Abstract
Background and Aims:
Dexmedetomidine has been demonstrated to be safe and efficacious in prolonging the duration of peripheral nerve blocks. This study was designed to compare the duration, quality of postoperative analgesia, hemodynamic stability, and patient's satisfaction with addition of dexmedetomidine to bupivacaine versus plain bupivacaine in pectoral nerve block (Pecs) type I and II in breast surgeries.
Material and Methods:
This prospective randomized double-blind study was carried out in 60 American Society of Anesthesiologists grade I–III female patients, aged 18–70 years randomly allocated into two equal groups. Group A received 10 ml 0.25% bupivacaine for pecs I block and 20 ml 0.25% bupivacaine for pecs II block. Group B received 10 ml 0.25% bupivacaine with dexmedetomidine for pecs I block and 20 ml 0.25% bupivacaine with dexmedetomidine in pecs II block, keeping a total dose of dexmedetomidine of 1 μg/kg body weight and the volume constant in both the groups.
Results:
Numerical rating scores at rest and on abduction of arm were significantly lower in Group B. There was a 40% increase in duration of complete analgesia in dexmedetomidine group (1024.0 ± 124.9 min) compared to plain bupivacaine (726.4 ± 155.3 min; P < 0.001). Total consumption of injection diclofenac sodium in 24 h was 23% less in Group B (77.5 ± 13.6 mg) compared to Group A (100.0 ± 35.9 mg, P = 0.003). Patient satisfaction score was significantly better in dexmedetomidine group. No adverse effects were noted in either group.
Conclusion:
Dexmedetomidine as an adjunct to bupivacaine helps prolong the duration and improves the quality of postoperative analgesia in pecs I and II block without serious side effects.
Keywords: Bupivacaine, dexmedetomidine, pectoral nerve block, ultrasound
Introduction
Optimal pain relief plays a pivotal role in provision and optimization of postoperative care. Ultrasound-guided pecs type I and II blocks provide good postoperative pain relief in patients undergoing breast surgeries as an alternative to paravertebral blocks and thoracic epidurals.[1,2] These blocks are easy, reliable, and devoid of any sympathetic blockade and consequent adverse hemodynamic effects. Pecs type I and II blocks provide both motor and sensory nerve blockade compared to wound infiltration techniques that block only sensory nerves.[2]
Plain local anesthetics provide postoperative pain relief for only a short duration, and insertion of catheter may not be a viable solution as most of these surgeries are done on a daycare basis. There has been considerable interest in adding adjuncts to local anesthetics, such as clonidine, epinephrine, dexamethasone, tramadol, and midazolam, to prolong the duration and improve the quality of analgesia and hence provide better postoperative pain relief.[3] However, only dexmedetomidine has been evaluated as an adjuvant for postoperative pain relief in pecs block.
Dexmedetomidine, a novel specific and selective α-2 adrenergic agonist, has been demonstrated to effectively prolong the duration of analgesia when added to local anesthetic agents in peripheral nerve blocks in animal and human studies without any significant side effects or neurotoxicity.[4,5,6,7]
Dexmedetomidine may produce analgesia by central action, α-2 receptor-mediated vasoconstriction, attenuation of inflammatory responses, direct action on peripheral nerves, or by enhancing the activity-dependent hyperpolarization through blocking the hyperpolarization-activated cation (Ih) current.[8] The available preclinical and clinical data suggest that the combination of dexmedetomidine with local anesthetics is well tolerated without signs of neurotoxicity.[9]
Our aim was to primarily assess the effect of dexmedetomidine as an adjuvant to bupivacaine in pecs block on the duration of postoperative analgesia, pain scores at rest and on abduction of ipsilateral arm, total consumption of analgesics in 24 h, intraoperative fentanyl requirements, and secondarily to evaluate hemodynamic stability, patient satisfaction scores, and any incidence of adverse events.
Material and Methods
This prospective double-blind randomized controlled study was conducted after approval from Institutional Ethical and Scientific Committee and with written informed consent from patients. Sixty female patients of American Society of Anesthesiologists (ASA) status I–III, aged 18–70 years undergoing breast surgeries were included in our study and randomly allocated into two equal groups using computer-generated sequence. Patients with chest wall deformity or pathology, history of recent drug or alcohol abuse, history of psychiatric problems, known hypersensitivity to any study drug, body mass index ≥40 kg/m2, bleeding disorders, or pregnancy were excluded from the study. The drug was prepared by a physician who was not involved in the study. All the personnel involved in the conduct of anesthesia, to the patient, and all the personnel involved in assessing the patient in the postoperative recovery period were blinded to the drug administered.
Intravenous line was established and all the patients received midazolam 1 mg, ondansetron 4 mg, and fentanyl 2 μg/kg before induction of anesthesia. General anesthesia was induced with propofol 1.5–2 mg/kg and atracurium 0.5 mg/kg body weight. Anesthesia was maintained with sevoflurane and oxygen/nitrous oxide admixture with an oxygen fraction of 0.4 to attain one minimum alveolar concentration (MAC) of anesthetic agents throughout the intraoperative period.
After induction of anesthesia, the patients were given pecs block under ultrasound guidance (M-Turbo, Sonosite Inc., Bothell, WA, USA). An in-plane technique was used to perform this block. The fascial plane between pectoralis minor and serratus anterior at the level of the third rib was infiltrated with 20 ml of the selected drug using a high frequency (6–13 MHz) linear array ultrasound probe and an echogenic (21G, 100 mm, SonoPlexStim cannula, Pajunk® GmbH, Germany) needle. The needle was then withdrawn and redirected and 10 ml of drug injected into the fascial plane between pectoralis major and pectoralis minor muscles.
Group A (n = 30) received ultrasound-guided injection of 10 ml 0.25% bupivacaine in between pectoralis major and pectoralis minor muscles (pecs I block) and another 20 ml 0.25% bupivacaine in between pectoralis minor muscle and serratus anterior muscle (pecs II block). Group B (n = 30) received ultrasound-guided injection of 10 ml 0.25% bupivacaine admixed with dexmedetomidine in pecs I block and another 20 ml 0.25% bupivacaine admixed with dexmedetomidine in pecs II block, with a total dose of dexmedetomidine being 1 μg/kg body weight. The calculated dose of dexmedetomidine was admixed with 30 ml of local anesthetic in a sterile bowl while preparing the study drug for the block. The volume of local anesthetic administered in each block was based on the study by Blanco et al.[2]
Intraoperatively, patients were continuously monitored for heart rate, blood pressure [systolic blood pressure, diastolic blood pressure (DBP), and mean arterial pressure (MAP)], SpO2, MAC, and end-tidal carbon dioxide (ETCO2) concentration. Readings were noted every 10 min of the procedure. Patients in whom MAP or heart rate exceeded preoperative value by 20% or more despite maintaining a MAC of 1.0 received intravenous bolus dose of fentanyl 0.5 μg/kg. Total intraoperative fentanyl consumption was noted.
Hypotension, defined as a decrease of >20% of the MAP from the baseline, was treated with 250 ml of Ringer lactate solution and increments of 3 mg bolus doses of mephentermine intravenously. At the end of surgery, neuromuscular blockade was reversed with intravenous neostigmine 50–80 μg/kg and glycopyrrolate 10 μg/kg.
Postoperatively, hemodynamic variables (heart rate, systolic blood pressure, DBP, and MAP) were recorded at 1, 3, 6, 12, 18, and 24 h. The user had the option to verbally rate their scale from 0 to 10 or to place a mark on a line indicating their level of pain. Pain intensity was measured at rest and during abduction of ipsilateral upper limb at 1, 3, 6, 12, 18, and 24 h.
Rescue analgesia was given in the form of intravenous aqueous diclofenac sodium 75 mg at the NRS of 4 or on patient's request. If the pain was still not relieved, intravenous infusion of paracetamol 1 g was given and the time of administration was noted. The duration of absolute postoperative analgesia, defined as the time from the administration of block to the first rescue analgesia, was noted. The total analgesic consumption in the first 24 h was noted. Nausea lasting more than 10 min or vomiting was treated with intravenous metoclopramide 0.15 mg/kg. Any other adverse events were also noted. Patient satisfaction for postoperative analgesia was recorded according to satisfaction score: poor = 0; fair = 1; good = 2; excellent = 3.
Statistical analysis
Our estimated sample size was based on anticipated total consumption of postoperative analgesics in a previous study by Mohamed et al.[10] using a similar protocol. A sample size of 30 patients per group provided an 80% power for detecting a 25% difference for local anesthetic consumption between the two groups (bupivacaine and bupivacaine plus dexmedetomidine) at an alpha level of 0.05.
Statistical testing was conducted with the Statistical Package for the Social Science system, version 17.0. Continuous variables are presented as mean ± standard deviation (SD) and categorical variables are presented as absolute numbers and percentage. The comparison of normally distributed continuous variables between the groups was performed using Student's t-test. Nominal categorical data between the groups were compared using Chi-square test or Fisher's exact test as appropriate. P < 0.05 was considered statistically significant.
Results
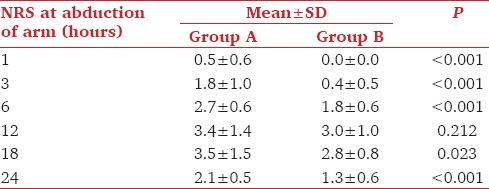
In our study demographic variables and operative characteristics were comparable in both the groups [Table 1]. None of the patients in both the groups required extra doses of intraoperative fentanyl. The addition of dexmedetomidine provided better postoperative pain relief to patients. The NRS scores at rest and at abduction of arm were significantly higher in patients in whom dexmedetomidine was not added to bupivacaine [Tables 2 and 3].
Table 1.
Demographic data and surgical characteristics
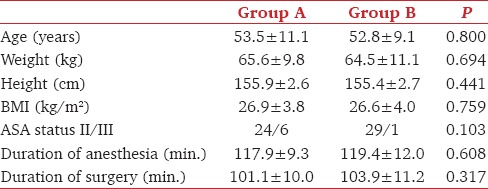
Table 2.
Postoperative pain (NRS) at rest
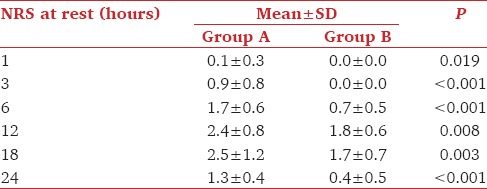
Table 3.
Postoperative pain (NRS) on abduction of arm
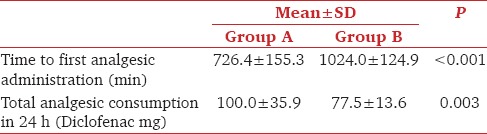
Dexmedetomidine resulted in 40% increase in the duration of complete analgesia. Time to administration of first rescue analgesic was shorter in Group A (726.4 ± 155.3 min) compared to Group B (1024.0 ± 124.9 min, P < 0.001). There was 40.9% increase in duration of absolute analgesia in the study group compared to plain bupivacaine group [Table 4]. Total diclofenac consumption in 24 h was 23% less in Group B (77.5 ± 13.6 mg) compared to Group A (100.0 ± 35.9 mg, P = 0.000) [Table 4]. None of the patients required supplemental paracetamol.
Table 4.
Time to first analgesic administration and total analgesic consumption in first 24 h
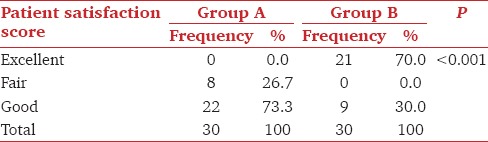
There was significant difference in the overall patient satisfaction score between the two groups (P < 0.001) with patients in Group B more satisfied with the pain relief than in Group A. The overall satisfaction score in Group A was (1.7 ± 0.4) as compared to Group B (2.7 ± 0.4). In Group A, 26.7% patients had fair satisfaction score and 73.3% patients had good satisfaction score. In Group B, 70% patients had excellent satisfaction score and 30% patients had good satisfaction score [Table 5].
Table 5.
Comparison of the patient satisfaction score between the two groups
Intraoperatively, blood pressure and heart rate were recorded at baseline, at surgical incision, and at 10 min intervals thereafter till the end of surgery. The baseline blood pressure and heart rate were comparable between the two groups. Addition of dexmedetomidine to bupivacaine in pecs block did not result in any intraoperative hemodynamic perturbation. Though there was statistically significant difference in the blood pressure between the two groups at 10 min postsurgical incision, it was not clinically significant; none of the patients required vasopressors for maintaining their blood pressure. None of the patients in dexmedetomidine group had bradycardia that required any pharmacological intervention. No period of desaturation was seen in any of our patients. One MAC concentrations were maintained in all the patients in both the groups.
Postoperatively, heart rate and blood pressure were recorded at 1, 3, 6, 12, 18, and at 24 h. None of our patients had bradycardia or hypotension. Statistically significant difference was found in the postoperative DBP, MAP between the two groups at 1 h (P = 0.031) but this difference was not clinically significant. There was no other adverse effect during surgery or at follow-up.
Discussion
Various modalities have been used to provide postoperative analgesia in breast cancer surgeries such as opiates, nonsteroidal antiinflammatory agents, wound infiltration with local anesthetic agents, thoracic epidural, and paravertebral blocks. Pecs I and II block is one such modality and may be an effective and safe alternative. These blocks are easy, reliable techniques, and are devoid of any sympathetic blockade and consequent adverse hemodynamic effects. In addition, peripheral nerve catheters may be inserted to provide prolonged or continuous analgesia but are associated with drawbacks such as dislocation[11] or bacterial colonization with subsequent possible catheter infection.[12,13] Breast cancer surgeries may be done on daycare basis, where perineural catheters are not a viable option.[14] Thus drugs such as dexmedetomidine, which may prolong the duration of single-shot peripheral nerve block, are of particular interest.
The present study was conducted to examine the effect of addition of 1 μg/kg dexmedetomidine to bupivacaine in pectoral nerve blocks. To the best of our knowledge, at the time of conducting the study, there were no published reports demonstrating the efficacy of dexmedetomidine in pectoral nerve blocks. Recently, dexmedetomidine has been shown to be efficacious in prolonging the duration of analgesia when used as an adjunct with levobupivacaine in pecs block.
Dexmedetomidine has been shown to produce antinociception in humans,[10,15] acute and chronic[16] pain states. Dexmedetomidine administered with local anesthetics in peripheral nerve blocks prolongs analgesia by multiple proposed mechanisms such as central action, α-2 receptor-mediated vasoconstriction, inhibition of inflammatory responses, direct action on peripheral nerves, or it may enhance activity-dependent hyperpolarization by blocking the hyperpolarization-activated cation (Ih) current and inhibits subsequent action potentials.[9,17,18] Perineural dexmedetomidine attenuates the bupivacaine-induced acute perineural inflammation.[19]
Mohamed et al.[10] observed that addition of dexmedetomidine 1 μg/kg to bupivacaine in paravertebral blocks for breast cancer surgery prolonged the duration of effective postoperative analgesia and reduced the requirement of analgesics. The meta-analysis of Abdallah et al.[20] showed that dexmedetomidine clearly prolonged the block duration of long-acting local anesthetics.
Addition of dexmedetomidine to bupivacaine in a femoral-sciatic nerve block significantly prolonged the duration of sensory and motor blockade by approximately 40%. Time to first analgesic request was 462.5 ± 54.3 min in bupivacaine group and 807.7 ± 112.9 min in dexmedetomidine group.[21] Dexmedetomidine added to bupivacaine in transversus abdominis plane block in patients undergoing abdominal hysterectomy increased in the time to first analgesic administration by 50%.[22]
Keplinger et al.[23] observed a significant dose-dependent increase in the duration of sensory block with dexmedetomidine. Dexmedetomidine in doses ranging from 20 to 150 μg/kg has been used in peripheral nerve blocks. Higher doses of dexmedetomidine may be associated with higher incidence of bradycardia/sedation. In most studies, dexmedetomidine in fixed dose of 100 μg has been used in peripheral nerve blocks. Dexmedetomidine in doses of 1 μg/kg seems to provide an optimal balance between adequate postoperative analgesia and adverse effects in peripheral nerve blocks.[20] Mohamed et al.[10] observed that addition of dexmedetomidine 1 μg/kg to bupivacaine in thoracic paravertebral block in patients undergoing modified radical mastectomies improved the quality and the duration of analgesia and reduced postoperative analgesic requirements with no serious effects. In our study we also did not observe any significant hemodynamic side effects at these doses.
Bharti et al.[24] noted no differences in the postoperative heart rate or blood pressure values when dexmedetomidine in the dose of 1 μg/kg was used as an adjunct to local anesthetic agents in peripheral nerve blocks.
Conclusion
In conclusion dexmedetomidine prolongs the duration and improves the quality of postoperative analgesia when used as an adjuvant to bupivacaine in pecs I and II blocks with no serious side effects.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Blanco R. The ‘pecs block’: A novel technique for providing analgesia after breast surgery. Anaesthesia. 2011;66:847–8. doi: 10.1111/j.1365-2044.2011.06838.x. [DOI] [PubMed] [Google Scholar]
- 2.Blanco R, Fajardo M, Parras Maldonado T. Ultrasound description of Pecs II (modified Pecs I): A novel approach to breast surgery. Rev Esp Anestesiol Reanim. 2012;59:470–5. doi: 10.1016/j.redar.2012.07.003. [DOI] [PubMed] [Google Scholar]
- 3.Brummett CM, Williams BA. Additives to local anesthetics for peripheral nerve blockade. Int Anesthesiol Clin. 2011;49:104–16. doi: 10.1097/AIA.0b013e31820e4a49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Virtanen R, Savola JM, Saano V. Characterization of the selectivity, specificity and potency of dexmedetomidine as an alpha 2-adrenoceptor agonist. Eur J Pharmacol. 1988;150:9–14. doi: 10.1016/0014-2999(88)90744-3. [DOI] [PubMed] [Google Scholar]
- 5.Calasans-Maia JA, Zapata-Sudo G, Sudo RT. Dexmedetomidine prolongs spinal anaesthesia induced by levobupivacaine 0.5% in guinea-pigs. J Pharm Pharmacol. 2005;57:1415–20. doi: 10.1211/jpp.57.11.0006. [DOI] [PubMed] [Google Scholar]
- 6.Esmaoglu A, Yegenoglu F, Akin A, Turk CY. Dexmedetomidine added to levobupivacaine prolongs axillary brachial plexus block. Anesth Analg. 2010;111:1548–51. doi: 10.1213/ANE.0b013e3181fa3095. [DOI] [PubMed] [Google Scholar]
- 7.Obayah GM, Refaie A, Aboushanab O, Ibraheem N, Abdelazees M. Addition of dexmedetomidine to bupivacaine for greater palatine nerve block prolongs postoperative analgesia after cleft palate repair. Eur J Anaesthesiol. 2010;27:280–4. doi: 10.1097/EJA.0b013e3283347c15. [DOI] [PubMed] [Google Scholar]
- 8.Brummett CM, Hong EK, Janda AM, Amodeo FS, Lydic R. Perineural dexmedetomidine added to ropivacaine for sciatic nerve block in rats prolongs the duration of analgesia by blocking the hyperpolarization-activated cation current. Anesthesiology. 2011;115:836–43. doi: 10.1097/ALN.0b013e318221fcc9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mehofer P, Brummett CM. Safety and efficiency of dexmedetomidine as adjuvant to local anaesthetics. Curr Opin Anesthesiol. 2016;29:632–7. doi: 10.1097/ACO.0000000000000364. [DOI] [PubMed] [Google Scholar]
- 10.Mohamed SA, Fares KM, Mohamed AA, Alieldin NH. Dexmedetomidine as an adjunctive analgesic with bupivacaine in paravertebral analgesia for breast cancer surgery. Pain Physician. 2014;17:E589–98. [PubMed] [Google Scholar]
- 11.Marhofer D, Marhofer P, Triffterer L, Leonhardt M, Weber M, Zeitlinger M. Dislocation rates of perineural catheters: A volunteer study. Br J Anaesth. 2013;111:800–6. doi: 10.1093/bja/aet198. [DOI] [PubMed] [Google Scholar]
- 12.Capdevila X, Pirat P, Bringuier S, Bernard N, Singelyn F, Bonnet F, et al. Continuous peripheral nerve blocks in hospital wards after orthopaedic surgery: A multicenter prospective analysis of the quality of postoperative analgesia and complications in 1416 patients. Anesthesiology. 2005;103:1035–45. doi: 10.1097/00000542-200511000-00018. [DOI] [PubMed] [Google Scholar]
- 13.Volk T, Engelhardt L, Spies C, Kutter B, Werner C, Wulf H, et al. Incidence of infection from catheter procedures for regional: First results from the network of DGAI and BDA. Anaesthesist. 2009;58:1107–12. doi: 10.1007/s00101-009-1636-7. [DOI] [PubMed] [Google Scholar]
- 14.Goodman AA, Mendez AL. Definitive surgery for breast cancer performed on an outpatient basis. Arch Surg. 1993;128:1149–52. doi: 10.1001/archsurg.1993.01420220069009. [DOI] [PubMed] [Google Scholar]
- 15.Sarita SS, Keniya VM, Ladi SD, Rao R. Comparison of dexmedetomidine and clonidine (a2 agonist drugs) as an adjuvant to local anaesthesia in supraclavicular brachial plexus block: A randomized double-blind prospective study. Indian J Anaesth. 2012;56:243–49. doi: 10.4103/0019-5049.98767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sitilci AT, Ozyuvaci E, Alkan Z, Demirgan S, Yigit O. The effect of perioperative infused dexmedetomidine on postoperative analgesic consumption in mastoidectomy operations. Agri. 2010;22:109–16. [PubMed] [Google Scholar]
- 17.Dalle C, Schneider M, Clergue F, Bretton C, Jirounek P. Inhibition of the I(h) current in isolated peripheral nerve: A novel mode of peripheral antinociception? Muscle Nerve. 2001;24:254–61. doi: 10.1002/1097-4598(200102)24:2<254::aid-mus110>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- 18.Shirasaka T, Kannan H, Takasaki M. Activation of a G protein-coupled inwardly rectifying K+ current and suppression of Ih contribute to dexmedetomidine-induced inhibition of rat hypothalamic paraventricular nucleus neurons. Anesthesiology. 2007;107:605–15. doi: 10.1097/01.anes.0000281916.65365.4e. [DOI] [PubMed] [Google Scholar]
- 19.El-Hennawy AM, Abd-Elwahab AM, Abd-Elmaksoud AM, El-Ozairy HS, Boulis SR. Addition of clonidine or dexmedetomidine to bupivacaine prolongs caudal analgesia in children. Br J Anaesth. 2009;103:268–74. doi: 10.1093/bja/aep159. [DOI] [PubMed] [Google Scholar]
- 20.Abdallah FW, Brull R. Facilitatory effects of perineural dexmedetomidine on neuraxial and peripheral nerve block: A systematic review and meta-analysis. Br J Anaesth. 2013;110:915–25. doi: 10.1093/bja/aet066. [DOI] [PubMed] [Google Scholar]
- 21.Helal SM, Eskandr AM, Gaballah KM, Gaarour IS. Effects of perineural administration of dexmedetomidine in combination with bupivacaine in a femoral-sciatic nerve block. Saudi J Anaesth. 2016;10:18–24. doi: 10.4103/1658-354X.169469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Almarakbi WA, Kaki AM. Addition of dexmedetomidine to bupivacaine in transversus abdominis plane block potentiates post-operative pain relief among abdominal hysterectomy patients: A prospective randomized controlled trial. Saudi J Anaesth. 2014;8:161–6. doi: 10.4103/1658-354X.130683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Keplinger M, Marhofer P, Kettner SC, Marhofer D, Kimberger O, Zeitlinger M. A pharmacodynamic evaluation of Dexmedetomidine as an additive drug to ropivacaine for peripheral nerve blockade: A randomized triple blind controlled study in volunteers. Eur J Anaesthesiol. 2015;32:790–6. doi: 10.1097/EJA.0000000000000246. [DOI] [PubMed] [Google Scholar]
- 24.Bharti N, Sardana DK, Bala I. The analgesic efficacy of dexmedetomidine as an adjuvant to local anaesthetics in supraclavicular brachial plexus block: A randomized controlled trial. Anesth Analg. 2015;121:1655–60. doi: 10.1213/ANE.0000000000001006. [DOI] [PubMed] [Google Scholar]


