Abstract
Patient: Male, 12
Final Diagnosis: Carotid jugular fistula
Symptoms: Tinnitus
Medication: —
Clinical Procedure: —
Specialty: Surgery
Objective:
Rare disease
Background:
There is a paucity of published literature on carotid-jugular fistulae in children. These injuries are uncommon in the pediatric age group and most of the current practice in managing such injuries is extrapolated from similar injuries in the adult population.
Case Report:
We report a case of an acquired carotid-jugular fistula (CJF) following penetrating neck trauma in a 12-year-old male, treated by minimally invasive endovascular covered stent. Successful endovascular management was achieved in this case with anatomical and symptomatic resolution at 6 weeks and normal duplex ultrasound at 18 months.
Conclusions:
The rarity of carotid-jugular fistulae in children means there is a lack of consensus for the appropriate management in the available literature. This case report adds to the evidence for endovascular management of this condition in a pediatric population.
MeSH Keywords: Carotid Artery Injuries, Endovascular Procedures, Jugular Veins, Vascular System Injuries
Background
Endovascular techniques have revolutionized the management of vascular trauma, especially in cases where the nature of open surgery carries particular risk. Penetrating neck trauma can be one of these cases and is a challenging condition requiring an expedited approach. Fortunately, these injuries in children are rare, but this creates a further challenge for the vascular surgeon, as current evidence for therapeutic management is extrapolated from similar injuries in the adult population and therefore may not be applicable [1]. We report a case of an acquired carotid-jugular fistula (CJF) following penetrating neck trauma in a 12-year-old male, treated by minimally invasive endovascular covered stent.
Case Report
A 12-year-old male initially presented to the emergency department of a district general hospital with acute hemorrhage following a penetrating stab wound to the left lateral aspect of his neck, above the angle of the mandible (Zone III). This was managed locally (the exact nature of this is unknown) and the patient was discharged seemingly well and asymptomatic. He was referred to our clinic 6 months later presenting with a pulsatile neck swelling, tinnitus below the left ear, blackouts, and inappropriate fatigability after low-intensity exercise.
Clinical examination revealed an oblique scar 2.5 cm in length anterior to the upper border of the left sternocleidomastoid muscle and posterior to the angle of the mandible (Figure 1). The patient had an obvious underlying soft swelling with a palpable thrill and a continuous machinery murmur associated with a blowing bruit. Neurological examination was unremarkable.
Figure 1.

Scar from the initial injury.
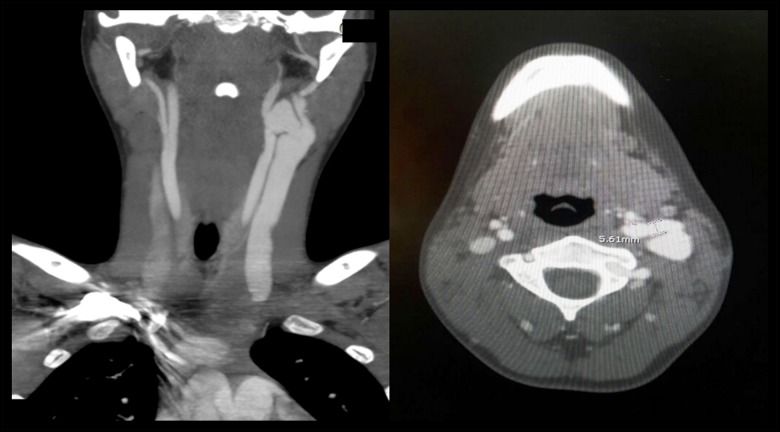
Duplex ultrasonography (DUS) demonstrated an arteriovenous fistula (AVF) between the left internal carotid artery (ICA) and the left internal jugular vein (IJV) 18 mm above the carotid bifurcation. Subsequent 3D CT angiography (CTA) confirmed these findings as well as huge dilatation of the IJV associated with aneurysmal swelling at the fistula site (Figure 2).
Figure 2.
Coronal and axial CTA image of the neck demonstrating the left CJF and dilatation of the IJV. CTA – CT angiography; CJF – carotid-jugular fistula; IJV – internal jugular vein.
Given the patient’s unfavorable experience with the primary surgery and subsequent reluctance for further open operative management, together with the presence of scarring in the neck and the challenging distal location of the fistula, which was just proximal to the base of the skull, minimally invasive endovascular management under general anesthesia was deemed the most appropriate course of action.
Procedure
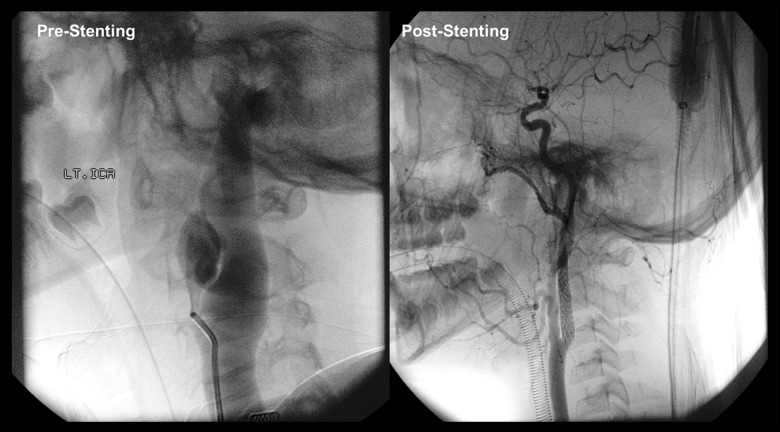
The procedure was performed in the angiography suite using the Philips Allura XPer FD 20/15 x-ray system. The patient was given 100 mg aspirin and 75 mg clopidogrel before induction of anesthesia. The right common femoral artery (CFA) was punctured under ultrasound guidance and a 6 French sheath inserted followed by intra-arterial administration of 3000 IU of heparin. Selective left carotid angiogram demonstrated a high flow AVF measuring 5 mm in diameter and 12 mm in length between the left ICA and IJV with a prominent dilatation of the IJV (Figure 3). Following the diagnostic angiogram, a small micro catheter was advanced over the wire to cross the lesion. Over an exchange wire the self-expanding Fluency Plus stent graft (BARD Peripheral Vascular, Tempe, AZ, USA) measuring 6 mm in diameter and 4 cm in length was successfully deployed into the ICA with complete obliteration of the fistulous tract and satisfactory apposition of the stent (Figure 3).
Figure 3.
Pre- and post-stenting left carotid angiogram.
Immediately post procedure, the swelling in the neck and the palpable thrill were resolved. Recovery was unremarkable, and the patient was discharged after 3 days on 100 mg aspirin and 75 mg clopidogrel which was continued for 6 weeks. Followed by lifelong aspirin 100 mg on daily basis.
Post procedure follow-up
CTA at 4 weeks revealed satisfactory position of the stent, a widely patent ICA and complete resolution of the CJF. At the 6-week outpatient follow-up, the patient was completely asymptomatic.
DUS at 18 months demonstrated a patent stent with normal flow velocities (peak systolic velocities (PSV)=85 cm/sec, end diastolic velocities (EDV)=25 cm/sec) and no evidence of AVF (Figure 4). The patient remains monitored by our carotid surveillance every 6 months with a duplex carotid ultrasound performed in our vascular lab.
Figure 4.
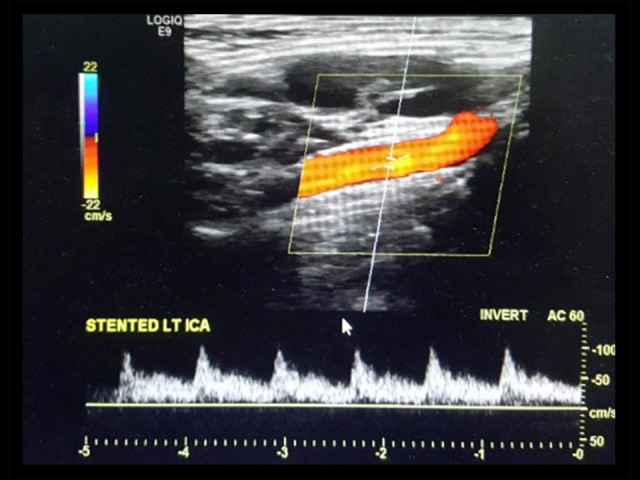
DUS demonstrating normal flow velocities through left ICA, patent IJV and resolution of the CJF.
DUS – duplex ultrasonography; ICA – internal carotid artery; IJV – internal jugular vein.
Discussion
Carotid jugular fistulas (CJF) are an uncommon clinical entity [2–4]. Although rare, they can be congenital, however, the majority of pediatric cases are due to neck trauma, with penetrating injuries the most common of these [3,5]. Their presentation, which depends on the hemodynamic effects and degree of arterial to venous shunting, can be subtle and this often leads to delays in diagnosis of weeks or even months following the initial injury [2,4,6].
Symptoms can vary from minor to intractable tinnitus, arrhythmias, heart failure, cerebral embolization and pseudo aneurysm formation, depending on the flow through the AVF and its proximity to the heart [2–6]. Any penetrating neck trauma should warrant a high index of suspicion of a CJF and this is key for timely diagnosis. DUS is usually the initial diagnostic modality; however, it is operator dependent and cannot completely exclude CJF [3]. CTA or magnetic resonance angiography (MRA) is therefore usually performed to provide the necessary imaging required to plan treatment which aims to seal the fistula and maintain forward antegrade flow to the brain [5,7,8]. Conventional surgical ligation, division of the fistula, and vascular reconstruction was traditionally the treatment of choice, but this carries a significant morbidity and requires technical expertise owing to the small vessel diameter, relative surgical inaccessibility, and potentially scarring in the not infrequent case of delayed diagnosis [8].
There is a variety of endovascular techniques for treating CJFs in the published literature varying from coil embolization to covered stent graft placement [3,8,9]. These techniques can be advantageous as they can be done under local anesthesia allowing intra-procedural cerebral function monitoring and can treat pathology at sites which are otherwise surgically inaccessible [10]. However, they do carry unique concerns when dealing with a pediatric patient; technically the procedures can be challenging. Both access and target vessels have significantly smaller diameters than those encountered in adult patients, increasing the risk of procedural complications. The rarity of presentation means there is no current consensus regarding therapeutic management nor follow-up, including antiplatelet regimes [1]. Moreover, technical issues related to endovascular advancement of the guidewire across the distal carotid can be very challenging particularly when the shunt is substantial, and the communicating fistula is aneurysmal.
Close follow-up of these patients is clearly imperative; in-stent re-stenosis and stent mismatch are pertinent potential complications in a growing child that can be managed with re-dilatation without clinical consequence, as long as they are detected early [11]. The development of biodegradable stents offers an exciting potential solution to avoid the stent-complications unique to the pediatric patient and could make endovascular techniques universally applicable in this population [12].
The reported morbidity of carotid stent insertion for vascular trauma is encouraging, with a 3.5% risk of stroke, though long-term patency data is not available, overall mortality is less than 1% [1]. This combined with the limited vessel tortuosity in pediatric patients, makes endovascular stent placement a viable option in this age group.
Conclusions
This case demonstrated the successful management of a CJF secondary to vascular neck trauma in a pediatric patient. The safety profile and minimally invasive nature of endovascular techniques make them a viable option in pediatric patients, especially for lesions that are not easily accessible through an open approach. Yet long-term patency and follow-up plans remains unknown especially in the pediatric age group.
Acknowledgments
Dr Ma’moon Al Omari, MD, Department of Radiology, Jordan University of Science and Technology, Irbid, Jordan.
Footnotes
conflict of interest
None.
References:
- 1.Lucas O, Naseem H-u-R, Davies JM, et al. Endovascular treatment of a carotid artery pseudoaneurysm due to penetrating trauma in a pediatric patient. J Pediatr Surg Case Rep. 2017;19(Suppl. C):19–21. [Google Scholar]
- 2.Lambropoulos V, Lazaridis I, Melas N, et al. Penetrating neck trauma in a 4-year-old child. Case Reports in Clinical Medicine. 2015;4:145–50. [Google Scholar]
- 3.Chi M-H, Wang N-K, Lu Y-Y. Treatment of a rare congenital external carotid arteriovenous fistula with transcatheter coil embolization. Acta Cardiol Sin. 2010;26:272–75. [Google Scholar]
- 4.Ezemba N, Ekpe EE, Ezike HA, Anyanwu CH. Traumatic common carotidjugular fistula: Report of 2 cases. Texas Heart Inst J. 2006;33(1):81–83. [PMC free article] [PubMed] [Google Scholar]
- 5.Erdi F, Kaya B, Keskin F, et al. Congenital carotid-jugular fistula in a child: A case report. Vasc Endovasc Surg. 2013;48(3):256–58. doi: 10.1177/1538574413513848. [DOI] [PubMed] [Google Scholar]
- 6.Kakkar S, Angelini P, Leachman R, Cooley DA. Successful closure of post-traumatic carotid-jugular arteriovenous fistula complicated by congestive heart failure and cerebrovascular insufficiency. Cardiovasc Dis. 1979;6(4):457–62. [PMC free article] [PubMed] [Google Scholar]
- 7.Baker JB, Ingraham CR, Fine GC, et al. Paediatric jugular vein aneurysm (phlebectasia): Report of two cases and review of the literature. Radiol Case Rep. 2017;12(2):391–95. doi: 10.1016/j.radcr.2016.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jang HW, Byun WM, Kim JW, Chang CH. Endovascular treatment of traumatic carotid-jugular fistula: Report of two cases. J Korean Radiol Soc. 2007;56(2):109–13. [Google Scholar]
- 9.Self ML, Mangram A, Jefferson H, et al. Percutaneous stent-graft repair of a traumatic common carotid-internal jugular fistula and pseudoaneurysm in a patient with cervical spine fractures. J Trauma. 2004;57(6):1331–34. doi: 10.1097/01.ta.0000151256.20476.7e. [DOI] [PubMed] [Google Scholar]
- 10.Lee TS, Ducic Y, Gordin E, Stroman D. Management of carotid artery trauma. Cranialmaxillofac Trauma Reconstr. 2014;7(3):175–89. doi: 10.1055/s-0034-1372521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sebastien H, Alban B, Zakaria J, et al. Stents in paediatric and adult congenital interventional cardiac catheterization. Arch Cardiovasc Dis. 2014;107:462–75. doi: 10.1016/j.acvd.2014.06.005. [DOI] [PubMed] [Google Scholar]
- 12.Di Mario C, Caiazzo G. Biodegradable stents: The golden future of angioplasty? Lancet. 2015;385(9962):10–12. doi: 10.1016/S0140-6736(14)61636-6. [DOI] [PubMed] [Google Scholar]