Abstract
Background and aims
Nonalcoholic fatty liver disease is one of the major complications of obesity, occurring already in pediatric age. Insulin like growth factor-I has been proposed as a potential therapeutic agent for its beneficial effect in experimental liver fibrosis. The aim of this work was to investigate the expression of insulin-like growth factor-I and its receptor in the liver of children with biopsy-proven nonalcoholic fatty liver disease and relate it to liver histological features.
Methods
45 obese children and adolescents (14 females and 31 males) with nonalcoholic fatty liver disease were included. Insulin like growth factor-I and its receptor expression was evaluated in liver tissue by immunofluorescence and qPCR.
Results
The expression of insulin like growth factor-I and its receptor were significantly related to fibrosis and were higher in children with stage 3 fibrosis compared to stage 1 and 2 (p<0.001 and p = 0.007 respectively). mRNA of insulin like growth factor-I receptor was higher in more advanced stages of fibrosis (p<0.001). Furthermore, the expression of insulin like growth factor-I and its receptor in hepatic stellate cells, the cell type mostly involved in fibrosis progression, was significantly increased in stage 3 fibrosis compared to stage 1 (p = 0.01 and p = 0.008 respectively).
Conclusions
We demonstrated for the first time that insulin like growth factor-I and its receptor are upregulated in children with nonalcoholic fatty liver disease. These findings give a new hint for the potential therapeutic use of insulin like growth factor-I in pediatric nonalcoholic fatty liver disease complicated by liver fibrosis.
Introduction
Nonalcoholic fatty liver disease (NAFLD) is one of the major co-morbidities associated with the obesity [1]. The term encompasses a spectrum of hepatic conditions ranging from simple steatosis to nonalcoholic steatohepatitis (NASH), fibrosis and possible progression into cirrhosis and hepatocellular carcinoma [2]. Prevalence of NAFLD has greatly increased during the last decades in both children and adults with an obese phenotype [3, 4].
The pathogenesis of NAFLD is characterized by two main phases [5]: the intra-hepatic lipid accumulation that could be driven by insulin resistance and lipotoxicity [6]; the development of NASH and fibrogenesis that depends on several mechanisms including adipocytokine imbalance, oxidative stress and gut dysbiosis-mediated endotoxemia [7, 8].
The activation of hepatic stellate cells (HSCs) plays a key role in fibrogenesis, the process that lead to fibrosis. HSCs are pericytes-like cells situated in contact with both endothelial cells and hepatocytes in the perisinusoidal space. Upon stimulation by inflammatory molecules, these cells activate into myofibroblasts that express α-smooth muscle actin (α-SMA) as hallmark [9]. Activated HSCs acquire a pro-inflammatory and fibrogenic phenotype and are able to migrate to the sites of liver injury where they produce large amounts of extracellular matrix molecules, such as collagen, and induce liver fibrosis [9]. In pediatric populations, where up to approximately 80% of obese individuals are affected by NAFLD, fibrosis is a histologic trait of disease, even if the advanced stage of fibrosis and cirrhosis rarely occur [10, 11].
There are no pharmacological treatments currently licensed for NAFLD and the weight loss via lifestyle interventions remains the mainstay of treatment [12]. However, several studies in children with NAFLD demonstrated that even if lifestyle interventions are able to revert steatosis [13–15], they are often ineffective on liver tissue damage, particularly on fibrosis that is currently the major target for designing novel therapies for NASH.
A second major issue in NAFLD is the diagnosis of NASH and fibrosis. To date the gold standard for the diagnosis and staging of NAFLD is liver biopsy that can expose the child to a series of risks [16]. Therefore, the identification of novel potential non-invasive biomarkers of NASH and fibrosis is challenging.
In the last two decades, growth hormone (GH)/insulin-like growth factor-I (IGF-I) axis has been investigated for its putative role in liver diseases. NAFLD prevalence is higher in patients with GH deficiency (GHD) [17, 18] and GH treatment has proven effective in reducing liver fibrosis [18, 19] and reversing NASH [20] in these patients. In vivo models of experimental cirrhosis have contributed to the knowledge from clinical studies, showing that IGF-I acts as anti-inflammatory, anti-oxidant, anti-fibrogenic and hepatoprotective molecule [21–25]. IGF-I does not affect hepatocyte function directly because the hepatocytes express few IGF-I receptor (IGF-IR) in normal condition [26]. On the other hand, the upregulation of IGF-IR in liver during pathologic conditions has been widely reported [27–29]. Moreover, IGF-IR is strongly expressed in activated HSCs and IGF-I-induced cellular senescence in HSCs, in vitro and in vivo [26, 30].
Cross-sectional studies in adult patients have demonstrated an association between circulating levels of GH and IGF-I and NAFLD severity [31–33], leading to speculative hypotheses about a role of these molecules as predictive markers or therapeutic targets in NAFLD. However, studies in pediatric cohorts are limited. We have previously demonstrated a relationship between circulating IGF-I and liver histological stages in a large cohort of obese children with NAFLD, suggesting that IGFs may be markers of liver damage progression in obese children [34].
Little is known about the IGF system status in the liver tissue of obese patients with NAFLD. The aim of the present study was to investigate IGF-I and IGF-I receptor (IGF-IR) expression in the liver of children with biopsy-proven NAFLD and relate it to liver histological features.
Materials and methods
Study population and design
A cohort of 45 Caucasian obese children and adolescents (14 females, 31 males, mean age 12.2 ± 3.0 y) with diagnosis of NAFLD who were referred to the Hepatometabolic Unit of Bambino Gesù Children’s Hospital between January 2012 and July 2014 was included in the study. The study was conducted in accordance to the guidelines of the 1975 Declaration of Helsinki. Written informed consent was obtained from all children and their parents. The experimental protocol and the process for obtaining informed consent were approved by the Institutional Review Board of Bambino Gesù Children's Hospital.
Eligibility criteria included obesity, established using body mass index (BMI) cutoffs of the International Obesity Task Force; absence of underlying diseases and medications that could influence the outcome measures (i.e. GH therapy); all 4 grandparents of Italian descent. Maternal diabetes (either preexisting or developed during or after the index pregnancy) was the sole exclusion criterion. After obtaining informed consent, we performed in-person study visits. At the in-person visit, trained research assistants measured height to the nearest 0.1 cm using a calibrated stadiometer and weight to the nearest 0.1 kg using a calibrated scale. Each child’s BMI was calculated using the following formula: BMI = weight (in kg)/height (in m2). The anthropometric data were compared with national standards. Waist circumference (WC) was measured using a tape measure at just above the uppermost lateral border of the right ilium, at the end of a normal expiration, as described by the National Center of Health Statistics.
Diagnosis of NAFLD and liver histopathology
All children underwent liver biopsy for persistently elevated serum aminotransferase level and/or diffusely hyperechogenic liver on ultrasonography and after exclusion of other common or less common liver diseases, including hepatitis B virus, hepatitis C virus and autoimmune hepatitis, celiac disease, genetic disorders (such as Wilson's disease, alpha-1-antitrypsin deficiency) hemochromatosis, hepatic malignancies and drug-induced liver disease [35].
The clinical indication for biopsy was to assess the presence of NASH and fibrosis or other likely independent or competing liver diseases. Liver biopsy was performed in all children, after an overnight fast, using an automatic core biopsy 18-gauge needle (BioPince; Amedic, Kista, Sweden) under general anesthesia and ultrasound guidance. The length of the liver specimen (in millimeters) was recorded. Only samples that were not fragmented, at least 15 mm long, and included at least 6 complete portal tracts were considered adequate for use in this study. Biopsy specimens were processed routinely (ie, formalin- fixed and paraffin-embedded), and 5-mm-thick liver tissue sections were stained with hematoxylin and eosin, van Gieson, periodic acid-Schiff diastase, and Prussian blue stains. Liver biopsy specimens were evaluated by a single expert pediatric hepatopathologist who established the histopathological diagnosis of NASH. To determine the intraobserver agreement, the pathologist scored the biopsy specimens twice while blinded and calculated the weighted k coefficients for various histological features. Steatosis, inflammation, hepatocyte ballooning, and fibrosis were scored based on the NAFLD Clinical Research Network criteria [36]. Steatosis was graded on a 4-point scale: grade 0, steatosis involving 66% of hepatocytes. Lobular inflammation also was graded on a 4-point scale: grade 0, no foci; grade 1, 4 foci per 200 x field. Hepatocyte ballooning was graded from 0 to 2: 0, none; 1, few balloon cells; 2, many/prominent balloon cells. The stage of fibrosis was quantified on a 5-point scale: stage 0, no fibrosis; stage 1, perisinusoidal or periportal (1a, mild, zone 3, perisinusoidal; 1b, moderate, zone 3, perisinusoidal; 1c, portal/periportal); stage 2, perisinusoidal and portal/periportal; stage 3, bridging fibrosis; stage 4, cirrhosis. Features of steatosis, lobular inflammation, and hepatocyte ballooning were combined to obtain the NAFLD activity score (NAS). As recommended by the NASH Clinical Research Network, a microscopic diagnosis based on overall injury pattern (eg, steatosis, hepatocyte ballooning, inflammation) as well as the presence of additional lesions (eg, zonality of lesions, portal inflammation, fibrosis) was assigned to each case.
RNA extraction and real-time polymerase chain reaction (RT-PCR)
In formalin-fixed paraffin-embedded (FFPE) tissue collected from 18 out of 45 NAFLD patients we evaluated the mRNA expression levels of IGF-1R by RT-PCR. Purification of total RNA was performed using RNeasy FFPE kit, (Qiagen Valencia, CA 91355, USA) combining for each sample 4 section up to 10 μm. FFPE tissue sections were deparaffinized by xylene and ethanol washes. After evaporation of residual ethanol, sections were incubated at 56ºC for 15 min and then 80°C for 15 min with proteinase K buffer and proteinase K for sample lysis and partial reverses formalin crosslinking. The supernatants were collected in a new micro-centrifuge tube and incubated with DNase Booster buffer and DNase at room temperature for 15 minutes. The last steps of RNA purification were performed using MinElute spin columns according to the manufacturer’s specification.
Total RNA (500 ng for each sample) was converted to cDNA using High-Capacity cDNA Reverse Transcription Kit (Thermo Fisher Scientific—Applied Biosystems, Carlsbad, CA, USA) and used as starting material for gene expression study by real-time PCR assay.
SensiFAST Probe Hi-ROX One-Step kit (Bioline USA Inc., MA, USA), Applied Biosystems Taqman Gene Expression Assay for IGF1R (ID: Hs00609566_m1) and 7500 Fast Real-Time PCR System were employed for gene expression analysis. The house keeping gene 18S (ID: Hs99999901_s1) (Thermo Fisher Scientific—Applied Biosystems, Carlsbad, CA, USA) was used as an endogenous control.
For each sample, the measures were done in triplicate for both IGF1R and 18S. Finally, the mRNA levels were relatively quantified using the ΔΔCT method considering patients with fibrosis of grade as value = 1.
Immunohistochemistry and immunofluorescence
Immunofluorescence was performed on 2 μm-thick sections obtained from formalin-fixed tissue embedded in paraffin. Antigen retrieval was performed with ethylenediaminetetraacetic acid (EDTA) (pH 9) (Dako, Glostrup, Denmark).
Sections were incubated over night at +4°C with anti-human: rabbit polyclonal anti-IGF-I antibody (dilution 1:300; Abcam, Cambridge, UK); rabbit polyclonal anti-IGF-IR antibody (dilution 1:50; Abcam, Cambridge, UK); mouse monoclonal anti-α-SMA antibody (dilution 1:100 Dako, Glostrup, Denmark).
The slides where then revealed with mouse anti-rabbit Alexa Fluor 488 (1:500, Applied Biosystems, Life Technologies, Carlsbad, CA, USA) and goat- anti-mouse Alexa Fluor 555 (1:500, Applied Biosystems, Life Technologies, Carlsbad, CA, USA).
Nuclei were counterstained with 4',6-Diamidino-2-phenylindole dihydrochloride (DAPI) for 5 minutes after extensive washing. Next sections were mounted with PBS/glycerol (1:1) and covered with a coverslip.
The confocal microscopy imaging was performed on Olympus Fluoview FV1000 confocal microscope equipped with FV10-ASW version 2.0 software, using 20× objective. Optical single sections were acquired with a scanning mode format of 1024 × 1024 pixels, sampling speed of 40 μs/pixel, and 12 bits/pixel images. Fluorochromes unmixing was performed by acquisition of automated-sequential collection of multi-channel images, in order to reduce spectral crosstalk between channels.
For quantification of expression were used at least five free area from single section that was used to manually draw the region of interest (ROI). The intensity average of fluorescence was calculated using NIS-Elements BR Analysis.
Statistical analysis
Results are expressed as mean ± SD unless specified otherwise. Correlations were calculated as Spearman correlation coefficients. Fisher Exact test was used to calculate differences between proportions. The continuous variables among groups were compared by ANOVA on ranks test. A P value < 0.05 was considered statistically significant. All analyses were performed using the SigmaStat (v 11.00) package (SPSS, Inc, Chicago, IL, USA).
Results
The expression IGF-I and IGF-IR in liver tissue correlates with fibrosis
The main demographic, anthropometric and biochemical features of the study population are reported in Table 1.
Table 1. Anthropometric, clinical and laboratory variables in study population.
| Parameters | Whole patients (45) |
|---|---|
| Female/Male | 14/31 |
| Age, years (SD) | 12.19 (3.05) |
| Weight, kg (SD) | 68.13 (20.82) |
| BMI, Kg/m2 (SD) | 28.33 (5.96) |
| WC, cm (SD) | 86.59 (12.16) |
| AST, UI/L (SD) | 35.45 (18.76) |
| ALT, UI/L (SD) | 51.50 (43.92) |
| GGT, UI/L (SD) | 22.71 (16.28) |
| Total Cholesterol, mg/dL (SD) | 153.49 (35.02) |
| LDL Cholesterol, mg/dL (SD) | 98.16 (31.75) |
| HDL cholesterol, mg/dL (SD) | 43.15 (7.79) |
| Triglycerides, mg/dL (SD) | 119.20 (62.41) |
| Glucose, mg/dL (SD) | 83.07 (10.51) |
| Insulin (SD) | 22.27 (12.78) |
BMI = body mass index; WC = waist circumference; AST = aspartate aminotransferase; ALT = alanine aminotransferase; HDL = high-density lipoprotein cholesterol; LDL = low-density lipoprotein cholesterol.
We analyzed the expression of IGF-I and IGF-IR quantified as intensity per area of liver tissue by immunofluorescence in order to evaluate whether the expression of the two factors correlate with histologic features of NAFLD (i.e. steatosis, lobular inflammation, ballooning and fibrosis) and with NAS. The intra-hepatic expression of IGF-I and IGF-IR significantly correlated with fibrosis (Spearman’s r = 0.355, p = 0.024; Spearman’s r = 0.413, p = 0.0048).
The expression of intra-hepatic IGF-I and IGF-IR increases in parallel with fibrosis progression
Obese children were subdivided according to the degree of fibrosis into three categories: stage 1 fibrosis (16 patients), stage 2 fibrosis (20 patients) and stage 3 fibrosis (9 patients). The main demographic, anthropometric and biochemical features of the study population at different stages of fibrosis are reported in Table 2.
Table 2. Anthropometric, clinical and laboratory variables in patients with different degrees of fibrosis.
| Parameters | Fibrosis 1 (n = 16) |
Fibrosis 2 (n = 20) |
Fibrosis 3 (n = 9) |
P |
|---|---|---|---|---|
| Female/Male | 4/12 | 7/13 | 3/6 | 0.802 |
| Age, years (SD) | 12.19 (2.61) | 12.53 (3.35) | 11.44 (3.28) | 0.639 |
| Weight, kg (SD) | 65.96(17.79) | 67.09(18.30) | 73.92(30.33) | 0.646 |
| BMI, SDS (SD) | 1.84 (0.23) | 2.01(0.78) | 2.34(0.97) | 0.199 |
| BMI, Kg/m2 (SD) | 26.51(4.14) | 28.90(6.01) | 30.15(8.03) | 0.305 |
| WC, cm (SD) | 85.61(5.56) | 86.06(10.14) | 89.33(21.90) | 0.770 |
| AST, UI/L (SD) | 29.33(13.01) | 37.10(18.18) | 42.00(26.19) | 0.127 |
| ALT, UI/L (SD) | 41.13(36.40) | 52.35(42.01) | 66.89(58.21) | 0.235 |
| GGT, UI/L (SD) | 17.19(7.98) | 22.25(16.45) | 33.56(22.42) | 0.229 |
| Total Cholesterol, mg/dL (SD) | 157.50(33.74) | 148.20(36.44) | 158.11(36.47) | 0.673 |
| LDL Cholesterol, mg/dL (SD) | 100.86(28.59) | 87.80(36.42) | 117.00(11.62) | 0.092 |
| HDL cholesterol, mg/dL (SD) | 43.36(6.52) | 43.33(8.70) | 42.44(8.31) | 0.956 |
BMI = body mass index; WC = waist circumference; AST = aspartate aminotransferase; ALT = alanine aminotransferase; HDL = high-density lipoprotein cholesterol; LDL = low-density lipoprotein cholesterol.
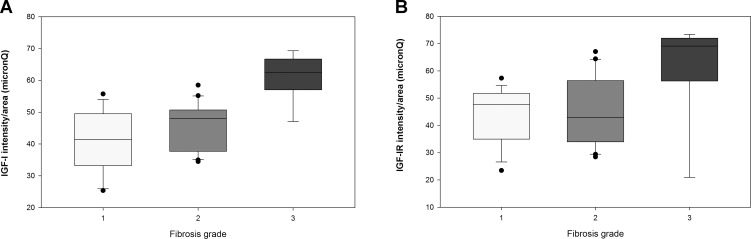
As shown in Fig 1A and 1B and S1 Table and S1 Fig, the expression of IGF-I and IGF-IR quantified as intensity per area of liver tissue was significantly higher in children with stage 3 fibrosis compared to stages 1 and 2 (p < 0.001 and p = 0.007 respectively).
Fig 1.
IGF-I (A) and IGF-IR (B) intensity/area (micronQ) in the different stages of fibrosis. Values are displayed as median and interquartile range (IQR).
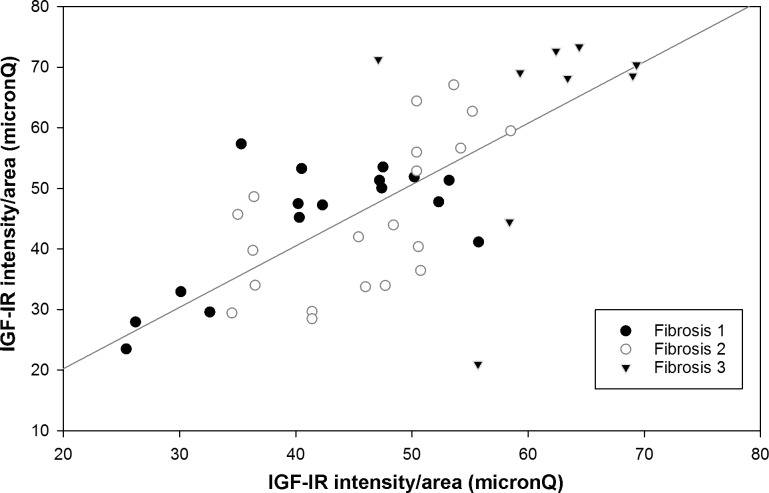
Moreover, the increased expression of IGF-I correlated with the IGF-IR expression in all fibrosis stages (Spearman’s r = 0.61, p < 0.001) (Fig 2).
Fig 2. Correlation between IGF-I and IGF-IR expression, as intensity/area (micronQ) in the different stages of fibrosis.
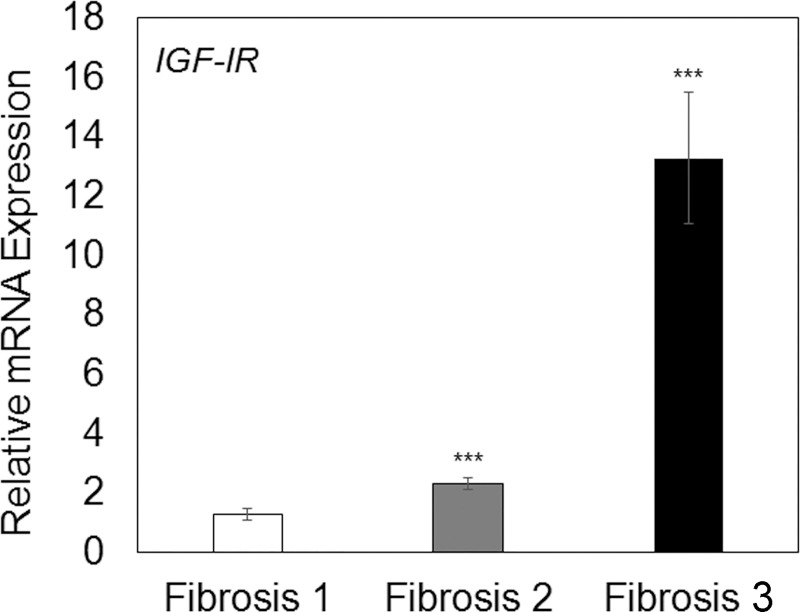
A significant increase of expression IGF-IR mRNA was also found in advanced stage of fibrosis (2 and 3) compared to tissues with stage 1 of fibrosis (p < 0.001) (Fig 3).
Fig 3. Relative mRNA expression of IGF-IR in the different stages of fibrosis.
Data represent mean ± SD. ***P≤0.001 versus fibrosis; unpaired t-test.
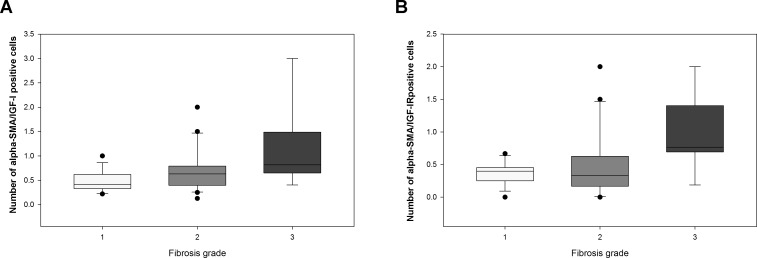
The increased expression of intra-hepatic IGF-I and IGF-IR is mainly associated to activated HSCs
Alpha-SMA expression is a reliable marker of HSCs activation in different type of fibrosis [37, 38]. As expected, the number of activated HSCs had an increasing trend with the progression of fibrosis (S2 Table). After normalization for the total number of HSCs, the number of HSCs expressing IGF-I was significantly increased in patients with stage 3 fibrosis compared to those with stage 1 fibrosis (p = 0.010) (Fig 4A and S2 Table and S2 Fig).
Fig 4.
Number of alpha-SMA positive cells (activated HSCs) expressing IGF-I (A) and IGF-IR (B) in the different stages of fibrosis. Values are displayed as median and interquartile range (IQR).
A significantly higher number of HSCs also expressed IGF-IR in stage 3 fibrosis compared to milder degrees (p = 0.008) (Fig 4B and S2 Table and S2 Fig).
Discussion
Here, we have demonstrated for the first time in a pediatric cohort that liver IGF-I and IGF-IR expression correlates with fibrosis and increases in parallel with fibrosis progression, in the whole liver parenchyma and, more importantly, in activated HSCs, the main cell type involved in fibrogenesis. Fibrogenesis is a complex process of remodeling of liver architecture occurring during wound-healing response to either acute or chronic cellular injury [9]. Liver fibrosis is the result of an imbalance between liver repair and excessive extracellular matrix deposition mainly driven by HSCs [9]. HSC proliferation and their differentiation into collagen-producing myofibroblasts is an important event in the development and progression of liver fibrosis. Some in vitro studies have shown a proliferative and pro-fibrogenic potential of IGF-I on cultured cells, including quiescent HSCs [39]. However, other in vitro data suggest that IGF-I action on HSCs is dependent on their stage of differentiation [26]. On the other hand, the hepatoprotective and antifibrogenic potential of IGF-I has been shown by numerous studies. Sanz et al. [40] showed that targeted over-expression of IGF-I in activated HSCs of transgenic mice accelerates liver regeneration limiting fibrosis. Exogenous administration of IGF-I in experimental liver fibrosis improved liver function [21], reduced oxidative damage [21, 22], provided mitochondrial protection [23] and limited fibrosis [24, 25, 30] in rodent species, suggesting potential clinical applications of IGF-I.
Furthermore, in hepatocytes under normal conditions IGF-IR is present at low levels [41], but its expression is upregulated during pathological conditions, such as chronic hepatitis C and liver cirrhosis [42]. This up-regulation could be a mechanism of cytoprotection by which exogenous IGF-I could exert its well-described positive effects on the liver.
Evidence of a hepatoprotective effect of IGF-I derives also from human studies, showing that growth hormone replacement therapy reverts liver damage in GH deficient patients, for whom NAFLD is an important complication of the disease [18–20]. Moreover, IGF-I has a well-described function in lowering insulin resistance, that plays a pivotal role in the pathogenesis of NAFLD[43] and has been shown to increase albumin levels after 120 days of subcutaneous administration in cirrhotic patients [44].
The observation of increased expression of IGF-I in the liver in the present work is not in contrast with our previous data reporting that serum levels of IGF-I are inversely associated with the severity of NAFLD. Indeed, we found that IGF-I levels increase locally with the progression of fibrosis, suggesting a hepatocellular production/release of IGF-I, as a further attempt to induce a local repair of the damage. Further studies are required to investigate the real role of IGF-I/IGF-IR axis and mechanistic connection with other circulating factors and NAFLD-related damage.
Our work has a few potential limitations. First, we could not include a control group of healthy age-matched individuals in order to exclude the influence of unknown individual-related factors on IGF-I expression in the liver. Second, we did not assess the expression of factors that could confirm a hepatoprotective effect of IGF-I on liver cells and unravel the underlying mechanism, such as molecules involved in oxidative damage (i.e. inducible nitric oxide synthase and myeloperoxidase levels) or hepatocyte growth factor (HGF) that is stimulated by IGF-I [45] and limit fibrosis in vivo by stimulating hepatocyte regeneration [46]. These determinations as well as the assessment of circulating levels of IGF-I in this cohort of patients are perspectives that might build the bases for future studies.
In conclusion, our study is the first to analyze the local expression of IGF-I/IGF-IR in the liver of NAFLD children. We demonstrated for the first time that IGF-I and IGF-IR liver expression is up-regulated in pediatric NAFLD and particularly in HSCs. These findings give a new hint for the potential therapeutic use of IGF-I in pediatric NAFLD complicated by liver fibrosis.
Supporting information
Magnification 20X.
(TIF)
Magnification 20X.
(TIF)
(DOCX)
(DOCX)
(XLSX)
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The authors received no specific funding for this work.
References
- 1.Fabbrini E, Sullivan S, Klein S. Obesity and nonalcoholic fatty liver disease: biochemical, metabolic, and clinical implications. Hepatology. 2010;51(2):679–89. 10.1002/hep.23280 ; PubMed Central PMCID: PMCPMC3575093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yeh MM, Brunt EM. Pathological features of fatty liver disease. Gastroenterology. 2014;147(4):754–64. 10.1053/j.gastro.2014.07.056 . [DOI] [PubMed] [Google Scholar]
- 3.Nobili V, Alisi A, Newton KP, Schwimmer JB. Comparison of the Phenotype and Approach to Pediatric vs Adult Patients With Nonalcoholic Fatty Liver Disease. Gastroenterology. 2016;150(8):1798–810. 10.1053/j.gastro.2016.03.009 ; PubMed Central PMCID: PMCPMC4887388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease-Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64(1):73–84. 10.1002/hep.28431 . [DOI] [PubMed] [Google Scholar]
- 5.Buzzetti E, Pinzani M, Tsochatzis EA. The multiple-hit pathogenesis of non-alcoholic fatty liver disease (NAFLD). Metabolism. 2016;65(8):1038–48. 10.1016/j.metabol.2015.12.012 . [DOI] [PubMed] [Google Scholar]
- 6.Cusi K. Role of obesity and lipotoxicity in the development of nonalcoholic steatohepatitis: pathophysiology and clinical implications. Gastroenterology. 2012;142(4):711–25 e6. 10.1053/j.gastro.2012.02.003 . [DOI] [PubMed] [Google Scholar]
- 7.Moschen AR, Kaser S, Tilg H. Non-alcoholic steatohepatitis: a microbiota-driven disease. Trends Endocrinol Metab. 2013;24(11):537–45. 10.1016/j.tem.2013.05.009 . [DOI] [PubMed] [Google Scholar]
- 8.Schuppan D, Schattenberg JM. Non-alcoholic steatohepatitis: pathogenesis and novel therapeutic approaches. J Gastroenterol Hepatol. 2013;28 Suppl 1:68–76. 10.1111/jgh.12212 . [DOI] [PubMed] [Google Scholar]
- 9.Lee YA, Wallace MC, Friedman SL. Pathobiology of liver fibrosis: a translational success story. Gut. 2015;64(5):830–41. 10.1136/gutjnl-2014-306842 ; PubMed Central PMCID: PMCPMC4477794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nobili V, Svegliati-Baroni G, Alisi A, Miele L, Valenti L, Vajro P. A 360-degree overview of paediatric NAFLD: recent insights. J Hepatol. 2013;58(6):1218–29. 10.1016/j.jhep.2012.12.003 . [DOI] [PubMed] [Google Scholar]
- 11.Feldstein AE, Charatcharoenwitthaya P, Treeprasertsuk S, Benson JT, Enders FB, Angulo P. The natural history of non-alcoholic fatty liver disease in children: a follow-up study for up to 20 years. Gut. 2009;58(11):1538–44. 10.1136/gut.2008.171280 ; PubMed Central PMCID: PMCPMC2792743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.European Association for the Study of the L, European Association for the Study of D, European Association for the Study of O. EASL-EASD-EASO Clinical Practice Guidelines for the management of non-alcoholic fatty liver disease. J Hepatol. 2016;64(6):1388–402. 10.1016/j.jhep.2015.11.004 . [DOI] [PubMed] [Google Scholar]
- 13.Africa JA, Newton KP, Schwimmer JB. Lifestyle Interventions Including Nutrition, Exercise, and Supplements for Nonalcoholic Fatty Liver Disease in Children. Dig Dis Sci. 2016;61(5):1375–86. 10.1007/s10620-016-4126-1 ; PubMed Central PMCID: PMCPMC4848041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Alisi A, Feldstein AE, Villani A, Raponi M, Nobili V. Pediatric nonalcoholic fatty liver disease: a multidisciplinary approach. Nat Rev Gastroenterol Hepatol. 2012;9(3):152–61. 10.1038/nrgastro.2011.273 . [DOI] [PubMed] [Google Scholar]
- 15.Iniguez IR, Yap J, Mager DR. Parental perceptions regarding lifestyle interventions for obese children and adolescents with nonalcoholic fatty liver disease. Paediatr Child Health. 2014;19(5):e24–9. ; PubMed Central PMCID: PMCPMC4029236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kaswala DH, Lai M, Afdhal NH. Fibrosis Assessment in Nonalcoholic Fatty Liver Disease (NAFLD) in 2016. Dig Dis Sci. 2016;61(5):1356–64. 10.1007/s10620-016-4079-4 . [DOI] [PubMed] [Google Scholar]
- 17.Ichikawa T, Hamasaki K, Ishikawa H, Ejima E, Eguchi K, Nakao K. Non-alcoholic steatohepatitis and hepatic steatosis in patients with adult onset growth hormone deficiency. Gut. 2003;52(6):914 ; PubMed Central PMCID: PMCPMC1773673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nishizawa H, Iguchi G, Murawaki A, Fukuoka H, Hayashi Y, Kaji H, et al. Nonalcoholic fatty liver disease in adult hypopituitary patients with GH deficiency and the impact of GH replacement therapy. Eur J Endocrinol. 2012;167(1):67–74. 10.1530/EJE-12-0252 . [DOI] [PubMed] [Google Scholar]
- 19.Matsumoto R, Fukuoka H, Iguchi G, Nishizawa H, Bando H, Suda K, et al. Long-term effects of growth hormone replacement therapy on liver function in adult patients with growth hormone deficiency. Growth Horm IGF Res. 2014;24(5):174–9. 10.1016/j.ghir.2014.07.002 . [DOI] [PubMed] [Google Scholar]
- 20.Takahashi Y, Iida K, Takahashi K, Yoshioka S, Fukuoka H, Takeno R, et al. Growth hormone reverses nonalcoholic steatohepatitis in a patient with adult growth hormone deficiency. Gastroenterology. 2007;132(3):938–43. 10.1053/j.gastro.2006.12.024 . [DOI] [PubMed] [Google Scholar]
- 21.Canturk NZ, Canturk Z, Ozden M, Dalcik H, Yardimoglu M, Tulubas F. Protective effect of IGF-1 on experimental liver cirrhosis-induced common bile duct ligation. Hepatogastroenterology. 2003;50(54):2061–6. . [PubMed] [Google Scholar]
- 22.Garcia-Fernandez M, Castilla-Cortazar I, Diaz-Sanchez M, Navarro I, Puche JE, Castilla A, et al. Antioxidant effects of insulin-like growth factor-I (IGF-I) in rats with advanced liver cirrhosis. BMC Gastroenterol. 2005;5:7 10.1186/1471-230X-5-7 ; PubMed Central PMCID: PMCPMC555751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Perez R, Garcia-Fernandez M, Diaz-Sanchez M, Puche JE, Delgado G, Conchillo M, et al. Mitochondrial protection by low doses of insulin-like growth factor- I in experimental cirrhosis. World J Gastroenterol. 2008;14(17):2731–9. 10.3748/wjg.14.2731 ; PubMed Central PMCID: PMCPMC2709039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Castilla-Cortazar I, Garcia M, Muguerza B, Quiroga J, Perez R, Santidrian S, et al. Hepatoprotective effects of insulin-like growth factor I in rats with carbon tetrachloride-induced cirrhosis. Gastroenterology. 1997;113(5):1682–91. . [DOI] [PubMed] [Google Scholar]
- 25.Muguerza B, Castilla-Cortazar I, Garcia M, Quiroga J, Santidrian S, Prieto J. Antifibrogenic effect in vivo of low doses of insulin-like growth factor-I in cirrhotic rats. Biochim Biophys Acta. 2001;1536(2–3):185–95. . [DOI] [PubMed] [Google Scholar]
- 26.Takahashi Y. The Role of Growth Hormone and Insulin-Like Growth Factor-I in the Liver. Int J Mol Sci. 2017;18(7). 10.3390/ijms18071447 ; PubMed Central PMCID: PMCPMC5535938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kim SO, Park JG, Lee YI. Increased expression of the insulin-like growth factor I (IGF-I) receptor gene in hepatocellular carcinoma cell lines: implications of IGF-I receptor gene activation by hepatitis B virus X gene product. Cancer Res. 1996;56(16):3831–6. . [PubMed] [Google Scholar]
- 28.Stefano JT, Correa-Giannella ML, Ribeiro CM, Alves VA, Massarollo PC, Machado MC, et al. Increased hepatic expression of insulin-like growth factor-I receptor in chronic hepatitis C. World J Gastroenterol. 2006;12(24):3821–8. 10.3748/wjg.v12.i24.3821 ; PubMed Central PMCID: PMCPMC4087928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Aleem E, Nehrbass D, Klimek F, Mayer D, Bannasch P. Upregulation of the insulin receptor and type I insulin-like growth factor receptor are early events in hepatocarcinogenesis. Toxicol Pathol. 2011;39(3):524–43. 10.1177/0192623310396905 . [DOI] [PubMed] [Google Scholar]
- 30.Nishizawa H, Iguchi G, Fukuoka H, Takahashi M, Suda K, Bando H, et al. IGF-I induces senescence of hepatic stellate cells and limits fibrosis in a p53-dependent manner. Sci Rep. 2016;6:34605 10.1038/srep34605 ; PubMed Central PMCID: PMCPMC5056388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dichtel LE, Corey KE, Misdraji J, Bredella MA, Schorr M, Osganian SA, et al. The Association Between IGF-1 Levels and the Histologic Severity of Nonalcoholic Fatty Liver Disease. Clin Transl Gastroenterol. 2017;8(1):e217 10.1038/ctg.2016.72 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hribal ML, Procopio T, Petta S, Sciacqua A, Grimaudo S, Pipitone RM, et al. Insulin-like growth factor-I, inflammatory proteins, and fibrosis in subjects with nonalcoholic fatty liver disease. J Clin Endocrinol Metab. 2013;98(2):E304–8. 10.1210/jc.2012-3290 . [DOI] [PubMed] [Google Scholar]
- 33.Sumida Y, Yonei Y, Tanaka S, Mori K, Kanemasa K, Imai S, et al. Lower levels of insulin-like growth factor-1 standard deviation score are associated with histological severity of non-alcoholic fatty liver disease. Hepatol Res. 2015;45(7):771–81. 10.1111/hepr.12408 . [DOI] [PubMed] [Google Scholar]
- 34.Cianfarani S, Inzaghi E, Alisi A, Germani D, Puglianiello A, Nobili V. Insulin-like growth factor-I and -II levels are associated with the progression of nonalcoholic fatty liver disease in obese children. J Pediatr. 2014;165(1):92–8. 10.1016/j.jpeds.2014.01.052 . [DOI] [PubMed] [Google Scholar]
- 35.Vajro P, Lenta S, Socha P, Dhawan A, McKiernan P, Baumann U, et al. Diagnosis of nonalcoholic fatty liver disease in children and adolescents: position paper of the ESPGHAN Hepatology Committee. J Pediatr Gastroenterol Nutr. 2012;54(5):700–13. 10.1097/MPG.0b013e318252a13f . [DOI] [PubMed] [Google Scholar]
- 36.Kleiner DE, Brunt EM, Van Natta M, Behling C, Contos MJ, Cummings OW, et al. Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology. 2005;41(6):1313–21. 10.1002/hep.20701 . [DOI] [PubMed] [Google Scholar]
- 37.Carpino G, Franchitto A, Morini S, Corradini SG, Merli M, Gaudio E. Activated hepatic stellate cells in liver cirrhosis. A morphologic and morphometrical study. Ital J Anat Embryol. 2004;109(4):225–38. . [PubMed] [Google Scholar]
- 38.Nouchi T, Tanaka Y, Tsukada T, Sato C, Marumo F. Appearance of alpha-smooth-muscle-actin-positive cells in hepatic fibrosis. Liver. 1991;11(2):100–5. . [DOI] [PubMed] [Google Scholar]
- 39.Svegliati-Baroni G, Ridolfi F, Di Sario A, Casini A, Marucci L, Gaggiotti G, et al. Insulin and insulin-like growth factor-1 stimulate proliferation and type I collagen accumulation by human hepatic stellate cells: differential effects on signal transduction pathways. Hepatology. 1999;29(6):1743–51. 10.1002/hep.510290632 . [DOI] [PubMed] [Google Scholar]
- 40.Sanz S, Pucilowska JB, Liu S, Rodriguez-Ortigosa CM, Lund PK, Brenner DA, et al. Expression of insulin-like growth factor I by activated hepatic stellate cells reduces fibrogenesis and enhances regeneration after liver injury. Gut. 2005;54(1):134–41. 10.1136/gut.2003.024505 ; PubMed Central PMCID: PMCPMC1774353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sedlaczek N, Hasilik A, Neuhaus P, Schuppan D, Herbst H. Focal overexpression of insulin-like growth factor 2 by hepatocytes and cholangiocytes in viral liver cirrhosis. Br J Cancer. 2003;88(5):733–9. 10.1038/sj.bjc.6600777 ; PubMed Central PMCID: PMCPMC2376349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Liu W, Li J, Cai Y, Wu Q, Pan Y, Chen Y, et al. Hepatic IGF-1R overexpression combined with the activation of GSK-3beta and FOXO3a in the development of liver cirrhosis. Life Sci. 2016;147:97–102. 10.1016/j.lfs.2016.01.037 . [DOI] [PubMed] [Google Scholar]
- 43.Clemmons DR. Involvement of insulin-like growth factor-I in the control of glucose homeostasis. Curr Opin Pharmacol. 2006;6(6):620–5. 10.1016/j.coph.2006.08.006 . [DOI] [PubMed] [Google Scholar]
- 44.Conchillo M, de Knegt RJ, Payeras M, Quiroga J, Sangro B, Herrero JI, et al. Insulin-like growth factor I (IGF-I) replacement therapy increases albumin concentration in liver cirrhosis: results of a pilot randomized controlled clinical trial. J Hepatol. 2005;43(4):630–6. 10.1016/j.jhep.2005.03.025 . [DOI] [PubMed] [Google Scholar]
- 45.Skrtic S, Wallenius V, Ekberg S, Brenzel A, Gressner AM, Jansson JO. Insulin-like growth factors stimulate expression of hepatocyte growth factor but not transforming growth factor beta1 in cultured hepatic stellate cells. Endocrinology. 1997;138(11):4683–9. 10.1210/endo.138.11.5540 . [DOI] [PubMed] [Google Scholar]
- 46.Matsuda Y, Matsumoto K, Yamada A, Ichida T, Asakura H, Komoriya Y, et al. Preventive and therapeutic effects in rats of hepatocyte growth factor infusion on liver fibrosis/cirrhosis. Hepatology. 1997;26(1):81–9. 10.1053/jhep.1997.v26.pm0009214455 . [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Magnification 20X.
(TIF)
Magnification 20X.
(TIF)
(DOCX)
(DOCX)
(XLSX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.