Abstract
Polyneuropathy, organomegaly, endocrinopathy, monoclonal gammopathy and skin changes (POEMS) syndrome is a rare systemic disease, often unrecognised in the primary care setting. POEMS syndrome is associated with plasma cell dyscrasias and upregulation of vascular endothelial growth factor leading to systemic oedema, papilloedema and pulmonary hypertension. A wide constellation of presenting symptoms often leads to late diagnosis. Unrecognised and untreated disease rapidly leads to death from neuropathic exhaustion or cardiopulmonary failure. Treatment is extrapolated from other plasma cell dyscrasias such as multiple myeloma. Autologous peripheral blood stem cell transplantation (PBSCT) is often an important component of treatment. There is no established standard of care for POEMS syndrome. Therapies include lenalidomide, bortezomib and targeted monoclonal antibodies. We present a patient with POEMS syndrome who achieved rapid complete response to triple therapy consisting of lenalidomide, cyclophosphamide and prednisone, followed by high-dose chemotherapy and PBSCT.
Keywords: cancer intervention, haematology (drugs and medicines), peripheral nerve disease, monoclonal gammopathy of undetermined significance associated neuropathy
Background
POEMS syndrome is a rare paraneoplastic syndrome secondary to an underlying plasma cell neoplasm characterised by polyneuropathy, organomegaly, endocrinopathy, monoclonal protein and skin changes.1 While the pathogenesis is poorly understood, vascular endothelial growth factor (VEGF), a cytokine that regulates endothelial cell proliferation, is commonly expressed and correlates with disease activity and response to therapy.2 3 The driver versus passenger role of plasma cells and associated monoclonal gammopathy is not well characterised. The monoclonal component may be a driving factor as therapies targeting plasma cells have shown promising results. VEGF is expressed by osteoblasts, macrophages, tumour cells and plasma cells and regulates endothelial cell proliferation, migration and permeability.2 3 While POEMS syndrome is treated by haematologist-oncologists, general internists are most likely to first encounter patients with POEMS syndrome. Thus, familiarity and working diagnostic knowledge of this entity are most certain to lead to early recognition, appropriate referral and early treatment.
Case presentation
A previously healthy 33-year-old woman was evaluated at our centre for 1 year history of progressive fatigue, 40 pound weight loss, dyspnoea, bilateral lower extremity polyneuropathy and bilateral drop foot. Two years prior to presentation, she developed progressive paraesthesia of bilateral distal lower extremities followed by significant lower extremity swelling and hypertension (190/110 mm Hg) for which she started carvedilol 10 mg two times a day. A transthoracic echocardiogram (TTE) was normal. Her neuropathy continued to worsen with paraesthesias and cold dysaesthesia extending proximally to her knees over the ensuing 12 months. Neurological examination 6 months prior to presentation revealed 2/5 motor strength of bilateral toe and ankle flexors, diminished reflexes and abnormal sensory examination consistent with distal polyneuropathy. Electromyography revealed widespread demyelinating peripheral neuropathy with considerable axonal loss suggestive of chronic inflammatory demyelinating polyneuropathy (CIDP). This diagnosis was further supported by lumbar puncture, which demonstrated albuminocytologic dissociation (cerebrospinal fluid revealed 2 WBC/mcL (94% lymphocytes), 1 RBC/mcL, glucose of 53 mg/dL, elevated protein (83 mg/dL) and negative gram stain and culture). Two months prior to admission, she developed lower back pain with disequilibrium and difficulty ambulating. MRI of the lumbar spine showed diffuse abnormal heterogeneous bone marrow signal, retroperitoneal lymphadenopathy and symmetric extradural peripheral nerve enlargement (figure 1). Over the next several weeks, she developed dyspnoea on exertion, orthopnoea and progressively worsening lower extremity swelling, prompting hospitalisation for further evaluation and planned intravenous immunoglobulin (IVIG) therapy for presumed CIDP. On admission, she endorsed anorexia, early satiety, abdominal fullness and diarrhoea, but denied fevers, chills or night sweats. She denied drug allergies, alcohol, tobacco or illicit drug use. She had no recent foreign travel. On admission, she was afebrile with a heart rate of 90, blood pressure of 187/115 mm Hg, respiratory rate of 16 and oxygen saturation of 100% on room air. Notable physical examination findings included an ill and cachectic appearance with conversational dyspnoea. Ophthalmic examination showed bilateral papilloedema, confirmed with dilated eye examination. Her lower extremities revealed hyperpigmentation and 3+ oedema. Her abdomen was full with non-tender hepatosplenomegaly. Neurological examination revealed 2/5 motor strength with ankle dorsiflexion and plantar flexion and difficulty ambulating.
Figure 1.
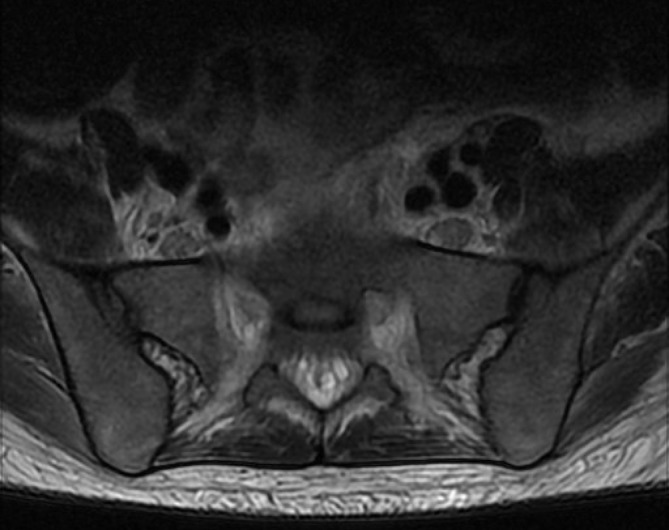
Axial T2-weighted MRI of the lumbar spine demonstrated symmetrical enlargement of the extradural peripheral nerves.
Investigations
Laboratory investigation showed haemoglobin of 11.1 g/dL, white blood cell count of 7.8×103/mm3, platelet count of 460×103/mm3 and pro-brain natriuretic peptide N-terminal level of 6303 pg/mL (5–125 pg/mL). She had normal kidney and liver function. Her esophagogastroduodenoscopy and colonoscopy were normal. Rapid plasma reagin was negative. Small bowel biopsies were negative for celiac disease. Serum protein electrophoresis with immunofixation showed an IgA-lambda monoclonal gammopathy with an M-spike of 0.5 g. Quantitative immunoglobulin levels showed elevated IgA (936 mg/dL) and normal IgG and IgM. Serum kappa and lambda light chain levels and their ratio were 41.3 mg/L, 90.7 mg/L and 0.46, respectively in a polyclonal pattern. Bone marrow biopsy showed 15%–20% lambda light chain restricted plasma cell infiltration without amyloid deposition by Congo red stain. Fat pad biopsy was negative for amyloidosis. Skeletal survey showed no lytic or sclerotic bone lesions. Her adrenocorticotropic hormone was on the upper limit of normal at 61.4 pg/mL (7.2–63.3 pg/mL), prolactin was elevated at 99.7 ng/mL (4.79–23.3 ng/mL) and thyroid-stimulating hormone level was normal. Her initial VEGF level was elevated at 1221 pg/mg (0–115 pg/mL). Abdominal CT showed hepatosplenomegaly, ascites, soft tissue oedema and pleural effusions without sclerotic bone lesions. Repeat TTE showed a reduced ejection fraction of 40%–45%, a moderately dilated left ventricle with mild global hypokinesis and a moderate, circumferential pericardial effusion. Brain MRI revealed diffuse calvarial osteosclerosis (figure 2) and papilloedema without intracranial mass. The patient was diagnosed with POEMS syndrome having met the mandatory diagnostic criteria: polyneuropathy and monoclonal plasmacytosis, elevated VEGF level, and several minor criteria (organomegaly, extravascular volume overload, endocrinopathy, skin changes and papilloedema.
Figure 2.
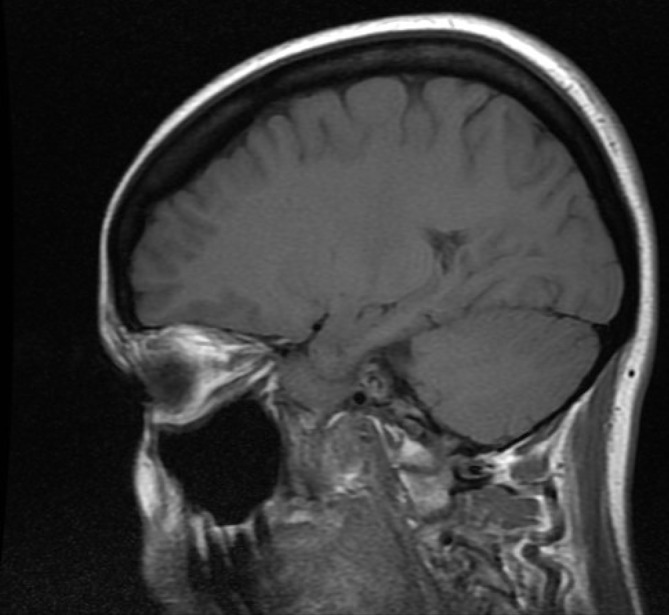
Sagittal T1-weighted MRI of the brain revealed diffusely decreased calvarial bone marrow signal related to osteosclerosis.
Treatment
The patient was treated with all oral therapy consisting of lenalidomide (25 mg daily for 21 of 28 days), prednisone (60 mg/m2 daily for 5 days) and cyclophosphamide (475 mg/m2 daily for 5 days). She was discharged within 3 weeks of starting therapy and except for mild residual neuropathy, all other abnormalities, including elevated VEGF and papilloedema, resolved after 3 cycles of lenalidomide based treatment. The initial dose of lenalidomide was reduced from initial 25 mg to 10 mg due to neutropaenia. A repeat CT scan of the abdomen and pelvis showed resolution of hepatosplenomegaly. The patient underwent successful autologous stem cell harvest followed by high-dose melphalan 140 mg/m2 and reinfusion of 4.8×106 CD34+ cells/kg.
Neutrophil and platelet engraftment was achieved on post-transplant (reinfusion) day 10 and 16, respectfully. Her difficulty walking prompted us to add monthly IVIG to improve foot drop and gait recovery. She was completely free of all presenting symptoms 3 months post-transplant.
Outcome and follow-up
She remains in clinical and serological remission 25 months after transplant. Her cardiac ejection fraction improved (43%) on TTE. Pulmonary function testing revealed a moderate (40%–59% predicted) reduction in Diffusing capacity of the Lungs for Carbon Monoxide (DLCO).
Discussion
POEMS syndrome is a rare, multiple organ systems paraneoplastic syndrome that is difficult to diagnose due to its insidious onset and the variability of its clinical manifestations. This case report demonstrates the diagnostic pitfalls and delay with the attendant severe morbidity that can arise with this disease. More importantly, we demonstrate successful therapeutic rescue of a severe case with triple therapy of lenalidomide, cyclophosphamide and followed by peripheral blood stem cell transplantation (PBSCT).
Our patient was diagnosed more than 2 years after the initial symptomatology of progressive symmetric bilateral lower extremity weakness and paraesthesia leading to a nearly bed-bound state. Established diagnostic criteria (table 1) are not all required for diagnosis. Furthermore, POEMS may be associated and present with initial symptoms of thrombotic microangiopathy, Waldenstrom’s macroglobulinemia, chronic kidney disease, Castleman disease and ischaemic stroke.2–6
Table 1.
Diagnostic criteria for POEMS (adapted from Dispenzieri 2015)1
| Major criteria |
|
| Minor criteria |
|
| Other signs and symptoms |
|
*Mandatory.
POEMS, polyneuropathy, organomegaly, endocrinopathy, monoclonal gammopathy and skin changes.
Plasma cells are implicated in POEMS syndrome, multiple myeloma and monoclonal gammopathy of unknown significance but overall, the pathophysiology of POEMS syndrome remains poorly understood.7 Polyneuropathy, mixed demyelination and axonal loss (as seen in our patient) are prominent clinical features of both POEMS syndrome and CIDP. This challenge in distinguishing between POEMS syndrome and CIDP often leads to diagnostic delays.8 9 Progressive demyelination from early to late disease seen with POEMS syndrome contributes to misdiagnosis as CIDP.10 Interestingly, pachymeningeal disease has also been reported in patients with POEMS syndrome.11 Our patient had an abnormal nerve conduction study, cranial MRI that showed papilloedema without pachymeningitis and spine MRI that revealed enlargement of the extradural peripheral nerves: all indicative of POEMS syndrome. Papilloedema decreased DLCO and depressed cardiac ejection fraction as seen in this patient are associated with poor outcomes.12 Serum VEGF levels, often used to monitor disease activity, may be a predictive biomarker for disease activity and prognosis.13 Treatment of POEMS syndrome requires both supportive care and specific treatments targeting underlying pathological plasma cells. No randomised controlled trials have established the best treatment for POEMS syndrome and approaches to therapy are mostly extrapolated from multiple myeloma and amyloidosis literature. Treatment usually includes upfront radiation therapy for sclerotic bone lesions-only disease or systemic therapy extraosseous manifestation. As with other plasma cell dyscrasias, treatment has rapidly evolved from previous reliance on alkylators and corticosteroids to current immunomodulatory agents and proteasome inhibitors. Early attempt to use bevacizumab, an anti-VEGF monoclonal antibody, based on the pathognomonic expression of VEGF in POEMS syndrome showed mixed results.14 Lenalidomide, more so than its older analogue thalidomide, and associated with increased neuropathy, has been used in the upfront and relapsed/refractory setting.15–18 Nozza and colleagues reported a high rate of clinical and neurological improvement in their small prospective, open-label pilot study of 18 new and relapsed/refractory patients with POEMS treated with lenalidomide 25 mg daily and dexamethasone 40 mg weekly for 21 days of 4 weeks cycles.17 Of the 18 patients who completed 6 cycles of this regimen, 72% responded but only 50% had both clinical and neurological improvement. Additional treatment options are therefore needed and both and proteasome inhibitors, such as bortezomib in combination with dexamethasone or addition of alkylating agents such as cyclophosphamide are been explored. Despite upfront autologous PBSCT in POEMS syndrome, relapse remains common. The European Society for Blood & Marrow Transplantation recently published their 13 years’ experience in 127 patients with POEMS syndrome who underwent transplant.19 The median age was 50 years (range 26–69 years) and the median time from diagnosis to autologous PBSCT was 7.5 months. Complete, partial and less than partial haematological response was achieved in 48.5%, 20.8% and 30.7%, respectively. With a median follow-up of 48 months (95% CI 38.3 to 58.6), 90% of patients are alive and 16.5% of patients have progressed. The 1-year transplant-related mortality was 3.3% and the 5-year probabilities of progression-free survival and overall survival of 74% and 89%, respectively. The incomplete clinical and neurological resolution, the complete remission rate less than 50% with lenalidomide and dexamethasone and with PBSCT warrants the consideration for triple induction therapy approach. Lenalidomide, cyclophosphamide and corticosteroids followed by autologous transplant as was used in this patient is one such option. We also used concurrent IVIG because of the severity of her motor disability but cannot specifically isolate its clinical benefit. Our patient with severe debilitation at onset of treatment achieved complete remission using this approach and has remained in remission for over 2 years.
Learning points.
Polyneuropathy, organomegaly, endocrinopathy, monoclonal gammopathy and skin changes (POEMS) syndrome is a rare and treatable disease, even in patients with severe disability.
A high index of suspicion, thorough history and physical examination followed by appropriate testing including vascular endothelial growth factor level measurement and a bone marrow biopsy are necessary.
Optimal treatment remains elusive, and despite an impressive response rate using dual therapy of lenalidomide and dexamethasone with or without peripheral blood stem cell transplantation, complete remission rate and neurological response remain less than 50%.
Triple induction therapy with lenalidomide, cyclophosphamide and prednisone or dexamethasone followed transplantation, as was used in our patient with delayed diagnosis and severe neurological morbidity, should be explored prospectively.
Footnotes
Contributors: SO: interviewing and caring for the patient, performing chart review and writing the manuscript. LG, SW: interviewing and caring for the patient, assisting with manuscript revision.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Dispenzieri A. POEMS syndrome: update on diagnosis, risk-stratification, and management. Am J Hematol 2015;90:951–62. 10.1002/ajh.24171 [DOI] [PubMed] [Google Scholar]
- 2.Kawano Y, Nakama T, Hata H, et al. Successful treatment with rituximab and thalidomide of POEMS syndrome associated with Waldenstrom macroglobulinemia. J Neurol Sci 2010;297:101–4. 10.1016/j.jns.2010.06.023 [DOI] [PubMed] [Google Scholar]
- 3.Ravindran A, Go RS, Fervenza FC, et al. Thrombotic microangiopathy associated with monoclonal gammopathy. Kidney Int 2017;91:691–8. 10.1016/j.kint.2016.09.045 [DOI] [PubMed] [Google Scholar]
- 4.Liang M, Jiang Z, Lin Z, et al. Polyneuropathy as Novel Initial Manifestation in a Case of "Nonsecretory" POEMS Syndrome with Sjögren’s Syndrome. Case Rep Med 2017;2017:1–6. 10.1155/2017/1276759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Naddaf E, Dispenzieri A, Mandrekar J, et al. Clinical spectrum of Castleman disease-associated neuropathy. Neurology 2016;87:2457–62. 10.1212/WNL.0000000000003405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yaghi S, Elkind MSV. Paraneoplastic Progressive Vasculopathy as the Presenting Manifestation of Polyneuropathy, Organomegaly, Endocrinopathy or Edema, M-Spike, and Skin Manifestations: A Case Report. J Stroke Cerebrovasc Dis 2016;25:e103–e107. 10.1016/j.jstrokecerebrovasdis.2016.03.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yuhei N, et al. Distinctive Genetic Features of Plasma Cells in POEMS Syndrome. Blood 2016;128:4404. [Google Scholar]
- 8.Misawa S. [Electrophysiologic aspects of Crow-Fukase (POEMS) syndrome--significance in early diagnosis and insights into the pathophysiology]. Brain Nerve 2008;60:595–601. [PubMed] [Google Scholar]
- 9.Liu M, Zou Z, Guan Y, et al. Motor nerve conduction study and muscle strength in newly diagnosed POEMS syndrome. Muscle Nerve 2015;51:19–23. 10.1002/mus.24267 [DOI] [PubMed] [Google Scholar]
- 10.Piccione EA, Engelstad J, Dyck PJ, et al. Nerve pathologic features differentiate POEMS syndrome from CIDP. Acta Neuropathol Commun 2016;4:116 10.1186/s40478-016-0389-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Briani C, Fedrigo M, Manara R, et al. Pachymeningeal involvement in POEMS syndrome: MRI and histopathological study. J Neurol Neurosurg Psychiatry 2012;83:33–7. 10.1136/jnnp-2011-300047 [DOI] [PubMed] [Google Scholar]
- 12.Cui R, Yu S, Huang X, et al. Papilloedema is an independent prognostic factor for POEMS syndrome. J Neurol 2014;261:60–5. 10.1007/s00415-013-7143-4 [DOI] [PubMed] [Google Scholar]
- 13.Misawa S, Sato Y, Katayama K, et al. Vascular endothelial growth factor as a predictive marker for POEMS syndrome treatment response: retrospective cohort study. BMJ Open 2015;5:e009157 10.1136/bmjopen-2015-009157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sekiguchi Y, Misawa S, Shibuya K, et al. Ambiguous effects of anti-VEGF monoclonal antibody (bevacizumab) for POEMS syndrome. J Neurol Neurosurg Psychiatry 2013;84:1346–8. 10.1136/jnnp-2012-304874 [DOI] [PubMed] [Google Scholar]
- 15.Zagouri F, Kastritis E, Gavriatopoulou M, et al. Lenalidomide in patients with POEMS syndrome: a systematic review and pooled analysis. Leuk Lymphoma 2014;55:2018–23. 10.3109/10428194.2013.869329 [DOI] [PubMed] [Google Scholar]
- 16.Royer B, Merlusca L, Abraham J, et al. Efficacy of lenalidomide in POEMS syndrome: a retrospective study of 20 patients. Am J Hematol 2013;88:207–12. 10.1002/ajh.23374 [DOI] [PubMed] [Google Scholar]
- 17.Nozza A, Terenghi F, Gallia F, et al. Lenalidomide and dexamethasone in patients with POEMS syndrome: results of a prospective, open-label trial. Br J Haematol 2017;179:748–55. 10.1111/bjh.14966 [DOI] [PubMed] [Google Scholar]
- 18.Misawa S, Sato Y, Katayama K, et al. Safety and efficacy of thalidomide in patients with POEMS syndrome: a multicentre, randomised, double-blind, placebo-controlled trial. Lancet Neurol 2016;15:1129–37. 10.1016/S1474-4422(16)30157-0 [DOI] [PubMed] [Google Scholar]
- 19.Cook G, Iacobelli S, van Biezen A, et al. High-dose therapy and autologous stem cell transplantation in patients with POEMS syndrome: a retrospective study of the Plasma Cell Disorder sub-committee of the Chronic Malignancy Working Party of the European Society for Blood & Marrow Transplantation. Haematologica 2017;102:160–7. 10.3324/haematol.2016.148460 [DOI] [PMC free article] [PubMed] [Google Scholar]


