Abstract
Chronic nonbacterial osteomyelitis (CNO) is a little known autoinflammatory bone disorder primarily affecting children and sometimes young adults. Diagnosis is often delayed due to its varied and nonspecific initial symptoms. Very few cases are reported from India. The aim of this report is to increase the awareness of this disease among physicians, orthopedic surgeons, and rheumatologists. Four male patients were diagnosed with CNO in the past 3 years. The age at onset varied from 9 to 23 years with a median diagnostic delay of 3.5 years. All patients presented with recurrent bony pain with or without localized swelling over the affected bones. Two patients had previously undergone open surgical procedures with bone biopsies and three patients had received at least one course of antibiotics. Two patients responded well to nonsteroidal anti-inflammatory drugs alone, one patient required a short course of glucocorticoids, and another patient required methotrexate to control disease activity. This case series includes males, onset at a relatively later age in most, and a longer diagnostic delay. Thus, in addition to children and adolescents, CNO should be suspected in young adults presenting with recurrent bony pain with or without localized swelling.
KEY WORDS: Auto-inflammatory disease, chronic nonbacterial osteomyelitis, chronic recurrent multifocal osteomyelitis
Introduction
Chronic nonbacterial osteomyelitis (CNO), or more commonly known as chronic recurrent multifocal osteomyelitis (CRMO), is a rare autoinflammatory bone disorder primarily affecting children.[1] Diagnosis is often difficult and delayed not only because it is a diagnosis of exclusion but also because of the decreased awareness about this condition worldwide, more so in India.[2] Many patients receive multiple courses of unnecessary antibiotics and surgical procedures with a mistaken diagnosis of bacterial osteomyelitis before the final diagnosis.
Case Series
Case records of patients diagnosed as CNO/CRMO as per Jansson et al.'s[3] criteria, at our tertiary care referral center in the past 3 years, were reviewed, and clinical features, biochemical parameters, and imaging [radiography, magnetic resonance imaging (MRI), and bone scintigraphy] data were collected. Four patients were diagnosed during this period and are included in this report.
Patient 1
A 24-year-old male presented with 1.5-year history of recurrent pain in distal two-thirds of right arm, right forearm, and right thigh. He had received multiple courses of antibiotics and had two surgeries without any improvement. Multiple bone and blood cultures were sterile. He had persistently increased erythrocyte sedimentation rate (ESR) up to 42 mm/h and C-reactive protein (CRP) up to 47 mg/L. Radiograph showed osteomyelitis of right humerus [Figure 1]. Tc99m-methylene diphosphonate (MDP) bone scan showed increased radiotracer uptake in diaphyses of right humerus, radius, and ulna; in diaphyses and metaphyses of bilateral distal femur and in metaphysis of left proximal tibia [Figure 2]. Based on the history of pain localized to bones, raised inflammatory markers, and sterile osteomyelitis, he was diagnosed as CNO and was started on 500 mg twice daily oral naproxen. He responded well to naproxen which was gradually tapered over 6 months. During the 3-year follow-up, a short course of prednisolone was given to control a relapse.
Figure 1.

Radiograph showing osteomyelitis of right humerus
Figure 2.
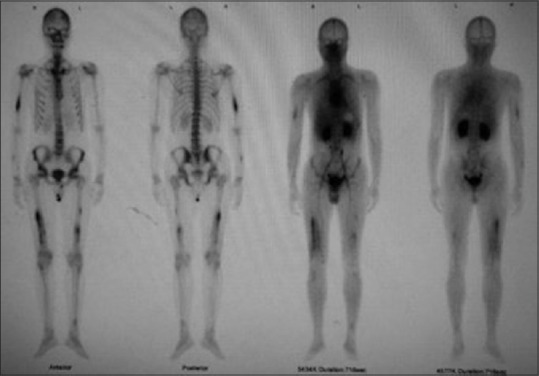
MDP bone scan showing increased radiotracer (Tc99m) uptake in right humerus, right forearm bones, bilateral femur, and left tibia on blood pool and delayed static images – findings consistent with active osteomyelitis
Patient 2
A 25-year-old male presented with 7-year history of recurrent pain and swelling in right thigh with no systemic features. Examination revealed a diffuse firm swelling in the right thigh posteriorly and a small scar from past incision and drainage. He did not respond to multiple courses of antibiotics and surgery. Bone biopsy was normal. MRI revealed an area of altered signal intensity with enhancement in the mid portion of diaphysis of right femur with evidence of cortical thickening, suggestive of chronic osteomyelitis. Tc99m-MDP bone scan showed mildly osteoblastic lesion with cortical thickening in the same area. He showed good response to 500 mg twice daily naproxen.
Patient 3
A 16-year-old boy presented with 2-year history of episodic pain and swelling localized to both lower legs and feet, with each episode lasting for about a week. He also complained of intermittent low backache and buttock pain. He had no other systemic features. Examination was noncontributory except for nonpitting swelling in the lower half of legs. HLA B27 was negative, but ESR and CRP were increased. MRI showed bone marrow edema in metaphyseal and peri-metaphyseal regions of bilateral proximal and distal tibia, and in bones of bilateral midfoot. There was no evidence of synovitis on MRI. Tc99m-MDP bone scan showed increased tracer uptake in metaphyses of bilateral proximal and distal tibia and in bones of bilateral midfoot. The tracer uptake in sacroiliac joints was not increased, which, along with absence of synovitis on MRI, made spondyloarthropathy unlikely. He was on 15 mg weekly dose of methotrexate (MTX) which was increased, leading to good control of disease activity.
Patient 4
A 14-year-old boy presented with history of bony pain in bilateral lower legs and upper forearms, left angle of mouth, and occipital area, with low-grade intermittent fever. The total duration of his illness was five years. He had an ESR of 40 mm/h and CRP of 24 mg/L. Radiographs of bilateral tibia showed osteosclerotic lesions and periosteal reaction. MRI showed bone marrow edema in diaphyses and metaphyses of distal tibia and femur bilaterally, and in left mandible [Figure 3]. Tc99m-MDP bone scan revealed increased uptake in the same areas. Bone biopsy showed no evidence of granuloma, malignancy, or histiocytes. Based on the long-standing history of pain localized to bones, moderately raised inflammatory markers, and radiological evidence of osteosclerosis and osteitis, in the absence of overt infection, diagnosis of CNO was made. He had an excellent response to 75 mg indomethacin daily which was gradually tapered over the next 3 months.
Figure 3.

(a) Axial T1-weighted postcontrast MR image showing contrast enhancement of mandible on left side. (b) Axial STIR MR image showing hyperintensity of mandible on left side
None of the patients in the present cohort had associated clinically apparent inflammatory bowel disease, psoriasis, or any other autoimmune disease. There was no family history of similar complaints in any patient. Clinical and radiological features of these patients are shown in Table 1.
Table 1.
Clinical and radiological features of four patients diagnosed with CNO
| Patient no. | Age at symptom onset (years) | Age at diagnosis (years) | Diagnostic delay (years) | Presentation | Sites involved clinically | Sites involved radiologically | Treatment given |
|---|---|---|---|---|---|---|---|
| 1 | 23 | 24 | 1.5 | Recurrent bony pain and swelling | Distal two-thirds of right arm, right forearm, and right thigh | Diaphyses of right humerus, radius, and ulna; diaphyses and metaphyses of bilateral distal femur and metaphysis of left proximal tibia | NSAIDs, short course of glucocorticoids |
| 2 | 18 | 25 | 7 | Recurrent bony pain and swelling | Right thigh | Diaphysis of right femur | NSAIDs |
| 3 | 14 | 16 | 2 | Recurrent bony pain and swelling | Bilateral lower legs and feet | Metaphyses of bilateral proximal and distal tibia, and bones of bilateral midfoot | NSAIDs, MTX |
| 4 | 9 | 14 | 5 | Recurrent bony pain | Bilateral lower legs and upper forearms, left angle of mouth and occipital area | Diaphyses and metaphyses of distal tibia and femur bilaterally, and in left mandible | NSAIDs |
CNO: chronic nonbacterial osteomyelitis, NSAIDs: nonsteroidal anti-inflammatory drugs, MTX: methotrexate
Discussion
CRMO is a rare autoinflammatory bone disorder first described by Giedion et al. in 1972. Around 500 cases have been now described in literature.[4] It primarily affects children and adolescents, and sometimes young adults. Earlier believed to be multifocal with a chronic and recurrent course, it is now established that the disease can be unifocal and acute. Hence, CNO is the preferred term over CRMO.[5]
The median age at symptom onset has been reported to be 9–10 years in different studies.[2,5,6,7] It is more common in girls with a girl: boy ratio of 2:1.[2,8]. However, in the present case series, all patients were male and the median age of symptom onset was higher at 15 years. This could be due to referral bias as ours is a tertiary care rheumatology unit and young children may have been referred to a pediatrician. The median delay in diagnosis was 42 months which is higher than the previously reported delay of 15 months.[2] This can be attributed to lack of awareness of this condition among physicians.
Bony pain with or without swelling is the most common presenting complaint.[2] Systemic features, including fever and malaise are usually mild. All our patients presented with recurrent bony pain with or without localized swelling over the affected bones. Only one patient reported systemic features, including mild intermittent fever. Mild or no constitutional features, prolonged and episodic course, absence of response to antibiotics, lack of abscess and sequestrum formation, absence of periosteal elevation radiologically, and sterile bone biopsy cultures are some of the clues that should raise the index of suspicion. Under-recognition of the disease leads to unnecessary antibiotics (usually intravenous) and bone biopsies before the diagnosis is reached, as happened in majority of cases in this study.[2] However, the delay in diagnosis is not only related to lack of awareness of this rare condition but also because it remains a diagnosis of exclusion. It is a difficult diagnosis with no specific clinical, laboratory, or radiological features. Multiple diagnostic criteria have been proposed, including the recent Bristol diagnostic criteria which may help in expediting the diagnosis.[2,3] Nonetheless, bone biopsy, which usually shows inflammatory changes (plasma cells, fibrosis), may be required in patients with unifocal disease to exclude more common diagnoses of malignancy or infection.
CNO predominantly involves metaphyses of tubular bones followed by clavicle and vertebrae. Among the tubular bones, distal femur, proximal tibia, distal tibia, and fibula are most commonly involved.[9] The inflammatory changes may also spread to diaphyses of long bones.[10] In the current cohort, three of the four patients had spread to diaphysis. Active lesions are characterized by lytic changes in metaphysis on radiography and presence of bone marrow edema with heterogeneous contrast enhancement on MRI. The lesions heal with sclerosis and as the bone remodels, radiographic appearance may normalize by 2 years.[9] Hence, radiographs may show a combination of osteolytic and osteosclerotic lesions.
CNO has been associated with various disorders, including palmoplantar pustulosis, peripheral arthritis, inflammatory bowel disease, psoriasis, and sacroiliitis.[9] It has also been considered to be a pediatric variant of synovitis, acne, pustulosis, hyperostosis, osteitis syndrome.[9] None of our patients had any associated features. Schnitzler's disease is an important differential diagnosis that should be considered in adults with CRMO and urticarial rash. The mean age of disease onset is 51 years though it has been rarely reported in adolescence.[11] Absence of urticarial rash made this diagnosis unlikely in our patients. Majeed syndrome and deficiency of the interleukin-1 receptor antagonist are the two monogenic syndromic forms of CRMO beginning in first 2 years of life.[12]
Nonsteroidal anti-inflammatory drugs (NSAIDs) are the first line of treatment and are effective in majority. Three of the four patients in this study had good response to NSAIDs. Among second-line agents, bisphosphonates (pamidronate) have emerged as a safe and effective therapy in patients who fail to response to NSAIDs.[13] MTX and anti-TNF agents may be used in refractory cases.
In conclusion, recognition of CNO/CRMO is extremely important to avoid treatment with multiple courses of intravenous antibiotics and surgical procedures for suspected bacterial osteomyelitis. It should be suspected not only in children and adolescents but also in young adults presenting with bony pain with or without swelling, at one or multiple sites.
Declaration of patient consent
The authors certify that appropriate patient consent was obtained.
Financial support and sponsorship
None.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Hedrich CM, Hofmann SR, Pablik J, Morbach H, Girschick HJ. Autoinflammatory bone disorders with special focus on chronic recurrent multifocal osteomyelitis (CRMO) Pediatr Rheumatol Online J. 2013;11:47. doi: 10.1186/1546-0096-11-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Roderick MR, Shah R, Rogers V, Finn A, Ramanan AV. Chronic recurrent multifocal osteomyelitis (CRMO) – Advancing the diagnosis. Pediatr Rheumatol Online J. 2016;14:47. doi: 10.1186/s12969-016-0109-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jansson A, Renner ED, Ramser J, Mayer A, Haban M, Meindl A, et al. Retrospective study of clinical, immunological and genetic aspects in 89 patients. Rheumatology. 2007;46:154–60. doi: 10.1093/rheumatology/kel190. [DOI] [PubMed] [Google Scholar]
- 4.Roderick MR, Sen ES, Ramanan AV. Chronic recurrent multifocal osteomyelitis in children and adults: Current understanding and areas for development. Rheumatology. 2018;57:41–8. doi: 10.1093/rheumatology/kex066. [DOI] [PubMed] [Google Scholar]
- 5.Kaiser D, Bolt I, Hofer M, Relly C, Berthet G, Bolz D, et al. Chronic nonbacterial osteomyelitis in children: A retrospective multicenter study. Pediatr Rheumatol Online J. 2015;13:25. doi: 10.1186/s12969-015-0023-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Catalano-Pons C, Comte A, Wipff J, Quartier P, Faye A, Gendrel D, et al. Clinical outcome in children with chronic recurrent multifocal osteomyelitis. Rheumatology. 2008;47:1397–9. doi: 10.1093/rheumatology/ken249. [DOI] [PubMed] [Google Scholar]
- 7.Beretta-Piccoli BC, Sauvain MJ, Gal I, Schibler A, Saurenmann T, Kressebuch H, et al. Synovitis, acne, pustulosis, hyperostosis, osteitis (SAPHO) syndrome in childhood: A report of ten cases and review of the literature. Eur J Pediatr. 2000;159:594–601. doi: 10.1007/s004310000500. [DOI] [PubMed] [Google Scholar]
- 8.Borzutzky A, Stern S, Reiff A, Zurakowski D, Steinberg EA, Dedeoglu F, et al. Pediatric chronic nonbacterial osteomyelitis. Pediatrics. 2012;130:e1190–7. doi: 10.1542/peds.2011-3788. [DOI] [PubMed] [Google Scholar]
- 9.Iyer RS, Thapa MM, Chew FS. Chronic recurrent multifocal osteomyelitis: Review. AJR Am J Roentgenol. 2011;196:S87–91. doi: 10.2214/AJR.09.7212. [DOI] [PubMed] [Google Scholar]
- 10.Jurik AG, Egund N. MRI in chronic recurrent multifocal osteomyelitis. Skeletal Radiol. 1997;26:230–8. doi: 10.1007/s002560050227. [DOI] [PubMed] [Google Scholar]
- 11.Schrödl K, Nigg A, Treitl M, Flaig M, Jansson A, Schulze-Koops H, et al. Schnitzler's disease as an important differential diagnosis of chronic recurrent multifocal osteomyelitis: A case report. Case Rep Rheumatol. 2012;2012:318791. doi: 10.1155/2012/318791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ferguson PJ, Sandu M. Current understanding of the pathogenesis and management of chronic recurrent multifocal osteomyelitis. Curr Rheumatol Rep. 2012;14:130–41. doi: 10.1007/s11926-012-0239-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Roderick M, Shah R, Finn A, Ramanan AV. Efficacy of pamidronate therapy in children with chronic non-bacterial osteitis: Disease activity assessment by whole body magnetic resonance imaging. Rheumatology. 2014;53:1973–6. doi: 10.1093/rheumatology/keu226. [DOI] [PubMed] [Google Scholar]


