Abstract
Background and Aims:
Adductor canal block (ACB) is now an established component of multimodal analgesia for knee replacement surgery and is slowly replacing femoral nerve block (FNB). It is also gaining popularity for providing pain relief in knee arthroscopies including anterior cruciate ligament reconstruction surgery (ACLR). Data is lacking from the Indian subcontinent on comparing ACB to the traditional FNB for ACLR. Hence, we conducted the present study to compare ACB and FNB in ACLR under general anesthesia.
Material and Methods:
Sixty patients were randomized to receive either ACB or FNB under ultrasound guidance. Postoperatively, quadriceps muscle strength (straight leg raise and time up and go; TUG test) and quality of analgesia (numeric rating scale; NRS and patient satisfaction score) were assessed every 6 hour, and thereafter, up to 48 hours. The time of rescue analgesia and total analgesic consumption (tramadol) were also recorded. Data was statistically analyzed and P < 0.05 was considered to be significant.
Results:
Patients receiving ACB had significantly less quadriceps weakness (P < 0.001) compared to FNB on postoperative day (POD) 1. In addition, patient satisfaction score was statistically higher (P < 0.05) in FNB on POD1. Both the above parameters were comparable on POD2. No statistically significant difference was recorded in NRS, time for rescue analgesia, and total analgesic consumption among the two groups.
Conclusion:
ACB preserves quadriceps motor strength while providing analgesia comparable to FNB in patients undergoing ACLR. However, patient satisfaction score is better with FNB than ACB.
Keywords: Adductor canal block, arthroscopic ACLR, femoral nerve block
Introduction
Anterior cruciate ligament (ACL) is the most commonly injured ligament of the knee.[1] Arthroscopic ACL repair (ACLR) is the technique of choice for surgery. Although arthroscopic procedures are minimally invasive surgeries, postoperative pain persists from graft anchoring into the ACL. Various modalities are used for analgesia by systemic and multiple non-systemic approaches such as local anesthetic infiltration, peripheral nerve block, intra-articular injection, and neuraxial blockade.[2] Peripheral nerve blocks provide maximum pain relief but the associated motor paralysis becomes the limiting factor. To fulfil our goals of having a pain-free patient with good motor preservation, we need a local anesthetic drug that selectively acts on sensory fibres. Nonetheless, no such drug exists in our armamentarium at present, and hence, the research for motor-sparing drugs continues.
Femoral nerve block (FNB) is a commonly used nerve block in patients undergoing knee surgery. However, FNB causes weakness of quadriceps muscle which impairs early ambulation and may increase the risk of falls.[3,4] Adductor canal block (ACB), on the other hand, is a motor-sparing block, and with the advent of ultrasonography, easy visualization of adductor canal has increased its success rate.[3] ACB mainly blocks the saphenous nerve and the nerve to vastus medialis while they pass through adductor canal.[5]
Hence, we decided to conduct the current study comparing the two blocks in patients undergoing ACLR under general anesthesia. The primary outcome of the study was to compare the motor paralysis between the two groups, while evaluating the quality of postoperative analgesia, duration of postoperative analgesia, total analgesic consumption, and patient satisfaction score were the secondary outcomes to be studied.
Material and Methods
After obtaining approval from the Institutional ethical committee, all patients who were scheduled to undergo elective ACLR surgery received information about the study, and patients who accepted to participate were enrolled in the study. Inclusion criteria were patients with American Society of Anaesthesiologists (ASA) physical status I and II, aged 25–35 years, and with body mass index (BMI) between18 and 35. Patients with bleeding diathesis or coagulopathy, infection at the site of injection, alcohol or drug abuse, renal impairment, patient with ASA physical status above II, body mass index above 35, and local anesthetic sensitivity were excluded from study. Participants were assigned to either ACB group or the FNB group (1:1 allocation) based on a computer-generated randomization list.
A written informed consent was obtained from the patients willing to participate in the study. All patients were informed about the numerical rating scale (NRS) for pain assessment as well as trained for the timed up and go (TUG) test. In the operating room, standard monitors were applied and an intravenous line was secured. After preoxygenation, general anesthesia was induced with injection propofol 2mg/kg and injection fentanyl2mcg/kg. After loss of consciousness, injection vecuronium 0.1mg/kg was administered. Endotracheal intubation was done with an appropriate-sized endotracheal tube. Patients were mechanically ventilated on volume control mode. Anesthesia was maintained using isoflurane in 50% O2 and 50% N2O to achieve stable hemodynamics. Incremental dose of vecuronium was given whenever required. Minimum monitoring standards were followed. All ACLR surgeries were done under femoral tourniquet by the same orthopedic surgeon, using same kind of autograft (patellar graft).
At the end of the surgery, patients were randomized to either receive ACB or FNB under ultrasound guidance. The anesthesiologist performing the block was not involved in any other aspect of study. A linear ultrasound probe (sonosite nanomaxx) was used for performing both the blocks. For ACB, the ultrasound probe was placed at the mid-thigh level halfway between the anterior superior iliac spine and patella. The femoral artery underneath the sartorius muscle was identified. The saphenous nerve lies just lateral to the artery. A 21-G,5-cm needle was introduced in plane and advanced into the adductor canal. On reaching the adductor canal, 2–3 ml of saline was injected to ensure correct placement of needle, i.e., spread of saline in the vicinity of saphenous nerve. After confirmation, 20ml of0.5% ropivacaine was injected in the adductor canal.
For FNB, the needle was inserted in plane with the probe parallel to inguinal crease with slight cephalic tilt to identify the femoral artery and femoral nerve. The needle was advanced towards the femoral nerve and 20ml of 0.5% ropivacaine was injected. Adequate local anesthetic spread was confirmed in both the techniques. After completion of block, patients were extubated post administration of reversal agents (neostigmine and glycopyrollate) and return of airway reflexes. Postoperatively, all patients received 1g of injection paracetamol intravenous infusion every 6 hours. Routine monitoring was continued in the postoperative period. Further, all the study-related monitoring and evaluation was done by independent observer. The primary outcome of the study, i.e., comparison of quadriceps muscle power was assessed by asking the patient to perform a straight leg raise test (SLR) in supine position. The motor block was graded as follows:
Grade 0: normal muscle power
Grade I: motor weakness
Grade II: complete motor paralysis.
The assessment began in the postoperative care unit (0h), every 6 h thereafter for 24 h. Monitoring for motor weakness continued for two postoperative days. On postoperative day (POD) 1, patients were assessed and encouraged to ambulate with assisted walking aids. Mobilization ability was assessed with TUG test, which measures the time to take the patient to get up from the chair, walk 3m, turn, walk back to chair, and sit down. This test was not performed if the patient felt that it is not possible to rise and walk and was at risk of fall. The number of patients admitting risk of fall was also recorded. Postoperative analgesia was assessed by NRS. Patients verbally rated pain intensity as an integer from 0 to10 (0 = no pain, 10 = worst possible pain).
Whenever demanded, rescue analgesia was given in the form of intravenous tramadol 2 mg/kg. The time of rescue analgesia was recorded. Total analgesia consumption in first 24 h was also recorded. To calculate the level of satisfaction, the scoring was done from 1 to 7 in which 1 = very satisfied, 2 = somewhat satisfied, 3 = slightly satisfied, 4 = neither satisfied or dissatisfied, 5 = slightly dissatisfied, 6 = somewhat dissatisfied, 7 = very dissatisfied. These were the secondary outcomes of our study.
Data analysis
The study by Charous et al. revealed a standard deviation of 18% concerning quadriceps strength in healthy volunteers.[6] Power analysis permitted a type-1 error rate of 0.05 with type-2 error rate of 0.02, a sample size of 27 patients was calculated in each group. We totalled the sample size to 60 patients, predicting a dropout of 10%. Statistical analysis was conducted with Statistical Package for Social Sciences, version 19.0 (SPSS, Inc, Chicago IL, USA). Parametric variables such as age, sex, and BMI were analyzed with Student's t-test. While for nonparametric data, Chi-square test was used. P < 0.05 was considered statistically significant and P < 0.001 as highly significant.
Results
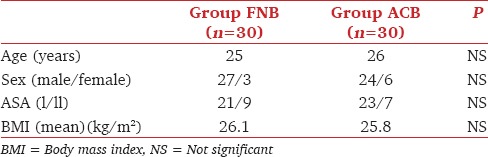
All the sixty patients completed the study with successful block. In both the groups, patients' demographic profile was comparable with regard to age, sex, ASA status, and BMI [Table 1].
Table 1.
Comparison of demographic profile and other details
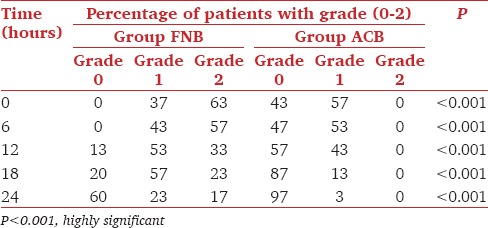
The patients in the ACB compared to the FNB group had less quadriceps muscle weakness as seen on SLR test. The difference was highly significant [Table 2].
Table 2.
Comparison of straight leg raise test between the two groups
On assessment of quadriceps muscle strength with TUG test on POD1, 26 patients in the ACB group were able to perform the test and none of the patients was at risk of fall; in the FNB group, only 18 patients were able to perform test and 6 patients were at risk of fall. This difference was statistically significant (P < 0.01). However, on POD2, all patients in both the groups performed the test without any risk of fall.
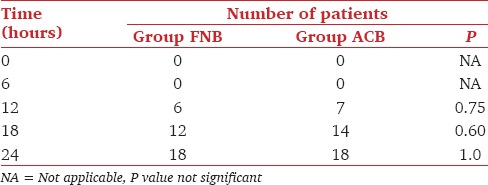
The difference between both the groups regarding NRS [Table 3] and total dose of rescue analgesia [Table 4] was statistically insignificant (P > 0.05). All patients were pain free in the first 6 h after block in both the groups. Also, the number of patients demanding rescue analgesia was not statistically significant thereafter [Table 5].
Table 3.
Comparison ofnumerical rating scale for pain in both the groups
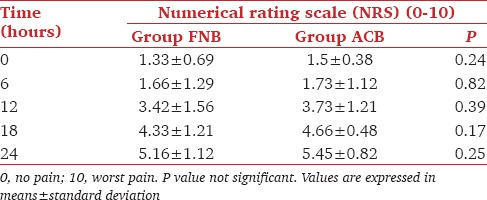
Table 4.
Total analgesic consumption (Tramadol in mg)
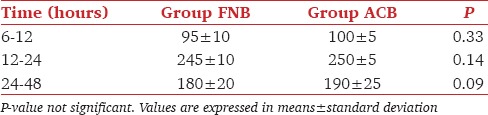
Table 5.
Comparison of number of patients demanding rescue analgesia in both groups
Patient satisfaction score was statistically significant on POD1 (P < 0.05), but the results were not significant on POD2 [Figure 1].
Figure 1.
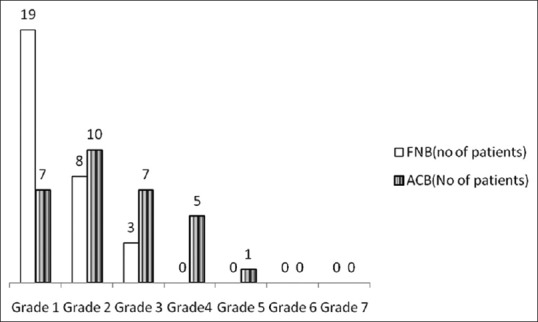
Comparison of patient satisfaction score on postoperative day 1 in both the groups. (Grade 1 to 7). P value <0.05, statistically significant
Discussion
We conducted the present study to evaluate the motor sparing effect of ACB versus FNB for arthroscopic ACLR. Our results demonstrated that ACB spares quadriceps muscle strength compared to FNB and reduces risk of falls. Patient satisfaction was however better with FNB.
FNB is a very commonly used technique of analgesia for postoperative pain relief for patients undergoing knee and below knee surgery, but as it causes weakness of quadriceps muscle, patient fall risk increases impairing early rehabilitation.[3,4,16] Hence, with FNB there always is a compromise between goals of adequate pain relief and muscle strength. Motor-sparing effect of block becomes important in the context of day care surgery. Unlike FNB, in ACB, the saphenous branch is blocked; making it a predominantly sensory block.[7,8] Adductor canal is the intermuscular space that lies in midthigh, between adductor longus, sartorius, and vastus medialis muscle. It contains only two branches of femoral nerve, saphenous nerve which is a purely cutaneous nerve, and nerve to vastus medialis.[7]
Till now, many studies have demonstrated the efficacy of ACB in providing adequate analgesia after knee arthroplasty.[8,9,10,11,12,13,14] There are few studies that have compared ACB to FNB in knee arthroscopic surgeries.[15,17,18] Most of these studies are from outside India and have compared the motor sparing effects and quality of analgesia provided by either blocks in knee scopies. We decided to restrict our study to ACLR and include patient satisfaction score to the studied parameters. Conventionally, FNB has remained the mainstay for postoperative analgesia for knee surgeries with good pain control and patient satisfaction.[15,16,17,18] While ACB is highly advocated for day care surgeries, we decided to study it in arthroscopic ACLR, which in our institute is an inpatient procedure. The primary outcomes of our study, i.e., quadriceps motor strength was measured by determining patient's ability to perform SLR test with the patient in a supine position.[13] On POD1, quadriceps muscle strength was assessed with the help of TUG test.[16] The duration of motor weakness with FNB was up to POD1. This is in congruence with other studies.[13,16] Therefore, FNB may not be the preferred technique of choice for day care knee scopies. ACB, although claimed to be a pure sensory block, may at times result in partial motor weakness. This is attributed to blockade of nerve to vastus medialis that lies in the adductor canal. Nevertheless, the chances of blocking the nerve to vastus medialis depends on the site of injection; i.e., paralysis is more if the ACB is carried out near the hiatus of adductor canal.[15]
Jaeger et al. and Kim et al. also demonstrated similar results.[7,12] The study by Jaeger et al. concluded that FNB reduces motor strength by 49% whereas ACB reduces it only by 8%, which was not considered functionally important.[7]
Chisholm et al. conducted a study comparing both the blocks on adequate pain control following ACLR.[17] They stated that there was no significant difference between the two groups in pain score and opioid consumption within postoperative 24 hours. However, they did not assess quadriceps weakness. A study by Faraj et al. suggested that ACB preserves quadriceps strength and provides noninferior postoperative analgesia for outpatients undergoing ACLR.[18] Our results are in concordance with these two studies. In another study, Mohammad et al. concluded that despite better preservation of quadriceps muscle power in ACB than FNB; VAS score was higher in ACB group.[15] In contradiction, our results reveal that pain relief was comparable in both the groups.
Persistent paralysis in FNB group delayed the assessment of motor function during the postoperative period.[19,20] Severity of pain and motor power are interrelated, and improving one factor impairs the other. This may explain better satisfaction score in the FNB group.[17,21,22]
Due to harvesting of graft, orthopedic surgeons in our institute do not prefer to ambulate the patient on the day of the surgery. Hence, motor sparing effect of ACB becomes less relevant. Although the analgesia provided by ACB is comparable to that of FNB, we found patient satisfaction score better with FNB. Consequently, the choice between ACB and FNB will depend on anesthetist's discretion and whether the procedure is day care or an indoor surgery. In addition, saphenous nerve block being pure sensory is amenable only to ultrasonography approach limiting; thereby limiting its accessibilty to all.
There are certain limitations of our study. We did not use dynamometer for assessing motor strength, which would have been more accurate. Our study results are restricted for in-patient ACLR surgeries only. The objectives for day care surgery are different and our study findings cannot be extrapolated for using a particular block in day-care surgery.
Conclusion
We studied ACB versus FNB in ACL repair for indoor patients. ACB, although epochal for its motor sparing effect, also provides analgesia comparable to FNB. However, we found patients' satisfaction better with FNB. Consequently, for arthroscopic ACLR, under general anesthesia either block may be used provided early ambulation is not desired.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Bollen SR, Scott BW. Rupture of the anterior cruciate ligament – A quiet epidemic? Injury. 1996;27:407–9. doi: 10.1016/0020-1383(96)00033-2. [DOI] [PubMed] [Google Scholar]
- 2.American Society of Anesthesiologists Task Force on Acute Pain Management. Practice guidelines for acute pain management in perioperative settings: An updated report by the American Society of Anesthesiologists Task Force on Acute Pain Management. Anesthesiology. 2012;116:248–73. doi: 10.1097/ALN.0b013e31823c1030. [DOI] [PubMed] [Google Scholar]
- 3.IIfeld BM, Duke KB, Donohue MC. The association between lower extremity continuous peripheral nerve blocks and patients falls after knee and hip arthroplasty. AnesthAnalg. 2010;111:1552–4. doi: 10.1213/ANE.0b013e3181fb9507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kandasami M, Kinninmonth AW, Sarungi M, Baines J, Scott NB. Femoral nerve block for total knee replacement – A word of caution. Knee. 2009;16:98–100. doi: 10.1016/j.knee.2008.10.007. [DOI] [PubMed] [Google Scholar]
- 5.Manickam B, Perlas A, Duggan E, Brull R, Chan VW, Ramlogan R. Feasibility and efficacy of USG guided block of saphenous nerve in the adductor canal. RegAnesth Pain Med. 2009;34:578–80. doi: 10.1097/aap.0b013e3181bfbf84. [DOI] [PubMed] [Google Scholar]
- 6.Charous MT, Madison SJ, Suresh PJ, Sandhu NS, Loland VJ, Mariano ER, et al. Continuous femoral nerve blocks: Varying local anesthetic delivery method (bolus versus basal) to minimize quadriceps motor block while maintaining sensory block. Anesthesiology. 2011;115:774–81. doi: 10.1097/ALN.0b013e3182124dc6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jaeger P, Neilsen ZJ, Henningsen MH, Hilsted KL, Mathiesen O, Dahl JB. Adductor canal block versus femoral nerve block and quadriceps muscle strength: A randomized, double blind, patient controlled, crossover study in healthy volunteers. Anesthesiology. 2013;118:409–15. doi: 10.1097/ALN.0b013e318279fa0b. [DOI] [PubMed] [Google Scholar]
- 8.Lund J, Jenstrup MT, Jaeger P, Sorensen AM, Dahl JB. Continuous adductor canal blockade for adjuvant post operative analgesia after major knee surgery: Preliminary results. ActaAnesthesiolScand. 2011;55:14–9. doi: 10.1111/j.1399-6576.2010.02333.x. [DOI] [PubMed] [Google Scholar]
- 9.Johnson RL, kopp SL, Hebl JR, Erwin PJ, Mantilla CB. Falls and major orthopaedic surgery with peripheral nerve blockade: A systematic review and Meta analysis. Br J Aneasth. 2013;110:518–28. doi: 10.1093/bja/aet013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Grevstad U, Mathiesen O, Lind T, Dahl JB. Effect of adductor canal block on pain in patients with severe pain after total knee arthroplasty: A randomized study in individual patient analysis. Br J Anaesth. 2014;112:912–9. doi: 10.1093/bja/aet441. [DOI] [PubMed] [Google Scholar]
- 11.Andersen HL, Gym J, Moller L, Christensen B, Zaric D. Continuous saphenous nerve block as supplement to single dose local infiltration analgesia for post operative pain management after total knee arthroplasty. RegAnaesth Pain Med. 2013;38:106–11. doi: 10.1097/AAP.0b013e31827900a9. [DOI] [PubMed] [Google Scholar]
- 12.Kim DH, Lin Y, Goytizolo EA, Kahn RL, Maalouf DB, Manohar A, et al. Adductor canal block versus femoral nerve block for total knee arthroplasty: A prospective, randomized, controlled trail. Anaesthesiology. 2014;120:540–50. doi: 10.1097/ALN.0000000000000119. [DOI] [PubMed] [Google Scholar]
- 13.Mudumbai SC, Kim TE, Howard SK, Workman JJ, Giori N, Woolson S, et al. Continuous adductor canal blocks are superior to continuous femoral nerve blocks in promoting early ambulation after TKA. ClinOrthopRelat Res. 2014;472:1377–83. doi: 10.1007/s11999-013-3197-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang H, Boctor B, Vermer J. The effect of single injection femoral nerve block on rehabilitation and length of hospital stay after total knee replacement. Reg Anesth Pain Med. 2002;27:139–44. doi: 10.1053/rapm.2002.29253. [DOI] [PubMed] [Google Scholar]
- 15.El Ahl MS. Femoral nerve block versus adductor canal block for post operative pain control after ACLR: A randomized controlled double blind study. Saudi J Anesth. 2015;9:279–82. doi: 10.4103/1658-354X.154708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hegazy NA, Sultan SS. Comparison between effect of adductor canal block and femoral nerve block on early post operative course in TKA: A prospective double blind randomized controlled study. Ain Shams J Anaesthesiol. 2015;8:124–8. [Google Scholar]
- 17.Chisholm MF, Bang H, Maalouf DB, Marcello M, Lotano MA, Marx RG, et al. Post operative Analgesia with saphenous nerve block appears equivalent to femoral nerve block in ACLR. HSSJ. 2014;10:245–51. doi: 10.1007/s11420-014-9392-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Abdallah FW, Whelan DB, Chan VW, Prasad GA, Endersby RV, Theodoropolous J, et al. Adductor canal block provides non inferior analgesia and superior quadriceps muscle strength compared with femoral nerve block in ACLR. Anaesthesiology. 2015;124:1053–64. doi: 10.1097/ALN.0000000000001045. [DOI] [PubMed] [Google Scholar]
- 19.Kwofie MK, Shastri UD, Gadsden JC, Sinha SK, Abrams JH, Xu D, et al. The effect of USG guided adductor canal block on quadriceps muscle strength and fall risk: A blinded, randomized trial of volunteers. RegAnesth Pain Med. 2013;38:312–5. doi: 10.1097/AAP.0b013e318295df80. [DOI] [PubMed] [Google Scholar]
- 20.Jenstrup MT, Jaeger P, Lund J, Fomsgaard JS, Bache S, Mathiesen O, et al. Effects of adductor canal blockade on pain and ambulation after TKA: A randomized study. ActaAnaesthesolScand. 2012;56:357–64. doi: 10.1111/j.1399-6576.2011.02621.x. [DOI] [PubMed] [Google Scholar]
- 21.Patterson ME, Bland KS, Thomas LC, Elliott CE, Soberon JR, Nossaman BD, et al. The adductor canal block provides effective analgesia similar to femoral nerve block in patient's undergoing TKA. J ClinAnesth. 2015;27:39–44. doi: 10.1016/j.jclinane.2014.08.005. [DOI] [PubMed] [Google Scholar]
- 22.Ludwigson JL, Tillmans SD, Galgon RE, Chambers TA, Heiner JP, Schroeder KM. A comparison of single shot adductor canal block versus femoral nerve block for TKA. J Arthroplasty. 2016;31:741. doi: 10.1016/j.arth.2015.09.017. [DOI] [PubMed] [Google Scholar]


