Abstract
Objective
To determine if positive emotion modifies the relationship between cognitive impairment and Activities of Daily Living disability status over 10 years in Mexican American adults aged 75 years and older.
Methods
A retrospective cohort design using data from the Hispanic Established Populations for the Epidemiologic Studies of the Elderly. 2,674 participants aged 75 years and older were included and followed over 10 years. Cognition was measured using the mini-mental state examination, positive emotion was measured using four questions from the Center for Epidemiologic Studies Depression Scale, and disability was measured using 7 Activities of Daily Living items. A series of Generalized Estimating Equations models were used, with the initial analysis including those with disability at baseline and subsequent analyses excluding disability at baseline.
Results
Positive emotion and cognitive impairment consistently decreased and increased risk for Activities of Daily Living disability, respectively. Positive emotion was a significant modifier in the cross-sectional analysis, and was not a statistically significant modifier in the longitudinal or predictive series analysis.
Conclusion
Positive emotion and cognitive impairment differentially affect the risk of developing Activities of Daily Living disability. Further research is needed to explore the interaction of positive emotion and cognitive impairment, and to identify appropriate interventions that address the specific cognitive and emotional needs of older Mexican Americans.
Keywords: Positive Emotion, Cognition, Activities of Daily Living, Hispanic, Older Adults
Introduction
Over the past few decades there has been a proliferation of research examining the role of emotions on physical health and recovery. Positive emotion is associated with increased longevity and better health outcomes for both healthy and diseased populations (1–4). Further benefits of positive emotion include enhanced pain management and decreased anxiety, cortisol output, hypertension, and risk of disability (3,5,6). Many of the observed benefits for positive emotion on health outcomes have been found among older adults (5,6). In a study by Ostir et al, each unit increase in positive emotion among older adults significantly reduced the risk of frailty by 3% (7) and in a study by Xu and Roberts, positive emotion predicted a 10% lower risk of mortality in adults aged 55 years and older (8). These findings are important given the current aging shift in the United States.
Due to improvements in healthcare, there is an increase in the number of adults aged 65 years and older (9). It is projected that by the year 2030, the United States will have 74 million older adults (10). The older adult population of the United States is also becoming increasingly diverse. The number of older Hispanic adults is expected to increase from nearly 300,000 older adults in 2012 to projections of 800,000 in 2030 and 1.5 million in 2050 (11). This projected increase makes it important to gain a better understanding of the unique health needs of the older Hispanic population.
The majority of Hispanics living in the United States are of Mexican origin (12). Mexican Americans have a higher prevalence of impaired cognition, diabetes, cardiometabolic conditions, infectious diseases, and obesity compared to non-Hispanic White Americans (7,13–15). Furthermore, Mexican Americans are more likely to live in poverty and less likely to have healthcare access than non-Hispanic Whites (7,16,17). These factors lead to Mexican Americans being susceptible to poor physical functioning and disability (18,19).
Factors affecting the progression of disability among older Mexican Americans must be identified. Studies have demonstrated the role of positive emotion in ameliorating the risk of incident disability among older Mexican Americans with arthritis, despite arthritis being a significant risk factor for disability (5). Additionally, cognitive impairment is associated with incident disability in older Hispanic adults (20–22). Raji and colleagues (20) found older Mexican Americans with impaired cognition had a 58% higher chance for disability compared to those with normal cognition.
A previous study found that positive emotion can modify the relationship between cognition and physical function of the lower body (23). However, there are no studies investigating how positive emotion may interact with cognition to modify the relationship with disability in the general population nor among older Mexican Americans. We examined the interaction between positive emotion and cognition on risk of incident disability in a large sample of community-dwelling older Mexican Americans. Positive emotion was hypothesized to modify the relationship between cognition and incident disability in activities of daily living. The findings of this study will provide important evidence to guide future research and clinical decisions to ameliorate the risk of disability.
Methods
Population
This study used data from the Hispanic Established Populations for the Epidemiologic Studies of the Elderly. The Hispanic Established Populations for the Epidemiologic Studies of the Elderly is a multistage, stratified sample representative of community-dwelling Mexican-American elderly, at least 65 years of age, and living in Arizona, California, Colorado, New Mexico, and Texas. The data were collected over 8 waves from 1993/94 to 2012/13. Each follow-up wave was 2-3 years apart and information was gathered via interview and assessment in the participant’s home. At the 5th wave, 902 participants aged 75 years and older were added to the sample (2004/05). Information on sampling and data collection was gathered from the National Archive of Computerized Data on Aging, Inter-university Consortium for Political and Social Research, and has been published elsewhere (5,24). This research used the publicly available waves 1-8, downloaded from the National Archive of Computerized Data on Aging website, and was therefore exempt from review by the institutional review board at the University of Texas Medical Branch.
Inclusion/Exclusion Criteria
Adults 75 years and older were included. Individuals missing data on cognition, positive emotion, or disability in all observation waves were excluded. This sample was used for the first analysis model. Then, in order to study incident disability, individuals with limitations for one or more activities of daily living at baseline were excluded.
Figure 1 illustrates the sample selection process. Initially, there were 2,916 adults aged 75 years and older. After excluding those missing data across all four observation waves for disability, cognition, or positive emotion (N 242) there were 2,674 participants included in the sample for model 1. Next, in order to study incident disability, those with disability at baseline (N = 701) and missing all baseline observation of any key variables (N = 4) were excluded. The final sample used for models 2 and 3 included 1,969 participants.
Figure 1.
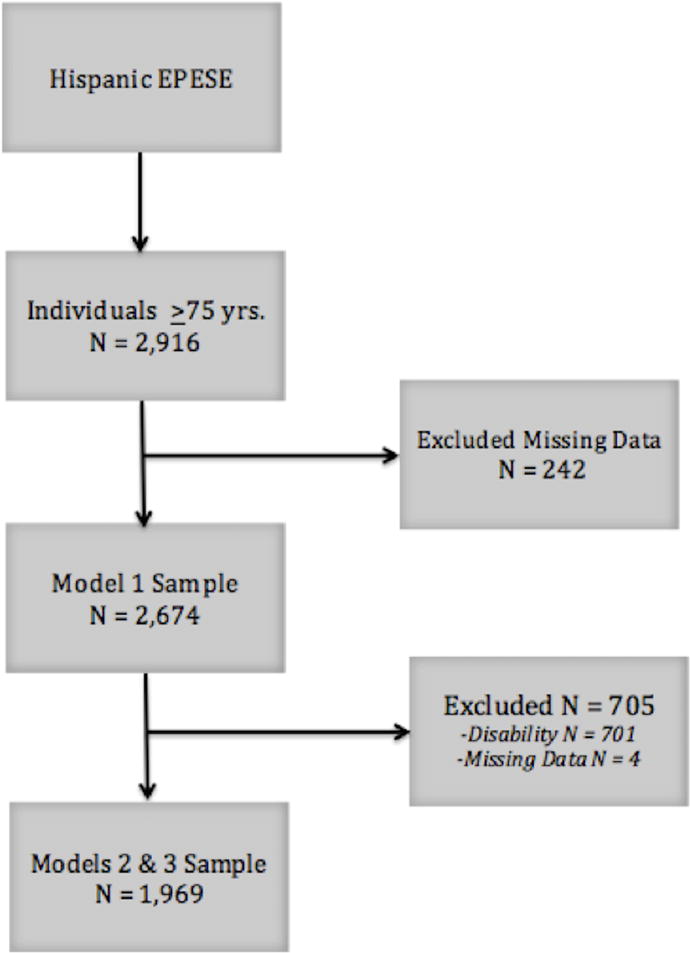
Sample selection from Hispanic Established Populations for the Epidemiologic Studies of the Elderly Data
Those participants excluded from the analytic sample were older, were more likely to be female; cognitively impaired; married; non-smokers; had history of a heart attack, high blood pressure, hip fracture, stroke, diabetes, and arthritis; required a proxy or proxy assistance to complete the interview; had higher BMI and negative emotion; and had less positive emotion and education. All differences were statistically significant p < 0.001.
Measures
Disability
Disability was assessed using self-reported answers to the 7-item version of the Katz Activities of Daily Living (ADL), which has been used frequently with older Hispanic adults (5,21,25). Participations were asked about their ability to walk across a small room, bath, brush their teeth, dress, eat, transfer from a bed to a chair, and use the toilet. They were asked if they were able to complete each task independently without help, if they need help to complete the activity, or if they could not complete activity at all. Disability was dichotomized as “no” (able to perform all ADLs without help) or “yes” (needed help with or were unable to complete one or more of the ADLs). Disability was assessed at baseline and each follow-up wave.
Cognition
The Mini Mental State Exam (MMSE) was used to assess cognition (26). The MMSE is the most common measurement tool used for studies on cognitive aging (27–29). The MMSE assesses several cognitive domains over 19 items; e.g., attention, memory, orientation, and language. Versions were available in both English and Spanish to suit the individual’s needs (30). The MMSE score is a continuous variable with possible scores ranging from 0 to 30. Due to the strong relationship between cognitive impairment and disability (20–22), we dichotomized the MMSE as poor/low cognitive function (≤ 21) and normal/high cognitive function (>21) (31; 32) in order to specifically study those with cognitive impairment. This dichotomy is standard when using the MMSE among aging populations with low levels of education and it has been validated for classifying impaired cognition in older Mexican Americans (28). Cognition was assessed at baseline and each follow-up wave.
Positive Emotion
The positive emotion summary score was created from the four items relating to positivity in the Center for Epidemiologic Studies Depression Scale (33). The four statements are: “I felt that I was just as good as other people”, “I felt hopeful about the future”, “I was happy”, and “I enjoyed life.” Participants rated their response to statements from 0 (“rarely or none of the time”) to 3 (“most or all of the time”). The score for this scale was created by adding the scores from the responses of the four items: range = 0-12. Higher scores indicate higher positive affect. This is the measure used in many studies investigating positive emotion within this population and has high internal consistency (alpha = 0.80) and is weakly correlated (r = −0.25) with the remaining 16 items on negative emotions (5,7). Positive emotion was assessed at baseline and each follow-up wave.
Covariates
Socio-demographic and medical characteristics were controlled for in this study. These variables included age, sex, marital status, and years of education, arthritis, diabetes mellitus, heart attack, hypertension, stroke, body mass index, negative emotion (31,34), and smoking status. Age, BMI, education, and negative emotion were included as continuous variables. Marital status was dichotomized as married or not married. Not married included not married, divorced, or widowed. Participants were asked if a doctor ever told them they had arthritis, diabetes, heart attack, hypertension, or stroke; the answers were all dichotomous yes or no. Sex was also dichotomized as male or female. Negative emotion was calculated by totaling the remaining items of the Center for Epidemiologic Studies Depression Scale after removing the 4 items pertaining to positive emotion (35).
Statistical Analysis
Descriptive characteristics and comorbidities were examined at baseline for the final sample after excluding individuals who were disabled at baseline (see figure 1). Those who never became disabled were compared to those who eventually became disabled. Additionally, those included and those excluded from the study were also compared to each other. T-tests were used for continuous variables and chi-square contingency tables for categorical variables.
To test the modifying effect of positive emotion on the relationship between cognition and disability, we used a series of Generalized Estimating Equations models. Generalized Estimating Equation modeling is appropriate for longitudinal data as it provides dependable estimators of the regression coefficients and of variances under weak assumptions in respect to the correlation between repeated observations of subjects (29). Because Generalized Estimating Equation modeling handles unbalanced data, participants with some missing information were included in the study until their last interview date (36). Due to the complex nature of the relationship between cognition and emotion (37), we employed multiple models for a thorough investigation of this interaction. The paragraphs below explain the differences between the models used. We controlled for all the covariates described above in all three models.
In model 1, cognition, positive emotion, and ADL scores from each wave were included. The data were structured to conduct a series of cross-sectional analyses and provide an overall association between cognitive impairment and ADL disability. The interaction term for positive emotion-by-cognition was included to determine if positive emotion had a modifying effect on the overall relationship between cognitive functioning and disability prevalence.
For models 2 and 3, individuals with disability at baseline were excluded. Model 2 assessed if baseline positive emotion had a moderating effect on the longitudinal relationship between baseline cognition and incident disability over time. Step 1 included a 3-way interaction for positive emotion-by-cohort-by-time, as well as each of the 3 paired combinations: cognition-by-positive emotion, cognition-by-time, and positive emotion-by-time. Non-significant interaction terms were removed; however, cognition-by-time and positive emotion-by-time interaction terms were kept in the model, regardless of significance level, as the focus was on incident disability over time.
For model 3 the data were restructured to conduct a predictive series analysis of the moderating effect of positive emotion on the relationship between cognition and incident disability by the next observation. Disability at baseline was excluded, and cognition scores from each wave were aligned with ADL disability status from the next wave; i.e., baseline cognition predicted disability at the 2nd observation, the 2nd observation of cognition predicted disability at the 3rd observation, etc. This model also included a positive emotion-by-cognition interaction term.
The culmination of these three models provided us with a comprehensive view of how positive emotion interacts with cognition and disability in older Mexican Americans. All analyses were two-tailed with p < 0.05 and performed using IBM SPSS 23.
Results
Table 1 compares population characteristics between those who never had an ADL disability to those who experienced incident ADL disability. Those who experience incident ADL disability were more likely to be older, female, and cognitively impaired; have a history of hip fracture, diabetes, and arthritis; and have higher BMI and less education. There were no significant differences in marital status or smoking status; history of heart attack, high blood pressure, or stroke; or positive or negative emotion.
Table 1.
Descriptive characteristics of the final sample
| No Disability | Disability | Total | |
|---|---|---|---|
|
|
|||
| N | 1141 | 828 | 1969 |
| Cognitively Impaired | 27.78% | 33.82% | 30.32% |
| Male | 47.24% | 35.75% | 42.41% |
| Married | 53.02% | 54.71% | 53.73% |
| Smoker/Former Smoker | 46.45% | 44.20% | 45.51% |
| Heart attack | 12.18% | 12.92% | 12.49% |
| Blood pressure | 51.71% | 54.47% | 52.87% |
| Hip fracture | 3.42% | 5.80% | 4.42% |
| Stroke | 6.92% | 8.45% | 7.57% |
| Diabetes | 25.24% | 29.95% | 27.22% |
| Arthritis | 40.75% | 53.38% | 46.06% |
| Completed by participant | 95.09% | 95.05% | 95.07% |
| Mean (SD) | |||
| Age | 79.82 (4.07) | 80.38 (3.68) | 80.05 (3.92) |
| Education | 5.2 (4.08) | 4.61 (3.9) | 4.95 (4.02) |
| Body mass index | 26.84 (4.56) | 27.33 (4.86) | 27.04 (4.69) |
| Cognition | 23.96 (4.66) | 23.03 (4.68) | 23.57 (4.69) |
| Positive Emotion | 9.46 (2.95) | 9.52 (2.83) | 9.48 (2.90) |
| Negative Emotion | 5.91 (6.87) | 6.44 (7.19) | 6.13 (7.01) |
Table 2 shows the results of model 1, which included a series of cross-sectional analyses using an interaction term of cognition by positive emotion. This tested the overall association between the cognition-by-positive emotion interaction term and concurrent disability across all observations. In this model, impaired cognition, positive emotion, time, and the interaction between cognition and positive emotion were all statistically significant. The largest predictive factor for disability was impaired cognition, demonstrating 2.73 higher odds of having disability than those without impaired cognition. Time was the next largest predictor of disability, with each subsequent wave increasing the odds by 49%. Positive emotion was protective against disability, with each unit increase in positive emotion decreasing the odds of disability by 11%.
Table 2.
Model 1: Cross-sectional series of cognition and positive emotion on ADL disability.
| Variables | OR (95% CI) |
|---|---|
| Impaired Cognition (Not impaired cognition) | 2.72 (1.74, 4.27) |
| Positive Emotion | 0.89 (0.86, 0.92) |
| Time | 1.49 (1.40, 1.59) |
| Impaired Cognition * Positive Emotion | 0.95 (0.90, 0.99) |
Socio-demographic and medical variables controlled for: age, sex, education, marital status, body mass index, smoking status, diabetes, heart attack, stroke, high blood pressure, hip fracture, arthritis, and negative emotion.
(Reference group in parentheses)
Lastly, positive emotion also modified the overall relationship between impaired cognition and disability (OR 0.95, 95% CI: 0.90, 0.99). The modifying effect of positive emotion is graphed in figure 2. This illustration clearly shows that individuals with impaired cognition always have higher probabilities of ADL disability. However, as positive emotion increases, the overall disability risk and the difference in risk between impaired cognition and not impaired cognition decreases considerably.
Figure 2.
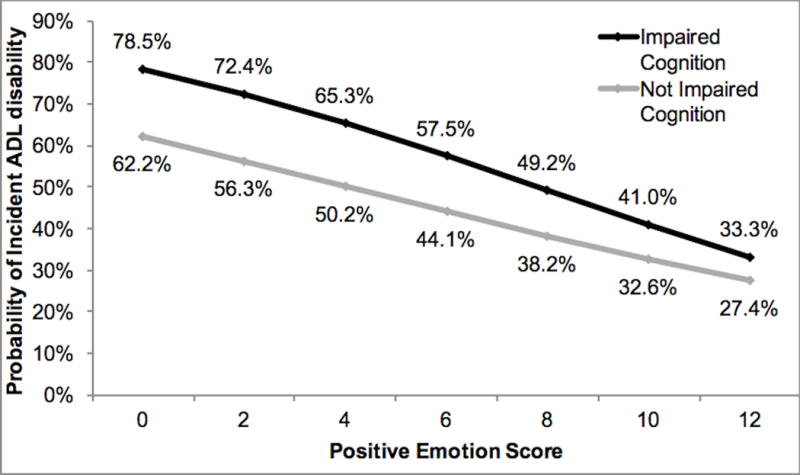
Probability estimates from the cross-sectional relationship between cognition, positive emotion, and disability.
Table 3 shows the results of Model 2, which examined the interaction of baseline positive emotion and baseline cognition on incident ADL disability over time. Step 1 included a three-way interaction term for cohort-by-cognition-by-time, but it was not statistically significant (OR 1.02 [95% CI 0.97, 1.06]). Baseline positive emotion did not modify the effect of baseline cognition on incident disability over time. In step 2, the three-way interaction was removed, and three separate interaction terms, cognition-by-positive emotion, positive emotion-by-time, and cognition-by-time, were examined. Cognition-by-positive emotion was not statistically significant (OR 1.05 [95% CI 0.97, 1.13]). Baseline positive emotion did not modify the relationship between baseline cognition on incident disability. This interaction term was removed in step 3, which included the main effects plus the two remaining interaction terms. In this model only time and cognition-by-time were statistically significant.
Table 3.
Model 2: Baseline cognition and positive emotion predicting incident disability over time
| Variables | Step 1 | Step 2 | Step 3 |
|---|---|---|---|
| OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Impaired Cognition | 1.00 (0.31, 3.22) | 0.69 (0.31, 1.51) | 1.04 (0.74, 1.47) |
| Positive Emotion | 0.99 (0.93, 1.06) | 0.98 (0.92, 1.04) | 1.00 (0.95, 1.06) |
| Time | 2.72 (2.17, 3.42) | 2.62 (2.14, 3.21) | 2.68 (2.18, 3.29) |
| Positive Emotion * Time | 1.00 (0.98, 1.03) | 1.01 (0.99, 1.03) | 1.01 (0.99, 1.03) |
| Cognition * Time | 1.01 (0.64, 1.61) | 1.17 (1.02, 1.33) | 1.17 (1.02, 1.33) |
| Cognition * Positive Emotion | 1.00 (0.89, 1.13) | 1.05 (0.97, 1.13) | |
| Cognition*Positive Emotion*Time | 1.02 (0.97, 1.06) |
Socio-demographic and medical variables controlled for: age, sex, education, marital status, body mass index, smoking status, diabetes, heart attack, stroke, high blood pressure, hip fracture, arthritis, and negative emotion
Table 4 shows the results of Model 3, which included time-varying variables to test whether positive emotion and cognition status over time were associated with relatively short-term incident ADL disability. An interaction term of cognition-by-positive emotion was included in the first step. This interaction term was not significant (OR 1.01 [95% CI: 0.95, 1.07]). Positive emotion did not modify the relationship between cognition and incident ADL disability at the subsequent wave. The term of cognition-by-position emotion was removed and the final step included the main variables, while controlling for socio-demographic and medical covariates. Cognition, positive emotion, and time were all significant predictors of incident ADL disability. Individuals with impaired cognition had 57% higher odds of developing incident ADL disability than those with intact cognition. Positive emotion had a strong protective relationship against incident ADL disability, with each unit increase decreasing the odds of developing ADL disability by 5%. Lastly, with each observation participants’ odds of incident disability increased by 66%.
Table 4.
Model 3: Predictive series of current cognition and positive emotion predicting incident disability at next observation.
| Step 1 | Step 2 | |
|---|---|---|
|
|
||
| Variables | OR (95% CI) | OR (95% CI) |
| Impaired Cognition | 1.44 (0.79, 2.61) | 1.57 (1.30, 1.90) |
| Positive Emotion | 0.95 (0.91, 0.99) | 0.95 (0.92, 0.98) |
| Time | 1.66 (1.51, 1.82) | 1.66 (1.51, 1.82) |
| Impaired Cognition * Positive Emotion | 1.01 (0.95, 1.07) | |
Socio-demographic and medical variables controlled for: age, sex, education, marital status, body mass index, smoking status, diabetes, heart attack, stroke, high blood pressure, hip fracture, arthritis, and negative emotion.
The main effects of model 3 step 2 are plotted in figure 3. Consistent with earlier models, participants with impaired cognition have a higher probability of developing ADL disability compared to those without cognitive impairment. For both groups, the higher the positive emotion score, the lower the probability of developing ADL disability.
Figure 3.
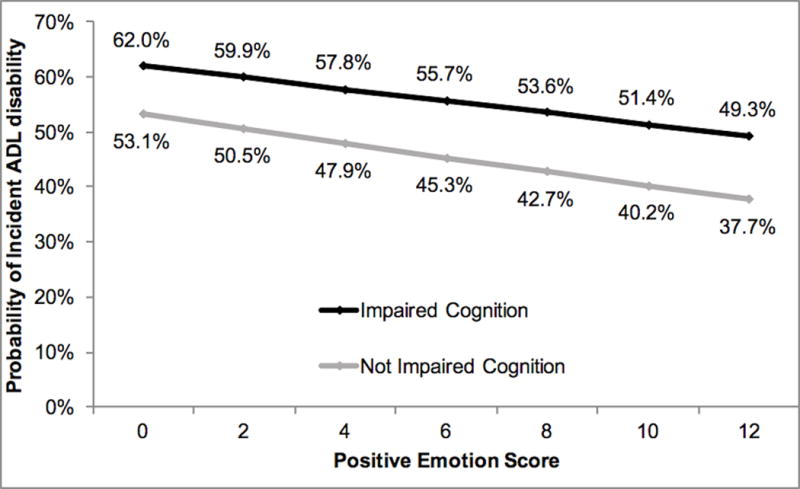
Probability estimates of incident Activity of Daily Living disability in predictive series
Discussion
This study examined if positive emotion modified the relationship between cognition and disability. We found this relationship to be statistically significant in our first, cross-sectional model. Positive emotion was hypothesized to be a modifier, based on the similar mechanisms by which cognition and positive emotion alter disability. Prior research suggests cognition and positive emotion have behavioral components (21,38,39) and neurological/neurochemical components (40–44). Behaviorally, impaired cognition may decrease an individual’s desire to engage in physical activities to maintain strength needed for independence (Raji et al., 2005) and positive emotion may increase an individual’s likelihood to maintain an active lifestyle, despite impairments or disease (39,45).
Neurologically, age related cognitive decline is often related to, and proceeded by, structural changes in the brain (46). Cognitive impairment may be an early indicator of neurologic deficits that may affect physical function later on (43). A common area for atrophy is the prefrontal cortices (43,46). Correspondingly, one study found that positive emotion produced significant brain activation in the prefrontal cortices, while simultaneously exhibiting an increase in dopamine (40), a neurotransmitter that plays an important role in neuroplasticity and recovery (40–42). Given that neurons that fire together wire together (41), along with the role dopamine plays in neurologic recovery, we hypothosized that the neurologic benefits of positive emotion would interact with the effects associated with impaired cognition and prevent incident disability over time.
Positive emotion was a significant modifier in the cross-sectional analysis of the relationship between cognition and disability. The difference in probability for disability between those with and without cognitive impairment decreases as positive emotion increases. This result suggests important implications at the community level. Monitoring and maintaining physical activity, such as reaching your target number of steps each day, has been wide spread at the population level (47). However, mental and emotional health may have a direct impact on physical health as well. It may be important to emphasize that adults take care of themselves from a whole-person approach. For example, prior work suggests that setting and attaining personal goals, maintaining social supports, and developing specific strategies for coping with stress are associated with increased positive emotion (39,48).
A lot has been written regarding positive emotion’s ability to maintain health and facilitate recovery in young and old alike (2,3,8,39). However, less information is available on positive emotion’s relationship with cognitive status and existing research has not considered the potential interaction of these two important variables on physical function. Ostir et al. (34) investigated positive emotion’s role in recovery from stroke post discharge from rehabilitation and found individuals with high positive emotion had higher cognitive status at follow-up compared to those with low positive emotion. Santos et al. (38) studied the impact of mood on cognitive performance among community dwelling individuals in Portugal. They showed that positive emotion stimulated cognitive ability and was protective of cognitive decline over time.
Positive emotion was not a significant modifier in the longitudinal or predictive series analyses on incident disability. Additionally, the main effect of positive emotion was not statistically significant in the longitudinal analysis, but was statistically significant in the predictive series. It is possible that emotional states may be quite dynamic by nature. When examining the association between baseline positive emotion and incident disability over 10 years, fluctuations in participants’ emotional state, and any influence those changes had on disability onset, may have been missed. In the predictive series, positive emotion was significantly associated with disability onset at the next wave. As other studies that have demonstrated positive emotion as a protective factor for disability have had shorter follow up, such as 3 months (35) or 2 years (5). Thus, positive emotion may best be used as a time-varying variable or in shorter longitudinal studies.
Cognition was a significant predictor of disability in the cross-sectional and the predictive series analyses. Cross-sectionally, impaired cognition was strongly associated with disability prevalence and increased the odds of ADL disability by 2.7. A prior cross-sectional analysis with older Mexican Americans found a significant relationship with instrumental activities of daily living, but not with ADL disability (13). It is possible that this study’s size (N = 1,969) compared to the prior research (N = 425) provided more statistical power. Furthermore, instead of being a single snapshot in time, these results are the overall association of cross-sectional analyses over 4 observation waves, allowing for a more in-depth assessment.
In the longitudinal analysis, cognition-by-time was a significant predictor of disability, but cognition was not. While a majority of the existing research has found a statistically significant relationship between baseline cognition and disability (20–22,49), there have been some studies that mirror these results. Jagger, Spiers, and Arthur (50) studied older adults over 11 years and found that MMSE at baseline was not significantly associated with incident ADL disability, but time-varying measures of the Information/Orientation sub-test of the Clifton Assessment Procedures for the Elderly were significantly associated. These inconsistencies emphasize the need for further research to delineate the appropriate way to study the relationship between cognitive impairment and incident disability.
Limitations
Our study has limitations. First, there is a lack of causality due to study design. Second, disability was over-simplified as activity only, without incorporating the environmental factors or the individual’s ability to participate in life situations. By assessing disability as the need for assistance with any one ADL it is possible to show an inflated prevalence of disability. Additionally, it is possible that high levels of impaired cognition may have altered the participants’ ability to accurately report their ADLs. Lastly, another limitation is our missing data due to attrition from death or loss to follow-up. Many participants became missing before a diagnosis of disability and were therefore included as never disabled. It is possible that during the 2-3 years between observations participants became disabled and declined rapidly resulting in institutionalization or even death.
Conclusion
Positive emotion and cognition largely influence the maintenance of health and the risk of developing ADL disability. These analyses provided evidence that time varying cognition and positive emotion had a strong association with disability prevalence and with predicting disability at the subsequent wave. Impaired cognition increases risk of ADL disability and positive emotion decreases the risk of ADL disability. However, the main effects of baseline measures only were not significant in predicting ADL disability over time. Lastly, in cross-sectional analyses, positive emotion modified the relationship between impaired cognition and prevalence of ADL disability among older Mexican Americans. This is the first study that we are aware of to investigate the interaction between positive emotion and cognition on ADL disability, and as such continued research is needed. Next steps to determine if these findings are due to the influence cognition and positive emotion have on health behaviors, neurological responses, or a combination of the two would be beneficial. Future research is needed to develop a better understanding of the influence of positive emotion on cognition and the outcomes improved by the interaction of these two characteristics. These future studies should include subgroup analyses, such as those who maintain high levels of positive emotion over time or a more detailed categorization of cognitive levels. This would pave the way for generating interventions to increase positive emotion as a strategy to potentially delay cognitive impairment. This work has the potential to sustain health, prevent disability, and enhance quality of life, which is important for populations such as older Mexican Americans who are pre-disposed to depression, chronic illness, and disability.
Implications for Rehabilitation.
Promoting emotional well-being may be protective against incident disability for older adults.
Cognitive impairment significantly predicts incident disability in activities of daily living and should be considered an early indicator of impending disability for older adults.
Acknowledgments
This Research was supported in parts by parts by the National Institutes of Health (R01-AG010939, R01-MD010355, P2C-HD065702) and the Jeane B. Kempner Predoctoral Fellowship. Special thanks to Dr. Marinel Ammenheuser for her assistance in editing this manuscript.
Footnotes
Declaration of Interest
The authors report no conflicts of interest.
References
- 1.Huppert FA, Whittington JE. Evidence for the independence of positive and negtive well-being: Implications for quality of life assessment. Br J Health Psychol. 2003;8:107–22. doi: 10.1348/135910703762879246. [DOI] [PubMed] [Google Scholar]
- 2.Horowitz S. Effect of Positive Emotions on Health: Hope and Humor. Altern Complement Ther. 2009;15(4):196–202. [Google Scholar]
- 3.Chida Y, Steptoe A. Positive psychological well-being and mortality: a quantitative review of prospective observational studies. Psychosom Med. 2008;70(7):741–56. doi: 10.1097/PSY.0b013e31818105ba. [DOI] [PubMed] [Google Scholar]
- 4.Greer S, Morris T, Pettingale K, Haybittle JL. Psychological response to breast cancer and 15 year outcome. Lancet. 1990;335:49–50. doi: 10.1016/0140-6736(90)90173-3. [DOI] [PubMed] [Google Scholar]
- 5.Fisher MN, Al Snih S, Ostir GV, Goodwin JS. Positive affect and disability among older Mexican Americans with arthritis. Arthritis Rheum [Internet] 2004;51(1):34–9. doi: 10.1002/art.20079. Available from: http://www.ncbi.nlm.nih.gov/pubmed/14872453. [DOI] [PubMed] [Google Scholar]
- 6.Ostir G, Berges I, Markides K, Ottenbacher K. Hypertension in older adults and the role of positive emotions. Psychosom Med. 2006;68(5):727–33. doi: 10.1097/01.psy.0000234028.93346.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ostir GV, Ottenbacher KJ, Markides KS. Onset of Frailty in Older Adults and the Protective Role of Positive Affect. Psychol Aging [Internet] 2004;19(3):402–8. doi: 10.1037/0882-7974.19.3.402. Available from: http://doi.apa.org/getdoi.cfm?doi=10.1037/0882-7974.19.3.402. [DOI] [PubMed] [Google Scholar]
- 8.Xu J, Roberts RE. The power of positive emotions: it’s a matter of life or death–subjective well-being and longevity over 28 years in a general population. Health Psychol. 2010;29(1):9–19. doi: 10.1037/a0016767. [DOI] [PubMed] [Google Scholar]
- 9.Wan H, Goodkind D, Kowal P. An Aging World: 2015 International Population Reports [Internet] 2016 Available from: http://www.census.gov/content/dam/Census/library/publications/2016/demo/p95-16-1.pdf.
- 10.Gill TM. Disentangling the disabling process: Insights from the precipitating events project. Gerontologist. 2014;54(4):533–49. doi: 10.1093/geront/gnu067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ortman JM, Velkoff VA, Hogan H. An aging nation: The older population in the United States. Econ Stat Adm US Dep Commer [Internet] 2014;1964:1–28. Available from: census.gov. [Google Scholar]
- 12.U.S. Census. Hispanic Heritage Month 2016. United States Census Bur. 2016:15–20. [Google Scholar]
- 13.Ávila-Funes JA, Pina-Escudero SD, Aguilar-Navarro S, Gutierrez-Robledo LM, Ruiz-Arregui L, Amieva H. Cognitive impairment and low physical activity are the components of frailty more strongly associated with disability. J Nutr Health Aging [Internet] 2011;15(8):683–9. doi: 10.1007/s12603-011-0111-8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21968865. [DOI] [PubMed] [Google Scholar]
- 14.Heller PL, Briones DF, Schiffer RB, Guerrero M, Jr, Royall DR, Wilcox JA, et al. Mexican-American ethnicity and cognitive function: Findings from an elderly southwestern sample. J Neuropsychiatry Clin Neurosci. 2006;18(3):350–5. doi: 10.1176/jnp.2006.18.3.350. [DOI] [PubMed] [Google Scholar]
- 15.Hildreth K, Grigsby J, Bryant LL, Wolfe P, Baxter J. Cognitive decline and cardiometabolic risk among Hispanic and non-Hispanic white adults in the San Luis Valley Health and Aging Study. J Behav Med. 2014;37:332–42. doi: 10.1007/s10865-013-9491-z. [DOI] [PubMed] [Google Scholar]
- 16.Lariscy JT, Nau C, Firebaugh G, Hummer RA. Hispanic-White Differences in Lifespan Variability in the United States. Demography. 2016;53(1):215–39. doi: 10.1007/s13524-015-0450-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Markides KS, Eschbach K. Aging, Migration, and Mortality: Current Status of Research on the Hispanic Paradox. Journals Gerontol Ser B Psychol Sci Soc Sci [Internet] 2005;60:S68–75. doi: 10.1093/geronb/60.special_issue_2.s68. Special Issue 2. Available from: http://psychsocgerontology.oxfordjournals.org/content/60/Special_Issue_2/S68.abstract. [DOI] [PubMed] [Google Scholar]
- 18.Gill TM, Gahbauer EA, Murphy TE, Han L, Allore HG. Risk factors and precipitants of long-term disability in community mobility: A cohort study of older persons. Ann Intern Med. 2012;156(2):131–40. doi: 10.1059/0003-4819-156-2-201201170-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fauth EB, Zarit SH, Malmberg B, Johansson B. Physical, cognitive, and psychosocial variables from the Disablement Process Model predict patterns of independence and the transition into disability for the oldest-old. Gerontologist [Internet] 2007;47(5):613–24. doi: 10.1093/geront/47.5.613. Available from: http://www.ncbi.nlm.nih.gov/pubmed/17989403. [DOI] [PubMed] [Google Scholar]
- 20.Raji MA, Al Snih S, Ray LA, Patel KV, Markides KS. Cognitive status and incident disability in older Mexican Americans: Findings from the Hispanic Established Population for the Epidemiological Study of the Elderly. Ethn Dis. 2004;14:26–31. [PubMed] [Google Scholar]
- 21.Raji MA, Kuo YF, Al Snih S, Markides KS, Peek MK, Ottenbacher KJ. Cognitive status, muscle strength, and subsequent disability in older Mexican Americans. J Am Geriatr Soc. 2005;53(9):1462–8. doi: 10.1111/j.1532-5415.2005.53457.x. [DOI] [PubMed] [Google Scholar]
- 22.Black SA, Rush RD. Cognitive and functional decline in adults aged 75 and older. J Am Geriatr Soc [Internet] 2002;50(12):1978–86. doi: 10.1046/j.1532-5415.2002.50609.x. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=emed5&AN=2002455869%5Cnhttp://lib.exeter.ac.uk:4556/resserv?sid=OVID:embase&id=pmid:&id=doi:10.1046/j.1532-5415.2002.50609.x&issn=0002-8614&isbn=&volume=50&issue=12&spage=1978&pages=1978. [DOI] [PubMed] [Google Scholar]
- 23.Raji MA, Ostir GV, Markides KS, Goodwin JS. The interaction of cognitive and emotional status on subsequent physical functioning in older mexican americans: findings from the Hispanic established population for the epidemiologic study of the elderly. J Gerontol A Biol Sci Med Sci [Internet] 2002;57(10):M678–82. doi: 10.1093/gerona/57.10.m678. Available from: http://www.ncbi.nlm.nih.gov/pubmed/12242324. [DOI] [PubMed] [Google Scholar]
- 24.Ottenbacher KJ, Graham JE, Al Snih S, Raji M, Samper-Ternent R, Ostir GV, et al. Mexican Americans and frailty: Findings from the hispanic established populations epidemiologic studies of the elderly. Am J Public Health. 2009;99(4):673–9. doi: 10.2105/AJPH.2008.143958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Beard HA, Markides KS, Al Ghatrif M, Kuo YF, Raji MA. Trends in diabetes medication use and prevalence of geriatric syndromes in older Mexican Americans from 1993/1994 to 2004/2005. Ann Pharmacother. 2010;44(9):1376–83. doi: 10.1345/aph.1M724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–98. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 27.Raji MA, Al Snih S, Ostir GV, Markides KS, Ottenbacher KJ. Cognitive status and future risk of frailty in older Mexican Americans. J Gerontol A Biol Sci Med Sci. 2010;65(11):1228–34. doi: 10.1093/gerona/glq121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mulgrew CL, Morgenstern N, Shetterly SM, Baxter J, Barón a E, Hamman RF. Cognitive functioning and impairment among rural elderly Hispanics and non-Hispanic whites as assessed by the Mini-Mental State Examination. J Gerontol B Psychol Sci Soc Sci. 1999;54(4):P223–30. doi: 10.1093/geronb/54b.4.p223. [DOI] [PubMed] [Google Scholar]
- 29.Samper-Ternent R, Al Snih S, Raji MA, Markides KS, Ottenbacher KJ. Relationship between frailty and cognitive decline in older Mexican Americans. J Am Geriatr Soc [Internet] 2008;56(10):1845–52. doi: 10.1111/j.1532-5415.2008.01947.x. Available from: http://www.scopus.com/inward/record.url?eid=2-s2.0-53149129444&partnerID=tZOtx3y1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bird HR, Canino G, Stipec MR, Shrout P. Use of the Mini-mental State Examination in a Probability Sample of a Hispanic Population. J Nerv Ment Dis. 1987;175:731–7. doi: 10.1097/00005053-198712000-00005. [DOI] [PubMed] [Google Scholar]
- 31.Raji M, Reyes-Ortiz C, Kuo Y-F, Markides K, Ottenbacher K. Depressive Symptoms and Cognitive Change in Older Mexican Americans. J Geriatr Psychiatry Neurol [Internet] 2007;20(3):145–52. doi: 10.1177/0891988707303604. Available from: http://jgp.sagepub.com/cgi/doi/10.1177/0891988707303604. [DOI] [PubMed] [Google Scholar]
- 32.Black S, Espino D, Mahurin R, Lichtenstein M, Hazuda H, Fabrizio D, et al. The influence of noncognitive factors on the Mini-Mental State Examination in older Mexican-Americans: findings from the Hispanic EPESE. Established Population for the Epidemiologic Study of the Elderly. J Clin Epidemiol [Internet] 1999;52(11):1095–102. doi: 10.1016/s0895-4356(99)00100-6. Available from: http://www.ncbi.nlm.nih.gov/pubmed/10527004. [DOI] [PubMed] [Google Scholar]
- 33.Radloff L. The CES-D Scale: A self-report depression scale for use in general populations. Appl Psychol Meas. 1977;1:385–400. [Google Scholar]
- 34.Ostir GV, Berges I, Ottenbacher M, Graham JE, Ottenbacher KJ. Positive emotion following a stroke. J Rehabil Med. 2008;40(6):477–81. doi: 10.2340/16501977-0193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ostir GV, Markides KS, Black SA, Goodwin JS. Emotional well-being predicts subsequent functional independence and survival. J Am Geriatr Soc. 2000;48(5):473–8. doi: 10.1111/j.1532-5415.2000.tb04991.x. [DOI] [PubMed] [Google Scholar]
- 36.Paik MC. The Generalized Estimating Equation Approach When Data Are Not Missing Completely at Random. J Am Stat Assoc. 1997;92(440):1320–9. [Google Scholar]
- 37.Hantke NC, Gyurak A, Van Moorleghem K, Waring JD, Adamson MM, O’Hara R, et al. Disentangling cognition and emotion in older adults: The role of cognitive control and mental health in emotional conflict adaptation. Int J Geriatr Psychiatry. 2016:840–8. doi: 10.1002/gps.4535. [DOI] [PubMed] [Google Scholar]
- 38.Santos NC, Costa PS, Cunha P, Cotter J, Sampaio A, Zihl J, et al. Mood is a key determinant of cognitive performance in community-dwelling older adults: A cross-sectional analysis. Age (Omaha) 2013;35(5):1983–93. doi: 10.1007/s11357-012-9482-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Brummett BH, Morey MC, Boyle SH, Mark DB. Prospective Study of Associations Among Positive Emotion and Functional Status in Older Patients With Coronary Artery Disease. J Gerontol Psychol Sci. 2009;64B(4):461–9. doi: 10.1093/geronb/gbp041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Matsunaga M, Isowa T, Kimura K, Miyakoshi M, Kanayama N, Murakami H, et al. Associations among central nervous, endocrine, and immune activities when positive emotions are elicited by looking at a favorite person. Brain Behav Immun. 2008;22(3):408–17. doi: 10.1016/j.bbi.2007.09.008. [DOI] [PubMed] [Google Scholar]
- 41.Stegemöller EL. Exploring a neuroplasticity model of music therapy. J Music Ther [Internet] 2014 Jan;51(3):211–27. doi: 10.1093/jmt/thu023. [cited 2015 Feb 26]; Available from: http://www.ncbi.nlm.nih.gov/pubmed/25316915. [DOI] [PubMed] [Google Scholar]
- 42.Bao S, Chan VT, Merzenich MM. Cortical remodelling induced by activity of ventral tegmental dopamine neurons. Nature. 2001;412(6842):79–83. doi: 10.1038/35083586. [DOI] [PubMed] [Google Scholar]
- 43.Doi T, Shimada H, Makizako H, Tsutsumimoto K, Hotta R, Nakakubo S, et al. Mild Cognitive Impairment, Slow Gait, and Risk of Disability: A Prospective Study. J Am Med Dir Assoc [Internet] 2015;16(12):1082–6. doi: 10.1016/j.jamda.2015.07.007. Available from: [DOI] [PubMed] [Google Scholar]
- 44.Canevelli M, Cesari M, van Kan GA. Frailty and cognitive decline: How do they relate? Curr Opin Clin Nutr Metab Care [Internet] 2015;18(1):43–50. doi: 10.1097/MCO.0000000000000133. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25405314. [DOI] [PubMed] [Google Scholar]
- 45.Berges I-M, Seale GS, Ostir GV. Positive Affect and pain ratings in persons with stroke. Rehabil Psychol. 2011;56(1):52–7. doi: 10.1037/a0022683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lo JC, Loh KK, Zheng H, Sim SKY, Chee MWL. Sleep duration and age-related changes in brain structure and cognitive performance. Sleep [Internet] 2014;37(7):1171–8. doi: 10.5665/sleep.3832. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=4098802&tool=pmcentrez&rendertype=abstract. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lewis ZH, Lyons EJ, Jarvis JM, Baillargeon J. Using an electronic activity monitor system as an intervention modality: A systematic review. BMC Public Health [Internet] 2015;15(1):585. doi: 10.1186/s12889-015-1947-3. Available from: http://www.biomedcentral.com/1471-2458/15/585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Seale Berges, Ivonne-Marie, Ottenbacher, Kenneth J, Ostir, Glenn V, Seale GS, Gary S, Berges, Ivonne-Marie, Ottenbacher, Kenneth J, Ostir GV, Seale GS, Berges I-M, Ottenbacher KJ, Ostir GV, et al. Change in Positive Emotion and Recovery of Functional Status Following Stroke. Rehabil Psychol. 2010;55(1):33–9. doi: 10.1037/a0018744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Blaum CS, Ofstedal MB, Liang J. Low cognitive performance, comorbid disease, and task-specific disability: findings from a nationally representative survey. J Gerontol A Biol Sci Med Sci. 2002;57(8):M523–31. doi: 10.1093/gerona/57.8.m523. [DOI] [PubMed] [Google Scholar]
- 50.Jagger C, Spiers N, Arthur A. The role of sensory and cognitive function in the onset of activity restriction in older people. Disabil Rehabil. 2005;27(5):277–83. doi: 10.1080/09638280400006523. [DOI] [PubMed] [Google Scholar]


