Abstract
In 2001, the World Health Organization (WHO) established a public–private partnership to fight human African trypanosomiasis (HAT). As a result of this continuous collaboration, and in addition to the coordination with nongovernmental organizations and bilateral cooperation agencies, the number of new cases of HAT annually reported by the WHO has strikingly decreased. In 2012, HAT was included in WHO’s roadmap on neglected tropical diseases with a 2020 target date for elimination. Although the prevalence of HAT is decreasing and its elimination is targeted, control approaches must be adapted to the different epidemiological patterns in order to adopt the most adequate strategies to maintain their cost-effectiveness. These strategies must be flexible and dynamic in order to be adapted to the disease progression, as well as to the changes affecting the existing health facilities in transmission areas, including their accessibility, their capabilities, and their involvement in the elimination process. Considering the different patterns of transmission (Trypanosoma brucei (T.b.) rhodesiense HAT) and transmission intensity (T.b. gambiense HAT), different settings have been defined. In the case of T.b. rhodesiense, this form exists primarily where wild animals are the main parasite reservoir, and where the main parasite reservoir is cattle. In T.b. gambiense, this form exists in areas with high intensity transmission, areas with moderate intensity transmission, and areas with low intensity transmission. Criteria and indicators must be established to monitor and evaluate the actions implemented toward the elimination of HAT.
Keywords: human African trypanosomiasis, HAT, sleeping sickness, disease elimination, T.b. rhodesiense, T.b. gambiense
Introduction
In 2001, the World Health Organization (WHO) and partners established a public–private partnership to fight human African trypanosomiasis (HAT). Since then, critical challenges have been overcome, mainly in terms of availability of drugs, technical and logistical support to disease endemic countries, harmonization of control procedures, monitoring of screening activities, and coordination with concerned nongovernmental organizations (NGOs) and bilateral cooperation agencies. That has led to both the improvement of epidemiological knowledge,1 and to the 75% decline of new cases that are annually reported to the WHO.2 In 2011, 6631 new cases of Gambiense and 112 new cases of Rhodesiense HAT have been reported for a total number of 6743 new cases (Table 1).
Table 1.
The number of new cases of human African trypanosomiasis (T.b. gambiense and T.b. rhodesiense) reported to the WHO (2001–2011)
| 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| T.b. gambiense | |||||||||||
| Angola | 4577 | 3621 | 3115 | 2280 | 1727 | 1105 | 648 | 517 | 247 | 218 | 154 |
| Benin | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Burkina Faso | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Cameroon | 14 | 32 | 33 | 17 | 3 | 15 | 7 | 13 | 24 | 15 | 15 |
| Chad | 138 | 715 | 222 | 483 | 190 | 276 | 97 | 196 | 510 | 232 | 276 |
| Central African Republic | 718 | 572 | 539 | 738 | 666 | 460 | 654 | 1194 | 1054 | 395 | 132 |
| Congo | 894 | 1005 | 717 | 873 | 398 | 300 | 189 | 182 | 87 | 87 | 61 |
| Côte d’Ivoire | 92 | 97 | 68 | 74 | 42 | 29 | 13 | 14 | 8 | 8 | 10 |
| Democratic Republic of Congo | 17,322 | 13,853 | 11,481 | 10,369 | 10,269 | 8023 | 8162 | 7326 | 7183 | 5629 | 5595 |
| Equatorial Guinea | 17 | 32 | 23 | 22 | 17 | 13 | 15 | 11 | 7 | 8 | 1 |
| Gabon | 30 | 26 | 26 | 49 | 53 | 31 | 30 | 24 | 14 | 22 | 17 |
| Gambia | – | – | – | – | – | – | – | – | – | – | – |
| Ghana | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Guinea | 72 | 132 | 130 | 95 | 94 | 48 | 69 | 90 | 79 | 68 | 57 |
| Guinea Bissau | – | – | – | – | – | – | – | – | – | – | – |
| Liberia | – | – | – | – | – | – | – | – | – | – | – |
| Mali | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Niger | – | – | – | – | – | – | – | – | – | – | – |
| Nigeria | 14 | 26 | 31 | 10 | 21 | 3 | 0 | 0 | 0 | 2 | 3 |
| Senegal | – | – | – | – | – | – | – | – | – | – | – |
| Sierra Leone | – | – | – | – | – | – | – | – | – | 0 | – |
| South Sudana | 1919 | 3121 | 3061 | 1742 | 1853 | 789 | 469 | 623 | 373 | 200 | 266 |
| Togo | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Uganda | 310 | 604 | 517 | 378 | 311 | 290 | 120 | 198 | 99 | 100 | 44 |
| Total reported | 26,117 | 23,836 | 19,963 | 17,130 | 15,644 | 11,382 | 10,473 | 10,388 | 9685 | 6984 | 6631 |
| T.b. rhodesiense | |||||||||||
| Botswana | – | – | – | – | – | – | – | – | – | – | – |
| Burundi | – | – | – | – | – | – | – | – | – | – | – |
| Ethiopia | – | – | – | – | – | – | – | – | – | – | – |
| Kenya | 10 | 11 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 |
| Malawi | 38 | 43 | 70 | 48 | 41 | 58 | 50 | 49 | 39 | 29 | 22 |
| Mozambique | – | 1 | – | 1 | – | – | – | – | – | – | – |
| Namibia | – | – | – | – | – | – | – | – | – | – | – |
| Rwanda | – | – | – | – | – | – | – | – | – | – | – |
| Swaziland | – | – | – | – | – | – | – | – | – | – | – |
| United Republic of Tanzania | 277 | 228 | 113 | 159 | 186 | 127 | 126 | 59 | 14 | 4 | 1 |
| Uganda | 426 | 329 | 338 | 335 | 473 | 261 | 119 | 138 | 129 | 112 | 82 |
| Zambia | 4 | 5 | 15 | 9 | 7 | 6 | 10 | 13 | 4 | 8 | 3 |
| Zimbabwe | – | – | – | – | 3 | – | – | 0 | 3 | 2 | 4 |
| Total reported | 755 | 617 | 536 | 552 | 710 | 453 | 305 | 259 | 190 | 155 | 112 |
| Total T.b. gambiense and T.b. rhodesiense | |||||||||||
| Total reported | 26,872 | 24,453 | 20,499 | 17,682 | 16,354 | 11,835 | 10,778 | 10,647 | 9875 | 7139 | 6743 |
Note:
Data for South Sudan in 2009 include a small revision (three fewer cases) of previously published figures due to a reassessment of the epidemiological data.
Abbreviation: T.b., Trypanosoma brucei.
Representatives from disease-endemic countries gathered in Geneva in May 2007, having noted the general trend in the reduction of new reported cases of HAT associated with improved surveillance system and the extended coverage of control activities; these representatives concluded that HAT could be eliminated as a public health problem.3
In 2011, the elimination of HAT was considered by the WHO Strategic and Technical Advisory Group on Neglected Tropical Diseases as a feasible goal, and this was included in WHO’s roadmap on neglected tropical diseases with a 2020 target date for its elimination as a public health problem.4
In 2012, different partners including major pharmaceutical companies, the World Bank, research institutes, charitable organizations, and government development agencies of the United Kingdom and the United States of America announced the implementation of collaborative measures that were included in the London Declaration on Neglected Tropical Diseases to support the objectives and to accelerate the achievements of the WHO’s roadmap.5
Findings
The generic term, “HAT,” covers the different epidemiological situations associated with the two different forms of the disease. Control approaches need to be defined in a clear and orderly fashion in order to adopt the most adequate strategies for the control and elimination of the disease.
In the foci where T.b. rhodesiense prevails, two different scenarios are considered:
Transmission areas where wild animals, mainly kept in natural protected areas, are the main parasite reservoir. In these areas, people most at risk are those living within or around national parks and game reserves where the risk of HAT exposure is related to the movement of animals and tsetse flies arise out of reserves, especially during particular seasons of the year. Also at risk are individuals who move into the protected areas mainly for collecting firewood or honey, and for fishing or poaching. Tourists and people involved in wildlife conservation or hunting activities (eg, rangers, guides, and so on) are also considered to be at risk.6 These areas where Rhodesiense HAT transmission occurs can be found around natural protected areas in southwestern Uganda, western and northern Tanzania, southern Kenya, Zambia, Malawi, and northern Zimbabwe.
Transmission areas where the main parasite reservoir is cattle are also at risk. Cattle often graze around villages and farming areas. Moreover, they are frequently kept in villages during the night. Occasionally, they are moved to local markets for trading. Thus, people at risk of contracting HAT in these areas are mainly cattle keepers, although all villagers are also exposed to a certain level of risk.7 We found these areas of Rhodesiense HAT transmission patterns in southeastern Uganda and western Kenya. In some areas, livestock and wildlife coexist, and a mixed transmission pattern is observed (eg, in western Tanzania).
A subacute clinical form of Rhodesiense HAT has been described in Zambia and Malawi,8,9 which could hint toward the role of human beings as a potential reservoir, thus humans may be involved in the transmission of the disease. In this case, active case finding could be considered in the control of this disease. However, the usual clinical presentation of Rhodesiense HAT is acute, leading the patient to seek heath assistance soon after infection. As a consequence, the most effective approach in tackling Rhodesiense HAT would be the reinforcement of a HAT diagnosis, and enhancing the treatment capabilities of existing health care facilities in transmission areas. This would ensure the rapid identification and treatment of cases, which coupled with vector control, would decrease vector density and subsequently diminish human–vector contact. The treatment of cattle with antitrypanosomal drugs combined with their elective insecticide impregnation has been shown to be effective for Rhodesiense HAT control by reducing the domestic animal reservoir and the vector density.10
Across the areas in which T.b. gambiense prevails, three scenarios are considered. Although some domestic and wild animals have been described as hosting parasites with an enzymatic profile comparable with T.b. gambiense,11,12 it is uncertain whether these animals can host the parasite long enough to play an important role in the transmission of Gambiense HAT.13 Therefore, humans are considered to be the main reservoir of this parasite. Consequently, differences between Gambiense HAT foci are not based on disease transmission patterns but on disease transmission intensity:14
Areas with high intensity transmission. These can be defined as areas where the average annual number of cases reported during the past 10 years is at least one per 1000 inhabitants. These areas are found in Chad (southern region); in the Central African Republic (northwestern and southeastern regions); Equatorial Guinea (southwestern region); Gabon (northwestern region); Congo (central and southern regions); the Democratic Republic of the Congo (in northern, northwestern, central, and eastern parts); Angola (northwest region); South Sudan (southwestern region); and Uganda (northwestern region).
Areas with moderate intensity transmission. These are areas where at least one case per 10,000 inhabitants has been reported yearly during the past 10 years. These areas are mainly found in the regions surrounding previously described high-intensity risk areas and in costal Guinea, Côte d’Ivoire (central region), Nigeria (southwestern region), and Cameroon (southwestern, northwestern, and eastern regions).
Areas with low intensity transmission. These are areas where less than one case per 10,000 inhabitants per annum has been observed during the past 10 years. They include areas around moderate intensity transmission zones, plus a few areas in northwestern and southeastern Guinea, western and southeastern Côte d’Ivoire, southeast Sierra Leone, and central and southeastern Cameroon.
In addition to the progress on the knowledge of Gambiense HAT distribution, there are still some areas that need further investigation, such as known active foci in regions that are characterized by difficult access due to topography or security constraints. Furthermore, foci which have not reported cases in the last decades and that have no effective surveillance system in place need to be assessed. Despite these limitations, the knowledge gap between the true and the reported number of cases has been significantly improved in recent years. An estimated multypling factor of 12 was applied to the knowledge gap in 1995,13 dropping more recently to three.15
Various estimates of the number and distribution of people at risk for both forms of the disease have been provided elsewhere (Figure 1).16 Precise geographical details of disease transmission areas are displayed in a specific atlas.1
Figure 1.
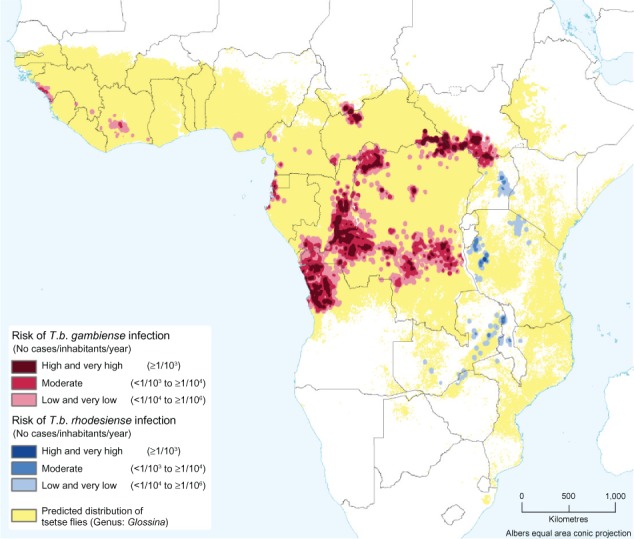
Various estimates of the number and distribution of people at risk for T.b. gambiense and T.b. rhodesiense infection.16
Abbreviation: T.b., Trypanosoma brucei.
To combat Gambiense HAT, it is necessary to appropriately combine the three classical control methods (ie, active case-finding through mobile teams, passive case-finding involving available health facilities, and vector control). The selection of the most appropriate combination and “dosage” of each method has to rely on: (1) the precise understanding of the epidemiological setting, including geographical and demographical data; (2) the accessibility and capabilities of the existing health facilities; and (3) vector knowledge including the sites where vector control must be applied, and methods that have to be utilized.
The sustainability of the control operation will depend upon the cost-effectiveness of the combination implemented. Sustainability also relies on the capacity of control programs to adapt the combination and “dosage” of the methods to the epidemiological evolution of the disease. This would avoid past situations where control and surveillance activities were reduced instead of adapted to the prevailing situation, which led to a dramatic resurgence of cases.17
Considering the remoteness of most foci, the moderate and unspecific clinical signs and symptoms, as well as the lack of efficient health facilities in some foci, it is necessary to continue to maintain mobile teams. However, the frequency of mobile team visits and the localities to be surveyed will vary according to the intensity of the observed disease transmission in each village. In areas with high levels of transmission, mobile teams can perform visits at least once a year to the concerned localities. In areas with moderate levels of transmission, mobile teams can visit villages in the area at least every other year. Areas with low intensity transmission are not considered eligible for regular active screening unless a targeted “reactive screening” is recommended due to the reactivating of a transmission area that was detected during the surveillance process.18 To implement this type of planning, a monitoring and evaluation system backed by an accurate and up-to-date mapping of disease distribution at the village level is required.
The involvement of the health system in HAT control has to be pondered across all stages. Indeed, when a mobile team visits a village, first, it does not examine the entire population, and second, it usually stays 1 day. Therefore, existing health facilities in the area are required to guarantee health care not only during the intervention periods to ensure that actively detected cases will be treated, but also between mobile team visits to ensure that the continuous diagnosis and treatment of cases that are passively detected occur. When the use of mobile teams is not considered to be the most appropriate approach, health facilities have to be able to detect HAT cases among individuals coming to seek health care services. Therefore, regardless of the intensity of transmission, the health care system must be involved in all areas where Gambiense HAT is present; what will vary is the shared responsibility between health services and mobile teams in areas of high and moderate transmission, and the sole responsibility held by health services in areas associated with low transmission rates.
The contribution of vector control to fight Gambiense HAT is basically aimed at reinforcing medical actions that are focused on the reduction of the human reservoir. Therefore, medical teams have to identify areas where diagnostic and treatment activities are not delivering the expected results, leaving human reservoirs untreated and able to maintain the transmission of the disease. This could occur due to very high transmission rates or due to low screening coverage of a given population; it could also occur due to the low sensitivity levels of the serological and parasitological tools used. Actions based on medical approaches could also fail due to healthy human carriers that are either not detected as having the disease, or who refuse treatment.19 Vector control staff members have to identify appropriate tse-tse control methods according to the vector species and the ecological setting. Effective vector control methods involving the community will have more chances of sustainability.
Conclusion
Human African trypanosomiasis is not only a focal disease, but the foci have different patterns of transmission (Rhodesiense HAT) and transmission intensity (Gambiense HAT). When elimination is targeted and the prevalence of the disease is decreasing, control strategies must be adapted to maintain their cost-effectiveness; thus, strategies must be flexible and dynamic enough to be adapted to the disease progression, as well as to the changes affecting the existing local health services, including their level of preparedness and their involvement in the elimination process.
The classical controversy between enthusiasts of “vertical” approaches through mobile teams and those of “horizontal” approaches through primary health care services is losing its relevance since both approaches are complementary and have their specific and synergic roles in the elimination process.
Current control tools are not the most appropriate when designing fine-tuned strategies for each epidemiological setting identified. Continuous research is needed to improve the current weaknesses of the control tools currently used, mainly to engage health services in HAT elimination.
In the process of eliminating HAT, criteria and indicators must be established to monitor and evaluate the actions implemented.
Acknowledgments
The authors would like to thank Giuliano Cecchi and Massimo Paone for their technical support in creating this paper, within the framework of the collaboration between the WHO and the FAO (Food and Agriculture Organization of the United Nations) through the Programme against African Trypanosomosis (PAAT) and Pierre Cattand for the critical reading of the document.
Footnotes
Disclosures
The authors report no conflicts of interest in this work. The boundaries and names shown and the designations used on the maps presented in this paper do not imply the expression of any opinion whatsoever on the part of the WHO concerning the legal status of any country, territory, city, or area, or of its authorities, or concerning the delimitation of its frontiers or boundaries. The views expressed in this paper are those of the authors and do not necessarily reflect the views of the WHO.
References
- 1.Simarro PP, Cecchi G, Paone M, et al. The Atlas of human African trypanosomiasis: a contribution to global mapping of neglected tropical diseases. Int J Health Geogr. 2010;9:57. doi: 10.1186/1476-072X-9-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Simarro PP, Diarra A, Ruiz Postigo JA, Franco JR, Jannin JG. The human African trypanosomiasis control and surveillance programme of the World Health Organization 2000–2009: the way forward. PLoS Negl Trop Dis. 2011;5(2):e1007. doi: 10.1371/journal.pntd.0001007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization . Report of a WHO Informal Consultation on Sustainable Control of Human African Trypanosomiasis. May 1–3, 2007. Geneva, Switzerland: World Health Organization; 2007. [Accessed November 30, 2012]. Available from: http://whqlibdoc.who.int/hq/2007/WHO_CDS_NTD_IDM_2007.6_eng.pdf. [Google Scholar]
- 4.World Health Organization . Accelerating Work to Overcome the Global Impact of Neglected Tropical Diseases. A Roadmap for Implementation. Geneva, Switzerland: World Health Organization; 2012. [Accessed November 30, 2012]. Available from: http://www.who.int/neglected_diseases/NTD_RoadMap_2012_Fullver-sion.pdf. [Google Scholar]
- 5.NTD Partners Uniting to Combat Neglected Tropical Diseases. London Declaration on Neglected Tropical Diseases. [Accessed November 8, 2012]. Available from: http://www.unitingtocombatntds.org/downloads/press/london_declaration_on_ntds.pdf.
- 6.Simarro PP, Franco JR, Cecchi G, et al. Human African trypanosomiasis in non-endemic countries (2000–2010) J Travel Med. 2012;19(1):44–53. doi: 10.1111/j.1708-8305.2011.00576.x. [DOI] [PubMed] [Google Scholar]
- 7.Zoller T, Fèvre EM, Welburn SC, Odiit M, Coleman PG. Analysis of risk factors for T. brucei rhodesiense sleeping sickness within villages in south-east Uganda. BMC Infect Dis. 2008;8:88. doi: 10.1186/1471-2334-8-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Buyst H. The epidemiology, clinical features, and treatment and history of sleeping sickness in the northern edge of the Luangwa fly belt. Med J Zambia. 1974;8:2–12. [Google Scholar]
- 9.MacLean L, Chisi JE, Odiit M, et al. Severity of human African trypanosomiasis in East Africa is associated with geographic location, parasite genotype, and host inflammatory cytokine response profile. Infect Immun. 2004;72(12):7040–7044. doi: 10.1128/IAI.72.12.7040-7044.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kabasa JD. Public-private partnership works to stamp out sleeping sickness in Uganda. Trends Parasitol. 2007;23(5):191–192. doi: 10.1016/j.pt.2007.03.006. [DOI] [PubMed] [Google Scholar]
- 11.Mehlitz D, Zillmann U, Scott CM, Godfrey DG. Epidemiological studies on the animal reservoir of Gambiense sleeping sickness. Part III. Characterization of trypanozoon stocks by isoenzymes and sensitivity to human serum. Tropenmed Parasitol. 1982;33(2):113–118. [PubMed] [Google Scholar]
- 12.Njiokou F, Laveissière C, Simo G, et al. Wild fauna as a probable animal reservoir for Trypanosoma brucei gambiense in Cameroon. Infect Genet Evol. 2006;6(2):147–153. doi: 10.1016/j.meegid.2005.04.003. [DOI] [PubMed] [Google Scholar]
- 13.World Health Organization Control and surveillance of African trypanosomiasis. Report of a WHO Expert Committee. World Health Organ Tech Rep Ser. 1998;881:I–VI. 1–114. [PubMed] [Google Scholar]
- 14.Simarro PP, Cecchi G, Franco JR, et al. Risk for human African trypanosomiasis, Central Africa, 2000–2009. Emerg Infect Dis. 2011;17(12):2322–2324. doi: 10.3201/eid1712.110921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Human African trypanosomiasis (sleeping sickness): epidemiological update. Wkly Epidemiol Rec. 2006;81(8):71–80. Available at: http://www.who.int/wer/2006/wer8108.pdf. [PubMed] [Google Scholar]
- 16.Simarro PP, Cecchi G, Franco JR, et al. Estimating and mapping the population at risk of sleeping sickness. PLoS Negl Trop Dis. 2012;6(10):e1859. doi: 10.1371/journal.pntd.0001859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ruiz-Postigo JA, Franco JR, Lado M, Simarro PP. Human African trypanosomiasis in South Sudan: how can we prevent a new epidemic? PLoS Negl Trop Dis. 2012;6(5):e1541. doi: 10.1371/journal.pntd.0001541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Simarro PP, Franco JR, Ndongo P, Nguema E, Louis FJ, Jannin J. The elimination of Trypanosoma brucei gambiense sleeping sickness in the focus of Luba, Bioko Island, Equatorial Guinea. Trop Med Int Health. 2006;11(5):636–646. doi: 10.1111/j.1365-3156.2006.01624.x. [DOI] [PubMed] [Google Scholar]
- 19.Jamonneau V, Ilboudo H, Kaboré J, et al. Untreated human infections by Trypanosoma brucei gambiense are not 100% fatal. PLoS Negl Trop Dis. 2012;6(6):e1691. doi: 10.1371/journal.pntd.0001691. [DOI] [PMC free article] [PubMed] [Google Scholar]


