Abstract
Patient: Male, 60
Final Diagnosis: Dengue cerebellitis
Symptoms: Dizziness • fever • headaches • vomiting
Medication: —
Clinical Procedure: Lumbar puncture
Specialty: Neurology
Objective:
Unusual clinical course
Background:
Dengue-associated neurological manifestations have recently been on the rise. Cerebellar syndrome complicating dengue fever has rarely been reported in the literature. We present a case report of dengue-associated cerebellar syndrome and performed a literature review to draw attention to this rare neurological complication.
Case Report:
A 60-year-old man presented with 4 days of fever, myalgia, arthralgia, headaches, and warning symptoms (persistent diarrhea and vomiting). He was admitted with serologically-confirmed dengue fever. He had been well until day 8 of illness, when he developed cerebellar signs and symptoms. The temporal relationship with the recent dengue fever suggested that he had dengue cerebellitis. He recovered well, with no neurological sequelae upon our clinic visit.
Conclusions:
Dengue cerebellitis is a rare but recognized manifestation, which should be considered in patients from endemic areas of dengue fever who develop cerebellar syndrome.
MeSH Keywords: Ataxia, Cerebellar Diseases, Dengue
Background
The incidence of dengue fever has grown exponentially around the globe in recent years. In Malaysia, dengue fever is a public health threat due to its alarming rise in morbidity and mortality rates. At present, there are 18 688 confirmed patients with dengue infection in Malaysia and 201 have died due to dengue [1]. With the escalating trend of dengue infection, atypical manifestations of dengue fever, such as dengue encephalitis, are also increasingly reported. We report a case of a diabetic patient with cerebellitis associated with dengue fever. Our literature review identified only 4 other similar cases, all from Sri Lanka. Our report underscores the importance of recognizing this rare neurological syndrome associated with dengue fever.
Case Report
A 60-year-old man presented to the Emergency Department with 4 days of fever, myalgia, arthralgia, headaches, and dengue warning symptoms (persistent diarrhea and vomiting). He lived in a dengue-prone area. He was on treatment for his type II diabetes mellitus, hypertension, dyslipidemia, and a previous stroke. He had presented with left upper limb weakness 5 years ago, which resolved within a few days. He could not recall his brain computed tomography (CT) results and had remained well with modified Rankin scale (mRS) of 0/6 upon discharge. His presenting vital signs, including glucose level, were stable. Apart from petechiae in his lower limbs, his physical examination was unremarkable. Full blood count revealed hemoglobin 15.1g/dL, hematocrit 43%, white blood cell 3.3×109/L, and platelet 81×109/L. His alanine transaminase was 59 U/L. Renal profile was normal. Dengue IgM was detected on day 5 of illness. Blood films for malarial parasites were repeatedly negative. A diagnosis of dengue fever was made and he was managed with intravenous fluids in the ward in view of his warning symptoms. A series of full blood count monitoring is summarized in Table 1.
Table 1.
Full blood count trend in the ward.
| Day of illness | Hemoglobin (g/dL) | Hematocrit (%) | White cell (109/L) | Platelet (109/L) |
|---|---|---|---|---|
| Day 4 | 15.1 | 43 | 3.3 | 81 |
| Day 5 | 13.7 | 41.6 | 3.0 | 53 |
| Day 6 | 14.6 | 42.4 | 4.3 | 34 |
| Day 7 | 14.3 | 41.3 | 7.1 | 66 |
| Day 8 | 15.8 | 45.8 | 8.9 | 92 |
| Day 9 | 14.2 | 40.9 | 7.5 | 148 |
He was well in the ward until day 8 of illness (in recovery phase). He suddenly complained of headaches, giddiness, and vomiting. On examination, he had nystagmus in all directions, bilateral dysmetria more prominent on the left and ataxic gait. His blood pressure was 150–160/80–90 mmHg during this acute episode. A preliminary diagnosis of acute brainstem stroke was entertained given his background of multiple underlying illnesses. The magnetic resonance imaging (MRI) of his brain revealed hyperintense signals at the right corona radiata and left frontal lobe in keeping with old stroke (Figures 1, 2). No abnormal signals were seen in his cerebellum, cerebellopontine angle, midbrain, and pons (Figure 3). His magnetic resonance angiogram (MRA) study was normal. Lumbar puncture was done and his cerebro-spinal fluids (CSF) showed normal opening pressure, cell count, and biochemistry. Dengue PCR (sent on day 9 of illness) was not detected from his CSF. Haemophilus influenzae, Neisseria meningitidis, and Streptococcus pneumoniae were not isolated from the CSF. Antigens of Cytomegalovirus, Epstein-Barr virus, herpes simplex virus 1 and 2, and varicella zoster virus were not detected by polymerase chain reaction (PCR) from his CSF. He tested negative from his serum for HIV, hepatitis, syphilis, varicella zoster, Epstein-Barr, herpes simplex, and mycoplasma.
Figure 1.
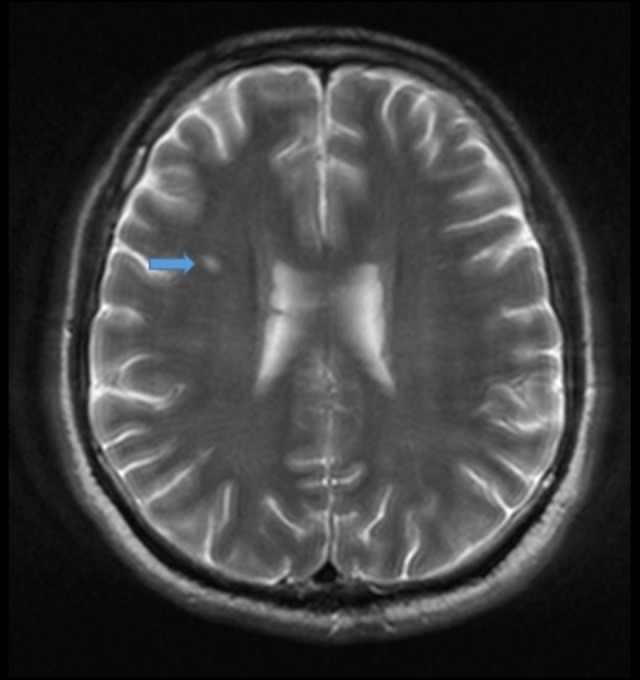
T2-weighted brain magnetic resonance imaging (MRI) reveals a hyperintense lesion in the right corona radiata (blue arrow).
Figure 2.
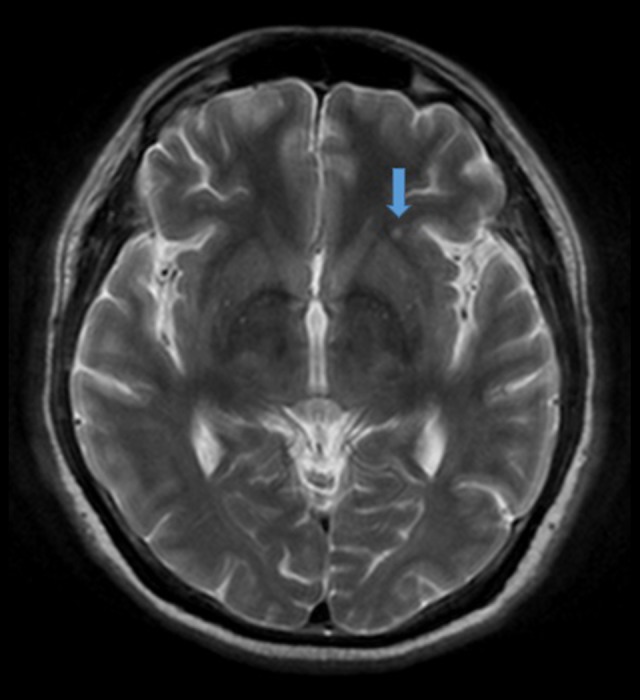
T2-weighted brain magnetic resonance imaging (MRI) reveals a hyperintense lesion in the left frontal lobe (blue arrow).
Figure 3.
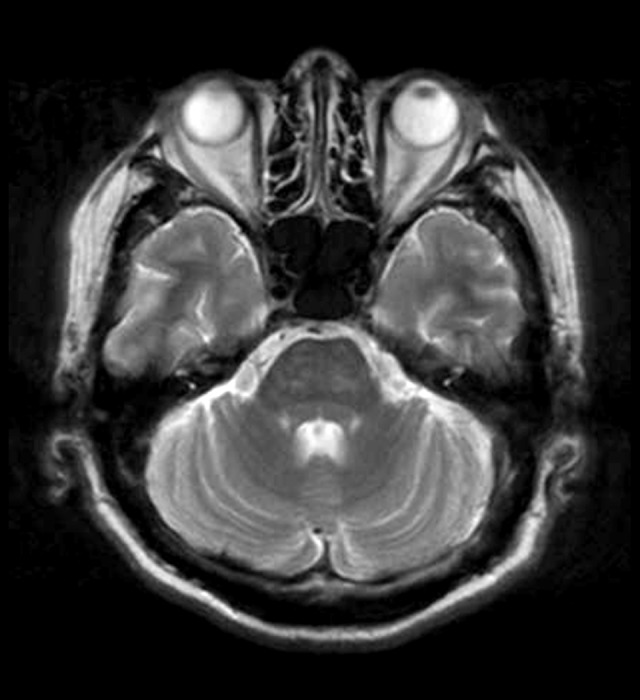
No abnormal signal intensity in the cerebellum in the T2-weighted brain magnetic resonance imaging (MRI).
He was managed with physiotherapy and rehabilitation therapy in the ward for 2 weeks. He was discharged with a walking frame. Twenty days after discharge, he could walk independently and all neurological signs resolved spontaneously.
Discussion
Dengue fever is a mosquito-borne viral disease transmitted principally by the mosquito Aedes aegypti. Dengue virus is a single-stranded RNA virus with 4 serological types [2]. The clinical manifestations of dengue fever are varied, ranging from self-limited infection to plasma leakage, hemorrhage, shock, or organ failure resulting in death. Atypical syndromes are increasingly recognized, such as neurological manifestations, myocarditis, acute kidney injury and cholecystitis [3].
According to Carod-Artal et al. [4], dengue fever can manifest with neurological features ranging from 0.5% to 21% of the cases presenting at hospital. Neurological manifestations associated with dengue fever can broadly be classified into encephalopathy, encephalitis, neuromuscular, and neuro-ocular complications. Among these manifestations, encephalopathy, encephalitis, Guillain-Barré syndrome, myositis, and maculopathy are commonly reported.
Cerebellar syndrome associated with dengue infection was first reported by Weeratunga et al. [5] as a case series in 2013 followed by Withana et al. [6] as a case report in 2014. Our case (the fifth case) and the literature review demonstrate that patients with dengue cerebellar syndrome tend to recover spontaneously without permanent neurological sequelae. The onset of symptoms ranged from 2 days to 2 weeks. Ataxia and bilateral nystagmus were present in all cases. Cerebellar signs resolved from 1 week to 2 months. It is noteworthy that there were no changes in the neuroimaging in all but 1 case. This may suggest a transient inflammation in dengue cerebellitis. Other differences are illustrated in Table 2.
Table 2.
Summary of the 5 cases of dengue cerebellar syndrome.
| Age | Sex | Phase of presentation | Cerebellar signs | Dengue serology | Brain MRI | CSF analysis | Duration of complete recovery | |
|---|---|---|---|---|---|---|---|---|
| Weeratunga et al. | 40 | Female | Critical | Dysarthria, bilateral nystagmus, bilateral limb and gait ataxia | IgM positive (both serum and CSF) | Normal | Normal | 2 months |
| Weeratunga et al. | 28 | Male | Post recovery | Bilateral vertical and horizontal nystagmus, gait ataxia | IgM positive (both serum and CSF) | Normal | Normal | 1 week |
| Weeratunga et al. | 25 | Male | Febrile | Bilateral nystagmus, dysmetria, severe ataxia | IgM positive (both serum and CSF) | Bilateral and symmetrical T2 hyperintense lesions in the cerebellum | Normal | 2 weeks |
| Withana et al. | 45 | Female | Febrile | Scanning dysarthria, horizontal nystagmus, bilateral dysmetria, dysdiadochokinesia more prominent on the right, ataxia, tendency to fall to the right | NS 1 Antigen and IgM positive (serum) | Normal | Not done | 17 days |
| Khoo | 60 | Male | Recovery | Nystagmus in all directions, bilateral dysmetria more prominent on the left, ataxia | IgM positive (serum); PCR negative (CSF) – taken on D9 of illness | Hyperintense signals in the right corona radiata and left frontal lobe suggestive of his previous stroke | Normal | 34 days |
The pathogenesis of neurological syndromes remains to be elucidated. Direct invasion of the virus and immune-mediated mechanisms are postulated to cause the neurological sequelae.
Several viral infections are reported to cause cerebellitis, such as varicella zoster, Epstein-Barr, herpes simplex, measles, HIV, and coxsackie [7]. Cerebellitis can be primary infective, post-infective, or post-vaccination. Among the 5 cases, 4 (including ours) are likely primary infective and 1 is likely post-infective.
Conclusions
Dengue-related cerebellitis, although rarely reported, is a recognized neurological manifestation. Clinicians should consider dengue infection as an etiology in patients with fever who live in endemic areas and develop cerebellar syndrome.
Dengue cerebellitis can occur in any phase of dengue fever and is self-limiting. Further studies are required to elucidate its pathophysiology.
Acknowledgments
The author would like to thank the staff of the Neurology Unit, Department of Medicine, Universiti Kebangsaan Malaysia Medical Center and Dr Siti Soraya Ab Rahman, Radiologist, from the Islamic Science University of Malaysia for her work in interpreting the MRI images.
Footnotes
Conflicts of interest
None.
References:
- 1. iDengue 2015. Available from: URL: http://idengue.remotesensing.gov.my/idengue/index.php.
- 2.Cheah WK, Ng KS, Marzilawati AR, et al. A review of dengue research in Malaysia. Med J Malaysia. 2014;69(A):59–67. [PubMed] [Google Scholar]
- 3.Gulati S, Maheshwari A. Atypical manifestations of dengue. Trop Med Int Health. 2007;12(9):1087–95. doi: 10.1111/j.1365-3156.2007.01891.x. [DOI] [PubMed] [Google Scholar]
- 4.Carod-Artal FJ, Wichmann O, Farrar J, Gascón J. Neurological complications of dengue virus infection. Lancet Neurol. 2013;12(9):906–19. doi: 10.1016/S1474-4422(13)70150-9. [DOI] [PubMed] [Google Scholar]
- 5.Weeratunga PN, Caldera HP, Gooneratne IK, et al. Spontaneously resolving cerebellar syndrome as a sequelae of dengue viral infection: A case series from Sri Lanka. Pract Neurol. 2014;14(3):176–78. doi: 10.1136/practneurol-2013-000571. [DOI] [PubMed] [Google Scholar]
- 6.Withana M, Rodrigo C, Chang T, et al. Dengue fever presenting with acute cerebellitis: A case report. BMC Res Notes. 2014;7:125. doi: 10.1186/1756-0500-7-125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sawaishi Y, Takada G. Acute cerebellitis. Cerebellum. 2002;1:223–28. doi: 10.1080/14734220260418457. [DOI] [PubMed] [Google Scholar]


