stressors, such as exams.20
The magnitudes of association for the relations of violence spikes with the outcomes were small. With respect to the variability in the outcome residuals, the associations corresponded to between 2% and 6% of a standard deviation. As an example, statewide the associations corresponded to an additional 120 anxiety, 183 substance use, and 218 asthma hospital visits and deaths, and 35 fatal MIs in a month with a violence spike. However, a few considerations provide context for these magnitudes. These associations only capture acute increases in the most severe health events and thus may underestimate the overall burden associated with violence spikes. Furthermore, the associations only capture the changes in health outcomes associated with acute violence, not with the overall exposure to community violence. We would anticipate that the health outcome changes associated with the overall exposure to community violence to be much greater than those associated with acute spikes. However, as discussed above, we have approached this analysis with the aim of minimizing the types of confounding that plague past work on community violence and health. Thus, we viewed this as a test of whether, despite these strong control measures, a signal of a relation between acute violence and these health outcomes could be detected. While a worthwhile endeavor to undertake in future work, capturing the true magnitude of the relation of community violence with health would require leveraging the full range of variability in violence, yet also controlling for strong structural confounders.
We examined outcomes in the same month as the violence spike because we hypothesized acute effects, but this raises a potential concern about the directionality of the associations. It is unlikely that increases in asthma or cardiac events would cause a violence spike. It is possible that increases in mental disorder or substance use could increase violence, since individuals who have a certain mental disorders or are using substances have increased risk of violent behavior.63 However, at the population level mental disorder is a very minor contributor to interpersonal violence (population attributable risk percent (PAR%) estimate of 4%), and the anxiety and episodic mood disorder outcomes examined here do not include personality disorders which are most strongly associated with perpetration of violence.64 Substance use is a more sizable contributor to perpetration of interpersonal violence at the population level than mental disorder (PAR% estimates range from 20–25%),64 and thus the relation documented may represent effects of violence on substance use as well as effects of substance use on violence.
The largest threat to this analysis would be a cause of both acute violence changes and the health outcomes that varies unpredictably over short time spans within place and has not been controlled. However, we have identified and controlled for numerous common causes of acute changes in violence and the health outcomes that may not follow predictable patterns. In particular, we controlled time-varying socioeconomic, weather, civil unrest, and demographic variables at the local level. Nonetheless, residual confounding is always a concern in observational studies, particularly when associations are small.
Our approach assumes that past acute violence only affects future health outcomes within a place through more proximal acute violence, and that past health outcomes within a place do not affect future acute violence changes.65 In considering the first part of this assumption, while the underlying health conditions likely developed over a long period and may have been affected by prior acute violence, we are examining only acute changes in manifestations of these health conditions which are far less likely to be affected by prior acute violence. We evaluated the second part of this assumption by examining the relations of the health outcomes with subsequent acute violence changes within a place, and we found largely null associations (see eAppendix 3). This suggests that reliance on this assumption is reasonable in our study.
Conclusion
Overall, our findings suggest that violence may affect health in the community more broadly, although magnitudes of associations were small. By examining acute changes in violence, using a design that controls for time-invariant confounders and incorporates careful control of predictable temporal patterning and observed factors that vary within place over time in ways that may not be predictable, we have strengthened the evidence for these potential health impacts.
Supplementary Material
Acknowledgments
Source of Funding
The results reported herein correspond to the aims of grant DP2HD080350 to investigator Jennifer Ahern from the National Institutes of Health. This work was also supported by pilot grant funds from the Robert Wood Johnson Health and Society Scholars Program and the University of California, Berkeley Committee on Research. Analyses, interpretations, and conclusions are those of the authors and not those of the California Department of Public Health or the National Institutes of Health.
Footnotes
Conflicts of Interest
None declared
Data and Code
The data are available from the State of California upon request for research purposes. We do not have the authority to share the data. Analysis code, in the program R, is provided in eAppendix 4 to facilitate replication or building upon our research.
References
- 1.US Department of Justice; Bureau of Labor Statistics. Homicide Trends in the United States, 1980–2008. 2011. [Google Scholar]
- 2.Krug EG, Dahlberg LL, Mercy JA, Zwi AB, Lozano R, editors. World report on violence and health. Geneva: World Health Organization; 2002. [Google Scholar]
- 3.Rutherford A, Zwi AB, Grove NJ, Butchart A. Violence: a priority for public health? (part 2) Journal of Epidemiology and Community Health. 2007;61(9):764–70. doi: 10.1136/jech.2006.049072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bronfenbrenner U. The Ecology of Human Development: Experiments by Nature and Design. Cambridge, MA: Harvard University Press; 1979. [Google Scholar]
- 5.Cassel J. The contribution of the social environment to host resistance: the Fourth Wade Hampton Frost Lecture. American Journal of Epidemiology. 1976;104(2):107–23. doi: 10.1093/oxfordjournals.aje.a112281. [DOI] [PubMed] [Google Scholar]
- 6.Kaplan GA, Everson SA, Lynch JW. The Contribution of Social and Behavioral Research to an Understanding of the Distribution of Disease: A Multilevel Approach. In: Smedley BD, Syme SL, editors. Promoting Health: Intervention Strategies from Social and Behavioral Research. Washington, D.C: National Academy Press; 2000. [Google Scholar]
- 7.Krieger N. Theories for social epidemiology in the 21st century: an ecosocial perspective. International Journal of Epidemiology. 2001;30(4):668–77. doi: 10.1093/ije/30.4.668. [DOI] [PubMed] [Google Scholar]
- 8.Suglia SF, Ryan L, Wright RJ. Creation of a community violence exposure scale: accounting for what, who, where, and how often. Journal of Traumatic Stress. 2008;21(5):479–86. doi: 10.1002/jts.20362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Finklehor D, Turner H, Ormrod R, Hamby S, Kracke K. Children’s exposure to violence: a comprehensive national survey. Juvenile Justice Bulletin. 2009:1–11. [Google Scholar]
- 10.Zimmerman GM, Messner SF. Individual, family background, and contextual explanations of racial and ethnic disparities in youths’ exposure to violence. American Journal of Public Health. 2013;103(3):435–42. doi: 10.2105/AJPH.2012.300931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hartinger-Saunders RM, Rine CM, Nochajski T, Wieczorek W. Neighborhood Crime and Perception of Safety as Predictors of Victimization and Offending Among Youth: A Call for Macro-Level Prevention and Intervention Models. Child Youth Serv Rev. 2012;34(9):1966–1973. doi: 10.1016/j.childyouth.2012.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wolfer TA. Coping with chronic community violence: the variety and implications of women’s efforts. Violence Vict. 2000;15(3):283–301. [PubMed] [Google Scholar]
- 13.Voisin D, Berringer K, Takahashi L, Burr S, Kuhnen J. No Safe Havens: Protective Parenting Strategies for African American Youth Living in Violent Communities. Violence Vict. 2016;31(3):523–36. doi: 10.1891/0886-6708.VV-D-14-00056. [DOI] [PubMed] [Google Scholar]
- 14.Horowitz K, McKay M, Marshall R. Community violence and urban families: experiences, effects, and directions for intervention. American Journal of Orthopsychiatry. 2005;75(3):356–68. doi: 10.1037/0002-9432.75.3.356. [DOI] [PubMed] [Google Scholar]
- 15.Acierno RA, Kilpatrick DG, Resnick HS, Saunders BE, Best CL. Violent assault, posttraumatic stress disorder, and depression. Risk factors for cigarette use among adult women. Behavior Modification. 1996;20(4):363–84. doi: 10.1177/01454455960204001. [DOI] [PubMed] [Google Scholar]
- 16.Sanders-Phillips K. The ecology of urban violence: its relationship to health promotion behaviors in low-income black and Latino communities. American Journal of Health Promotion. 1996;10(4):308–17. doi: 10.4278/0890-1171-10.4.308. [DOI] [PubMed] [Google Scholar]
- 17.Hobel CJ, Goldstein A, Barrett ES. Psychosocial stress and pregnancy outcome. Clinical Obstetrics and Gynecology. 2008;51(2):333–348. doi: 10.1097/GRF.0b013e31816f2709. [DOI] [PubMed] [Google Scholar]
- 18.McEwen BS. Protective and damaging effects of stress mediators. New England Journal of Medicine. 1998;338(3):171–179. doi: 10.1056/NEJM199801153380307. [DOI] [PubMed] [Google Scholar]
- 19.Wadhwa PD. Psychoneuroendocrine processes in human pregnancy influence fetal development and health. Psychoneuroendocrinology. 2005;30(8):724–743. doi: 10.1016/j.psyneuen.2005.02.004. [DOI] [PubMed] [Google Scholar]
- 20.Chen E, Miller GE. Stress and inflammation in exacerbations of asthma. Brain Behav Immun. 2007;21(8):993–9. doi: 10.1016/j.bbi.2007.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Clark C, Ryan L, Kawachi I, Canner MJ, Berkman L, Wright RJ. Witnessing community violence in residential neighborhoods: a mental health hazard for urban women. Journal of Urban Health. 2008;85(1):22–38. doi: 10.1007/s11524-007-9229-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fitzpatrick KM, Piko BF, Wright DR, LaGory M. Depressive symptomatology, exposure to violence, and the role of social capital among African American adolescents. American Journal of Orthopsychiatry. 2005;75(2):262–74. doi: 10.1037/0002-9432.75.2.262. [DOI] [PubMed] [Google Scholar]
- 23.Boxer P, Sloan-Power E, Piza E, Schappell A. Using police data to measure children’s exposure to neighborhood violence: a new method for evaluating relations between exposure and mental health. Violence Vict. 2014;29(1):24–33. doi: 10.1891/0886-6708.vv-d-12-00155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Barcelona de Mendoza V, Harville EW, Savage J, Giarratano G. Experiences of Intimate Partner and Neighborhood Violence and Their Association With Mental Health in Pregnant Women. J Interpers Violence. 2015 doi: 10.1177/0886260515613346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shiue I. Neighborhood epidemiological monitoring and adult mental health: European Quality of Life Survey, 2007–2012. Environ Sci Pollut Res Int. 2015;22(8):6095–103. doi: 10.1007/s11356-014-3818-3. [DOI] [PubMed] [Google Scholar]
- 26.Polling C, Khondoker M, Hatch SL, Hotopf M team SEs. Influence of perceived and actual neighbourhood disorder on common mental illness. Soc Psychiatry Psychiatr Epidemiol. 2014;49(6):889–901. doi: 10.1007/s00127-013-0813-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wilson-Genderson M, Pruchno R. Effects of neighborhood violence and perceptions of neighborhood safety on depressive symptoms of older adults. Social Science and Medicine. 2013;85:43–9. doi: 10.1016/j.socscimed.2013.02.028. [DOI] [PubMed] [Google Scholar]
- 28.Mair C, Diez Roux AV, Golden SH, Rapp S, Seeman T, Shea S. Change in neighborhood environments and depressive symptoms in New York City: the Multi-Ethnic Study of Atherosclerosis. Health and Place. 2015;32:93–8. doi: 10.1016/j.healthplace.2015.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Goldman-Mellor S, Margerison-Zilko C, Allen K, Cerda M. Perceived and Objectively-Measured Neighborhood Violence and Adolescent Psychological Distress. Journal of Urban Health. 2016;93(5):758–769. doi: 10.1007/s11524-016-0079-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Astell-Burt T, Feng X, Kolt GS, Jalaludin B. Does rising crime lead to increasing distress? Longitudinal analysis of a natural experiment with dynamic objective neighbourhood measures. Social Science and Medicine. 2015;138:68–73. doi: 10.1016/j.socscimed.2015.05.014. [DOI] [PubMed] [Google Scholar]
- 31.Rogers JD, Ramaswamy M, Cheng CI, Richter K, Kelly PJ. Perceptions of neighborhood social environment and drug dependence among incarcerated women and men: a cross-sectional analysis. Subst Abuse Treat Prev Policy. 2012;7:39. doi: 10.1186/1747-597X-7-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Curry A, Latkin C, Davey-Rothwell M. Pathways to depression: the impact of neighborhood violent crime on inner-city residents in Baltimore, Maryland, USA. Social Science and Medicine. 2008;67(1):23–30. doi: 10.1016/j.socscimed.2008.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lambert SF, Brown TL, Phillips CM, Ialongo NS. The relationship between perceptions of neighborhood characteristics and substance use among urban African American adolescents. American Journal of Community Psychology. 2004;34(3–4):205–18. doi: 10.1007/s10464-004-7415-3. [DOI] [PubMed] [Google Scholar]
- 34.Fagan AA, Wright EM, Pinchevsky GM. The protective effects of neighborhood collective efficacy on adolescent substance use and violence following exposure to violence. J Youth Adolesc. 2014;43(9):1498–512. doi: 10.1007/s10964-013-0049-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Brady SS. Lifetime community violence exposure and health risk behavior among young adults in college. Journal of Adolescent Health. 2006;39(4):610–3. doi: 10.1016/j.jadohealth.2006.03.007. [DOI] [PubMed] [Google Scholar]
- 36.Apter AJ, Garcia LA, Boyd RC, Wang X, Bogen DK, Ten Have T. Exposure to community violence is associated with asthma hospitalizations and emergency department visits. Journal of Allergy and Clinical Immunology. 2010;126(3):552–7. doi: 10.1016/j.jaci.2010.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sternthal MJ, Jun HJ, Earls F, Wright RJ. Community violence and urban childhood asthma: a multilevel analysis. Eur Respir J. 2010;36(6):1400–9. doi: 10.1183/09031936.00003010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Walker J, Lewis-Land C, Kub J, Tsoukleris M, Butz A. The effect of violence on asthma: are our children facing a double-edged sword? J Community Health. 2008;33(6):384–8. doi: 10.1007/s10900-008-9113-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wilson DK, Kliewer W, Teasley N, Plybon L, Sica DA. Violence exposure, catecholamine excretion, and blood pressure nondipping status in African American male versus female adolescents. Psychosom Med. 2002;64(6):906–15. doi: 10.1097/01.psy.0000024234.11538.d3. [DOI] [PubMed] [Google Scholar]
- 40.Hering D, Lachowska K, Schlaich M. Role of the Sympathetic Nervous System in Stress-Mediated Cardiovascular Disease. Curr Hypertens Rep. 2015;17(10):80. doi: 10.1007/s11906-015-0594-5. [DOI] [PubMed] [Google Scholar]
- 41.Rosenberg SL, Miller GE, Brehm JM, Celedon JC. Stress and asthma: novel insights on genetic, epigenetic, and immunologic mechanisms. J Allergy Clin Immunol. 2014;134(5):1009–15. doi: 10.1016/j.jaci.2014.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lagraauw HM, Kuiper J, Bot I. Acute and chronic psychological stress as risk factors for cardiovascular disease: Insights gained from epidemiological, clinical and experimental studies. Brain Behav Immun. 2015;50:18–30. doi: 10.1016/j.bbi.2015.08.007. [DOI] [PubMed] [Google Scholar]
- 43.Steptoe A, Brydon L. Emotional triggering of cardiac events. Neurosci Biobehav Rev. 2009;33(2):63–70. doi: 10.1016/j.neubiorev.2008.04.010. [DOI] [PubMed] [Google Scholar]
- 44.Sundquist K, Theobald H, Yang M, Li X, Johansson SE, Sundquist J. Neighborhood violent crime and unemployment increase the risk of coronary heart disease: a multilevel study in an urban setting. Social Science and Medicine. 2006;62(8):2061–71. doi: 10.1016/j.socscimed.2005.08.051. [DOI] [PubMed] [Google Scholar]
- 45.Lee EH, Bruckner TA. Threats to security and ischaemic heart disease deaths: the case of homicides in Mexico. International Journal of Epidemiology. 2017;46(1):173–179. doi: 10.1093/ije/dyw110. [DOI] [PubMed] [Google Scholar]
- 46.Kamphuis CB, Mackenbach JP, Giskes K, Huisman M, Brug J, van Lenthe FJ. Why do poor people perceive poor neighbourhoods? The role of objective neighbourhood features and psychosocial factors. Health and Place. 2010;16(4):744–54. doi: 10.1016/j.healthplace.2010.03.006. [DOI] [PubMed] [Google Scholar]
- 47.Oakes JM. Commentary: advancing neighbourhood-effects research--selection, inferential support, and structural confounding. International Journal of Epidemiology. 2006;35(3):643–7. doi: 10.1093/ije/dyl054. [DOI] [PubMed] [Google Scholar]
- 48.Bureau of the Census. Census Designated Place (CDP) Program for the 2010 Census - Final Criteria. Federal Register. 2008;73(30):8269–73. [Google Scholar]
- 49.Chauhan P, Cerda M, Messner SF, Tracy M, Tardiff K, Galea S. Race/Ethnic-Specific Homicide Rates in New York City: Evaluating the Impact of Broken Windows Policing and Crack Cocaine Markets. Homicide Stud. 2011;15(3):268–290. doi: 10.1177/1088767911416917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Durbin J, Koopman SJ. Time series analysis by state space methods. 2. Oxford: Oxford University Press; 2012. Oxford statistical science series. [Google Scholar]
- 51.Goin DE, Jewell N, Brillinger D, Ahern J. Identification of spikes in time series. Under Review. 2017 [Google Scholar]
- 52.Catalano R, Ahern J, Bruckner T. Estimating the health effects of macrosocial shocks: a collaborative approach. In: Galea S, editor. Macrosocial Determinants of Population Health. New York: Springer; 2007. [Google Scholar]
- 53.Bhaskaran K, Gasparrini A, Hajat S, Smeeth L, Armstrong B. Time series regression studies in environmental epidemiology. International Journal of Epidemiology. 2013;42(4):1187–95. doi: 10.1093/ije/dyt092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wooldridge JM. Econometric analysis of cross section and panel data. 2. Cambridge, Mass: MIT Press; 2010. [Google Scholar]
- 55.White H. A Heteroskedasticity-Consistent Covariance-Matrix Estimator and a Direct Test for Heteroskedasticity. Econometrica. 1980;48(4):817–838. [Google Scholar]
- 56.Center WRC. WestMap Climate Analysis, PRISM Climate Mapping Program. 2016 http://www.cefa.dri.edu/Westmap/
- 57.Bureau of Labor Statistics. US Department of Labor. Local Area Unemployment Statistics: Monthly Unemployment Rates. 2015 https://data.bls.gov/cgi-bin/srgate.
- 58.Glymour MM, Rudolph KE. Causal inference challenges in social epidemiology: Bias, specificity, and imagination. Social Science and Medicine. 2016;166:258–65. doi: 10.1016/j.socscimed.2016.07.045. [DOI] [PubMed] [Google Scholar]
- 59.Radley DC, Schoen C. Geographic variation in access to care--the relationship with quality. The New England Journal of Medicine. 2012;367(1):3–6. doi: 10.1056/NEJMp1204516. [DOI] [PubMed] [Google Scholar]
- 60.Fotheringham AS, Rogerson P. The SAGE handbook of spatial analysis. Los Angeles ; London: SAGE Publications; 2009. [Google Scholar]
- 61.Galea S, Ahern J, Resnick H, Kilpatrick D, Bucuvalas M, Gold J, Vlahov D. Psychological sequelae of the September 11 terrorsit attacks in Manhattan, New York City. The New England Journal of Medicine. 2002;346(13):982–987. doi: 10.1056/NEJMsa013404. [DOI] [PubMed] [Google Scholar]
- 62.Roberts B, Ocaka KF, Browne J, Oyok T, Sondorp E. Factors associated with post-traumatic stress disorder and depression amongst internally displaced persons in northern Uganda. BMC Psychiatry. 2008;8:38. doi: 10.1186/1471-244X-8-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Harford TC, Yi HY, Grant BF. Other- and self-directed forms of violence and their relationships to DSM-IV substance use and other psychiatric disorders in a national survey of adults. Compr Psychiatry. 2013;54(7):731–9. doi: 10.1016/j.comppsych.2013.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Swanson JW, McGinty EE, Fazel S, Mays VM. Mental illness and reduction of gun violence and suicide: bringing epidemiologic research to policy. Annals of Epidemiology. 2015;25(5):366–76. doi: 10.1016/j.annepidem.2014.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Imai K, Kim IS. Working Paper. Princeton University; 2016. When should we use linear fixed effects regression for causal inference with longitudinal data? [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.