Abstract
Background
Treatment for hoarding disorder is typically performed by mental health professionals, potentially limiting access to care in underserved areas.
Aims
We aimed to conduct a non-inferiority trial of group peer-facilitated therapy (G-PFT) and group psychologist-led cognitive–behavioural therapy (G-CBT).
Method
We randomised 323 adults with hording disorder 15 weeks of G-PFT or 16 weeks of G-CBT and assessed at baseline, post-treatment and longitudinally (≥3 months post-treatment: mean 14.4 months, range 3–25). Predictors of treatment response were examined.
Results
G-PFT (effect size 1.20) was as effective as G-CBT (effect size 1.21; between-group difference 1.82 points, t = −1.71, d.f. = 245, P = 0.04). More homework completion and ongoing help from family and friends resulted in lower severity scores at longitudinal follow-up (t = 2.79, d.f. = 175, P = 0.006; t = 2.89, d.f. = 175, P = 0.004).
Conclusions
Peer-led groups were as effective as psychologist-led groups, providing a novel treatment avenue for individuals without access to mental health professionals.
Declaration of interest
C.A.M. has received grant funding from the National Institutes of Health (NIH) and travel reimbursement and speakers’ honoraria from the Tourette Association of America (TAA), as well as honoraria and travel reimbursement from the NIH for serving as an NIH Study Section reviewer. K.D. receives research support from the NIH and honoraria and travel reimbursement from the NIH for serving as an NIH Study Section reviewer. R.S.M. receives research support from the National Institute of Mental Health, National Institute of Aging, the Hillblom Foundation, Janssen Pharmaceuticals (research grant) and the Alzheimer's Association. R.S.M. has also received travel support from the National Institute of Mental Health for Workshop participation. J.Y.T. receives research support from the NIH, Patient-Centered Outcomes Research Institute and the California Tobacco Related Research Program, and honoraria and travel reimbursement from the NIH for serving as an NIH Study Section reviewer. All other authors report no conflicts of interest.
Keywords: Hoarding disorder, community treatment, peer treatment, cognitive–behavioural therapy, treatment outcomes, randomised clinical trial
Hoarding disorder is a highly debilitating psychiatric illness that poses a profound public health burden.1,2 Up to 25% of deaths by house fire are attributable to hoarding,3 and hoarding-related clutter in homes increases fall risk, health code violations and difficulty with self-care, especially among older adults, who are disproportionately affected.2,4–7 Over 50% of individuals with hoarding disorder have co-occurring depression or a chronic anxiety disorder.8 Executive dysfunction, particularly impairments in visual categorisation, learning and memory, is a prominent feature of hoarding disorder and may also affect functioning (summarised in Mackin et al9).
Treatment for hoarding disorder
Effective treatment options for hoarding disorder are limited. Although there is a role for pharmacological treatment,10 the current standard of care based on the published evidence is cognitive–behavioural therapy (CBT), which varies in implementation (e.g. number of sessions, individual versus group, inclusion of home visits) and is dependent on access to trained mental health providers.11,12 Currently published studies are small (range 6–58 participants), and suggest that with CBT, hoarding symptoms improve by 20–30% on average (range 12–37%) (see Mathews et al13 and Tolin et al11). A recent meta-analysis indicates that individual and group CBT are similarly effective;11 however, by definition, group CBT allows for the treatment of more individuals within a given timeframe, making it the preferable choice when access to treatment providers is limited.
Because clinician-delivered CBT tailored for hoarding disorder is not widely available,14 additional treatment options are needed, and factors such as lack of recognition of hoarding disorder as a medical (psychiatric) condition, poor insight into illness, stigma and shame may make community-based approaches an inviting alternative.15 Of the few previously studied alternatives, group peer-facilitated therapy (G-PFT) with a CBT-based workbook appears to be the most effective, with improvement rates similar to group psychiatrist-led CBT (G-CBT) (summarised in Mathews et al13). However, to date, no prospective, randomised clinical trials directly comparing G-PFT with G-CBT have been published.
Predictors of treatment response
In addition, studies examining predictors of treatment response have been limited to a few demographic and clinical variables (e.g. gender, less severe pre-treatment hoarding severity, co-occurring anxiety or depressive symptoms and in one study, treatment adherence).11,13,16 None of the variables examined in previous studies were consistently found to predict treatment outcome. Given its chronic nature and high degree of functional impairment,2 there continues to be a pressing need to identify predictors of treatment response for hoarding disorder. Such predictors might include, in addition to demographic factors, clinical variables such as neurocognitive function and psychiatric status, and treatment-related factors such as treatment adherence.
This study was a randomised, controlled non-inferiority trial aimed at formally evaluating the effectiveness of G-CBT and G-PFT and identifying predictors of treatment response. We hypothesised that G-CBT and G-PFT would be similarly effective and that both would lead to clinically meaningful improvement, as well as that individual characteristics (e.g. age, psychiatric symptoms and pre-treatment cognitive function including visual learning, memory and sustained attention) and treatment adherence would be associated with treatment response.9
Method
Study procedures
The study took place at the University of California, San Francisco and the Mental Health Association of San Francisco. It was approved by the University of California, San Francisco Institutional Review Board (#13-12100), and was prospectively registered at Clinicaltrials.gov (trial registration identifier: NCT02040805). Study procedures, which were designed to maximise generalisability and to be implemented by community agencies and individuals in a real-world setting, are described below and in the Supplementary Methods, available at https://doi.org/10.1192/bjo.2018.30. Further details about the academic/community collaborative partnership and study design have previously been published.17
Recruitment and screening
Participants were recruited through advertisements, mental health clinics and senior centres throughout the San Francisco Bay Area, and through outreach by the Mental Health Association of San Francisco. Potential participants gave verbal consent and were screened for hoarding symptoms via telephone and online self-report questionnaires. To increase specificity of these measures in identifying hoarding disorder, two or more of the following were required for inclusion: Saving Inventory, Revised (SI-R) score of ≥42,18 University of California, Los Angeles Hoarding Symptom Scale (UHSS) score of ≥2019 and Clutter Image Rating Scale score of ≥12.20 Those who met screening criteria subsequently provided written informed consent for all ensuing study procedures. All pre-treatment assessments were completed before randomisation. Eligible participants were stratified by gender and randomised by computer in a 1:1 ratio in blocks of five, to either G-CBT or G-PFT, by a member of the research team who was blind to clinical status.17
Clinical interviews were completed at baseline only, and neuropsychological assessments and self-report questionnaires (Supplementary Methods and Supplementary Table 1) were completed pre- and post-treatment.17 Group facilitators were blinded to the neurocognitive and psychiatric status of participants, other than the required diagnosis of hoarding disorder.
Participants were financially compensated for completing the assessments, although they were not compensated for participating in the treatment groups. As a post hoc follow-up, symptom severity and functional assessment were also re-assessed in randomised individuals who agreed to re-contact at least 3 months (range 3–25 months) after the end of their assigned treatment groups (longitudinal assessment) (Supplementary Methods).
Inclusion/exclusion criteria
To maximise generalisability, inclusion criteria were deliberately broad. Individuals were eligible for participation if they met the screening criteria listed above and DSM-5 criteria for hoarding disorder,1 assessed with the Structured Interview for Hoarding Disorder.21 Participants were excluded if they had known intellectual disability, moderate to severe dementia (scores of ≤17 on the Montreal Cognitive Assessment22), were unable to actively participate in treatment (e.g. because of acute medical conditions, high suicide risk or actively disruptive psychotic or behavioural symptoms) or had received individual or group CBT or peer-facilitated therapy for hoarding in the previous year. Concurrent participation in other forms of treatment (e.g. medication management, Clutterers' Anonymous, psychotherapy for non-hoarding symptoms) was allowed and was tracked during the course of treatment. Participants were not excluded based on co-occurring psychiatric illness, active substance use, psychosis or suicidal ideation (unless, as noted, they were actively disruptive or deemed to be at high risk of suicide).
Interventions
The interventions were based on published manualised treatments for hoarding disorder23–26 and modified for this study based on input from our community partners (Supplementary Methods and Uhm et al17). Groups were composed of 8–12 participants. G-CBT groups met weekly for 16 sessions over 20 weeks and were led by postdoctoral-level psychologists. Two 30-minute home visits were conducted in the G-CBT group, one after week 3 and the other after week 15. G-CBT participants were assigned (but not required to accept) clutter buddies (individuals who were available to provide encouragement and maintain accountability for treatment adherence) from within the group. G-PFT groups met weekly for 15 sessions over 20 weeks and were led by trained peer facilitators who had lived experience of hoarding. G-PFT participants did not receive home visits and were encouraged to identify (but were not assigned) clutter buddies. Peer facilitators checked in with each group member by telephone between each session.
Assessments
The primary outcome was hoarding symptom severity, assessed by the SI-R,18 with hoarding-related functional impairment as a secondary outcome, assessed by the Activities of Daily Living Scale in Hoarding Disorder (ADL-H).27 Hoarding-related beliefs were assessed by the Saving Cognition Inventory.28 Symptoms of depression, anxiety and attention-deficit hyperactivity disorder were assessed by the Beck Depression Inventory, Second Edition,29 the Beck Anxiety Inventory30 and the Swanson, Nolan, and Pelham Rating Scale,31 respectively.
Neurocognition was assessed by standard neuropsychological measures, which are detailed in the Supplementary Methods. Neurocognitive domains of particular interest included sustained visual attention (Conners’ Continuous Performance Test II32), visual memory and learning (Brief Visuospatial Memory Test, Revised)33) and visual spatial processing and problem solving (Block Design subtest of the Wechsler Adult Intelligence Scale34). For all measures, scaled scores were used in the analyses.
Treatment-related measures
Beliefs about treatment and treatment preferences were assessed with questions developed for this study (Supplementary Fig. 1). Homework completion was assessed weekly and a group evaluation (Supplementary Figs 2 and 3) was completed bi-weekly throughout treatment. Continuing support after the end of treatment was assessed at the longitudinal evaluation (Supplementary Fig. 4).
Analyses
All analyses were conducted with SAS software version 9.4. Standard methods were used to summarise and describe the collected data, including the number who met the criteria for clinically significant change (SI-R change ≥14 points)35,36 and functional remission (SI-R reduction ≥14 points and post-test SI-R of <42).36,37 All participants who provided baseline data, whether or not they completed the treatment, were eligible for inclusion, although only participants with complete outcome data for any given measure were included in the analyses for that measure.
Treatment drop-outs were defined as individuals who completed fewer than 60% of the sessions. To test for evidence of effects of non-completion, we re-estimated and tested our models of non-inferiority and predictors of treatment response, using only participants who completed treatment (completers-only analysis). In a similar way, sensitivity analyses were conducted to examine the effects of including/excluding participants who dropped out of treatment before the third session and later re-joined a group (n = 12). Post-treatment assessments were obtained, when possible, on all participants, and particularly for individuals who attended at least one group.
A one-tailed t-test for non-inferiority comparing the mean post-treatment SI-R scores between G-PFT and G-CBT groups, with a margin of equivalence of 5 points, was used. This margin represents half of the minimal change score that was determined to represent noticeable and meaningful improvement from a patient and healthcare provider's perspective (SI-R change ≥10 points or 15% improvement from a mean SI-R baseline of 65) (R. Frost, personal communication, 2013, and based on our prior work).13 The margin was set at 2.5 for the ADL-H, using a similar approach (e.g. 15% improvement from baseline total score divided by two). Effect sizes for the SI-R and ADL-H were computed as mean change divided by the s.d. of the change. The change in SI-R and ADL-H scores by treatment group over time (pre-treatment, post-treatment and longitudinal) was examined by linear mixed models. Testing for individual characteristics that were associated with treatment response was conducted by regression models of change in SI-R scores, incorporating each individual measure (e.g. insurance status, socioeconomic, demographic, clinical and neuropsychological factors) as a covariate. Variables that were associated with SI-R change at P ≤ 0.15 were carried forward into multivariable models.
Results
Pre-treatment characteristics
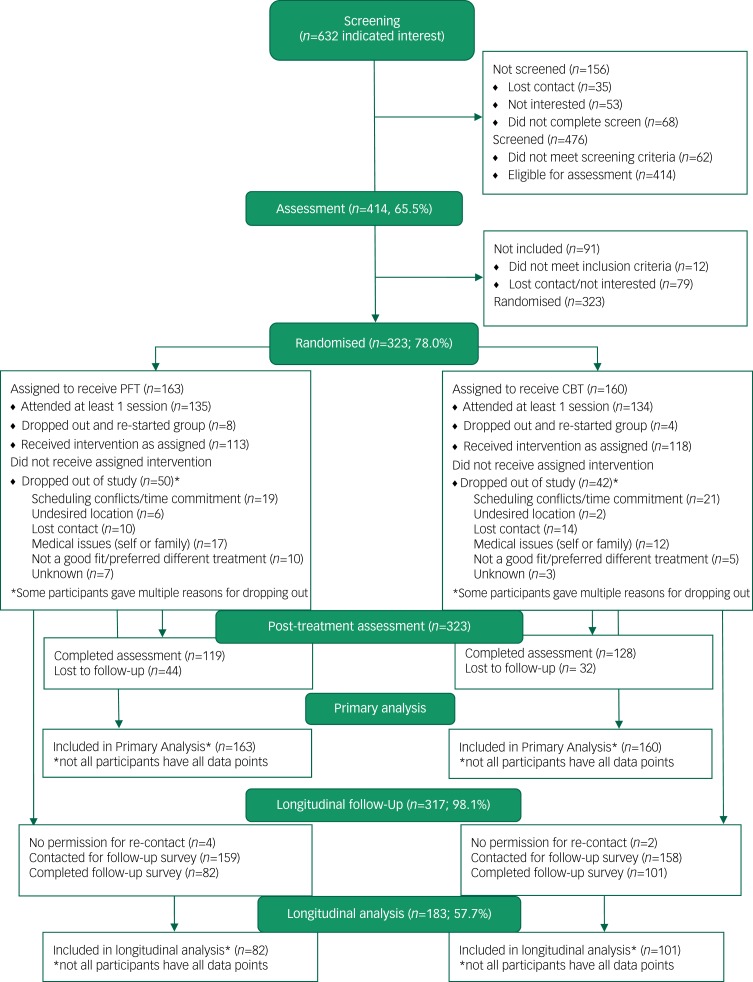
Recruitment occurred from April 2014 to January 2016. A total of 632 individuals expressed interest in the study; 414 were clinically assessed and 323 were randomised into G-CBT or G-PFT (Fig. 1). Only 13% of screened individuals and 3% of those clinically assessed were excluded; the remainder declined to participate or were lost to follow-up. Individuals who were screened but not randomised (n = 149) had lower mean hoarding severity scores, poorer insight and were more likely to be male than those who were randomised to treatment (Supplementary Table 2).
Fig. 1.
Study flow diagram. CBT, cognitive–behavioural therapy; PFT, peer-facilitated therapy.
There were no significant differences in baseline characteristics between participants randomised to G-CBT or G-PFT (Table 1). The majority of the sample were female (74.5%), with mean age of 59 years (range 18–89). The ethnic-racial composition was diverse, comprising 59.5% White, 11.3% Asian, 7.6% Black, 1.2% Native American, Native Hawaiian or Pacific Islander and 20.4% multi-racial or other. Further, 9.3% participants reported as Hispanic.
Table 1.
Baseline characteristics for G-CBT and G-PFT groups
| G-CBT (N = 160) | G-PFT (N = 163) | χ2 or t statistic | P-value | ||
|---|---|---|---|---|---|
| Demographic characteristics | |||||
| Male,a n (%) | 43 (26.9) | 39 (24.1) | 0.33 | 0.56 | |
| Age, years, mean (s.d.) | 59.0 (10.9) | 58.9 (10.6) | −0.13 | 0.90 | |
| Race, n (%) | White | 89 (57.1) | 101 (64.3) | 0.06 | 0.11 |
| Asian | 16 (10.3) | 17 (10.8) | |||
| Black | 17 (10.9) | 6 (3.8) | |||
| Multi-racial/other | 34 (21.8) | 33 (21.0) | |||
| Hispanic/Latino, n (%) | 14 (9.3) | 13 (8.5) | 0.07 | 0.80 | |
| LGBT, n (%) | 22 (15.8) | 22 (16.3) | 0.01 | 0.92 | |
| Marital status, n (%) | Married | 40 (26.5) | 37 (24.2) | 1.74 | 0.42 |
| Divorced/widowed/separated | 55 (36.4) | 48 (31.4) | |||
| Never married/roommate | 56 (37.1) | 68 (44.4) | |||
| Number of people in household (adults and children), mean (s.d.) | 1.13 (0.74) | 0.94 (0.89) | 1.21 | 0.23 | |
| Children (yes/no), n (%) | 88 (56.4) | 97 (61.0) | 0.69 | 0.41 | |
| Employment status, n (%) | Employed (full or part time) | 54 (34.4) | 29 (25.0) | 3.41 | 0.33 |
| Unemployed/disabled | 55 (35.0) | 65 (41.7) | |||
| Retired | 37 (23.6) | 40 (25.6) | |||
| Other | 11 (7.0) | 12 (7.7) | |||
| Insurance status (insured versus underinsured or not insured), n (%) | 150 (95.5) | 144 (90.0) | 3.62 | 0.06 | |
| Education, mean (s.d.) | 15.3 (2.2) | 15.3 (2.4) | 0.01 | 0.90 | |
| Clinical characteristics | |||||
| Pre-treatment UHSS score, mean (s.d.) | 28.5 (5.5) | 29.8 (5.5) | 2.13 | 0.04 | |
| Pre-treatment SI-R score, mean (s.d.) | 64.5 (11.7) | 66.4 (11.6) | 1.53 | 0.13 | |
| Pre-treatment ADL-H score, mean (s.d.) | 29.9 (9.5) | 32.0 (11.2) | 1.85 | 0.07 | |
| Pre-treatment CI-R score, mean (s.d.) | 13.0 (4.8) | 14.0 (5.1) | 1.62 | 0.10 | |
| Pre-treatment SCI score, mean (s.d.) | 97.8 (29.7) | 100.2 (29.1) | 0.72 | 0.47 | |
| Pre-treatment MoCA score,b mean (s.d.) | 26.3 (2.9) | 26.2 (2.6) | −0.06 | 0.95 | |
| Pre-treatment NART, mean (s.d.) | 115.6 (6.9) | 116.0 (6.1) | 0.59 | 0.55 | |
| Pre-treatment BAI score, mean (s.d.) | 17.6 (12.5) | 18.6 (12.2) | 0.67 | 0.50 | |
| Pre-treatment BDI score, mean (s.d.) | 20.1 (12.2) | 19.4 (13.1) | −0.43 | 0.66 | |
| SNAP-IV total score, mean (s.d.) | 38.1 (15.0) | 36.1 (13.5) | 1.28 | 0.20 | |
| Excessive acquisition (yes/no), n (%) | 98 (64.5) | 87 (60.8) | 0.41 | 0.52 | |
| Poor insight, n (%) | 18 (11.3) | 21 (12.9) | 0.21 | 0.65 | |
| Age at symptom onset <18 v. ≥18 years, n (%) | 69 (45.1) | 69 (43.7) | 0.11 | 0.91 | |
| Any current or lifetime psychiatric diagnosis (not including hoarding disorder), n (%) | 96 (61.9) | 91 (59.5) | 0.13 | 0.72 | |
| Mean number of psychiatric diagnoses, mean (s.d.) | 0.12 (0.14) | 0.10 (0.12) | 1.29 | 0.20 | |
| Taking psychiatric medications, n (%) | 66 (41.8) | 76 (47.5) | 1.05 | 0.30 | |
| Moderate or high suicide risk, n (%) | 19 (12.1) | 13 (8.4) | 2.95 | 0.23 | |
ADL-H, Activities of Daily Living Scale in Hoarding Disorder; BAI, Beck Anxiety Inventory; BDI, Beck Depression Inventory; CI-R, Clutter Image Rating Scale; G-CBT, group psychiatrist-led cognitive–behavioural therapy; G-PFT, group peer-facilitated therapy; LGBT, lesbian, gay, bisexual and transgender community; MoCA, Montreal Cognitive Assessment; NART, National Adult Reading Test Full Scale IQ; SCI, Saving Cognition Inventory; SI-R, Saving Inventory, Revised; SNAP-IV, Swanson, Nolan and Pelham attention-deficit hyperactivity disorder Rating Scale; UHSS, University of California, Los Angeles Hoarding Severity Scale.
a. One participant in each group reported their gender as other.
b. MoCA data available for 60 participants in the G-CBT group and 80 participants in the G-PFT group.
Participants had moderately severe hoarding, depression and anxiety symptoms at baseline (Table 1). More than half had a current or lifetime history of an additional psychiatric disorder, most commonly major depressive disorder (44.8%) and anxiety disorders (30.5%). Approximately 10% had a moderate to high suicide risk. Most (72%) expressed no strong preference for either treatment. Only one of the ten participants who preferred G-PFT was randomised to G-CBT, whereas 36 out of 77 participants who preferred G-CBT were randomised to G-PFT (χ2 = 6.72, d.f. = 2, P = 0.04).
Participation in treatment
Of the 323 individuals randomised to treatment, 269 (83%) attended at least one session and 231 (71.5%) completed treatment. There were no significant differences in drop-out rates between G-CBT and G-PFT groups (Fig. 1). Session attendance (per cent of total groups attended) was higher in the G-CBT group (73.3%) than G-PFT group (57.7%) (t = −4.09, d.f. = 245, P < 0.0001), whereas homework completion was similar between groups (54.3% of G-CBT participants and 48.9% of G-PFT participants, t = −1.50, d.f. = 245, P = 0.13). A total of 69% of G-CBT participants and 37% of G-PFT participants had a clutter buddy (χ2 = 33.11, d.f. = 1, P < 0.0001). Most participants with a clutter buddy (82.5% of G-CBT participants and 83.8% of G-PFT participants) found them to be helpful (χ2 = 0.03, d.f. = 1, P = 0.86).
Treatment outcomes
Hoarding severity
Post-treatment data were available for 247 individuals (231 treatment-completers; 16 non-completers). G-CBT participants had a 27.7% reduction in SI-R scores (mean post-treatment score 45.9, s.d. = 15.0), whereas G-PFT participants had a 25.6% reduction in SI-R scores (mean post-treatment score 47.8, s.d. = 14.6) (Table 2). The test of non-inferiority indicated that the null hypothesis (i.e. that G-PFT outcomes would be statistically worse than G-CBT outcomes) was rejected (between-group difference 1.82 points, one-sided 95% CI 4.89, t = −1.71, d.f. = 245, P = 0.04), indicating that G-PFT was as effective as G-CBT. A total of 37% of G-CBT and 36% of G-PFT participants had post-treatment SI-R scores of <42, and 55% of G-CBT and 57% of G-PFT participants had ≥14-point reduction in SI-R scores pre- to post-treatment. There was no significant difference in the number of participants who achieved remission (32.8% of G-CBT participants and 29.4% of G-PFT participants, χ2 = 0.33, d.f. = 1, P = 0.56). There were no differences when treatment-completers only were analysed (data not shown).
Table 2.
Pre-treatment, post-treatment and longitudinal scores for G-CBT and G-PFT groups
| Measure | G-CBT group | G-PFT group | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean pre-treatment total score (s.d.) N = 160 | Mean post-treatment total score (s.d.) N = 128 | Pre- to post-treatment change t-statistic, P-value | Mean longitudinal follow-up total score (s.d.) N = 101 | Post-treatment to longitudinal change t-statistic, P-value | Mean pre-treatment total score (s.d.) N = 163 | Mean post-treatment total score (s.d.) N = 119 | Pre- to post-treatment change t-statistic, P-value | Mean longitudinal follow-up total score (s.d.) N = 82 | Post-treatment to longitudinal change t-statistic, P-value | |
| SI-R | 64.5 (11.7) | 45.9 (15.0) | 13.67, P < 0.0001 | 48.2 (14.9) | −1.84, P = 0.07 | 66.4 (11.6) | 47.8 (14.2) | 13.14, P < 0.0001 | 47.9 (13.9) | 1.79, P = 0.08 |
| SI-R (completers only) | 64.3 (12.0) | 45.1 (14.4) | 13.42, P < 0.0001 | 47.8 (15.1) | −1.92, P = 0.06 | 65.6 (11.3) | 47.2 (14.2) | 12.60, P < 0.0001 | 46.6 (14.2) | 2.19, P = 0.03 |
| ADL-H | 29.9 (9.5) | 25.5 (10.1) | 5.80, P < 0.0001 | 27.6 (11.6) | −2.23, P = 0.03 | 32.0 (11.2) | 26.1 (8.7) | 6.55, P < 0.0001 | 27.8 (9.7) | −1.51, P = 0.14 |
| CI-R | 13.0 (4.8) | 9.8 (4.4) | 8.64, P < 0.0001 | N/A | 14.0 (5.1) | 10.5 (4.9) | 7.52, P < 0.0001 | N/A | ||
| SCI | 97.8 (29.7) | 81.1 (30.1) | 5.72, P < 0.0001 | 100.2 (29.1) | 79.6 (27.8) | 8.53, P < 0.0001 | ||||
| BDI | 20.1 (12.2) | 17.3 (14.5) | 2.92, P = 0.004 | 19.4 (13.1) | 20.0 (22.1) | −0.79, P = 0.43 | ||||
| BAI | 17.6 (12.5) | 16.1 (12.8) | 0.89, P = 0.38 | 18.6 (12.2) | 17.0 (20.1) | 0.28, P = 0.78 | ||||
All numbers are for all participants who were randomised to treatment with one exception: the SI-R results are reported both for all participants and for those who completed treatment. Treatment-completers N = 118 for the G-CBT group and N = 113 for the G-PFT group.
ADL-H, Activities of Daily Living Scale in Hoarding Disorder; BAI, Beck Anxiety Inventory; BDI, Beck Depression Inventory; CI-R, Clutter Image Rating Scale; G-CBT, group psychiatrist-led cognitive–behavioural therapy; G-PFT, group peer-facilitated therapy; N/A, not available; SCI, Saving Cognition Inventory; SI-R, Saving Inventory, Revised.
Functional impairment
The G-CBT group had a 10.5% reduction in ADL-H scores pre- to post-treatment (mean post-treatment score 25.5, s.d. = 10.1), whereas the G-PFT group had a 12.4% reduction in ADL-H scores (mean post-treatment score 26.1, s.d. = 8.7) (Table 2). The test of non-inferiority was significant (between-group difference 1.82 points, one-sided 95% CI 2.67, t = −1.52, d.f. = 245, P = 0.05), again indicating equivalence between the groups.
Predictors of treatment response
Predictors of treatment response were examined at post-treatment only; the longitudinal assessment was not included in this analysis. Variables that were associated with change in either SI-R or ADL-H scores at a P-value of ≤0.15 were included in multivariable models (Supplementary Tables 3 and 4). For highly correlated variables, only the most strongly associated in the univariate analyses were included. In the univariable models, more severe pre-treatment severity and hoarding-related thoughts and beliefs were associated with treatment improvement and more severe anxiety and/or depression were associated with less improvement in both groups (Supplementary Tables 3 and 4). Higher rates of homework completion were associated with improvement for both treatment groups; higher group attendance and finding a clutter buddy helpful were associated with treatment improvement for G-PFT but not G-CBT participants.
The multivariable models for SI-R change included pre-treatment hoarding (assessed with UHSS total score rather than SI-R total score, to avoid circularity), depressive, anxiety and attention-deficit hyperactivity disorder symptoms, hoarding cognitions, mean number of psychiatric diagnoses, homework adherence, group attendance, finding a clutter buddy helpful and treatment preference. The multivariable models for both G-CBT and G-PFT groups accounted for only a small amount of the total variance (adjusted R2 = 0.08, f(9,115) = 2.17, P = 0.03 for the G-CBT group; adjusted R2 = 0.05, f(9,103) = 1.59, P = 0.13 for the G-PFT group). For both conditions, pre-treatment UHSS score was the only independent predictor of treatment outcome (β = 0.73, s.e. = 0.29, t = 2.56, d.f. = 1, P = 0.01 for the G-CBT group; β = 0.65, s.e. = 0.29, t = 2.26, d.f. = 1, P = 0.03 for the G-PFT group); higher pre-treatment severity was associated with greater improvement. For the G-PFT but not for the G-CBT group, lower pre-treatment depressive symptoms (β = −0.28, s.e. = 0.15, t = −1.89, d.f. = 1, P = 0.06) indicated a trend for association with improvement. These results did not change when the analyses were repeated in treatment-completers only (data not shown).
Continuing treatment and maintenance of treatment gains
We obtained longitudinal follow-up data ≥3 months post-treatment on 183 of the 323 randomised participants (101 in the G-CBT group and 82 in the G-PFT group). The average time to follow-up was 14.4 months (s.d. = 6.5, range 3–25). Most participants (64%) were re-contacted >1 year after completing treatment. Participants who provided longitudinal data were more likely to be women (χ2 = 9.3, d.f. = 1, P = 0.002), White (χ2 = 11.8, d.f. = 1, P = 0.001) and have higher education levels (t = −3.6, d.f. = 182, P = 0.0004) than those who did not. There were no significant differences in pre- or post-treatment SI-R scores between those who provided longitudinal data and those who did not. There were no differences in time to follow-up between groups (G-CBT group: 13.9 months, s.d. = 7.2; G-PFT group: 13.2 months, s.d. = 6.9; t = −0.68, d.f. = 182, P = 0.50).
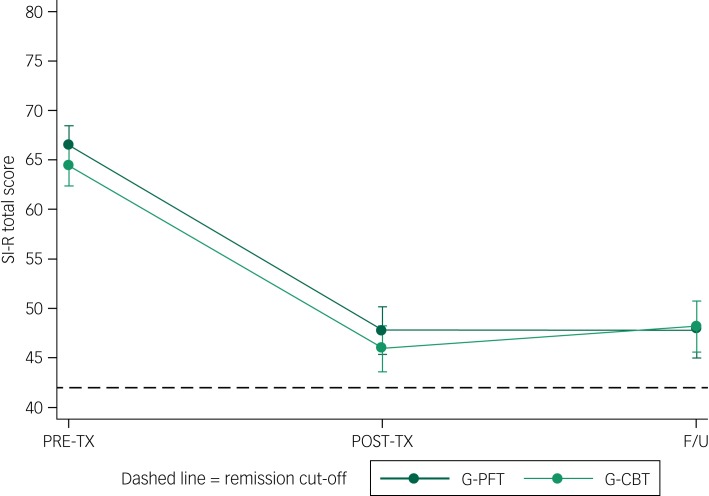
The linear mixed models analysis incorporating treatment group (G-CBT and G-PFT) and time (pre-treatment, post-treatment and longitudinal) was significant for both SI-R (likelihood ratio χ2 = 115.5, d.f. = 1, P < 0.0001) and ADL-H (LR χ2 = 162.1, d.f. = 1, P < 0.0001). For both outcomes, only time significantly contributed to the model (SI-R: f = 250.5, d.f. = 2, P < 0.0001; ADL-H: f = 34.3, d.f. = 2, P < 0.0001); there were no significant differences between G-CBT and G-PFT groups at any time point (Tables 1 and 2). There were no significant differences between SI-R scores immediately post-treatment and at longitudinal follow-up (mean difference −0.45, s.d. = 12.7, t = −0.45, d.f. = 182, P = 0.66), indicating that the treatment gains were generally maintained at 3 months post-treatment or later (Fig. 2). However, mean ADL-H scores were higher at follow-up than post-treatment (difference −2.2, s.d. = 10.5, t = –2.68, d.f. = 182, P = 0.008), indicating that gains in function were not as well sustained. Longer time from post-treatment to longitudinal follow-up was associated with worsening SI-R (r = −0.173, P = 0.03) and ADL-H (r = −0.240, P = 0.01) scores. Higher rates of homework completion were associated with better (lower) longitudinal SI-R scores (β = 10.21, s.e. = 3.66, t = 2.79, d.f. = 1, P = 0.006).
Fig. 2.
Hoarding symptom severity scores (SI-R total score) before (PRE-TX), immediately after (POST-TX) and at least 3 months after treatment (longitudinal follow-up, F/U). Dashed line indicates remission cut-off (SI-R < 42). G-CBT, group psychiatrist-led cognitive–behavioural therapy; G-PFT, group peer-facilitated therapy; SI-R, Savings Inventory, Revised.
The remission rate for the longitudinal follow-up was 32.8% for the G-CBT group and 29.4% for the G-PFT group (χ2 = 0.33, d.f. = 1, P = 0.56). There were no statistically significant differences between those who remitted and those who did not, for gender, age, pre-treatment hoarding severity or cognitions, psychiatric comorbidity, treatment completion, group attendance rates or homework completion rates (data not shown). A total of 28 of the 54 participants who achieved remission at post-treatment no longer met remission criteria at longitudinal follow-up, whereas 24 of the 109 participants who did not meet criteria for remission at post-treatment did meet these criteria at longitudinal follow-up.
Of the 176 participants who provided data about ongoing support after treatment, 71.2% continued to receive either formal or informal help for hoarding after the treatments ended. Of these, 71% remained in contact with members of their treatment group, 31% remained in contact with their clutter buddies, 23% attended hoarding support groups (including drop-in groups), 17.5% received formal treatment for hoarding disorder(e.g. by a psychiatrist or psychologist) and 5% had worked with a professional organiser. Further, 38% continued to receive help with hoarding from family and/or friends. Of the 87 who remained in contact with a clutter buddy or treatment group member, or received help from a support group or professional, 83 (95.4%) were still in contact or receiving help from these sources at least 3 months after treatment. There were no significant differences in time to longitudinal follow-up between those who were still in contact or receiving help at longitudinal follow-up and those who were not (t = 1.008, d.f. = 182, P = 0.32).
Of those who continued to receive support with hoarding behaviours post-treatment, only ongoing help from family and/or friends was significantly associated with maintenance of gains. Individuals who received such help had mean longitudinal SI-R scores of 43.9 (s.d. = 13.3), whereas those who did not had mean scores of 50.2 (s.d. = 4.7; t = 2.89, d.f. = 175, P = 0.004, N = 177). A total of 48% of those who met remission criteria at post-treatment and ≥3 months later and 61.8% of those who remitted only at longitudinal follow-up, compared with 26% of those who did not meet criteria for remission at either time point and 21.3% of those who met remission criteria only at post-treatment, received help from family and friends (χ2 = 12.63, d.f. = 3, P = 0.006). No other post-treatment interventions were associated with treatment-response patterns.
Discussion
In this randomised clinical trial of 323 treatment-seeking individuals with hoarding disorder, G-PFT was as effective as G-CBT in reducing hoarding symptom severity, and treatment gains were maintained for at least 3 months. Although effective, the availability of trained mental health professionals who can provide CBT for hoarding disorder is limited,14 and access to care remains a substantial impediment for many individuals and families. Previous small studies have demonstrated the efficacy of peer-facilitated treatment under idealised conditions,13,35,38 but this study is the first, and to our knowledge, the only randomised clinical trial to directly compare peer-facilitated treatment to clinician-led treatment. Our finding that community-based peer-facilitated groups were as effective in treating hoarding disorder as groups led by trained mental health professionals represents a potential paradigm shift, and has important implications for treatment providers, for individuals with hoarding disorder and their families, and for policymakers.
The sample size, which is five times larger than the largest previously published CBT study,11,13 the racial, ethnic, and sociodemographic diversity of the sample, and the study protocol, which was deliberately designed with our community partners to make the implementation of treatment feasible by providers in a community-based practice setting, maximises our confidence in the robustness and generalisability of the findings. Although there was a risk of decreasing treatment response, as we had comparatively few sessions (15 or 16, compared with a previously published range of 13–35), large group sizes (8–12, compared with a previously published range of 6–8), few or no home visits and somewhat less intensive clinician/facilitator training than has been reported previously,11,13 this balance between optimising feasibility and treatment outcomes appears to have paid off. The 25–30% improvement in hoarding symptom severity is consistent with what has been previously reported,11,13 and was similar across treatment types, despite differences in treatment protocols.23–26 Although there is still a long way to go in optimising treatment for hoarding disorder, as only one-third of participants achieved symptomatic remission, over 50% had a clinically significant treatment response (≥14 point improvement), suggesting that most individuals received noticeable benefit from treatment.
Predictors of treatment outcome
Contrary to our hypothesis, the only participant-related variable that consistently independently predicted treatment response in multivariable analyses was more severe hoarding symptoms at baseline. In particular, psychiatric symptoms/diagnoses and neurocognitive status were not predictive of treatment outcome, nor were treatment preferences or beliefs about treatment. In fact, the majority of individuals expressed no strong preference for one type of treatment over another. Similarly, there were no treatment-related variables that independently predicted differential responses to G-CBT or G-PFT in multivariable models. Of interest, however, for the G-PFT but not G-CBT group, higher percentage of homework completed, finding a clutter buddy helpful and mean percentage of groups attended were all associated with treatment improvement in univariable analyses. Similarly, receiving ongoing help from family and friends post-treatment was associated with maintenance of treatment gains at ≥3 months of follow-up. Although possibly discouraging from a precision medicine perspective, which aims to tailor appropriate interventions for individuals based on specific characteristics, these findings reinforce the importance of identifying ways to improve treatment adherence and promote ongoing community engagement (both during and after treatment) to maximise effectiveness and promote ongoing maintenance of gains for this chronic disorder.
Limitations
The primary limitation in this study was loss to follow-up. As has been seen in other studies, approximately 30% of participants dropped out of treatment before completion; we obtained post-treatment data on only 16% of drop-outs. Similarly, the longitudinal follow-up was post hoc rather than being planned before study initiation. As a result, participants were assessed at varying time points after treatment, and we obtained follow-up data on only 55% of randomised participants, with substantial differences between treatment groups (n = 82 for the G-PFT group and n = 101 for the G-CBT group).
As with many studies, as participants typically sought out the hoarding treatment, participants in our study may have had a higher awareness of their disorder than those who did not seek out treatment. Individuals who were screened but did not seek treatment had milder hoarding disorder symptoms and/or less insight into their illness, and therefore may not have seen it as problematic, as has been posited in other hoarding disorder-related research.39,40 Despite our diverse recruitment approaches, most of the participants in the study were female, as has also been seen in previous studies.11
There were also potential limitations to the study design. First, the outcome variables were dependent on self-report measures rather than objective observations. Second, we made several modifications to the published manuals to fit the needs of our intended population and treatment providers, and did not formally assess treatment fidelity. These changes represent a potential weakness of the study, but also a potential strength. For example, although treatment fidelity may not have been as rigorous as in a more controlled trial, a departure from treatment fidelity not only mimics what might happen in a real-world setting, and thus increases generalisability, but would also tend to bias our results toward the null. As the degree of improvement under the protocol described here was similar to what has been previously reported, and the two treatment types did not significantly differ in outcomes despite the departures from previously published work, we feel confident in the results and in their relevance to a treatment-seeking population of individuals with hoarding disorder.
In conclusion, this study, a collaborative effort between an academic medical centre and a community-based advocacy group, provides empirical support for peer-facilitated treatment, thus offering an alternative form of evidence-based treatment that can substantially increase access to care for this chronic and common disorder. The findings of this study underscore the importance of investing resources in building treatment capacity via community entities, and promoting ongoing community engagement in care to provide an additional avenue for effective evidence-based treatment for individuals who do not have ready access to care by mental health professionals. Additional studies should focus on the role that specific elements of treatment (e.g. assigning clutter buddies) play in increasing adherence and/or treatment response.
Funding
This work was supported through a Patient-Centered Outcomes Research Institute (PCORI) Assessment of Prevention, Diagnosis, and Treatment Options Program Award (number CE-1304-6000). The funder had no role in the design and conduct of the study; collection, management, analysis and interpretation of the data; preparation, review or approval of the manuscript or decision to submit the manuscript for publication.
All statements in this report, including its finding and conclusions are solely those of the authors and do not necessarily represent the views of the PCORI, its Board of Governors or Methodology Committee.
Supplementary material
For supplementary material accompanying this paper visit http://dx.doi.org/10.1192/bjo.2018.30.
click here to view supplementary material
References
- 1.American Psychiatric Association A. Diagnostic and Statistical Manual of Mental Disorders (5th edn). American Psychiatric Association, 2013. [Google Scholar]
- 2.Tolin DF, Frost RO, Steketee G, Gray KD, Fitch KE. The economic and social burden of compulsive hoarding. Psychiatry Res 2008; 160(2): 200–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Harris J. Household hoarding and residential fires. Proceedings of Int Congr Appl Psychol, Melbourne, 2010. [Google Scholar]
- 4.Frost RO, Steketee G, Williams L. Hoarding: a community health problem. Health Soc Care Community 2000; 8(4): 229–34. [DOI] [PubMed] [Google Scholar]
- 5.Tolin DF, Frost RO, Steketee G, Fitch KE. Family burden of compulsive hoarding: results of an internet survey. Behav Res Ther 2008; 46(3): 334–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Frost RO, Steketee G, Williams LF, Warren R. Mood, personality disorder symptoms and disability in obsessive compulsive hoarders: a comparison with clinical and nonclinical controls. Behav Res Ther 2000; 38(11): 1071–81. [DOI] [PubMed] [Google Scholar]
- 7.Ayers CR, Saxena S, Golshan S, Wetherell JL. Age at onset and clinical features of late life compulsive hoarding. Int J Geriatr Psychiatry 2010; 25(2): 142–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Frost RO, Steketee G, Tolin DF. Comorbidity in hoarding disorder. Depress Anxiety 2011; 28(10): 876–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mackin RS, Vigil O, Insel P, Kivowitz A, Kupferman E, Hough CM, et al. Patterns of clinically significant cognitive impairment in hoarding disorder. Depress Anxiety 2016; 33(3): 211–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brakoulias V, Eslick GD, Starcevic V. A meta-analysis of the response of pathological hoarding to pharmacotherapy. Psychiatry Res 2015; 229(1–2): 272–6. [DOI] [PubMed] [Google Scholar]
- 11.Tolin DF, Frost RO, Steketee G, Muroff J. Cognitive behavioral therapy for hoarding disorder: a meta-analysis. Depress Anxiety 2015; 32(3): 158–66. [DOI] [PubMed] [Google Scholar]
- 12.Williams M, Viscusi JA. Hoarding disorder and a systematic review of treatment with cognitive behavioral therapy. Cogn Behav Ther 2016; 45(2): 93–110. [DOI] [PubMed] [Google Scholar]
- 13.Mathews CA, Uhm S, Chan J, Gause M, Franklin J, Plumadore J, et al. Treating hoarding disorder in a real-world setting: results from the Mental Health Association of San Francisco. Psychiatry Res 2016; 237: 331–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Muroff J, Steketee G, Himle J, Frost R. Delivery of internet treatment for compulsive hoarding (D.I.T.C.H.). Behav Res Ther 2010; 48(1): 79–85. [DOI] [PubMed] [Google Scholar]
- 15.Koenig TL, Leiste MR, Spano R, Chapin RK. Multidisciplinary team perspectives on older adult hoarding and mental illness. J Elder Abuse Negl 2013; 25(1): 56–75. [DOI] [PubMed] [Google Scholar]
- 16.Muroff J, Steketee G, Frost RO, Tolin DF. Cognitive behavior therapy for hoarding disorder: follow-up findings and predictors of outcome. Depress Anxiety 2014; 31(12): 964–71. [DOI] [PubMed] [Google Scholar]
- 17.Uhm SY, Tsoh JY, Mackin RS, Gause M, Chan J, Franklin J, et al. Comparison of a peer facilitated support group to cognitive behavior therapy: study protocol for a randomized controlled trial for hoarding disorder. Contemp Clin Trials 2016; 50: 98–105. [DOI] [PubMed] [Google Scholar]
- 18.Frost RO, Steketee G, Grisham J. Measurement of compulsive hoarding: saving inventory-revised. Behav Res Ther 2004; 42(10): 1163–82. [DOI] [PubMed] [Google Scholar]
- 19.Saxena S, Ayers CR, Dozier ME, Maidment KM. The UCLA Hoarding Severity Scale: development and validation. J Affect Disord 2015; 175: 488–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Frost RO, Steketee G, Tolin DF, Renaud S. Development and validation of the Clutter Image Rating. J Psychopathol Behav Assess 2008; 30: 193–203. [Google Scholar]
- 21.Nordsletten AE, de la Cruz LF, Pertusa A, Reichenberg A, Hotopf M, Hatch SL, et al. The Structured Interview for Hoarding Disorder (SIHD): development, further validation, and pragmatic usage. J Obsessive Compuls Relat Disord 2013; 2(3): 346–50. [Google Scholar]
- 22.Nasreddine ZS, Phillips NA, Bedirian V, Charbonneau S, Whitehead V, Collin I, et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc 2005; 53(4): 695–9. [DOI] [PubMed] [Google Scholar]
- 23.Steketee G, Frost RO. Compulsive Hoarding and Acquiring: Therapist Guide. Oxford University Press, 2006. [Google Scholar]
- 24.Steketee G, Frost RO. Compulsive Hoarding and Acquiring: Workbook. Oxford University Press, 2007. [Google Scholar]
- 25.Tolin DF, Steketee G, Frost RO. Buried in Treasures: Help for Compulsive Acquiring, Saving, and Hoarding. Oxford University Press, 2007. [Google Scholar]
- 26.Shuer LJ, Frost RO. Leading the Buried in Treasures Workshop: A Facilitator's Manual. Smith College, 2011. (https://www.nationalcouncildocs.net/wp-content/uploads/2013/11/Shuer-Frost-2011-Buried-in-Treasures-Workshop.pdf).
- 27.Frost RO, Hristova V, Steketee G, Tolin DF. Activities of Daily Living Scale in hoarding disorder. J Obsessive Compuls Relat Disord 2013; 2(2): 85–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Steketee G, Frost RO, Kyrios M. Cognitive aspects of compulsive hoarding. Cogn Ther Res 2003; 27(4): 463–79. [Google Scholar]
- 29.Beck AT, Steer RA, Ball R, Ranieri W. Comparison of Beck Depression Inventories -IA and -II in psychiatric outpatients. J Pers Assess 1996; 67(3): 588–97. [DOI] [PubMed] [Google Scholar]
- 30.Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol 1988; 56(6): 893–7. [DOI] [PubMed] [Google Scholar]
- 31.Swanson JM, Schuck S, Mann MM, Carlson C, Hartman CA, Sergeant JA, et al. Categorical and dimensional definitions and evaluations of symptoms of ADHD: the SNAP and the SWAN rating scales. Int J Educ Psychol Assess 2012; 10(1): 51–70. [PMC free article] [PubMed] [Google Scholar]
- 32.Conners CK. Conners’ Continuous Performance Test II: Computer Program for Windows Technical Guide and Software Manual. Multi-Health Systems, 2000. [Google Scholar]
- 33.Benedict RH. Brief Visuospatial Memory Test-Revised. Psychological Assessment Resources, Inc, 1997. [Google Scholar]
- 34.Wechsler D. Wechsler Abbreviated Scale of Intelligence. Psychological Corporation, 1999. [Google Scholar]
- 35.Frost RO, Ruby D, Shuer LJ. The buried in treasures workshop: waitlist control trial of facilitated support groups for hoarding. Behav Res Ther 2012; 50(11): 661–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gilliam CM, Norberg MM, Villavicencio A, Morrison S, Hannan SE, Tolin DF. Group cognitive-behavioral therapy for hoarding disorder: an open trial. Behav Res Ther 2011; 49(11): 802–7. [DOI] [PubMed] [Google Scholar]
- 37.Frost RO, Hristova V. Assessment of hoarding. J Clin Psychol 2011; 67(5): 456–66. [DOI] [PubMed] [Google Scholar]
- 38.Frost RO, Pekareva-Kochergina A, Maxner S. The effectiveness of a biblio-based support group for hoarding disorder. Behav Res Ther 2011; 49(10): 628–34. [DOI] [PubMed] [Google Scholar]
- 39.Grisham JR, Norberg MM. Compulsive hoarding: current controversies and new directions. Dialogues Clin Neurosci 2010; 12(2): 233–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mataix-Cols D, Pertusa A. Annual research review: hoarding disorder: potential benefits and pitfalls of a new mental disorder. J Child Psychol Psychiatry 2012; 53(5): 608–18. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit http://dx.doi.org/10.1192/bjo.2018.30.
click here to view supplementary material