Abstract
Patient: Male, 39
Final Diagnosis: Infective endocarditis
Symptoms: Cough
Medication: —
Clinical Procedure: None
Specialty: Critical Care Medicine
Objective:
Unexpected drug reaction
Background:
Right-sided infective endocarditis is a classic complication of intravenous drug abuse. Without timely bactericidal antibiotics, the disease process can progress to septic pulmonary emboli. Rarely, a pneumothorax can occur as a result of the emboli, and progressive persistent valvular disease may require a valve replacement. Tricuspid valve replacement has a high morbidity rate even in stable patients.
Case Report:
We present a case of tricuspid valve replacement in a 39-year-old man with peripheral intravenous drug abuse who had bilateral pneumothoraces secondary to septic pulmonary emboli originating on large tricuspid valve infected vegetations. The patient died 21 days after the valve replacement.
Conclusions:
Tricuspid valve replacement is an especially dangerous procedure in intravenous drug abusers who present with bilateral pneumothoraces and advanced cardiopulmonary pathology.
MeSH Keywords: Endocarditis, Pneumothorax, Pulmonary Embolism, Sepsis, Tricuspid Valve Insufficiency
Background
Infective endocarditis (IE) is a life-threatening infectious disease involving endocardial surfaces of the heart. The clinical manifestations can be highly variable but typically include a combination of fever, positive blood cultures, and the presence of a valvular vegetation on echocardiography [1].
Injecting drug use (IDU) is an important risk factor for developing right-sided IE, mostly involving the tricuspid valve [2]. Staphylococcus aureus is the predominant causative micro-organism for right-sided IE, occurring in 60–90% of cases. Pseudomonas aeruginosa, other gram-negative microorganisms, fungi, enterococci, streptococci, and polymicrobial infections occur less frequently.
Complications of right-sided IE are frequent and include valvular insufficiency, abscess formation, and septic pulmonary embolic (SPE) events. [3] Secondary spontaneous pneumothorax (PTX) is a rare but established complication of SPE [4]. Right-sided IE more often requires right heart valve replacement, with an approximately 10–20% surgical mortality rate [5]. However, this mortality rate does not differentiate between those patients treated for recent bilateral PTX and those without this lung complication. We present the case of a 39-year-old male IVDU (intravenous drug user) who presented with tricuspid IE and had both septic pulmonary emboli and bilateral spontaneous pneumothorax. Because of advancing IE, urgent tricuspid surgery was performed and 21 day later the patient died.
Case Report
We present the case of a 39-year-old, HIV (human immunodeficiency virus)-negative male with a 4-year history of cocaine and peripheral intravenous drug abuse who presented to an outside facility with altered mental status (AMS), fever, and hemoptysis. Outside blood cultures grew methicillin-sensitive Staphylococcus aureus (MSSA) and a transesophageal echocardiogram showed 1.8×1.4 cm tricuspid valve (TV) vegetation with moderate tricuspid insufficiency (Figure 1). Nafcillin and gentamycin were initially administered. On arrival, he had a temperature of 37.6°C, heart rate of 105 bpm, respiratory rate of 27/min, and oxygen saturation of 91% on assist control ventilation with 40% FiO2. Physical examination revealed diminished breath sounds bilaterally and a grade 2 systolic murmur along the left sternal border. White blood cell count was 24 400/ml, creatinine 0.76 mg/dL, BUN (blood urea nitrogen) 31 mg/dL, and albumin level was 2.1 g/dl. Chest radiography (CXR) demonstrated large bilateral subpulmonic pneumothoraces, with diffuse patchy opacities throughout the aerated lungs (Figure 2). A diagnosis of TV endocarditis with subsequent pulmonic embolization resulting in bilateral pneumothoraces was made. Emergent placement of chest tubes resulted in lung expansion and cardiopulmonary stabilization. Another set of blood cultures returned no growth on hospital day 2. Additional CXR and computed tomography performed 3 days after admission showed lung expansion with persistent patchy infiltrates and multiple bilateral cavitary lesions, determined to be from pulmonary septic embolization. Due to the large vegetation size and evidence of continued multiple pulmonary embolization events, he underwent a prosthetic TV replacement on day 4 of hospitalization (Edwards Manga Model 7300tfx, Edwards Lifesciences, Irvine, CA, USA). Throughout the hospital stay, he spiked fevers and became progressively more hemodynamically unstable. His antimicrobial regimen was adjusted multiple times, including vancomycin and meropenem for possible extended-spectrum beta-lactamase gram-negative rods, prior MSSA, and ventilator-associated serratia pneumonia. Two additional chest tubes were placed bilaterally, and continuous renal replacement therapy was administered secondary to worsening kidney function, most likely vasopressor-associated acute tubular necrosis. The patient died 21 days after the TV replacement, having never left the ICU.
Figure 1.
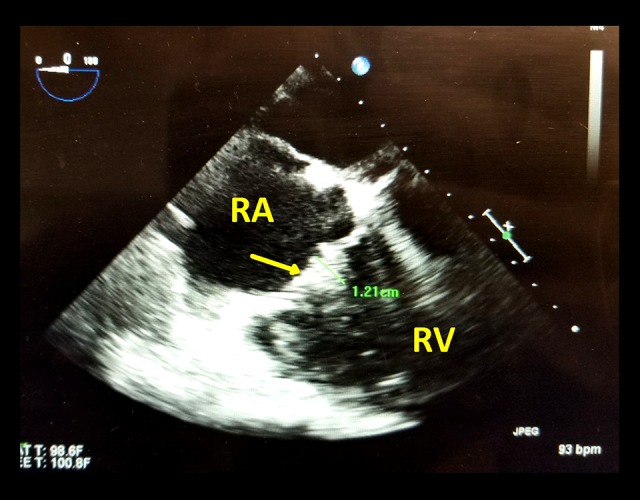
Transesophageal echocardiography of right ventricular (RV) inflow (from parasternal long-axis view).
RA – right atrium, RV – right ventricle, and arrow is at the vegetation lodged on the tricuspid valve (1.2 cm).
Figure 2.
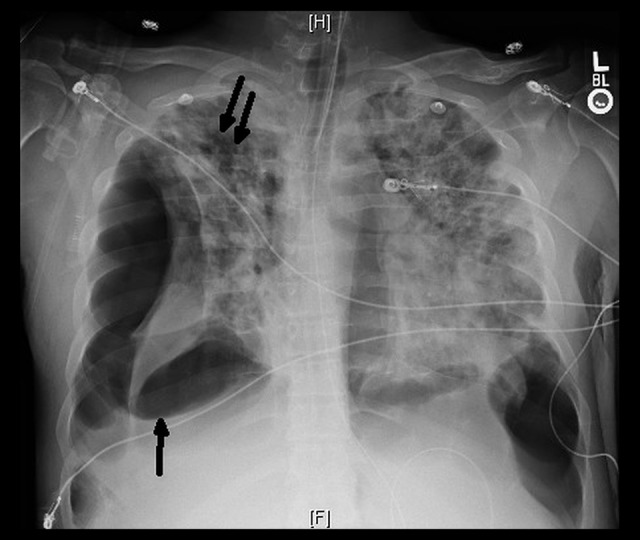
Chest radiography (CXR) demonstrating large bilateral subpulmonic pneumothoraces at the single black arrow, with diffuse patchy opacities throughout the aerated lungs at the double black arrows.
Discussion
This case is unique in 3 ways. First, PTX caused by septic pulmonary emboli from right-sided endocarditis is uncommon, especially when it is bilateral [4]. Neither the exact incidence rate nor the exact pathophysiologic developmental process is known. However, PTX appears to be a more common complication when the etiologic microbiological organism is Staphylococcus aureus. This virulent pathogen is found to account for around 70% of right-sided IE, with blood cultures positive in a high proportion of cases [6–8]. Thus, it is possible that the formation of bronchopulmonary fistulas results from an embolic bacterial cavity containing Staphylococcus aureus. Whatever the cause, in our case, multiple cavitary lesions secondary to septic pulmonary emboli from the IE ruptured, which lead to the PTX. The widespread pulmonary destruction seen in this case at presentation possibly reflects his choice to delay seeking treatment. One other important clinical variable is that multiple pulmonary septic emboli are very strongly associated with advanced TV disease.
Second, this case was characterized by persistent and progressive TV disease despite appropriate bactericidal therapy. Typically, IE can be treated medically [9] but in this instance, the pathological process deteriorated until there was need for urgent surgery. The vegetations on the leaflet were large, and subcutaneous edema and micro-abscesses became apparent at the time of surgery. Therefore, valve repair was not an option, and TV replacement was required 4 days after admission. TV replacement is a procedure with high morbidity and mortality but is urgent in certain situations such as locally uncontrolled infection [10].
Third, this patient died 3 weeks after surgery. The early mortality rate for TV replacement is 10–20% but this does not specifically define those patients with PTX, IE, and renal insufficiency. We performed a MEDLINE search of the English language literature from January 1, 1966, to October 20, 2017, using the keywords “Bilateral Pneumothoraces,” “Septic Pulmonary Emboli,” “right-sided Infective endocarditis,” and “tricuspid valve replacement.” However, we could find no cases of bilateral pneumothoraces from septic pulmonary emboli that underwent urgent tricuspid valve replacement; thus, mortality rates in similar groups are not known. Many of the patients reported in mortality rates of TV replacement had non-infectious valvular disease rather than IE and probably the acute and chronic organ system damage seen in this patient significantly increased his surgical risk. Moreover, there is an increased risk in prosthetic heart valves of endocarditis and post-surgical complications, as well as increased mortality risk and complications due to clotting risks. The outstanding variable in the surgical risk to this patient was his delay in seeking health care, which likely can be measured by the advanced bilateral pulmonary cavitation, pneumothoraces, and degree of systemic organ system disruption. It is possible the PTX may, in fact, be a marker for advanced pulmonary disease from SPE secondary to TV endocarditis, and counseling of these patients about the risks of TV replacement in the face of a PTX should be adjusted accordingly. One other pertinent clinical variable is that IVDA has a cumulative effect on the TV [11].
Conclusions
Our case illustrates the effect of delayed intervention in IE caused by MSSA. SPE progressed to PTX and multisystem involvement. Uncontrolled TV disease resulted in medical failure and a requirement for surgical intervention. The overall unstable condition and advanced disease prevented recovery. TV replacement in unstable patients with PTX may have a much higher postoperative risk than fine-tuned valve recipients, and families should be counseled accordingly.
Acknowledgments
Kauser Akhter, MD.
Footnotes
Conflict of interest
None.
References:
- 1.Cahill TJ, Prendergast BD. Infective endocarditis. Lancet. 2016;387(10021):882. doi: 10.1016/S0140-6736(15)00067-7. [DOI] [PubMed] [Google Scholar]
- 2.Crane LR, Levine DP, Zervos MJ, Cummings G. Bacteremia in narcotic addicts at the Detroit Medical Center. I. Microbiology, epidemiology, risk factors, and empiric therapy. Rev Infect Dis. 1986;8:364–73. doi: 10.1093/clinids/8.3.364. [DOI] [PubMed] [Google Scholar]
- 3.Yuan S-M. Right-sided infective endocarditis: Recent epidemiologic changes. Int J Clin Exp Med. 2014;7(1):199–218. [PMC free article] [PubMed] [Google Scholar]
- 4.Sheu C-C, Hwang J-J, Tsai J-R, et al. Spontaneous pneumothorax as a complication of septic pulmonary embolism in an intravenous drug user: A case report. Kaohsiung J Med Sci. 2006;22:89–93. doi: 10.1016/S1607-551X(09)70226-8. [DOI] [PubMed] [Google Scholar]
- 5.Musci M, Siniawski H, Pasic M, et al. Surgical treatment of right-sided active infective endocarditis with or without involvement of the left heart: 20-year single center experience. Eur J Cardiothorac Surg. 2007;32:118–25. doi: 10.1016/j.ejcts.2007.02.034. [DOI] [PubMed] [Google Scholar]
- 6.Lowy FD. Staphylococcus aureus Infections. N Engl J Med. 1998;339(8):520–32. doi: 10.1056/NEJM199808203390806. [DOI] [PubMed] [Google Scholar]
- 7.DiNubile MJ. Abbreviated therapy for right-sided Staphylococcus aureus endocarditis in injecting drug users: The time has come? Eur J Clin Microbiol Infect Dis. 1994;13(7):533–34. doi: 10.1007/BF01971302. [DOI] [PubMed] [Google Scholar]
- 8.Moss R, Munt B. Injection drug use and right sided endocarditis. Heart. 2003;89(5):577–81. doi: 10.1136/heart.89.5.577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Baddour LM, Wilson WR, Bayer AS, et al. American Heart Association Committee on Rheumatic Fever. Endocarditis. Kawasaki Disease of the Council on Cardiovascular Disease in the Young. Council on Clinical Cardiology. Council on Cardiovascular Surgery and Anesthesia. Stroke Council Infective endocarditis in adults: diagnosis, antimicrobial therapy, and management of complications: A scientific statement for health-care professionals from the American Heart Association. Circulation. 2015;132(15):1435–86. doi: 10.1161/CIR.0000000000000296. [DOI] [PubMed] [Google Scholar]
- 10.Civelek A, Ak K, Akgün S, et al. Tricuspid valve replacement: An analysis of risk factors and outcomes. Thorac Cardiovasc Surg. 2008;56(8):456–60. doi: 10.1055/s-2008-1038730. [DOI] [PubMed] [Google Scholar]
- 11.Pons-Lladó G, Carreras F, Borrás X, et al. Findings on Doppler echocardiography in asymptomatic intravenous heroin users. Am J Cardiol. 1992;69:238–41. doi: 10.1016/0002-9149(92)91312-r. [DOI] [PubMed] [Google Scholar]


