Abstract
Background and Aims:
Ultrasound (US)-guided transversus abdominis plane (TAP) block is used as a part of a multimodal analgesic regimen in the postoperative period. Lateral approach TAP block (LTAP) has been widely used for postoperative analgesia after lower abdominal surgeries. Posterior approach TAP block (PTAP), which is achieved by more posterior blockade of the anterior ramus of the spinal nerve, also provides profound postoperative analgesia after transverse lower abdominal incision. We investigated the dermatomal sensory block following LTAP and PTAP under US guidance.
Material and Methods:
Twenty-seven adult female patients undergoing the laparoscopic resection of ovarian tumors under general anesthesia were randomly divided into two groups, those receiving LTAP (Group L, n = 14) and those receiving PTAP (Group P, n = 13). Before induction of general anesthesia, all patients were given bilateral TAP blocks with 15 ml of 0.25% levobupivacaine on each side under US guidance, and the sensory blockade was evaluated.
Results:
The data are expressed as median (interquartile range [IQR]). PTAP produced a median sensory blockade to sharp touch of three dermatomal segments (IQR 3–4), the most cephalad being T-10 (IQR T-9–T-10), whereas LTAP produced blockade of a median of two segments (IQR 2–2, P = 0.002), the most cephalad being T-10 (IQR T-10–T-10, P = 0.005).
Conclusions:
PTAP produced a sensory block that involved a greater number of dermatomes and involvement of more cephalad dermatome blocked to sharp touch, compared with LTAP under US guidance.
Keywords: Sensory blockade, transversus abdominis plane block, ultrasound guidance
Introduction
Recently, ultrasound (US)-guided transversus abdominis plane (TAP) block has been used in the postoperative period as a part of analgesic regimens. US-guided lateral approach TAP block (LTAP) has been widely used for analgesia after surgeries that require a skin incision on the lower abdominal wall since it effectively reduces pain scores and opioid requirements for up to 24 h after surgery, especially following laparoscopic procedures[1,2] and minimally invasive procedures.[3] LTAP procedure is considered a compartment block due to the local anesthetic being injected into the space between internal oblique abdominis muscle (IOAM) and transversus abdominis muscle (TAM). The procedure has the advantage of not requiring rigorous needle tip positioning in the transversus abdominis fascial plane (TAFP). Since TAP blocks are given under general anesthesia for perioperative analgesia, verification of the blocked sensory segments following LTAP has not been sufficiently evaluated.
It has been previously demonstrated that posterior approach TAP block (PTAP), which is achieved by more posterior blockade of the anterior ramus of the spinal nerve, appears to produce more prolonged analgesia after transverse incision lower abdominal surgeries than LTAP.[4] Carney described that during posterior block the drug extends around the quadratus lumborum and paravertebral space following injection into TAFP, this being confirmed using magnetic resonance imaging (MRI).[5]
For the feasibility of the paravertebral block that additionally results from the spread of the local anesthetic agent to the paravertebral space, various and/or broad sensory segments blocked are probably provided by PTAP, compared with LTAP. Here, we designed a single-blind randomized controlled study involving patients undergoing laparoscopic resection of ovarian tumors, to verify the extent of sensory segments blocked following US-guided LTAP and PTAP performed before general anesthesia induction.
Material and Methods
After obtaining the approval of the Hospital Ethics Committee and written informed consent of the patient, thirty American Society of Anesthesiologists Physical Status I or II adult female patients between the ages of 20 and 79 years, who were scheduled to undergo laparoscopic resection of ovarian tumors under general anesthesia, were enrolled in the study. Patients were excluded if they had an allergy to local anesthetics, coagulation disorder, or a history of previous abdominal surgery. Patients whose body mass index was ≤18 or ≥34 kg/m2 and who weighed <35 kg or ≥100 kg were also excluded from the study. Using sealed envelopes, patients were randomly allocated into two groups: one to undergo LTAP (Group L, n = 15) or another to undergo PTAP (Group P, n = 15). The single anesthesiologist confirming the analgesic segments was blinded to group assignment and was not in the operation theater during the nerve block.
Patients were not premedicated before coming to the operation theater. All TAP blocks were performed before induction of general anesthesia, by one of two adequately skilled investigators. All patients were sedated with midazolam 1–2 mg and fentanyl 50–100 μg intravenously to relieve their anxiety. In case of difficulty in confirming the effect of sensory blockade due to oversedation, 0.2 mg of flumazenil was administrated intravenously.
With the patient in the supine position (LTAP) or prone position (PTAP) and the investigator standing on the ipsilateral side, each block was performed under US guidance using a linear probe (M-Turbo®, SonoSite Inc., Bothell, WA; HFL38 13-6 MHz linear probe). After local anesthesia provided by 2–3 ml of 1% lidocaine, a 22-gauge, 70-mm short-bevel nerve block needle (Plexufix®, B. Braun Melsungen AG. Melsungen, Germany) was inserted and advanced using an in-plane technique.
Ultrasound-guided lateral approach transversus abdominis plane
US-guided LTAP was performed as previously described.[3] The US probe was placed posterior to the midaxillary line between the iliac crest and the costal margin. The needle entry point on the skin was chosen based on the adequate identification of the muscle layers at the umbilical level. After identification of the muscle layers, namely, the external oblique abdominis muscle (EOAM), IOAM, and TAM, a nerve block needle was inserted and advanced using an in-plane technique passing from posterior to anterior so that the drug injected was located at approximately the midaxillary line.
Ultrasound-guided posterior approach transversus abdominis plane
The US probe was placed on the posterolateral abdominal wall [Figure 1] to visualize the edge of the transversus abdominis, and the US sonography showed the transversus abdominis disappearing, the aponeurosis consisted of IOAM and EOAM; furthermore, the appearance of the quadratus lumborum was noticed. Figure 2 shows the typical arrangement of the muscle layers and fascia. A nerve block needle was inserted using an in-plane technique passing from posterior to anterior until the needle tip was positioned in the muscle aponeurosis [Figure 3].
Figure 1.
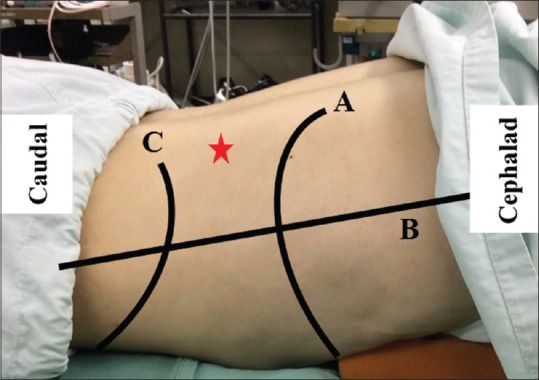
Landmark for posterior approach transversus abdominis plane. A = Subcostal margin, B = Mid-axillary line, C = Iliac crest, Star sign = Nerve block needle entry point
Figure 2.
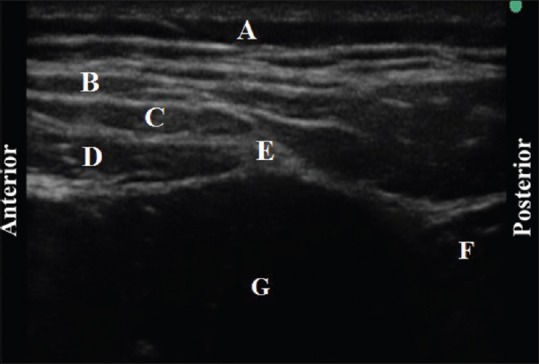
Sonography for posterior approach transversus abdominis plane. A = Subcutaneous tissue, B = External oblique abdominis muscle, C = Internal oblique abdominis muscle, D = Transversus abdominis muscle, E = The muscle aponeurosis, F = Quadratus lumborum, G = Peritoneal cavity
Figure 3.
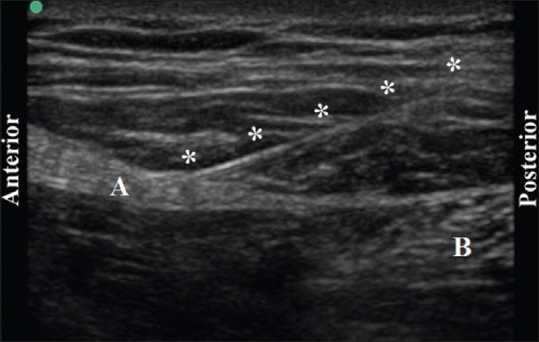
Sonography for the needle tip in aponeurosis. A = The muscle aponeurosis, B = Quadratus lumborum, * = Needle
In each block, after aspiration to avoid inadvertent intravascular injection and abdominal paracentesis, 1 ml of 0.25% levobupivacaine was injected as a test dose. After the correct position of the needle tip for TAP was confirmed by observation of diffusion of the local anesthetic into TAFP, another 14 ml of 0.25% levobupivacaine was injected. A similar procedure was performed on the opposite side, with the injection of 15 ml of 0.25% levobupivacaine. Therefore, 30 ml of 0.25% levobupivacaine solution was injected in each patient.
Evaluation of sensory blockade
After administration of both TAP blocks, all patients were placed in the supine position, and sensory blockade to sharp touch and cold sensation were determined using the pinprick test and ice, respectively, at 20 min after injection of the local anesthetic. Sensory segments were assessed bilaterally along the midclavicular line, to assess right- and left-sided blocks. Any area of sensory blockade was then compared to standard dermatome charts where the subcostal margin T6 dermatome, the umbilicus T10, and the inguinal ligament L-1. The pinprick test was applied with a force adequate to indent the skin without puncturing it, which produced a consistent painful sensation when applied to nonblocked areas. The ice was gently applied on the skin so as to avoid acute temperature changes. All assessments were performed by a single investigator.
Subsequently, all patients received standardized general anesthesia, and the trachea was intubated. During the surgical procedure, we monitored for local anesthetic toxicity symptoms and cardiovascular collapse. After completion of the surgical procedure and emergence from anesthesia, the presence of complications secondary to the block, i.e., numbness in the lower extremities, hematoma, and bleeding; infection was explored until the patients were discharged a few days after undergoing the surgery. All patients were transferred to the high care unit (HCU) in the ward. When patients complained of pain in the HCU, either rectal diclofenac 100 mg or intravenous pentazocine 25 mg was administered as is the standard postoperative analgesic regimen.
Measurements
The number of blocked segments and the highest dermatome of blocked segments were assessed and expressed as median (interquartile range [IQR]). The frequency at which individual sensory segments were blocked was calculated.
Statistical analysis
By means of a preliminary clinical study performed to calculate sample size, it showed that LTAP produced blockade of two sensory segments to sharp touch at 20 min after injection of 15 ml of 0.25% levobupivacaine. Meanwhile, we estimated that the analgesia of four or more sensory segments produced by PTAP would be clinically more useful for postoperative analgesia as compared to the limited analgesia of LTAP. The incidence of four or more sensory segments blockade to sharp touch, determined by the pinprick test, following LTAP and PTAP was approximately 10% and 85%, respectively, in the preliminary study. Therefore, we calculated that 11 blocks per group, i.e., five or six patients, would be required in a design incorporating two equal sized groups, assuming α = 0.05 and β = 0.8. To compensate for the probability of data loss, we enrolled 15 patients per group in the study. All of the patients' demographic data and duration of analgesia with TAP block are presented as a mean ± standard deviation and analyzed using unpaired F-test for parametric data and Mann–Whitney test for nonparametric data. To compare the total number of blocked segments and the highest dermatome segment, as skewed data, Wilcoxon rank-sum test was used. All statistical processing and sample size estimations were performed using SPSS for Windows 16.0 (Chicago, IL, USA). P < 0.05 was considered statistically significant.
Results
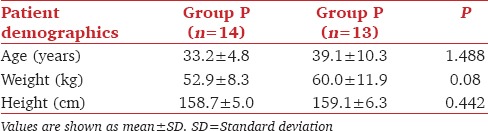
Thirty patients were initially enrolled in the study although three patients with psychiatric disorders were later excluded due to the probability of insufficient evaluation of sensory segments under light sedation. As a result, 14 patients were randomized to Group L and 13 were randomized to Group P. There were no differences in patient characteristics between the two groups [Table 1]. All blocks were performed within 12 min. The mean duration required for performing the block was 10.1 (±1.3) and 10.9 (±1.0) for LTAP and PTAP, respectively (P = 0.332). None of the patients required intravenous administration of flumazenil during any of the procedures, and we were able to confirm the blocked segments in all the patients.
Table 1.
Patient characteristics (n=27)
The median number of segments anesthetized to sharp touch at 20 min after local anesthetic injection was statistically significantly different between the two groups, being 2 (2–2) and 3 (3–4) in Group L and P, respectively (P < 0.001 for both left- and right-sided blocks). Further, the median number of dermatomal segments blocked to cold sensation was statistically significantly different, being 2 (1–2) and 2 (2–3) for Group L and P, respectively (P < 0.001 for both left- and right-sided blocks).
The highest dermatome blocked to sharp touch was T-10 (T-9–T-10) in Group P, which was significantly different from T-10 (T-10–T-10) observed in Group L (P = 0.005 for both left- and right-sided blocks). The highest dermatome blocked to cold sensation tended to be higher in Group P at T-10 (T-9–T-10) although the difference as compared to T-10 dermatome analgesia (T-10–T-11) observed in Group L did not achieve statistical significance (P = 0.058 for both left- and right-sided blocks).
Table 2 depicts the frequency at which individual sensory segments were blocked at 20 min after TAP blocks. All blocks were performed without any complications including evidence of central or systemic toxicity at 20 min after local anesthetic injection. Neither complications nor unintended effects were registered throughout the course of the study.
Table 2.
Frequency of sensory segments blockade to sharp touch and cold sensation in each technique, for right- and left-sided blocks combined (n=54) at 20 min following transversus abdominis plane block

Discussion
In this clinical study, PTAP produced sensory block in a greater number of dermatomes and involved more cephalad dermatome blocked to sharp touch than LTAP at 20 min after bilateral injection of 15 ml of 0.25% levobupivacaine. LTAP commonly produced sensory block to sharp touch of T-10 and T-11, whereas PTAP commonly produced a block of T-9–T-11 dermatomes.
In our LTAP results, a high success rate of blocked segments was shown at T-10 and T-11, whereas low success rates were confirmed above T-9 and at T-12 to L-1. This result is in accordance with the previous study evaluating analgesia with LTAP before induction of general anesthesia in patients undergoing scheduled surgery.[6] As was seen in the blocked T-10 (approximately 90%) and T-11 dermatome (approximately 80%) 30 min after injection of 20 ml of 1% or 0.5% ropivacaine, it is easy to block the T-10 and T-11 dermatomes flowing LTAP. This might suggest that LTAP is recommended as part of an analgesic regimen for abdominal surgeries that require incisions on the lower abdominal wall around the T-10 and T-11 dermatome.
Dermatomal segments produced by our LTAP procedure were narrow as compared to three segments blocked at 30 min after injection of 20 ml of 1% or 0.5% ropivacaine as observed in a previous study.[6] This difference in the number of segments blocked was probably due to the difference in time from local anesthetic injection into TAFP to confirmation of the dermatomal extent of the block, and to the volume of local anesthetic injected.
In a similar consequence of the previous report,[6] which showed the low success rate of L-1 (approximately 50%), it was not easy to block L-1 nerves following LTAP. The iliohypogastric and ilioinguinal nerves, which perforate TAFP by passing through TAM from the deep surface, are always found in TAFP superior to the anterior superior iliac spine although with some variations.[7] Improvement of blockade of L-1 nerves probably requires more anterior placement of the lateral TAFP injection, close to the iliac crest.
According to a cadaveric dissection study,[8] the anterior ramus of the spinal nerves originating between T-9 and L-1 is located between the costal margin and inguinal ligament at the anterior axillary line. Therefore, these segments are likely to be blocked by LTAP performed by local anesthetic injection into TAFP, where the thoracolumbar T-9 to L-1 nerves course before innervating the anterior abdominal wall. Two tissue studies staining by dye injection through the lateral approach in cadavers showed the high success rate of blocking T-11 (100%), T-12 (100%), and L-1 (93%) in one report[9] and T-10 (100%), T-11 (100%), and T-12 (71%) in the other report.[10] However, these studies revealed the low success rate of affection of T-10 (only 50%)[10] and L-1 (only 43%).[10] Segments above T-9 were not stained.[9]
Hence, the sensory segments blocked by TAP block have not been previously clearly defined, and the results of clinical studies and cadaveric dissection studies on the effect on the anterior ramus of the spinal nerve following LTAP are controversial. This mismatch is probably related to individual differences in the branching position of the anterior ramus of the spinal nerve,[8] and the lack of specific prescriptions for needle tip position in TAP block procedure.
PTAP produced a sensory block that was characterized by the involvement of more cephalad dermatomes blocked to sharp touch and a greater number of dermatomes compared to LTAP. As LTAP is recognized as a compartment block, the extent of sensory segments blocked depends on the spread of the local anesthetic over TAFP. Meanwhile, as was seen in an extension of contrast enhancement around the quadratus lumborum and paravertebral space following posterolateral injection,[5] posterolateral injection of the local anesthetic into TAFP probably also produces a paravertebral block effect and sympathetic blockade, as a consequence of posterolateral spread of the local analgesic agent into the paravertebral space. The wider extent of sensory segments blocked following PTAP indicates the possibility of its broad application to postoperative analgesia following several surgical procedures. Therefore, further improvement and modification of PTAP technique, including needle approach and injectate deposition, is required to improve the efficacy and reliability of the block.
TAP block is achieved following local anesthetic injection into an intermuscular plane, in which multiple mixed segmental nerves that branch and communicate within TAFP and run with the deep circumflex iliac artery (TAP plexus).[8] Since TAP block procedure is a compartment block, it requires injection of a large volume of local anesthetics. Therefore, the plasma concentration of levobupivacaine is probably elevated after injection into TAFP. We performed bilateral TAP block with a total dose of 30 ml of 0.25% levobupivacaine, which approximates to 75 mg of levobupivacaine, with neither local anesthetic toxicity symptoms nor cardiovascular collapse being detected during the perioperative period.
In this study, the distribution of sensory blockade was confirmed only along the midclavicular line and not over other areas of the abdomen; therefore, the present study did not evaluate the distribution of sensory blockade completely. According to MRI analysis, the areas of distribution of the local anesthetic administered by LTAP and subcostal approach TAP block do not overlap,[11] implying that the semilunar line can disturb the cephalad and ventral spread of local anesthetics. Therefore, verification of the distribution of sensory block following LTAP and PTAP over a wider area may be required for more complete assessment of the block. Besides, the paravertebral block effect resulting from PTAP probably influences visceral pain, in contrast to the effect only on somatic pain with LTAP. Hence, application of PTAP procedure for postoperative analgesia following a wider range of abdominal surgeries as compared to that with LTAP requires investigation of the effect on visceral pain during surgery and in the postoperative period. A further limitation is a lack of recoding the sedation degree during block procedure and sensory assessment. Putting subjects under definite sedation using evaluation of the detailed sedation degree, for instance, Richmond Agitation-Sedation Scale might provide further reliable evaluation of dermatomal sensory block.
Conclusions
In female patients undergoing laparoscopic resection of ovarian tumors, US guided PTAP block with 15 ml of 0.25% levobupivacaine produced a sensory block affecting an increased number of dermatomes and a more cephalad sensory block to sharp touch as compared to LTAP block. Increased number of dermatomes are affected probably due to posterolateral spread of the local analgesic agent to the paravertebral space.
Further, improvement and modification of PTAP technique, including needle approach and injectate deposition, is required to improve the efficacy and reliability of the block for a postoperative analgesia technique following several abdominal surgeries.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors would like to thank Department of Gynecology, Nihon University School of Medicine, for allowing us to target the patients undergoing laparoscopic resection of ovarian tumors in this clinical study and for their assistance and helpful advice.
References
- 1.Walter CJ, Maxwell-Armstrong C, Pinkney TD, Conaghan PJ, Bedforth N, Gornall CB, et al. A randomised controlled trial of the efficacy of ultrasound-guided transversus abdominis plane (TAP) block in laparoscopic colorectal surgery. Surg Endosc. 2013;27:2366–72. doi: 10.1007/s00464-013-2791-0. [DOI] [PubMed] [Google Scholar]
- 2.Kawahara R, Tamai Y, Yamasaki K, Okuno S, Hanada R, Funato T. The analgesic efficacy of ultrasound-guided transversus abdominis plane block with mid-axillary approach after gynecologic laparoscopic surgery: A randomized controlled trial. J Anaesthesiol Clin Pharmacol. 2015;31:67–71. doi: 10.4103/0970-9185.150547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Niraj G, Searle A, Mathews M, Misra V, Baban M, Kiani S, et al. Analgesic efficacy of ultrasound-guided transversus abdominis plane block in patients undergoing open appendicectomy. Br J Anaesth. 2009;103:601–5. doi: 10.1093/bja/aep175. [DOI] [PubMed] [Google Scholar]
- 4.Abdallah FW, Laffey JG, Halpern SH, Brull R. Duration of analgesic effectiveness after the posterior and lateral transversus abdominis plane block techniques for transverse lower abdominal incisions: A meta-analysis. Br J Anaesth. 2013;111:721–35. doi: 10.1093/bja/aet214. [DOI] [PubMed] [Google Scholar]
- 5.Carney J, Finnerty O, Rauf J, Bergin D, Laffey JG, Mc Donnell JG. Studies on the spread of local anaesthetic solution in transversus abdominis plane blocks. Anaesthesia. 2011;66:1023–30. doi: 10.1111/j.1365-2044.2011.06855.x. [DOI] [PubMed] [Google Scholar]
- 6.Lee TH, Barrington MJ, Tran TM, Wong D, Hebbard PD. Comparison of extent of sensory block following posterior and subcostal approaches to ultrasound-guided transversus abdominis plane block. Anaesth Intensive Care. 2010;38:452–60. doi: 10.1177/0310057X1003800307. [DOI] [PubMed] [Google Scholar]
- 7.Jamieson RW, Swigart LL, Anson BJ. Points of parietal perforation of the ilioinguinal and iliohypogastric nerves in relation to optimal sites for local anaesthesia. Q Bull Northwest Univ Med Sch. 1952;26:22–6. [PMC free article] [PubMed] [Google Scholar]
- 8.Rozen WM, Tran TM, Ashton MW, Barrington MJ, Ivanusic JJ, Taylor GI. Refining the course of the thoracolumbar nerves: A new understanding of the innervation of the anterior abdominal wall. Clin Anat. 2008;21:325–33. doi: 10.1002/ca.20621. [DOI] [PubMed] [Google Scholar]
- 9.Tran TM, Ivanusic JJ, Hebbard P, Barrington MJ. Determination of spread of injectate after ultrasound-guided transversus abdominis plane block: A cadaveric study. Br J Anaesth. 2009;102:123–7. doi: 10.1093/bja/aen344. [DOI] [PubMed] [Google Scholar]
- 10.Murouchi T, Yamauchi M, Gi E, Takada Y, Mizuguchi A, Yamakage M, et al. Ultrasound-guided subcostal and mid-axillary transverus abdominis plane block: A cadaveric study of the spread of injectate. Masui. 2013;62:60–3. [PubMed] [Google Scholar]
- 11.Børglum J, Jensen K, Christensen AF, Hoegberg LC, Johansen SS, Lönnqvist PA, et al. Distribution patterns, dermatomal anesthesia, and ropivacaine serum concentrations after bilateral dual transversus abdominis plane block. Reg Anesth Pain Med. 2012;37:294–301. doi: 10.1097/AAP.0b013e31824c20a9. [DOI] [PubMed] [Google Scholar]


