Abstract
Background:
The objectives of this study were the evaluation of pathological characteristics of patients with obesity or metabolic syndrome (MS) as basic cause of death, associating the autopsy findings with some clinical aspects and the abdominal adipose panicle thickness.
Methods:
A total of 88 autopsy cases were studied, divided into 2 groups based on the main cause of death: group 1 (n = 15) obesity and group 2 (n = 73) MS. Clinical summaries of autopsy requests, macroscopic findings, and histologic sections were reviewed.
Results:
The definition of obesity as the basic cause of death is associated with larger thickness of the abdominal adipose panicle, being 8.5 cm (P = .001) the best measurement, according to the receiver operating characteristic curve. Hypertensive cardiopathy (P = .001), ischemic cardiopathy (P = .003), coronary (P = .008)/systemic (P = .005) atherosclerosis, and arterial (P = .014)/arteriolar (P = .027) nephrosclerosis are associated with the diagnosis of MS. Steatohepatitis is associated with the diagnosis of obesity (P = .030); however, its association with the thickness of the abdominal adipose panicle is not statistically significant (P = .211).
Conclusions:
In the context of an obese patient in autopsy, pathologist may use the information about abdominal adipose panicle associated with heart, kidney, and liver findings, even macroscopic ones, to decide the basic cause death between obesity and MS.
Keywords: Autopsy, metabolic X syndrome, obesity
Background
Obesity used to be a disease characteristic of developed countries, but has now become a public health issue of ample geographic distribution, with its prevalence more than doubling between 1980 and 2014. Approximately 13% of the adult world population was obese in 2014.1 In Brazil, the prevalence of this disease in adults rose progressively, from 13.9% in 2009 to 17.9% in 2014.2,3
The most useful measurement to define obesity is the body mass index (BMI), defined as the weight of an individual (in kilograms) divided by the height squared (in meters). According to the classification established by the World Health Organization (WHO), individuals with a BMI score above 30 kg/m2 are considered obese, whereas BMI values above 40 kg/m2 indicate morbid obesity.1
Autopsies are naturally complex and enlightening procedures, representing a theoretical milestone in the understanding of the natural history of diseases.4 Beyond the technical issues, obesity is a disease related to systemic inflammatory phenomenon capable of developing pathologies in different portions of the organism.5 Besides this, obesity is one of the criteria groups which defines metabolic syndrome (MS): central obesity (abdominal circumference above 88 cm for women and above 102 cm for men), systemic arterial hypertension (SAH) (systolic value of 130 mm Hg and diastolic value of 85 mm Hg), diabetes mellitus (DM) or blood glucose above 110 mg/dL, triglycerides levels above 150 mg/dL, and high-density lipoprotein cholesterol below 40 mg/dL for men and below 50 mg/dL for women.1,4,5
This study aimed to describe the morphologic and clinical characteristics of patients whose basic causes of death were defined as obesity or MS after the autopsy procedure.
Methods
Scenario and research outline
This retrospective study was conducted in the Department of Pathology of the Botucatu School of Medicine of the São Paulo State University (FMB-UNESP), along with the autopsy service, located in the same institution.
Our autopsy service is responsible for the autopsy procedure of patients who die within and outside of the hospital environment, as long as there is no evidence of death by external causes. The standard protocol, applied to all cases, includes the macroscopic and microscopic evaluation of the organs, with immediate issuing of the death certificate and complementary report 40 days after the procedure. This study was submitted for appraisal to the Research Ethics Committee of FMB-UNESP and was approved (no. 54588616.2.0000.5411).
The reports of autopsies performed between 1998 and 2014, of patients who died both within and outside of the hospital environment, were retrieved and reviewed. Only patients whose autopsy reports stated obesity or MS as basic cause of death were included in this study. The reports were retrieved from the Department of Pathology computerized database. The patients were categorized according to the basic cause of death into 2 groups: obesity (G1) and MS (G2). Both groups underwent identical clinical and pathologic analysis. We reviewed only the autopsy reports which have the sum of macroscopic and microscopic information, besides a correlation with some clinical data. The report structure is similar to death declaration, but with more details. Pathologists have more data to do the report than the death declaration. Thus, pathologists may use terms that are not necessarily in the international codes of diseases.
Clinical history review
The clinical histories were reviewed using the information from the “clinical summary” section of the reports. The “clinical summary” section in the reports is the exact text that was sent to the pathologist with the autopsy request. Data referring to age, sex, and previous morbidities were collected. The personal background looked for in the clinical summary of the reports was smoking, alcoholism, SAH, DM, dyslipidemia, ischemic or hemorrhagic stroke, acute myocardial infarction (AMI), coronary artery disease (CAD), peripheral artery disease (PAD), infectious diseases, clinical obesity, congestive heart failure, and endocrinal diseases.
Macroscopic aspects review
Data from the patient reports were analyzed: organ weight, morphological patterns of injuries in different organs and systems, thickness of abdominal adipose tissue, and terminal causes of death. Information about systemic and/or coronary atherosclerosis was also collected. Systemic atherosclerosis is an evaluation of aorta, iliac arteries, renal arteries, carotid arteries, and brain arteries. Coronary arteries evaluated were anterior descendant, circumflex, and right coronary.
Microscopic aspects review
Histologic sections of all the patients of the study were reevaluated. For liver sections, a search was completed for the diagnosis of nonalcoholic steatohepatitis (NASH) with its respective staging. For heart sections, verification of the presence of hypertrophy and/or ischemia was done, as well as the infiltration of the muscle by the adipose tissue. For kidney sections, the focus was on arterial, arteriolar, and glomerular injuries.
Statistical analysis
The tabulated data underwent descriptive analysis and the associations, when appropriate, were analyzed by means of the χ2 test or Fisher exact test. Nonparametric variables were studied using the Mann-Whitney test. The significance level adopted was 5%. A complementary analysis was performed because of the variety of quantitative data. The authors applied a correspondence analysis, which is a graphic representation of variable of a contingency table, verifying the degree of interaction between them. The correspondence analysis is mainly applied in contingency tables with a large number of categories to allow a visualization of “attraction” or “repulsion” between categories of variables.
Results
The study analyzed 88 patients, 15 in the obesity group (G1) and 73 in the MS group (G2). Of the 88 individuals, 50 (56.8%) were women. In the MS group, 40 (54.8%) were women, whereas in the obesity group, 10 (66.7%) were women. Regarding age, the MS group comprised patients with a mean age of 66 years (30-108 years). The obesity group had a mean age of 55 years (24-85 years).
Clinical aspects in autopsy “summary” evaluation
The associations between clinical information detected in the “clinical summary” of reports and the groups are presented in Table 1. There was a statistically significant association between the clinical histories of SAH (P < .0001), DM (P < .0001), and dyslipidemia (P = .011) with the diagnosis of MS. Independent of the groups, harmful habits are found. In spite of vascular diseases as strokes and infarcts may occur in patients with obesity or MS, these complications were diseases cited more in the clinical history of MS patients.
Table 1.
Associations between information of “clinical summary” in the request for the necroscopic procedure and the basic cause of death defined as either obesity or metabolic syndrome.
| MS (n = 73) |
Obesity (n = 15) |
P valuea | |
|---|---|---|---|
| No. (%) | No. (%) | ||
| Smoking | 17 (23.3) | 2 (13.3) | .319 |
| Alcoholism | 5 (6.8) | 1 (6.7) | .730 |
| PAD | 1 (1.4) | 0 (0) | .830 |
| CAD | 5 (6.8) | 0 (0) | .383 |
| AMI | 6 (8.2) | 0 (0) | .314 |
| Ischemic stroke | 11 (15.1) | 0 (0) | .111 |
| Hemorrhagic stroke | 1 (1.4) | 0 (0) | .830 |
| SAH | 60 (82.2) | 3 (20.0) | <.001 |
| DM | 58 (79.5) | 2 (13.3) | <.001 |
| Dyslipidemia | 21 (28.8) | 0 (0) | .011 |
| Hypothyroidism | 2 (2.7) | 1 (6.7) | .433 |
| Neoplasm | 2 (2.7) | 0 (0) | .687 |
| Obesity | 9 (12.3) | 4 (26.7) | .152 |
| CHF | 10 (13.7) | 0 (0) | .138 |
Abbreviations: AMI, acute myocardial infarction; CAD, coronary artery disease; CHF, congestive heart failure; DM, diabetes mellitus; PAD, peripheral arterial disease; MS, metabolic syndrome; SAH, systemic arterial hypertension.
χ2 or Fisher exact test, P < .05.
Macroscopic findings
Table 2 represents macroscopic features reported by pathologists in these patients’ autopsies. The findings of hypertensive cardiopathy (P = .001), ischemic heart disease (P = .003), coronary (P = .008) and systemic (P = .005) atherosclerosis, arterial (P = .014), and arteriolar nephrosclerosis (P = .027) are associated with the diagnosis of MS. Only the occurrence of pulmonary embolism (P = .033) showed association with obesity. Pancreatic lipomatosis and cardiac lipomatosis, commonly visualized at obesity patients, do not have any association with one or other diagnostic group. Pulmonary emphysema presented an association with MS (P = .036) and it is interesting because smoking was a harmful habit described more in the “clinical summary” of MS patients.
Table 2.
Association of macroscopic characteristics with the obesity or MS as the basic cause of death.
| MS (n = 73) |
Obesity (n = 15) |
P valuea | |
|---|---|---|---|
| No. (%) | No. (%) | ||
| Cardiac lipomatosis | 5 (6.8) | 1 (6.7) | .730 |
| Hypertensive cardiomyopathy | 71 (97.3) | 10 (66.7) | .001 |
| Acute myocardial infarction | 10 (13.7) | 0 (0) | .138 |
| Ischemic cardiomyopathy | 28 (38.3) | 0 (0) | .003 |
| CHF | 15 (20.5) | 1 (6.7) | .187 |
| Aneurism | 2 (2.7) | 0 (0) | .687 |
| Aortic dissection | 1 (1.4) | 0 (0) | .830 |
| Coronary atherosclerosis | 63 (86.3) | 8 (53.3) | .008 |
| Systemic atherosclerosis | 64 (87.7) | 8 (53.3) | .005 |
| Pulmonary emphysema | 30 (41.1) | 2 (13.3) | .036 |
| Pulmonary embolism | 2 (2.7) | 3 (20.0) | .033 |
| Pancreatic lipomatosis | 11 (15.1) | 3 (20.0) | .439 |
| Arterial nephrosclerosis | 45 (61.4) | 4 (26.7) | .014 |
| Arteriolar nephrosclerosis | 47 (64.4) | 5 (33.3) | .027 |
| Ischemic brain stroke | 9 (12.3) | 0 (0) | .170 |
| Hemorrhagic brain stroke | 3 (4.1) | 0 (0) | .567 |
Abbreviations: CHF, congestive heart disease; MS, metabolic syndrome.
χ2 or Fisher exact test, P < .05.
Abdominal fat panicle thickness was disponible in 34 reports of autopsy patients, 6 were G1 patients and 28 were G2 patients. A relationship between obesity as the basic cause of death and increased thickness of adipose panicle was found (P = .001; normal behavior, according to the Shapiro-Wilk, Kolmogorov-Smirnov, and Mann-Whitney tests). Values between 8.5 and 9.5 cm showed the best sensitivity and specificity ratio in the receiver operating characteristic curve. The thickness sensitivity of 8.5 cm was 100% and the specificity was 75%. For the thickness of 9.5 cm, the sensitivity was 83.3% and the specificity was 78.6%. The abdominal fat panicle thickness was also evaluated in comparison with NASH and myocardial infiltration by adipose tissue, but the associations found were not statistically significant (P = .2111 and P = .152, respectively).
Microscopic findings
Steatosis, mainly in the context of NASH, is expected in patients with obesity, which can be an isolated disease or a part of a MS. There were 9 (60%) patients with NASH in G1 (P = .030), whereas in G2, there were 22 (30.1%). Most of the cases are classified as stage 1 (21.9%, MS; 46.7%, obesity).
Cardiac hypertrophy was present in both groups (P = .302). Previous infarction was a finding of only MS patients (P = .003). Vascular alterations in the kidneys had also a significantly association with MS, as other sort of pathologic aspects that are linked to diseases that compound the syndrome. Other associations are shown in Table 3.
Table 3.
Association between histopathologic parameters and obesity or MS as the basic cause of death.
| MS (n = 73) |
Obesity (n = 15) |
P value | |
|---|---|---|---|
| No. (%) | No. (%) | ||
| Nonalcoholic steatohepatitis | 22 (30.1) | 9 (60.0) | .030 |
| Myocardial hypertrophy | 56 (76.7) | 10 (66.7) | .302 |
| Acute myocardial infarct | 10 (13.7) | 0 (0) | .138 |
| Previous myocardial infarct | 26 (35.6) | 0 (0) | .003 |
| Myocardial adipose infiltration | 23 (31.5) | 5 (33.3) | .556 |
| Arterial fibroelastosis | 67 (91.8) | 6 (40.0) | <.001 |
| Arteriolar nephrosclerosis | 38 (52.1) | 3 (20.0) | .021 |
| Diabetic glomerulosclerosisb | 12 (16.4) | 0 (0) | .090 |
Abbreviation: MS, metabolic syndrome.
χ2 or Fisher exact test, P < .05.
Diabetic glomerulosclerosis = Kimmelstiel-Wilson glomerulosclerosis.
The relationship of adipose tissue and heart was investigated by presence of cardiac lipomatosis, which was found in 13 (17.8%, P = .259) patients in G2 and 1 (6.7%) in G1. Adipose infiltration in myocardium was detected in 23 (31.5%, P = .556) patients with MS and in 5 (33.3%) patients with obesity. The differences were not statistically significant, but it can represent an important aspect of these patients, mainly because obesity may be a problem in both groups.
Terminal causes of death
Sudden cardiac death was indicated in 8 (53.33%) reports of G1 and 35 (47.94%) of G2. Congestive heart failure was considered a terminal cause in 2 (13.33%) G1 patients and 6 (8.21%) G2 patients. Mesenteric ischemia was indicated in 1 (6.66%) patient of G1 and in 1 (1.36%) of G2. Respiratory insufficiency was reported in 1 (6.66%) G1 patient. Pulmonary embolism was the terminal cause in 2 (13.33%) G1 patients and 4 (5.47%) G2 patients. Shock was the terminal cause in 1 (6.66%) G1 patient and 5 (6.84%) G2 patients. Cardiac tamponade, acute cor pulmonale, sepsis, bronchopneumonia, cardiac arrhythmia, hemorrhagic stroke, diabetic ketoacidosis, and AMI were terminal causes for, respectively, 4 (5.47%), 5 (6.84%), 1 (2.73%), 2 (2.73%), 2 (2.73%), 2 (2.73%), 1 (1.36%), and 2 (4.10%) of G2 patients.
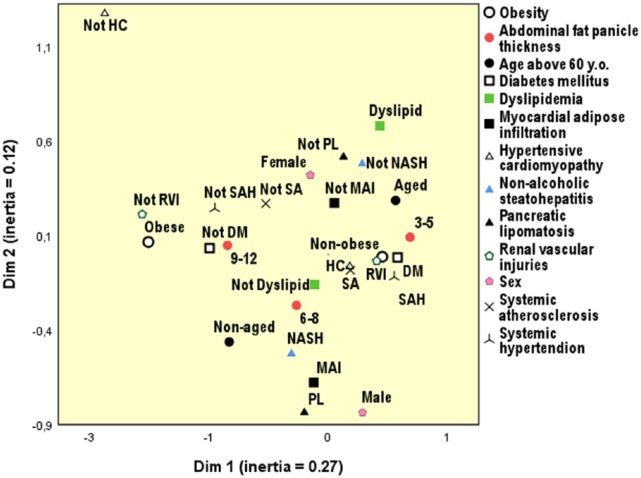
Correspondence analysis
Figure 1 is the graphic product of a correspondence analysis. It is a form of multivariate statistic whose representation is a graphic, in which it is possible to see the variables closer or further in relation to the main aspect. In our case, the main aspect is the basic cause of death: obesity versus MS. The variables more related to basic cause of death obesity were absence of renal vascular injuries as, for example, nephrosclerosis, absence of SAH or DM, and adipose abdominal panicle around 9 to 12 cm of thickening. However, basic cause of death nonobesity was more related to SAH, DM, renal vascular injuries, systemic atherosclerosis, and adipose abdominal panicle around 3 to 5 cm of thickening. Interestingly, NASH and adipose abdominal panicle around 6 to 8 cm of thickening are variables situated in the middle of the distance between obesity and nonobesity as basic cause of death.
Figure 1.
Correspondence analysis graphic. There is a representation of obese patients and nonobese patients. Some diseases were studied regarding their distance in relation to the patients. Conditions that are closer to the obese individual are those with greater association with this variable. DM indicates diabetes mellitus; HC, hypertensive cardiomyopathy; MAI, myocardial adipose infiltration; NASH, nonalcoholic steatohepatitis; RVI, renal vascular injuries; PL, pancreatic lipomatosis; SA, systemic atherosclerosis; SAH, systemic arterial hypertension.
Discussion
This study characterized the morphological aspects of patients with obesity and MS as basic causes of death. It is important to note the lower number of patients in the obesity group, which may be related to the difficulties faced by pathologists to define this diagnosis, either because of the lack of a confirmatory clinical history or due to the impossibility of calculating BMI, because data of weight not always are available, even in reference services. Only 4 patients (26.7%, P = .152) among the 15 patients with basic cause of death obesity had this morbidity reported in the “clinical summary” received by the pathologist.
In an editorial by Cooper and Lucas6 and in a research by Fryer et al,7 the complexity of obesity diagnosis in the autopsy procedure is highlighted, especially due to lack of BMI or absence of clinical indication of this morbidity. The editorial states that this diagnosis is often based on indirect factors such as the thickness of the abdominal adipose panicle and the presence of NASH.6 Fryer et al7 point out that the diagnosis of obesity is not present on death certificates as much as it should be. The authors studied 212 patients who underwent autopsy in the United Kingdom and who had a history of obesity. Only 41 patients (22%) from this set of final autopsy reports had obesity as an item contributing to their death. This also occurred in cases of diseases classically associated with obesity such as obstructive sleep apnea and thrombotic diseases.7
Nonalcoholic steatohepatitis is classically a factor used in the obesity definition. This was a finding associated with obesity as the underlying cause in 60% (9/15, P = .030) of obese patients in our study. However, in the MS group, this percentage was 30.1% (22/73). It should be noted, however, that among the 73 individuals with MS as the underlying cause, 39 were also obese. That is, given the sample size of this study, steatohepatitis may be an inaccurate reference for the diagnosis of isolated obesity in place of a metabolic disease. Thus, NASH must be understood as a marker of obesity, independent of its use as factor to define basic cause of death between obesity and MS. Besides, the correspondence analysis shows that NASH is the middle of the distance between obesity and nonobesity, representing that it is not a perfect marker for one or other as main cause of death.
In this context, one option would be abdominal adipose tissue thickness. In this study, values between 8.5 and 9.5 cm in thickness were associated with obesity as the underlying cause of death (P = .001), with good sensitivity/specificity ratios. However, the measurement values are quite high and with very evident macroscopic effects. The small sample size of only 34 patients with this measurement may have interfered in the results. This lack of data probably exposes the misunderstanding among the pathologists themselves of the inference power of this measurement. It is a simple method which may help in the cause of death definition and due to this it must be stimulated and taught to pathology residents.
However, the study showed that the cases of MS are more associated with microscopic and macroscopic cardiovascular findings. The results found that G2 patients had more statistically significant associations with SAH-related morphological aspects and atherosclerosis, such as hypertensive heart disease, coronary atherosclerosis, systemic atherosclerosis, arterial/ arteriolar nephrosclerosis, and ischemic heart disease. This suggests to the pathologists that, in cases with multiple findings, metabolic condition must be considered in the genesis of the processes that culminated in the death of the patient. Rodríguez-Flores et al8 highlight the association between atherosclerosis and DM, hypertension, obesity, overweight, and increased waist circumference in an autopsy study. Interestingly, myocardium hypertrophy did not have any significant relation with obesity or MS. We suppose that obesity may also stimulate myocardium cells, but other types of study were needed for a precise evaluation of obesity effects in the heart.
Obesity alone in this study was not significantly associated with any of the other cardiovascular findings. Thus, heart diseases, nephrosclerosis, atherosclerosis, and infarcts are also findings that can possibly be used to distinguish between isolated obesity and MS in the definition of the underlying cause at autopsy.
The relationship between DM and obesity is important as insulin resistance is an intersection factor between these 2 morbidities. Experimental studies, in animal models, pointed to associations between DM, obesity and cardiac steatosis. 9,10 In this study, there was no statistically significant association between myocardial adipose infiltration and the clinical history of DM or the morphological findings of diabetic nephrosclerosis. Despite this, the infiltration of myocardial muscle by adipose tissue was seen in 5 of the 15 G1 patients and in 23 of the 73 G2 patients. The same authors9,10 found that myocardial infarction was more frequent in individuals with fatty deposits in the myocardium. This is an interesting subject to be analyzed in future studies with a greater number of patients.
In Brazil, there are no similar studies, and the research presented here draws attention to the difficulties of establishing this diagnosis at autopsy. It is important to reflect on this. It is possible that, even medical assistants, with all the diagnostic possibilities, do not report obesity on death certificates. This is true for patients with MS because the term is not recognized by the international classification of diseases, and therefore, diseases such as hypertension or DM are often chosen for the basic cause and obesity is not mentioned. It is very likely that there is an epidemiologic gap in the statistics leading to a lack of knowledge about the actual number of deaths caused by obesity or MS in Brazil.
It is interesting to note that, in the clinical summaries of the autopsy request, obesity is rarely identified. It leads to think about how health professionals define obesity, mainly if it is understood as a disease. In our study, we discuss the death certificate with an emphasis on basic causes of death, which support public health policies. Thus, their correct completion influences the organization of health services in its different spheres.11 In addition, the study discusses the difficulties faced by pathologists in the distinction between obesity as the underlying cause of death and a death in which obesity is one of the constituents of the MS. An emphasis was on the advancement of pathophysiological knowledge by recognizing the MS as a specific entity. It is a fact that a patient with SAH or DM or obesity or dyslipidemia alone is distinct from a patient who has combinations of these morbidities. Thus, it would be important to correctly codify public actions focused on the change of lifestyle and diagnosis of these individuals.
Metabolic syndrome and obesity are diseases with multiple pathophysiological changes12 and that must be addressed, both clinically and in autopsies, with a broad view of the pathological process. In addition, the recognition of these multifactorial conditions in pathology is of great importance for public health, considering the role of death data in the development of public policies. As explained by Rezende et al,11 the analysis of death from the perspective of a single basic “cause” results in a significant loss of information about mortality, given the high percentage of death certificates with more than one diagnosis due to increasing prevalence of multifactorial diseases, such as obesity and MS.11
Our study has a retrospective model, with limitations, mainly due to our small number of patients in the obesity group. We worked with autopsy reports and their associations between macroscopic and microscopic findings. Pathologists may be more precise in their diagnostics using data as abdominal fat panicle thickness, kidney aspects, heart condition, and liver findings of steatosis. Despite MS is not an official diagnosis, it is used in autopsy reports, and this diagnosis is supported by features in specific organs, similar to what is observed in the clinical and laboratory scenario. Although this context, more studies are necessary for a better definition of morphological criteria that allow select with security obesity or MS as basic cause of death at autopsy.
Acknowledgments
The authors would like to thank Zoe Hamlet from A2Z services of language editing.
Footnotes
Funding:The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work is supported by Brazilin National Council for Scientific and Technological Development (CNPq). L.B.G. is undergraduate student in medicine (FMB-UNESP) and was awarded a scholarship from CNPq (PIBIC) during this research.
Declaration of conflicting interests:The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author Contributions: LBG and CCO are the main authors of the project and are responsible for idea, study plan, research of the reports, review of the histological slides, preparation of tables of data, and writing of the manuscript version. HAM helped with statistical analysis and interpretation. MACD took part of review of the histologic slides. CCO was the professor responsible for the research. All authors approved the final version.
Availability of Data and Materials: Our results are supported by reports and histologic slides whose information is added in the tables. These tables are available. Thus, the corresponding author can be contacted by email for the information, data, and materials to be provided.
Ethical Approval and Consent to Participate: This study was submitted for appraisal to the Research Ethics Committee of FMB-UNESP and was approved (no. 54588616.2.0000.5411).
References
- 1. World Health Organization. Obesity and Overweight. World Health Organization; http://www.who.int/mediacentre/factsheets/fs311/en/. Atualizada em janeiro de 2015. acessada em dezembro de 2015. [Google Scholar]
- 2. Ministério da Saúde. Secretaria de Vigilância em Saúde. Vigilância de fatores de risco e proteção para doenças crônicas por inquérito telefônico—Estimativas sobre frequência e distribuição sociodemográfica de fatores de risco e proteção para doenças crônicas nas capitais dos 26 Estados brasileiros e no Distrito Federal em 2009. Brasília: Ministério da Saúde; 2009. [Google Scholar]
- 3. Ministério da Saúde. Secretaria de Vigilância em Saúde. Vigilância de fatores de risco e proteção para doenças crônicas por inquérito telefônico—Estimativas sobre frequência e distribuição sociodemográfica de fatores de risco e proteção para doenças crônicas nas capitais dos 26 Estados brasileiros e no Distrito Federal em 2014. Brasília: Ministério da Saúde; 2014. [Google Scholar]
- 4. Peres LC. Post-mortem examination in the United Kingdom: present and future. Autops Case Rep. 2017;7:1-3. 10.4322/acr.2017.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Byard RW, Bellis M. Significant increases in body mass indexes (BMI) in an adult autopsy population from 1986 to 2006—implication for modern forensic practice. J Forensic Leg Med. 2008;15:356-358. [DOI] [PubMed] [Google Scholar]
- 6. Cooper H, Lucas S. Letter to the editor: obesity and autopsy reports. Int J Obesity. 2009;33:181. doi: 10.1038/ijo.2008.199. [DOI] [PubMed] [Google Scholar]
- 7. Fryer E, Roberts ISD, Sheppard MN, Verrill C. Postmortem examination in the morbidly obese. Histopathology. 2014;64:200-210. [DOI] [PubMed] [Google Scholar]
- 8. Rodríguez-Flores M, Rodríguez-Saldaña J, Cantú-Brito C, Aguirre-García J, Alejandro GG. Prevalence and severity of atherosclerosis in different arterial territories and its relation with obesity. Cardiovasc Pathol. 2013;22:332-338. [DOI] [PubMed] [Google Scholar]
- 9. Nakanishi T, Kato S. Impact of diabetes mellitus on myocardial lipid deposition: an autopsy study. Pathol Res Pract. 2014;210:1018-1025. [DOI] [PubMed] [Google Scholar]
- 10. Castro AVB, Kolka CM, Kim SP, Bergman RN. Obesity, insulin resistance and comorbidities? mechanisms of association. Arq Bras Endocrinol Metab. 2014;58:600-609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Rezende EM, Sampaio IBM, Ishitani LH. Causas múltiplas de morte por doenças crônico-degenerativas: uma análise multidimensional. Cad Saúde Pública. 2004;20:1223-1231. [DOI] [PubMed] [Google Scholar]
- 12. Mandal R, Loeffler AG, Salamat S, Fritsch MK. Organ weight changes associated with body mass index determined from a medical autopsy population. Am J Forensic Med Pathol. 2012;33:382-389. [DOI] [PubMed] [Google Scholar]