Abstract
Objective
Identify contemporary noise exposures and hearing protection use among adults.
Study Design
Cross-sectional analysis of national health survey.
Methods
Adult respondents in the 2014 National Health Interview Series hearing survey module were analyzed. Potentially harmful exposures to occupational and recreational noises in the past 12 months were extracted and quantified. Patterns of hearing protection use also were analyzed.
Results
Among 239.7 million adults, “loud” and “very loud” occupational noise exposures were reported by 5.3% and 21.7%, respectively. Of those exposed to “loud” or “very loud” sounds at work, only 18.7% and 43.6%, respectively, always used hearing protection. A total of 38.2% (1.9 million) of those with “very loud” occupational exposures never used hearing protection. Frequent (> 10/year) “loud” and “very loud” recreational noise exposures were reported by 13.9% and 21.1%, respectively, most commonly to lawn mowers (72.6% and 55.2%, respectively). When exposed to recreational “loud/very loud” noise, only 11.4% always used hearing protection, whereas 62.3% (6.3 million) never used any protection. Lifetime exposure to firearm noise was reported by 36.6% of adults, 11.5% of whom had used firearms in the prior 12 months. Of those, only 58.5% always used hearing protection, whereas 21.4% (7.4 million) never used hearing protection.
Conclusion
Substantial noise exposures with potentially serious long-term hearing health consequences frequently are occurring in occupational and recreational settings, and with the use of firearms. Only a minority of those exposed consistently are using hearing protection. Healthcare providers should actively identify and encourage the use of hearing protection with those patients at risk.
Keywords: Firearms, noise exposure, recreational noise, hearing protection
INTRODUCTION
Chronic high-intensity noise exposure is a common environmental hazard in the United States, which can not only lead to hearing loss and tinnitus1–3 but also can contribute to the development of numerous other health issues, including sleep disturbance, cardiovascular disease,4,5 and diabetes.6,7 Similarly, acute exposure to short bursts of intense sound also can result in noise-induced temporary or permanent hearing loss.8–11 Recent animal studies have provided remarkable insight into the impact of noise exposure on the auditory system, including acute loss of afferent synaptic terminals followed by degeneration of the cochlear nerve in a delayed fashion, with even mild noise traumas resulting in temporary shifts in hearing thresholds.8,12,13 In certain cases, this synaptopathy will have a negligible impact on standard audiometry, although it can lead to a compromised ability in understanding complex auditory stimuli.14,15 Furthermore, the subsequent degeneration of auditory neurons has been suggested to contribute to hearing difficulties in challenging listening environments, tinnitus, and hyperacusis.16,17
Although occupational noise historically has been the primary source of chronic high-intensity noise exposure, there increasing is evidence of clinically relevant contributions from other sources. For example, music from compact disc (CD) and MP3 players has been shown to increase the risk of noise-induced permanent threshold shifts.18 Moreover, even short exposures from loud concerts, sporting events, or use of power tools may have a permanent impact on hearing.19,20 The extent of this type of leisure or recreational noise exposure often is underappreciated, and there are no existing regulations for its control or guidelines for hearing protection. As such, millions of Americans may be exposed to high-intensity sounds, potentially resulting in previously unrecognized long-term effects on the auditory system.2,21,22
In addition to loud household appliances, firearms are another common source of occupational and recreational noise. Notably, there are an estimated 310 million firearms in the United States,23 and more than 23 million new background checks for firearms were performed in 2015—more than double the number of checks performed in 1999.24 In 2014, an estimated 31% of U.S. households possess a gun.25
Given the suspected commonality of these often hidden and unrecognized noise exposures, we sought to quantify and evaluate the prevalence of high-intensity work, recreational, and firearms exposures among U.S. adults. We utilized the National Health Interview Series (NHIS), which has collected information on a broad range of health topics through personal household interviews in the United States since the 1950s.26,27 In particular, the 2014 NHIS contains a survey module on hearing, which was analyzed for exposure patterns, as well as use of hearing protection during common noisy environments.
MATERIALS AND METHODS
Adult responses in the household-based 2014 NHIS were analyzed as aggregated in the Integrated Health Interview Series. The study protocol was deemed exempt from review by our Committee on Clinical Investigations because it analyzes de-identified data that are publicly available. Data from responses in the hearing modules were extracted for all adult patients age 18.0 and older and imported into SPSS (version 22.0, IBM Corp., Armonk, NY) for analysis.
The self-reported incidence of noise exposure was evaluated at work and at leisure-time activities. At work, the noise exposure had to have occurred for at least 4 hours a day, several days a week. When outside of work, a positive response in the survey was defined as at least 10 exposures in the year during any of the following activities: lawn mowers, power tools, household appliances, recreational vehicles, rock concerts or clubs and bars, music players such as iPods and MP3 players, loud sporting events, firearms, video/computer games, and others. When meeting the above criteria, the data were evaluated for exposure in the prior 12 months. Additionally, data for the use of hearing protection were also analyzed under these conditions.
All respondents were specifically asked to characterize the noise exposure as “loud” or “very loud,” and these subgroups were independently analyzed. “Loud” was defined as noise that is so loud that a raised voice must be used to be heard, whereas “very loud” was defined as noise so intense that shouting volumes must be used to be heard at 3 feet (arm’s length). Additionally, firearms use in both work and recreational settings was analyzed. Further subgroup analysis was performed to evaluate where the firearms were used in occupational or leisure settings, the number of rounds fired in the last year, and the frequency of hearing protection use.
The raw sample size was extrapolated to representative statistics for the national population in the United States by using sample weights and survey statistics that account for the weighted and stratified survey design. The data are reported as the mean with its associated standard error. Statistical comparisons were conducted with chi-square, with significance set at P ≤ 0.05.
RESULTS
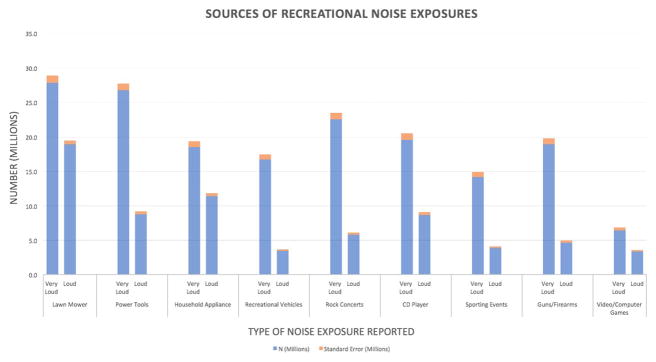
Among the 239.7 million ± 2.5 million subjects (raw = 36,697), mean age was 47.0 years, with 51.8% female respondents. The sampled cohort (Fig. 1) was distributed in the South (37.2%), Midwest (23.0%), West (22.5%), and Northeast (17.3%). While at work, 21.7% of respondents reported “very loud” sound exposure in the last 12 months, at least 4 hours a day, several times a week, requiring them to shout in order to be understood at arm’s length. In this cohort, 33.7% report having greater than 15 years of such noise exposure (Table I), 43.6% always used hearing protection in the last year, whereas 38.2% (1.9 million) never did (Table I). In contrast, 5.3% of respondents reported “loud” sound exposure at work, mostly commonly in the last 1 to 2 years (22.7%), as seen in Table II. These respondents used hearing protection less frequently because 67.3% never used hearing protection when exposed to loud sounds (Table II).
Fig. 1.
Geographic region of respondents. Distribution of respondents in the United States.
Table 1.
Occupational “Very Loud” Sounds Exposure With Duration of Exposure and Use of Hearing Protection in the Last Year.
| N (millions) | SE (millions) | Percent Total (%) | SE (%) | |
|---|---|---|---|---|
| Very Loud Sounds | 48.9 | 1.1 | 21.7 | 0.4 |
| Exposure | ||||
| In last year | 5.0 | 0.3 | 10.2 | 0.5 |
| Before last year | 29.0 | 0.8 | 59.5 | 0.9 |
| During and before last year | 14.8 | 0.5 | 30.3 | 0.8 |
| Duration of Exposure | ||||
| Less than 3 months | 3.3 | 0.2 | 6.7 | 0.4 |
| 3–11 months | 4.6 | 0.2 | 9.5 | 0.5 |
| 1–2 years | 6.0 | 0.4 | 12.3 | 0.7 |
| 3–4 years | 5.3 | 0.3 | 11.0 | 0.5 |
| 5–9 years | 7.1 | 0.3 | 14.7 | 0.6 |
| 10–14 years | 5.9 | 0.3 | 12.1 | 0.5 |
| 15 years or more | 16.4 | 0.5 | 33.7 | 0.9 |
| Hearing Protection Used in the Last 12 Months | ||||
| N (Millions) | SE (Millions) | Percent Total (%) | SE (%) | |
| Always | 2.2 | 0.2 | 43.6 | 2.7 |
| Sometimes | 0.9 | 0.1 | 18.2 | 2.2 |
| Never | 1.9 | 0.2 | 38.2 | 2.7 |
SE = standard error of the population estimate.
Table 2.
Occupational “Loud” Sounds Exposure With Duration of Exposure and Use of Hearing Protection in the Last Year.
| N (thousands) | SE (thousands) | Percent Total (%) | SE (%) | |
|---|---|---|---|---|
| Loud Sounds | 9,347 | 364 | 5.3 | 0.2 |
| Exposure | ||||
| In last year | 1,150 | 114 | 12.3 | 1.1 |
| Before last year | 5,167 | 234 | 55.4 | 1.9 |
| During and before last year | 3,001 | 236 | 32.2 | 1.9 |
| Duration of Exposure | ||||
| Less than 3 months | 746 | 94 | 10.4 | 1.2 |
| 3–11 months | 297 | 128 | 18.1 | 1.5 |
| 1–2 years | 1,622 | 137 | 22.7 | 1.6 |
| 3–4 years | 1,139 | 115 | 15.9 | 1.5 |
| 5–9 years | 1,366 | 113 | 19.1 | 1.5 |
| 10–14 years | 913 | 99 | 12.8 | 1.3 |
| Refused | 27 | 20 | 0.4 | 0.3 |
| Don’t know | 50 | 25 | 0.7 | 0.4 |
| Hearing Protection Used in the Last 12 Months | ||||
| Always | 216 | 46 | 18.7 | 3.6 |
| Sometimes | 161 | 38 | 14.0 | 3.1 |
| Never | 774 | 95 | 67.3 | 4.3 |
SE = standard error of the population estimate.
When asked about the use of firearms, 36.6% of all respondents reported having fired a firearm in their lifetime. Of those, 76.6% (67.0 million) reported having fired one for recreational purposes (Table III). Although the majority users (59.6%) fired fewer than 100 rounds, there were 2.9 million (8.4%) who reported firing between 1,000 to 10,000 rounds. Of those, only 67.0% used hearing protection consistently, as noted in Table IV. Overall, 58.5% of all respondents used hearing protection at all times, whereas 21.4% never did. The use of hearing protection was more common in occupational use of firearms (77.9% always used hearing protection at work), whereas only 56.3% used it consistently with recreational use (P <0.001).
Table 3.
Firearms Exposure: Firearms Use and Estimated Number of Rounds Fired in the Prior 12 Months.
| N (millions) | SE (millions) | Percent Total (%) | SE (%) | |
|---|---|---|---|---|
| Ever Use Firearms | ||||
| Yes | 87.6 | 1.6 | 36.6 | 0.5 |
| No | 151.0 | 18.0 | 63.4 | 0.5 |
| Purpose for Firearms Use | ||||
| Work | 10.3 | 0.4 | 11.8 | 0.4 |
| Leisure | 67.0 | 1.4 | 76.6 | 0.6 |
| Both | 10.2 | 0.4 | 11.6 | 0.4 |
| When Did You Use Them | ||||
| In the last 12 months | 10.0 | 0.4 | 11.5 | 0.4 |
| Over 1 year ago | 52.5 | 1.1 | 60.1 | 0.6 |
| Both | 24.7 | 0.7 | 28.4 | 0.6 |
| Number of Rounds (12 months) | ||||
| 1 to less than 100 rounds | 20.3 | 0.6 | 59.6 | 1.0 |
| 100 to less than 1,000 rounds | 10.4 | 0.4 | 30.5 | 0.9 |
| 1000 to less than 10,000 rounds | 2.9 | 0.2 | 8.4 | 0.6 |
| 10,000 rounds or more | 0.5 | 0.0 | 1.5 | 0.3 |
SE = standard error of the population estimate.
Table 4.
Use of Hearing Protection With Firearms: Rates of Hearing Protection Use and Relationship of Use of Protection With Number of Rounds Fired.
| N (millions) | SE (millions) | Percent Total (%) | SE (%) | |
|---|---|---|---|---|
| Hearing Protection With Firearms (last 12 months) | ||||
| Always | 20.3 | 0.6 | 58.5 | 1.0 |
| Sometimes | 6.9 | 0.3 | 20.0 | 0.8 |
| Never | 7.6 | 0.4 | 21.4 | 0.9 |
| Hearing Protection at Work-Related Use of Firearms | ||||
| Always | 1.4 | 0.1 | 77.9 | 3.5 |
| Sometimes | 0.2 | 0.05 | 10.7 | 2.5 |
| Never | 0.2 | 0.05 | 11.5 | 2.8 |
| Hearing Protection at Leisure Use of Firearms | ||||
| Always | 15.6 | 0.5 | 56.3 | 1.3 |
| Sometimes | 5.8 | 0.3 | 20.8 | 0.9 |
| Never | 6.3 | 0.3 | 22.9 | 1.0 |
| Hearing Protection Used Related to Rounds Fired in Last 12 months | ||||
| 1–100 rounds | ||||
| Always | 10.1 | 0.4 | 53.2 | 1.5 |
| Sometimes | 3.8 | 0.2 | 18.5 | 1.0 |
| Never | 5.7 | 0.3 | 28.3 | 1.3 |
| 100 to less than 1,000 rounds | ||||
| Always | 7.0 | 0.3 | 67.0 | 1.8 |
| Sometimes | 2.2 | 0.2 | 21.5 | 1.7 |
| Never | 1.2 | 0.1 | 11.5 | 1.1 |
| 1,000 to less than 10,000 rounds | ||||
| Always | 1.9 | 0.2 | 66.6 | 3.0 |
| Sometimes | 0.7 | 0.1 | 23.4 | 2.7 |
| Never | 0.3 | 0.1 | 10.0 | 1.8 |
| 10,000 or more rounds | ||||
| Always | 0.3 | 0.1 | 53.4 | 8.2 |
| Sometimes | 0.1 | 0.04 | 26.3 | 6.9 |
| Never | 0.1 | 0.04 | 20.3 | 7.1 |
SE = standard error of the population estimate.
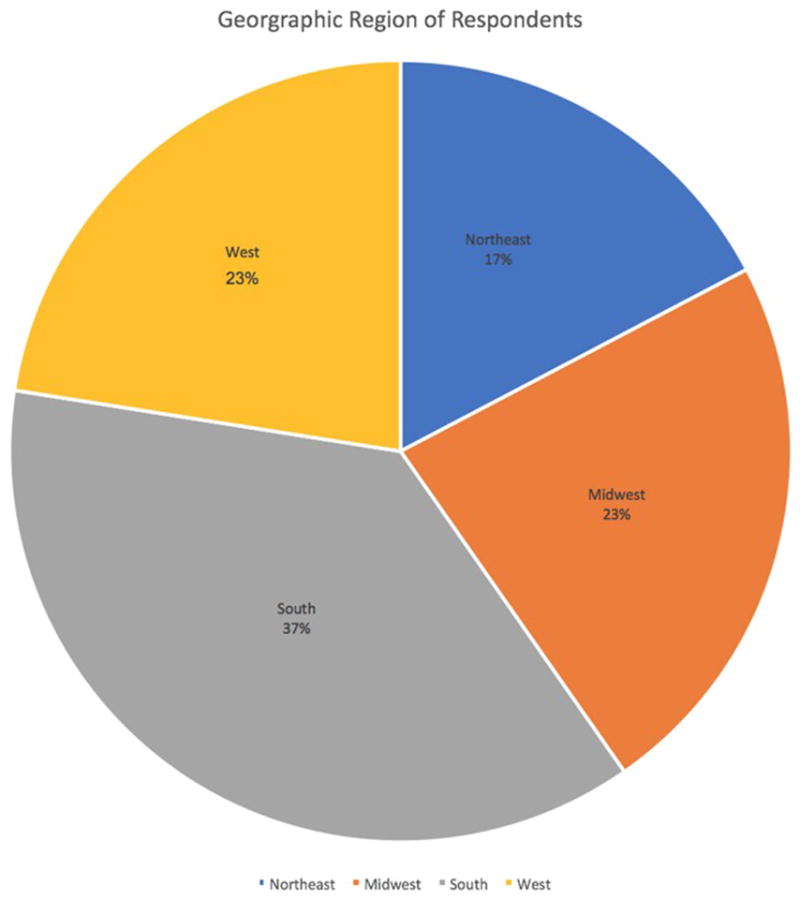
Noise exposures greater than 10 times per year in leisure/recreational settings were also queried. “Very loud” sound exposure was more common (21.1%), whereas only 13.9% were exposed to “loud” sounds. The most common noise exposure was the lawn mower for both levels of exposure, followed by power tools for “very loud” sounds (52.9%) and household appliances (43.7%) (Fig. 2). When exposed to recreational “loud” or “very loud” noises, only 11.4% always used hearing protection, and 62.3% (6.3 million) never used any hearing protection (Table V).
Fig. 2.
Sources of recreational noise exposures. Most commonly reported lifetime recreational noise exposures, with at least 10 exposures per year.
Table 5.
Hearing Protection Use During Recreational Noise Exposure in the Prior 12 Months.
| Hearing Protection | ||||
|---|---|---|---|---|
| During Last 12 Months | N (millions) | SE (millions) | Percent Total (%) | SE (%) |
| Always | 1.2 | 0.1 | 11.4 | 1.3 |
| Sometimes | 2.7 | 0.2 | 26.3 | 1.6 |
| Never | 6.3 | 0.3 | 62.3 | 1.9 |
SE = standard error of the population estimate.
Additionally, when examining the subset of respondents with very high intensity (“very loud”) current work noise exposure, we found that among these individuals, 41.7% and 31.6% also reported exposure to very high-intensity recreational and firearms noise, respectively, in the prior 12 months. Furthermore, 15.6% had both nonwork-related very high-intensity noise exposures.
DISCUSSION
Noise-induced hearing loss (NIHL) is considered to be one of the most common occupational health concerns in the United States because both chronic high-intensity noise and intense impulse noise can have detrimental effects on human hearing.28 Although both types of noise trauma are harmful, some believe that impulse noise may be even more deleterious to hearing than continuous noise.29 Effects of NIHL may be exacerbated with age-related threshold shifts because the body undergoes summative loss from impulse noise and chronic noise exposure, resulting in clinically significant hearing loss over time.30 Occupational groups at the highest risk of NIHL are military personnel, construction workers, and farmers, among others29; however, even in the everyday environment of the current technologically advanced world, nearly all people are susceptible to acoustic trauma.
In 1981, the United States Occupational Safety and Health Administration (OSHA) created noise exposure guidelines and standards for workers in the manufacturing and service sectors out of concern for the harmful effects of occupational acoustic exposure.28 They mandated a limit of 8 hours of exposure to an average of 85 dBA, along with company-sponsored annual hearing exams, training, and hearing protection. However, as evident from our data, fewer than half of the respondents use hearing protection regularly in occupational settings when exposed to “loud” and “very loud” sounds for greater than several hours a day. In fact, an overwhelming majority of respondents who are exposed to “loud” sounds never have used hearing protection in occupational settings; accordingly, occupational hearing protection should be discussed when evaluating a patient with hearing loss or tinnitus. Given that 0.91 million (18.2%) and 1.9 million (38.2%) workers sometimes or never, respectively, used hearing protection at work when exposed to very intense sounds in the last year, a case could be made for screening at the primary care level or other interventions to identify these at risk populations.
In addition to occupational noise trauma, high-intensity noise exposures also can occur during recreational or leisure time, and can be associated with hearing loss as well as tinnitus.27 Similarly, in a population-based study, Dalton et al. reported that recreational noise from woodworking (100 dBA+), metalworking (100 dBA+), and chainsaw use (125 dBA), among others, produced an increased risk of a hearing loss.21,31 Other impulse noises can present in the form of firearms (150 dBA+), music players (100 dBA+), household appliances (80 dBA+), rock concerts (110–120 dBA), and sports venues (110 dBA+).31 These types of impulse noises frequently were reported in our cohort, with the lawnmower— which can generate sound pressure levels of over 100 dBA noise level—as the most commonly reported “loud” and a “very loud” sound exposure. 32 Such sound levels at a worksite would mandate a limitation of 2 hours per day with hearing protection per OSHA guidelines.28 Other common sources of “loud” and “very loud” sounds are shown in Figure 2. Our data not only highlight the widespread use of equipment that can be “very loud,” but more importantly, that an overwhelming 62.3% of Americans never use hearing protection while operating such machinery. Healthcare providers should therefore screen for and counsel their patients on the use of hearing protection in such environments because the use of hearing protection such as ear plugs can be beneficial in preventing hearing loss from recreational noise exposures.19
The prevalence of hearing loss in adolescents has been increasing, from 14.9% in 1988 to 1994 to 19.5% in 2005 to 2006,33 which may be attributable to an environment increasingly filled with amplified sounds. Since the rise in CD/MP3 player popularity in the 2000s, there has been concern that long-term exposure to high-intensity music would increase the risk of hearing loss.34 As common users of MP3 players and gaming systems, children and young adults may be particular at risk35,36 because, although the newer generations of MP3 players have an upper-volume limit, these devices still can generate sounds up to 100 dBA.37 This exposure should be monitored because sustained listening to high-intensity music at such unsafe levels can have a detrimental effect on hearing.38,39 Nearly a third of the respondents indicate that they repeatedly have been exposed to “loud” and “very loud” sounds (Fig. 2) with a music player; thus, screening for high-intensity music noise exposure in children and adults is of paramount importance.
Exposures to short-impulse noise, including from firearm use, have been shown to exacerbate age-related hearing loss, and have been estimated to contribute an additional 7 to 8 dBA of hearing loss.40 Helfer et al. noted a higher incidence of hearing loss and tinnitus in military personnel following deployment,41,42 and the authors suggest that this is the likely consequence of firearm and impulse noise exposures. In a large population-based study, Nondahl et al. found a significant association between recreational shooting and hearing loss.43 It is well-established that sounds above 140 dBA can cause permanent hearing damage, and nearly all firearms can surpass this level.44,45 Consequently, just one round may be sufficient to create noise-induced threshold shifts,46 contributing to cumulative auditory damage.44,47,48 Interestingly, we found that over a third (36.6%) of Americans have used a firearm, predominantly in recreational settings, and over 40% of this group have fired over 100 rounds in the past 12 months. Notably, only 58.5% of those who shot firearms used hearing protection consistently in the last year, whereas the remainder inconsistently or never used hearing protection. Additionally, an astonishingly high percentage (20.3%) of those who shot greater than 10,000 rounds in the past 12 months never used any protection. Given these data, screening for firearms use and discussing the benefits of regular hearing protection use by health-care providers could improve the hearing health of a large segment of the American population.
There are several limitations to our study, including the subjective nature of the responses to these questions, because personal definitions of “loud” and “very loud” sounds will vary. However, in the survey questionnaire these were defined as practical levels with respect to the survey respondent (e.g., “very loud” as a sound requiring them to shout to be understood at an arm’s length). Interestingly, these very same qualifiers for noise level likely could be adapted into screening questions for noise exposures at the primary care level. Additionally, audiometric data for survey respondents are not available; therefore, it is difficult to establish a causative relationship between these noise exposures and hearing loss, if present. Furthermore, the potential for recall bias in the respondents is of significance. Respondents may have misremembered the true nature of the quality and quantity of noise exposure in both recreational and occupational settings. Nevertheless, the strongest attribute of our study is the utilization of a large database that samples the general citizen population in the United States. The respondents in the NHIS are surveyed from all the 50 states and District of Columbia, with a nonzero probability of selection. As such, the current data provide the most contemporary, large-scale insight into noise exposures in the U.S. adult population.
CONCLUSION
This 2014 NHIS survey highlights the common sources of “loud” and “very loud” continuous and impulse noises in the daily life of a person living in the United States, ranging from occupational hazards to common household tools such as lawn mowers, power tools, music players, and video games. Substantial noise exposures with potentially serious long-term hearing health consequences also are frequently occurring with use of firearms. In most settings, only a minority of those exposed consistently are using hearing protection during noise exposure. Due to the short- and long-term sequelae of noise-induced auditory trauma, healthcare providers should actively identify and encourage the use of hearing protection among those patients at risk.
Footnotes
Institutions where work was performed: University of California, Irvine, Irvine, California, U.S.A, and Harvard Medical School, Boston, Massachusetts, U.S.A.
Presented as an oral presentation at The Triological Society 2017 Combined Sections Meeting, New Orleans, Louisiana, U.S.A., January 19–21, 2017.
Level of Evidence: 4.
The authors have no funding, financial relationships, or conflicts of interest to disclose.
BIBLIOGRAPHY
- 1.Stamper GC, Johnson TA. Auditory function in normal-hearing, noise-exposed human ears. Ear Hear. 2015;36:172–184. doi: 10.1097/AUD.0000000000000107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Basner M, Babisch W, Davis A, et al. Auditory and non-auditory effects of noise on health. Lancet. 2014;383:1325–1332. doi: 10.1016/S0140-6736(13)61613-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Garcia A, Boston M. Environmental Urban Noise. Boston, MA: Wentworth Institute of Technology Press; 2001. [Google Scholar]
- 4.Passchier-Vermeer W, Passchier WF. Noise exposure and public health. Environ Health Perspect. 2000;108(suppl 1):123–131. doi: 10.1289/ehp.00108s1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stansfeld S, Crombie R. Cardiovascular effects of environmental noise: research in the United Kingdom. Noise Health. 2011;13:229–233. doi: 10.4103/1463-1741.80159. [DOI] [PubMed] [Google Scholar]
- 6.Sorensen M, Andersen ZJ, Nordsborg RB, et al. Long-term exposure to road traffic noise and incident diabetes: a cohort study. Environ Health Perspect. 2013;121:217–222. doi: 10.1289/ehp.1205503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Belojevic G, Paunovic K. Recent advances in research on non-auditory effects of community noise. Srp Arh Celok Lek. 2016;144:94–98. doi: 10.2298/sarh1602094b. [DOI] [PubMed] [Google Scholar]
- 8.Kujawa SG, Liberman MC. Adding insult to injury: cochlear nerve degeneration after “temporary” noise-induced hearing loss. J Neurosci. 2009;29:14077–14085. doi: 10.1523/JNEUROSCI.2845-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rezaee M, Mojtahed M, Ghasemi M, Saedi B. Assessment of impulse noise level and acoustic trauma in military personnel. Trauma Mon. 2012;16:182–187. doi: 10.5812/kowsar.22517464.2674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Howgate S, Plack CJ. A behavioral measure of the cochlear changes underlying temporary threshold shifts. Hear Res. 2011;277:78–87. doi: 10.1016/j.heares.2011.03.009. [DOI] [PubMed] [Google Scholar]
- 11.Suter A. Standards and Regulations. Fairfax, VA: American Industrial Hygiene Association; 2000. [Google Scholar]
- 12.Lin HW, Furman AC, Kujawa SG, Liberman MC. Primary neural degeneration in the guinea pig cochlea after reversible noise-induced threshold shift. J Assoc Res Otolaryngol. 2011;12:605–616. doi: 10.1007/s10162-011-0277-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Furman AC, Kujawa SG, Liberman MC. Noise-induced cochlear neuropathy is selective for fibers with low spontaneous rates. J Neurophysiol. 2013;110:577–586. doi: 10.1152/jn.00164.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bharadwaj HM, Verhulst S, Shaheen L, Liberman MC, Shinn-Cunningham BG. Cochlear neuropathy and the coding of supra-threshold sound. Front Syst Neurosci. 2014;8:26. doi: 10.3389/fnsys.2014.00026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bramhall N, Ong B, Ko J, Parker M. Speech perception ability in noise is correlated with auditory brainstem response wave I amplitude. J Am Acad Audiol. 2015;26:509–517. doi: 10.3766/jaaa.14100. [DOI] [PubMed] [Google Scholar]
- 16.Liberman MC. Noise-induced hearing loss: permanent versus temporary threshold shifts and the effects of hair cell versus neuronal degeneration. Adv Exp Med Biol. 2016;875:1–7. doi: 10.1007/978-1-4939-2981-8_1. [DOI] [PubMed] [Google Scholar]
- 17.Tremblay KL, Pinto A, Fischer ME, et al. Self-reported hearing difficulties among adults with normal audiograms: the Beaver Dam offspring study. Ear Hear. 2015;36:e290–e299. doi: 10.1097/AUD.0000000000000195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lewis RC, Gershon RR, Neitzel RL. Estimation of permanent noise-induced hearing loss in an urban setting. Environ Sci Technol. 2013;47:6393–6399. doi: 10.1021/es305161z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ramakers GG, Kraaijenga VJ, Cattani G, van Zanten GA, Grolman W. Effectiveness of earplugs in preventing recreational noise-induced hearing loss: a randomized clinical trial. JAMA Otolaryngol Head Neck Surg. 2016;142:551–558. doi: 10.1001/jamaoto.2016.0225. [DOI] [PubMed] [Google Scholar]
- 20.Kraaijenga VJ, Ramakers GG, Grolman W. The effect of earplugs in preventing hearing loss from recreational noise exposure: a systematic review. JAMA Otolaryngol Head Neck Surg. 2016;142:389–394. doi: 10.1001/jamaoto.2015.3667. [DOI] [PubMed] [Google Scholar]
- 21.Dalton DS, Cruickshanks KJ, Wiley TL, Klein BE, Klein R, Tweed TS. Association of leisure-time noise exposure and hearing loss. Audiology. 2001;40:1–9. [PubMed] [Google Scholar]
- 22.Scientific Committee on Emerging and Newly Identified Health Risks. Potential health risks of exposure to noise from personal music players and mobile phones including a music playing function: preliminary report. Brussels, Belgium: SCENIHR European Commission; 2008. [Google Scholar]
- 23.Desilver D. [Accessed July 15, 2016];A minority of Americans own guns, but just how many is unclear. 2016 Jul 15; Available at: http://www.pewresearch.org/fact-tank/2013/06/04/a-minority-of-americans-own-guns-but-just-how-many-is-unclear/
- 24.NICS Firearm Checks: Month/Year. Federal Bureau of Investivation; 2016. [Accessed July 16, 2016]. https://www.fbi.gov/file-repository/nics_firearm_checks_-_month_year.pdf. [Google Scholar]
- 25.Son JTS. General Social Survey Final Report: Trends in Gun Ownership in the United States NORC at the University of Chicago. Chicago, IL: NORC at the University of Chicago; 2015. [Accessed July 15, 2016]. http://www.norc.org/PDFs/GSS%20Reports/GSS_Trends%20in%20Gun%20Ownership_US_1972-2014.pdf. [Google Scholar]
- 26.Bhatt JM, Bhattacharyya N, Lin HW. Relationships between tinnitus and the prevalence of anxiety and depression. Laryngoscope. 2017;127:466–469. doi: 10.1002/lary.26107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bhatt JM, Lin HW, Bhattacharyya N. Prevalence, severity, exposures, and treatment patterns of tinnitus in the United States. JAMA Otolaryngol Head Neck Surg. 2016;142:959–965. doi: 10.1001/jamaoto.2016.1700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.United States Department of Labor, OSHA. [Accessed August 1, 2016];Occupational Noise Exposure. Available at: https://www.osha.gov/SLTC/noisehearingconservation/
- 29.Lie A, Skogstad M, Johannessen HA, et al. Occupational noise exposure and hearing: a systematic review. Int Arch Occup Environ Health. 2016;89:351–372. doi: 10.1007/s00420-015-1083-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dobie RA. The burdens of age-related and occupational noise-induced hearing loss in the United States. Ear Hear. 2008;29:565–577. doi: 10.1097/AUD.0b013e31817349ec. [DOI] [PubMed] [Google Scholar]
- 31.Center for Hearing and Communication, The Noise Center. [Accessed August 21 2016];Common Environmental Noise Levels. Available at: http://chchearing.org/noise/common-environmental-noise-levels/
- 32.American Speech-Language-Hearing Association (ASHA) [Accessed August 16 2016];Noise. Available at: http://www.asha.org/public/hearing/Noise/
- 33.Shargorodsky J, Curhan SG, Curhan GC, Eavey R. Change in prevalence of hearing loss in US adolescents. JAMA. 2010;304:772–778. doi: 10.1001/jama.2010.1124. [DOI] [PubMed] [Google Scholar]
- 34.Zhao F, Manchaiah VK, French D, Price SM. Music exposure and hearing disorders: an overview. Int J Audiol. 2010;49:54–64. doi: 10.3109/14992020903202520. [DOI] [PubMed] [Google Scholar]
- 35.Harrison RV. The prevention of noise induced hearing loss in children. Int J Pediatr. 2012;2012:473541. [Google Scholar]
- 36.Gilles A, Schlee W, Rabau S, Wouters K, Fransen E, Van de Heyning P. Decreased speech-in-noise understanding in young adults with tinnitus. Front Neurosci. 2016;10:288. doi: 10.3389/fnins.2016.00288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Torre P., 3rd Young adults’ use and output level settings of personal music systems. Ear Hear. 2008;29:791–799. doi: 10.1097/AUD.0b013e31817e7409. [DOI] [PubMed] [Google Scholar]
- 38.Thorne P. Noise induced hearing loss: final report. Aukland, NZ: Auckland UNIservices; 2006. [Accessed July 20, 2016]. http://www.acc.co.nz/DIS_EXT_CSMP/groups/external_ip/documents/internet/wim2_065096.pdf. [Google Scholar]
- 39.Ivory R, Kane R, Diaz RC. Noise-induced hearing loss: a recreational noise perspective. Curr Opin Otolaryngol Head Neck Surg. 2014;22:394–398. doi: 10.1097/MOO.0000000000000085. [DOI] [PubMed] [Google Scholar]
- 40.Tambs K, Hoffman HJ, Borchgrevink HM, Holmen J, Samuelsen SO. Hearing loss induced by noise, ear infections, and head injuries: results from the Nord-Trondelag Hearing Loss Study. Int J Audiol. 2003;42:89–105. doi: 10.3109/14992020309078340. [DOI] [PubMed] [Google Scholar]
- 41.Helfer TM, Jordan NN, Lee RB, Pietrusiak P, Cave K, Schairer K. Noise-induced hearing injury and comorbidities among postdeployment U.S. Army soldiers: April 2003–June 2009. Am J Audiol. 2011;20:33–41. doi: 10.1044/1059-0889(2011/10-0033). [DOI] [PubMed] [Google Scholar]
- 42.Helfer TM, Jordan NN, Lee RB. Postdeployment hearing loss in U.S. Army soldiers seen at audiology clinics from April 1, 2003, through March 31, 2004. Am J Audiol. 2005;14:161–168. doi: 10.1044/1059-0889(2005/018). [DOI] [PubMed] [Google Scholar]
- 43.Nondahl DM, Cruickshanks KJ, Wiley TL, Klein R, Klein BE, Tweed TS. Recreational firearm use and hearing loss. Arch Fam Med. 2000;9:352–357. doi: 10.1001/archfami.9.4.352. [DOI] [PubMed] [Google Scholar]
- 44.Flamme GA, Stewart M, Meinke D, Lankford J, Rasmussen P. Auditory risk to unprotected bystanders exposed to firearm noise. J Am Acad Audiol. 2011;22:93–103. doi: 10.3766/jaaa.22.2.4. [DOI] [PubMed] [Google Scholar]
- 45.Stewart M. Recreational Firearm Noise Exposure. American Speech-Language-Hearing Association (ASHA); [Accessed August 5, 2016]. Available at: http://www.asha.org/public/hearing/Recreational-Firearm-Noise-Exposure/ [Google Scholar]
- 46.Pawlaczyk-Luszczynska M, Dudarewicz A, Bak M, Fiszer M, Kotylo P, Sliwinska-Kowalska M. Temporary changes in hearing after exposure to shooting noise. Int J Occup Med Environ Health. 2004;17:285–293. [PubMed] [Google Scholar]
- 47.Segal S, Eviatar E, Lapinsky J, Shlamkovitch N, Kessler A. Inner ear damage in children due to noise exposure from toy cap pistols and firecrackers: a retrospective review of 53 cases. Noise Health. 2003;5:13–18. [PubMed] [Google Scholar]
- 48.Flamme GA, Wong A, Liebe K, Lynd J. Estimates of auditory risk from outdoor impulse noise. II: Civilian firearms. Noise Health. 2009;11:231–242. doi: 10.4103/1463-1741.56217. [DOI] [PubMed] [Google Scholar]