Abstract
Patient: Female, 53
Final Diagnosis: Thyroid lipomatosis
Symptoms: Dysphasia
Medication: —
Clinical Procedure: Total thyroidectomy
Specialty: Otolaryngology
Objective:
Rare disease
Background:
Diffuse lipomatosis of the thyroid gland is a particularly rare histopathological condition characterized by diffuse fatty infiltration within the thyroid stroma.
Case Report:
We report a case of a 53-year-old woman who presented with a 2-year history of massive neck goiter and mild dysphagia. A computed tomography (CT) scan revealed heterogeneous enhancing of an enlarged thyroid gland with left lobe cranial extension and compression of the pharynx, and caudal bilateral retrosternal growth. The patient underwent total thyroidectomy and histopathological examination revealed mature fatty tissue diffusely distributed throughout the thyroid gland. Excision of the gland was somewhat challenging due to the very thin thyroid capsule and recurrent protrusion of fat from the capsule.
Conclusions:
Diffuse thyroid lipomatosis is an extremely rare histopathological condition characterized by diffuse fatty infiltration in thyroid stroma. Despite its rarity, it should be considered in the differential diagnoses of a patient presenting with a goiter.
MeSH Keywords: Goiter, Lipomatosis, Thyroid Diseases
Background
Thyroid lipomatosis is defined as a progressive enlargement of the thyroid gland caused by diffuse, mature stromal adipose cell infiltration intermixed with follicles with lack of encapsulation [1]. Unlike adenolipoma of the thyroid, diffuse infiltration of mature adipose tissue in thyroid gland is a rare entity. Our literature search, limited to publications in English, revealed less than 25 cases of diffuse thyrolipomatosis. The most recent study reported the concurrence of an encapsulated lipoma of the thymus and diffuse lipomatosis of the thyroid in a 19-year-old man [2]. Despite their different locations, both lesions showed histological similarities, suggesting a common etiology. Previously reported cases showed that thyrolipomatosis affected patients with a wide range of ages but were mostly middle-aged patients with no sex predominance. Most patients presented with progressive enlargement of a soft or nodular goiter with or without pressure symptoms. Thyroid function was normal in most cases; however, a few cases were reported to have hyper- or hypothyroidism [2–7].
The aim of our report is to describe a case of thyrolipomatosis, its presentation, and management. Additionally, the pathophysiology and histopathological characteristics that differentiate thyroid lipomatosis from other fat-containing thyroid lesions are discussed.
Case Report
A 53-year-old female patient was referred to the Otolaryngology Head and Neck Surgery clinic due to the presence of a painless, diffusely enlarged lower-neck mass. The mass was slowly growing for the past 2 years. The patient also complained of mild dysphagia but no associated hoarseness or shortness of breath were noted. The patient had a 10-year history of chronic renal failure secondary to long-standing type 2 diabetes mellitus. She had no known thyroid disease and claimed to be a non-smoker. There was no family history of similar complaints. On physical exam, the patient was calm with no notable tremor, sweating, or exophthalmos. She had a diffusely enlarged, soft lower-neck mass extending bilaterally up to the angle of the mandible with a large, slightly tender thyroid noticed on palpation.
Flexible laryngoscopy showed significant lateral pharyngeal bulging that hindered laryngeal assessment. The presumptive diagnosis at the time was non-toxic diffuse multinodular goiter.
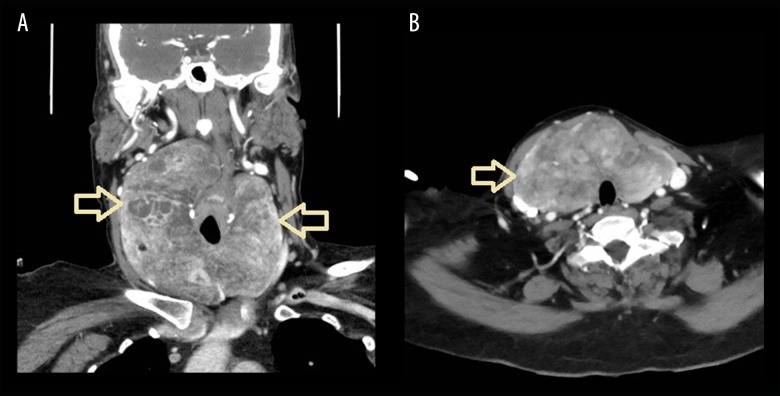
Thyroid function test (TFT) was within normal limits, and serum thyroperoxidase antibody and anti-thyroglobulin antibodies were undetectable. Fine-needle aspiration was performed. No malignant cells were seen. Contrast-enhanced computed tomography scanning was performed and showed a heterogeneous, enhancing, large thyroid gland with left-lobe cranial extension and compression of the pharynx, and caudal bilateral retrosternal growth (Figure 1A). The trachea was slightly deviated to the right side. No cervical lymphadenopathy was detected (Figure 1B).
Figure 1.
(A) A coronal CT with contrast showing heterogeneous enhanced thyroid with cystic changes and a heterogeneous enhanced thyroid mass lesion. The thyroid gland extends up to the pharynx and down to the sternum (arrows). (B) An axial CT with contrast showing heterogeneous thyroid with a heterogeneous enhanced mass lesion. The thyroid extends up and posteriorly reaching the right pyriform fossa, exerting compression on the oropharynx and extending down the retrosternal (arrow). The tracheal air column in the neck is patent and displaced to the left side.
Total thyroidectomy was performed via a horizontal lower-neck incision. Intraoperatively, the thyroid capsule was noted to be extremely thin with very soft gland texture. The dissection of lipomatous glands was challenging given their thin capsule and very soft content. The thyroid capsule was accidentally breeched in several locations, with fatty-gelatinous material protruding from the gland.
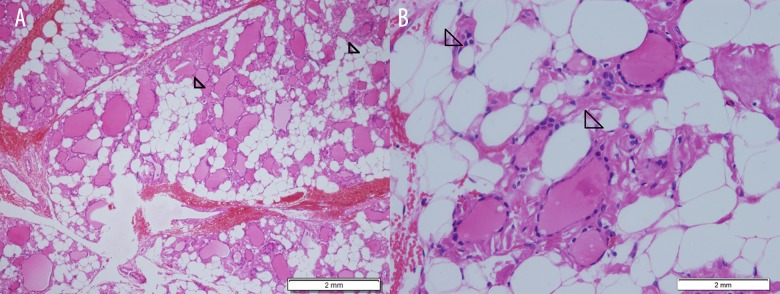
Upon resection, the whole gland was found to be replaced by soft, yellow, homogenous spaces. The specimen weighed 415 grams and the left lobe, right lobe, and isthmus measured 11×7×3.5 cm, 5×2.5×2 cm, and 2.5×2×1.5 cm, respectively. Pathology findings of multiple sections from both lobes and isthmus revealed extensive infiltration by mature adipose tissue. Microscopic examination showed fat cells admixed with bland follicular cells (Figure 2A, 2B) No chronic inflammation was encountered apart from focal aggregations of lymphocytes. No evidence of malignancy was detected. The final histopathological diagnosis was diffuse lipomatosis of the thyroid gland.
Figure 2.
(A) Microscopic examination at low magnification showing admixture of adipocytes (arrows) with follicular thyroid cells (hematoxylin and eosin stain). (B) Microscopic examination at higher magnification of adipocytes (arrows).
Discussion
Thyrolipomatosis is a rare and benign condition of the thyroid gland resulting from diffuse stromal infiltration by mature adipose tissue [5]. Dhayagude first observed the entity in 1942 [3]. In 2016, Bell and colleagues reported a case of thyroid lipomatosis and reviewed the cases of 20 previously reported patients [4]. Since then, 4 additional cases were reported in the literature [2,5–7].
The differential diagnosis of fat in the thyroid gland falls into 2 groups: benign entities (e.g., thyrolipoma [also known as adenolipoma], heterotopic nests of adipocytes, amyloid goiter, lipid-rich thyroid follicular adenoma, parathyroid lipoma, and lipomatosis) and malignant neoplasms (e.g., liposarcoma) [1,4,5,8]. Thyrolipoma is a well-circumscribed and encapsulated nodule composed of a proliferation of thyroid follicles admixed with mature adipose tissue [9]. Heterotopic nests of fat cells in the thyroid gland are fat cells that are located in the subcapsular areas and scattered among the follicles [10]. Thyrolipomatosis, in contrast, shows diffuse fatty infiltration throughout the thyroid, with no evidence of encapsulation [11]. Amyloid goiter, which often contains fat cells, is not difficult to distinguish from thyrolipomatosis. The thyroid parenchyma is usually replaced with amyloid and adipose tissue, with the latter filling the spaces between the sites of amyloid deposition [12]. Lipid-rich thyroid follicular adenoma is a variant of follicular adenoma, where follicular cells have a microvesicular cytoplasmic appearance due to intracytoplasmic lipid droplets. These microvesicles may coalesce to form larger vacuoles that result in a large vacuole, imparting a signet ring morphology to the cells [13]. Parathyroid lipoma should also be considered in the differential diagnosis of thyrolipoma, especially in patients with extrathyroidal nodules and positive parathyroid scans [11]. In such cases, a stromal component of lobulated adult adipose tissue, with trabecular and follicular formations of uniform parathyroid chief cells, is seen by microscopic examination [14]. Liposarcoma of the thyroid is a rare type of malignancy that is classified according to its histopathological criteria into well-differentiated, myxoid, round cell, pleomorphic, and dedifferentiated types. At presentation, the majority of liposarcomas are found to be extended beyond the capsule [15].
Adipose tissue is commonly seen in salivary glands, parathyroid glands, thymus, pancreas, and breast tissues. However, aside from the presence of a few pericapsular and perivascular adipocytes, adipose tissue in the thyroid gland is rare [6]. The exact mechanism by which adipose tissue is deposited within the thyroid parenchyma remains unknown. There are several theories attempting to explain the pathophysiology of thyroid lipomatosis. Trites et al. reported a case of a syndrome of thyrolipoma, thymolipoma, and pharyngeal lipoma. As the thyroid, thymus, and aryepiglottic fold all arise from the primitive foregut, the authors hypothesized that the fat lesions resulted from disturbed differentiation of the primitive foregut early in embryogenesis [16]. Although this theory could explain the presence of adipose tissue in congenital goiters, it does not explain the presence of fat in acquired thyroid lesions. Schroder et al. suggested that adipose tissue may be caused by meta-plasia of stromal fibroblasts due to tissue hypoxia or senile involution [17]. More recently, Lau et al. suggested a possible relationship between diffuse lipomatosis and loss of expression of a protein called succinate dehydrogenase-subunit B in the follicular or adipose cells [15].
Conclusions
Diffuse thyroid lipomatosis is an extremely rare histopathological condition of unknown etiology, characterized by diffuse fatty infiltration in thyroid stroma. Despite its rarity, it should be considered in the differential diagnoses of a patient presenting with a goiter. With more cases reported over time, the criteria for diagnosing thyrolipomatosis may become better understood.
Footnotes
Conflict of interest
None.
References:
- 1.Gupta R, Arora R, Sharma A, Dinda AK. Diffuse lipomatosis of the thyroid gland: A pathologic curiosity. Indian J Pathol Microbiol. 2009;52:215–16. doi: 10.4103/0377-4929.48922. [DOI] [PubMed] [Google Scholar]
- 2.Stanaway A, Lam T. Consecutive cases of thyrolipomatosis and thymolipoma: A case report. ANZ J Surg. 2017 doi: 10.1111/ans.14216. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 3.Dhayagude RG. Massive fatty infiltration in a colloid goiter. Arch Pathol. 1942;33:357–60. [Google Scholar]
- 4.Bell S, Sosa GA, del Valle Jean A, Russo Picasso MF. Thyroid lipomatosis in a 36-year-old patient with rheumatoid arthritis and a kidney transplant. Endocrinol Diabetes Metab Case Rep. 2016;2016:160007. doi: 10.1530/EDM-16-0007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ishida M, Kashu I, Morisaki T, et al. Thyrolipomatosis: A case report with review of the literature. Mol Clin Oncol. 2017;6:893–95. doi: 10.3892/mco.2017.1249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ben Gamra O, Romdhane N, Nefzaoui S, et al. Diffuse lipomatosis of the thyroid gland. Egyptian J Ear Nose Throat Allied Sci. 2016;17:167–69. [Google Scholar]
- 7.Mitra A, Fisher C, Rhys-Evans P, Harmer C. Liposarcoma of the thyroid. Sarcoma. 2004;8:91–96. doi: 10.1080/1357-7140400001517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Choi JW, Kim TH, Roh HG, et al. Radiologic and pathologic findings of a follicular variant of papillary thyroid cancer with extensive stromal fat: A case report. Korean J Radiol. 2015;16:1349–52. doi: 10.3348/kjr.2015.16.6.1349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kitagawa W, Kameyama K, Tamai S, et al. Adenolipoma of the thyroid gland: Report of a case. Surg Today. 2004;34:593–96. doi: 10.1007/s00595-004-2772-y. [DOI] [PubMed] [Google Scholar]
- 10.Soda G, Baiocchini A, Nardoni S, et al. Benign tumors of heterotopic tissue in the thyroid gland: A report of two cases of lipomatous lesions. J Exp Clin Cancer Res. 2000;19:245–48. [PubMed] [Google Scholar]
- 11.Ge Y, Luna MA, Cowan DF, et al. Thyrolipoma and thyrolipomatosis: 5 case reports and historical review of the literature. Ann Diagn Pathol. 2009;13:384–89. doi: 10.1016/j.anndiagpath.2009.08.003. [DOI] [PubMed] [Google Scholar]
- 12.Ozdemir BH, Uyar P, Ozdemir FN. Diagnosing amyloid goitre with thyroid aspiration biopsy. Cytopathology. 2006;17:262–66. doi: 10.1111/j.1365-2303.2006.00399.x. [DOI] [PubMed] [Google Scholar]
- 13.Frennby B, Nyman U, Aspelin P, et al. CT of a parathyroid lipoadenoma: Case report. Acta Radiol. 1993;34:369–71. [PubMed] [Google Scholar]
- 14.Kumar R, Bhargava A, Jaiswa G. A case report on radiologic findings of thyrolipomatosis: A rare fat containing lesion diffusely infiltrating throughout the thyroid gland. J Kathmandu Med Col. 2017;5:71–73. [PubMed] [Google Scholar]
- 15.Lau E, Freitas P, Costa J, et al. Loss of mitochondrial SDHB expression: What is its role in diffuse thyroid lipomatosis? Horm Metab Res. 2015;47:165–67. doi: 10.1055/s-0034-1398559. [DOI] [PubMed] [Google Scholar]
- 16.Trites AE. Thyrolipoma, thymolipoma and pharyngeal lipoma: A syndrome. Can Med Assoc J. 1996;95:1254–59. [PMC free article] [PubMed] [Google Scholar]
- 17.Schröder S, Böcker W. Lipomatous lesions of the thyroid gland: A review. Appl Pathol. 1985;3:140–49. [PubMed] [Google Scholar]