ABSTRACT
Pregnancy is an ideal time to communicate with women about vaccines for themselves and their infants, yet maternal immunization rates remain suboptimal. This study aimed to identify clinic, provider, and staff-related attributes and facilitators to be utilized for a comprehensive vaccine intervention in ob-gyn clinical settings. We conducted in-depth interviews with 24 providers, both healthcare providers (e.g., physicians, nurse practitioners, midwives) and practice managers, from urban and suburban ob-gyn practices in Georgia and Colorado about their immunization attitudes, practices, and patient experiences. Qualitative analyses included Pearson correlation tests to evaluate patterns and relationships within the data to determine themes. Six major themes emerged: 1) strong provider “buy in” for maternal immunization; 2) the supporting role of clinical/interpersonal cues for vaccine promotion; 3) varying provider-patient communication approaches and its influence on maternal and pediatric uptake; 4) an urgent need for a designated office immunization champion; 5) reimbursement and practice implementation challenges; and 6) region differences in attitudes and values toward maternal immunization. Although providers expressed strong support for maternal immunization practices and offered environmental cues for vaccine promotion, practices often lacked a designated, structured role for an immunization champion equipped to manage delicate conversations with patients. The findings reflect needs for immunization champion identification, training, and support, along with best practices guidelines to improve coordination of vaccine promotion and delivery efforts in ob-gyn provider offices. Additionally, provider training on communication approaches to enhance acceptance and uptake of maternal vaccines is warranted.
KEYWORDS: Maternal Immunization, Influenza Immunization, Ob-gyn Physicians, Attitudes, Vaccine, Pregnant Women, Patient-Provider Communication, Health Communication
Introduction
Immunization during pregnancy is one of the most effective ways to prevent certain infectious diseases among infants and their associated morbidity, mortality, and costs.1 Successes in childhood vaccine uptake have not been equaled in adults, including pregnant women.2 As of November 2016, the most recent coverage rates for maternal influenza immunization (prior to and during pregnancy) was estimated at 46.6% across the United States.3 Similarly, national pertussis immunization rates have also lagged at approximately 49–55% in recent years,4-11 even with issuance of federal and professional organizational antenatal vaccine recommendations.12-14 Pregnant women are at increased risk of serious complications and mortality from influenza.15-18 Young infants are also at risk for severe outcomes stemming from pertussis.9,19-23 Moreover, infants younger than 6 months, for whom there is no licensed influenza vaccine, are one of the highest risk groups for influenza-associated hospitalizations and deaths.24,25
Vaccination during pregnancy protects pregnant women against influenza and pertussis and their infants against these diseases.26-28 With respect to influenza immunization, for example, studies have shown a reduction in influenza-related adverse outcomes such as hospital admissions, mother and infant mortality, and illness severity.29,30 Fetuses acquire antibody protection in utero via maternal immunization, as well as at the post-partum stage (≤ 6 months) wherein antibodies are transferred through breastfeeding; study outcomes reflect greater birth weight among infants of mothers who received maternal immunization, as well as influenza disease protection, and moderately favorable nutritional status difference compared to non-immunized women.31-34 Recent evidence has suggested that vaccine education during pregnancy will boost future uptake of infant vaccines.35 In other words, early exposure to positive immunization messages during pregnancy may make women (and their partners) more likely to vaccinate their infants, as they have received immunization information during a time when they are open to health education.
Therefore, pregnancy is the optimal time to inform women about vaccines for themselves and their infants to increase uptake.36-40 However, obstetric providers often lack the tools to achieve and maintain high coverage of maternal immunization among their patient base as immunization has not historically fallen within the scope of obstetric practice.41,42 As a result, there is a need for more tools and training on effective communication approaches with pregnant patients about maternal and childhood vaccines, especially considering other persuasive influences surrounding women's decision-making during pregnancy.43-49 The barriers for increasing coverage of recommended maternal vaccines and addressing parental concerns for infant v0accines are complex and multifactorial, ranging from systems level barriers (e.g., vaccine supply, inadequate standing orders) to individual provider and patient attitudes.50-55 A comprehensive approach that addresses multiple barriers would be most likely to increase coverage of maternal and infant vaccination rates.53,56
We conducted this study to facilitate the introduction of an effective, comprehensive maternal vaccine promotion strategy in obstetrics and gynecology (ob-gyn) clinical settings. Using established behavioral theories to guide our work (i.e., Elaboration Likelihood Model (ELM), the Stages of Change Model, and the Systems Model of Clinical and Preventive Care), we specifically sought to identify a set of clinic, provider, and staff-related attributes and facilitators that could be utilized for intervention development and implementation.37,57-59
Results
We identified six major themes aligned with a socioecological model that emerged from the data collected from this sample (Figure 1). They include: 1) strong provider “buy in” for maternal immunization; 2) the persuasive role of clinical/interpersonal cues (e.g., posters) in influencing maternal and pediatric uptake; 3) provider-patient communication approaches and its influence on maternal and pediatric uptake; 4) regional differences in attitudes and values toward maternal immunization; 5) reimbursement and practice implementation challenges; and 6) the need for a designated office immunization champion.
Figure 1.
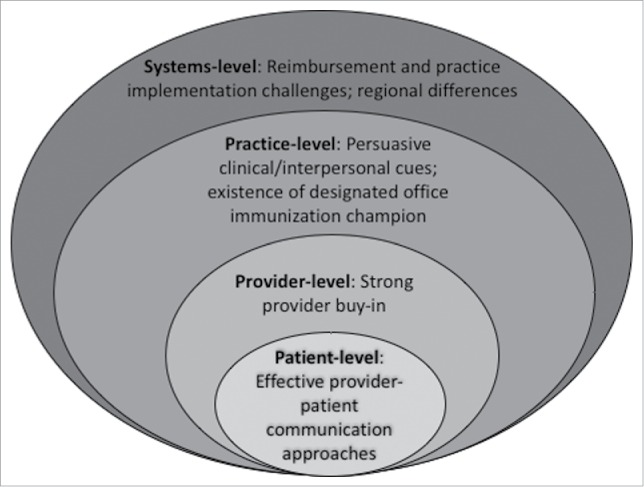
Factors to Improve patient Maternal Immunization through a Socio-Ecological Model.
Strong provider “buy in”
We found strong consensus among providers supporting maternal vaccination. They indicated that vaccine promotion and discussion with patients was a general established practice norm, as opposed to a novel clinical activity. A Georgia provider stated the practice's position:
Yes, it's a consensus. That we promote vaccines to all patients.
In Colorado, the attitude was similar:
We're all very – very pro-vaccine here. Not [a difference of opinion] for any of the providers that I've ever talked to, and we all work – between the midwives and nurse practitioners and the residents – very closely together, and we're all very pro-vaccine in our practices here.
Additionally, most of the providers also indicated that they were informed about current maternal immunization recommendations. One indicated the consistency in their approach:
…we try to make things like this standardized across individuals. We don't put in a lot of leeway for artistry…it comes to following ACOG recommendations and standard of care…
Most of the providers claimed they were knowledgeable about the current recommendations and did their part to ensure that they passed the information along to their patients. Typically, providers stated they offered encouragement to patients to obtain their immunizations and directed them to resources such as brochures, their practice immunization champion if one existed, or a specific website to follow up on their medical advisement if the patient expressed immunization concerns.
Role of clinical/interpersonal cues
The providers in our study described the clinical environment as conducive for promotion of maternal immunization. They discussed aspects such as the physical layout of the clinic and their waiting rooms and the decisional tools contained in these spaces. They also described the role of wait times as opportune for priming immunization decisions with the availability of educational materials on the topic and the allowance of sufficient time for patients and others with them to review and cogitate on the decision. A provider summarized how this setup facilitates the immunization decision:
It helps that we have handouts, and they have time since it gets initiated when they check in, or when they're getting into their room, then they have time while they're waiting on us to read it.
Others added:
I think the most important thing is have the education available to them before they get the vaccine. So, either do it the visit before, with a handout that they can read, so that they know that they're coming in – or doing it that day, if they have some time, they know that in your practice, they generally are waiting 15 minutes before they are seen by their practitioner, that they can review the vaccine protocol, make it easy enough to read, so that they can understand, and give that vaccine that day without any problems.
Since it gets initiated when they check in, or when they're getting into the room, then they have time while they're waiting on us to read it…then they have time to contemplate it, and come up with questions, because if you spring it on them at the end of the visit, they're going to be like, ‘What are you talking about?’
In addition, the providers discussed a need for specific types of education materials that are needed from credible sources and intentional placement of materials such as posters and brochures around the clinic to surround women with reminders to promote immunization. Specifically, they indicated that they had staff place posters and reminders to vaccinate around the waiting room, in the bathrooms, and in treatment rooms. They also highlighted the use of informational pamphlets from the Centers for Disease Control and Prevention (CDC), manufacturers, the American College of Obstetricians and Gynecologists (ACOG) and those designed by the providers themselves as persuasive materials for their patients. In Georgia, a nurse stated that she believed that a pharmaceutical pamphlet was sufficient material for their practice, in addition to the consent form presented to patients:
What we have, along with the consent form, is the information form – that's the flu, and the Tdap, and Gardasil 9…It's a printed off pamphlet, yes.
In Colorado, a provider who had been in the practice for over 4 years described the information they have readily available to women in their waiting room areas and clinical space:
We have at (healthcare entity), kind of a single page information sheet for the patient of what the vaccine is what the – well, and for. Either the Tdap or the flu vaccine: What the disease is that we're trying to prevent, why it's important, um. And specifically for the Tdap, why it's important for them to get vaccinated in pregnancy, because their fetus and/or subsequently their neonate will not be able to mount that immune response, and so it's better for them to get vaccinated now, as well as giving them the information that everyone else in the family also needs to be vaccinated.
In addition to discussion about the materials and placement in clinics, the providers also indicated that immunization information was available on practice websites. However, the availability of designated sections on websites dedicated to this topic was inconsistent across practices. In other words, immunization is not a prominent topic in many of their sites but rather is covered as one of many issues relating to healthy pregnancy. One office manager described how they use their practice website as a tool for patients to view following clinical encounters:
We have a lot of information on our website. I believe that patients do go on there a lot…and when patients call in, the girls out front are really good about sending people to the website for information.
When vaccine-specific information is placed on websites, often it is addressed as a novelty or topical issue as is the case with influenza vaccine. As one participant stated at the end of August (commencement of flu season):
So, on our website, we, you know, monthly push out articles, and so, intermittently that is something that may be addressed, specifically as we get closer to vaccine season. We'll tell people ‘Hey, 'flu season's around the corner…’ This is why you should do it. ‘This is when we expect to have the vaccine available, give us a call and as soon as it's available, we want to accommodate.'
Provider-patient communication approaches
Most of the providers we interviewed discussed that they approach the introduction and promotion of maternal immunizations through one-on-one discussions in clinical encounters. Specifically, they reported discussing immunizations with patients based on what they know the patient values so that they can speak to their issues in a more salient manner. They indicated that this form of messaging is most effective in persuading women to immunize themselves, even if they are reluctant:
I will definitely base the conversation on kind of how they're phrasing their questions and what their questions are. So I try to answer the question, and then may ask a couple questions back to just get a feel for what they already know about vaccinations, or what they already believe about it. And then we'll kind of reframe it based on their system of beliefs.
Have I ever encountered them having questions, or just saying ‘I don't want it’? Yes. And then, by the time they've finished talking to the provider, and he gives references as well, I say nine times out of ten they do go ahead and say yes…some people are misinformed about vaccines, because of what they've heard through the media, negative things through the media. So, what I have heard is ‘Oh, well…”
In addition, we found differences between the states (where the practice is located) and the extent to which women's choice to get vaccinated or not get vaccinated is pursued in clinical encounters. Those in Colorado reported giving women much more time to consider their vaccine decisions (e.g., over the course of several months) and having designated “time out” points when they no longer attempt to persuade women to immunize themselves (e.g., after 3 attempts). A Colorado physician stated:
I mean, we can't – we're not as forceful with clients…it's offered to them at every visit. And in the charts it'll say – we have a section in the chart that'll say, once they've declined three times then we'll stop asking them. But we do offer them up to three times, influenza and Tdap.
Another added:
We have sort of a three time rule. Where you can – you need to offer the vaccine to the patient at least three times – For our pregnant patients, for Tdap and for flu. If they refuse all three times, then you can stop bugging them about it.
In Georgia, we learned that providers also have patients that are reluctant to get immunized during pregnancy; however, none stated that they no longer pursue the decision after certain milestones. A nurse in Georgia offered insight on her practice's approach to the management of patients with immunization concerns:
If they have questions, then we can give them information, or Google if that's not enough, what we have, what we've given them in the office. And they can come back on their next visit, or they can just schedule to come back the next day. Whenever's convenient for them…
Another physician described their strategy with managing and surmounting vaccine hesistance:
I give them all the same information. Uh, we can't force anybody to get a vaccination, we can only educate them to the best of our ability, in our location… They have enough time – we see them, sometimes, every week. Um, they don't have to make a decision on the spot. They can go home, decide, come back at their next appointment and – and obtain the vaccine. So they have ample time.
Regional attitudinal differences toward maternal immunization
The providers in our sample also described differences in patients' beliefs, fears, values and questions on maternal vaccinations. The types of myths and issues they encountered resulted from exposure to others' in their local social networks that promulgate vaccine concerns and fears. These challenges are described as more difficult to surmount in Colorado compared to those in Georgia. A Colorado physician detailed the types of scenarios he has encountered and the need for stronger policies to encourage maternal immunization:
Just the mythology that's out there is the main, real thing I've encountered that's a barrier…sometimes it's just a lack of knowledge, or sometime it's too much phony, pseudo-knowledge about, like, ‘the flu vaccine causes flu’. All the things that you've heard before, vaccines cause autism, that kind of stuff, that you still have to address. And sometimes you're gonna get through to people, and sometimes you're not, but that's kind of a recognized component of our state vaccination epidemiology right [or?] not. So there's all kinds of legislation that has failed trying to kind of shift this balance of people making a lot of statements that aren't evidence based and supported by science.
Another nurse manager in Colorado offered her perspective on the challenges they encounter with persuasive influences shaping vaccine decisions outside of the practice and how the clinical team assists patients in their choices:
I think, um, right now the media obviously plays a huge role in these patients not wanting vaccines. Some people think that vaccines are bad, and some people – you know, it just really depends on their beliefs and their opinions on it. Usually, if I don't – not persuade, but talk them to do it or, you know, tell them the facts, that they really should have it for them and baby – then the doctor usually can. Just because I think they're not informed all the way, they just read what other people say, and they don't really know.
In contrast to the issues described in Colorado, providers in Georgia described the challenges associated with maternal immunization as having more to do with the fear of needles and addressing concerns effectively with those who have limited literacy. They noted that very few patients expressed any reluctance to get immunized with a recommendation:
We get the occasional that say ‘I don't want to do that’, you know, ‘I've read this', you know, or ‘I don't believe in that’, but that's very few and far between that we get that…
Another Georgia provider discussed what she found as the predominant barrier to immunization among the patients in her practice:
Really, it's just more fear, patient fear you know, of getting an injection during pregnancy. They don't usually ask very much…we usually bring it up to them.
In addition, the Georgia practices described the challenges of working with limited English-speaking patients on the topic of maternal immunization. Although they recognize there may be cultural beliefs deterring women from getting a vaccine, often these could be surmounted with clear, understandable dialogue between the provider and the patient. As one provider described, patient beliefs were an issue but the language barriers were a far more considerable challenge to work with effectively:
I would say, I guess, we have a number of international patients, and sometimes the language barrier…we have the language line that we can do, but sometimes it's just not their beliefs.
Another provider in Georgia added that the types of questions asked by patients are often very direct given limited literacy and language barriers with the populations. Thus, being able to directly and succinctly communicate with patients on these points offers them assurance needed that immunizations are more beneficial than harmful to their health and to their baby's health. Such questions posed may include:
Um, 'is it going to hurt the baby?' ‘Do I have to have it?’ ‘Can I wait until after the baby is born?’ ‘If I get it, will the baby be immune?’
Reimbursement and practice implementation challenges
In the context of discussing immunization communication and practice promotion, other issues arose in the context of these conversations including challenges with cost recovery. Providers were recognized for their efforts with maternal immunization, yet managers grappled with the practicality of generating vaccine administration-related revenue:
I think in this area, they're really good. I mean they really are, um, trying to promote them. Um, but that- what we were talking about earlier about cost and everything, I mean, I think that – Mm, helping to make sure that cost wasn't prohibitive would be the big thing, but I – I really think most of the providers, well, I know in this practice, for sure, are all really.
These challenges posed important obstacles that cannot be overlooked in ob-gyn practices attempting to implement immunization guidelines. Managers in particular spoke about the conflicts they faced with providing patients with access to vaccines in the clinic, yet needing proper renumeration for the practice to make their fledgling immunization programs work. This was specifically mentioned as a challenge to implement for Tdap. As one manager reasoned:
I think with the pertussis we have just, kind of, been afraid to spend the money on it versus the reimbursment…it's been the cost prohibitiveness of it. Plus, with those it's – it's very easy to say, ‘go over to Walgreens,’ or, ‘go over to CVS.’
Need for a designated immunization champion
The providers we interviewed offered important perspective what an “immunization champion” meant to them, how prevalent this role was in ob/gyn practices, what tasks were associated with the role, and its value to the practice. Notably, very few of the providers that we interviewed described an actual designation of this role (<30%) in their practice. For those practices that acknowledged having a champion, often this individual was identified as the attending physician; it was not regarded as a discrete role as often designated within pediatric practices. An ob/gyn offered the following statement when asked about who she considered was the “champion” in their practice:
I think (name withheld), my colleague, Dr. “X”, she has – Is a very – She's a big champion of vaccines, and preventative care…
Another nurse stated that in their practice a physician championed a specific vaccine wherein others in the practice may take on the cause of other maternal immunizations. She gave this example:
If it were specifically for the Tdap, I'd say (name withheld) would be that person, because she is the attending who – every patient you sign out to her, she says “Has this person had the Tdap? Yes – great. No – why not? What is her reasoning? What have you counseled her on? What did you tell her?”
According to the providers, the majority indicated that the tasks could be handled by anyone with minimal clinical and/or health training, even considering the challenges associated with functioning in this role for a long period of time. Few described a strategy for identifying the champion, equipping the individual to do an effective job, and retaining the person in this role for a long period of time. When one was asked how a champion would be identified and retained, a Georgia provider stated:
Probably an MA or a nurse. That's just something that falls more within their scope, and they have more access to that. I mean, the providers have so much going on that I don't know that it's something that they could, necessarily…that's just one more thing to add to their plate of having to deliver babies and all that stuff.
Similarly, a Colorado provider noted that they don't specifically have a title for such a role, but he would identify medical assistants responsible for administering the vaccines in this scope of work:
We never have labeled someone that, but pretty much all of the medical assistants have been trained. Like, because we have medical assistants assigned to each provider, so they know what their provider wants, they know how they want it approached they know what to talk to the patients about.
Although the few practices that acknowledged having a champion were ones in which ob/gyns were taking on that role, most offered that this task was not suited for busy, time-constrained providers. As one Georgia nurse stated:
I think they already have so many things – so many roles that they're trying to fulfill. They have a lot on their plate already.
Those that we interviewed also noted a lack of guidance offered to them in selecting, hiring, training, and supporting individuals who take on this role to avoid burnout and a lack of comfort in discussing immunizations with patients who challenge their recommendations. A Georgia provider indicated that their practice currently did not have anyone in such a role, nor was it discussed as a practice priority. Additionally, the selection criteria for an immunization champion was not well defined:
If we could definitely talk about it and find somebody, I think that would be easy to do. I think as long as we're all on the same page that it's ok, I mean, I think it would be more important in an office where they weren't as into the immunizations, and didn't really talk about it with their patients…Probably one of our midlevels, so either midwives or nurse practitioners…Just because they tend to be, definitely, in tune to the patients, and I think they're very encouraging for their staff and the patients to try and have everybody involved…
In the scope of the effort to promote immunizations in their offices, they placed enormous value on having a designated immunization champion. Many expressed that the individual in this role was essential in promoting the messages presented concurrently though clinical cues (i.e., education materials in the waiting and treatment areas) as well as to reinforce the importance of immunization through patient-provider conversations. A Colorado provider stated they have a designated champion who is regarded as an essential team member for practice updates and information dissemination:
I do, yeah. She – she keeps us informed, if there are changes in things we need to know. Like, we just – there's the new HPV-9 vaccine that's coming out, you know, that is available…She sends emails, like to the managers, and then she attends our manager meetings if there's a big change. She makes sure that we're always up to date. We have a daily huddle, my staff. And as far as the providers go… I can give that information to them, and they can disseminate it.
In Georgia another provider added that although they didn't have such a role, the designation of one in the future would be beneficial for immunization promotion:
I think that would be good…Because you could go to him about all your immunization needs. A nurse. 'Cause they would have some clinical knowledge and probably the time to do it. I don't see a physician doing that here. Just as far as timing. Um, and then a practice manager, I don't know that they would have all the clinical knowledge, and all the information.
Discussion
The results from this study offer important insight on contextual, structural, operational, and interpersonal factors broadly aligned with a socioecological model that may be critical in the promotion of maternal immunization (and subsequent pediatric immunization).36 Our study results provide unique information on how to improve communication between the provider and the patient, as well as the practice and the patient, for the purpose of increasing vaccine uptake in ob-gyn setttings. The findings lend to several suggestions for ob-gyn practices on steps they can take to improve vaccine uptake, related to communication materials, interpersonal communication approaches, and the use of immunization champions.
As we expected, those we interviewed expressed their support of the Advisory Committee on Imunization Practices (ACIP) recommendations and ACOG endorsements, thus making them ideally positioned to promote Tdap and influenza immunzations during clinical visits.60,61 However, challenges were mentioned about the provision of vaccines in the course of discussions with practice managers. They cited barriers such as insurance reimbursement, particularly for Tdap vaccine, and especially with known experiences of patient refusal in the practice resulting in unrecouped costs to the practice. These were particularly salient for the relatively newer Tdap vaccine recommendation and given as a reason why one practice did not administer Tdap vaccine on-site and instead referred patients elsewhere.
We also identified the role of “clinical cues” as important in the practice space as playing a critical supporting role in the immunization persuasion process.50,51,62 Providers indicated that the presence of communication materials, such as posters and flyers, were important in creating an environment that conveys the importance of and supports vaccine uptake. Our findings support other studies that speak to the importance of practice materials.63 As materials are widely available from several public health websites, such as the CDC, practices could easily download communication materials to display in their waiting rooms and exam rooms to be used in combination with other immunization interventions. Additionally, as waiting times were seen as an opportune moment to provide educational material, practices should provide vaccine-related information, such as brochures or vaccine information summary sheets, once a patient checks in with the reception team.64 This allows the patient to read through the material before interacting with the provider, thus priming the vaccine-related conversation for the provider.
Providers in our study discussed the importance of interpersonal communication between the provider and patient. We note that this links to the geographic differences observed in the approach providers spoke about in addressing vaccine hesitancy and refusal encountered in their practices. Providers in Colorado were less inclined to challenge women's vaccine refusal after a maximum of three times, placing power back in the hands of the patient citing her “choice.” This contrasted to those in Georgia who did not indicate having such “hard stop” milestones on vaccine discussions.
Several studies indicate the association between effective and ongoing provider communication and patient uptake of vaccines.65,66 When patients have concerns, providers may surmount patient doubts by adopting an empathetic approach, where providers first acknowledge patient concerns, and then ask several follow up questions to assess the patients' concerns. By establishing empathy, providers are allaying patient concerns and fears, which, in turn, can build trust between the patient and provider.67
Those interviewed in our study described their communication approaches with the patient that tend to be more standardized, as opposed to individualized to the needs of the patient. Our study results support other studies that suggest that there is a need for providers to utilize communication materials that are tailored to the patient as this forms a basis for a trusting relationship.68,69 Trust is predictive of several health behaviors, including vaccination.70 For example, patients that have declined vaccines several times may require different persuasive techniques than those that are having an initial conversation with their provider about vaccines. In this same vein, interpersonal communication with patients that have concerns about vaccine safety, for example, should be structured differently from interpersonal communication with patients that have concerns about vaccine effectiveness. Providers should communicate in a way so that patients feel as though their concerns have been addressed, through open questioning and through an agreement between the patient and the provider about the nature of the concern.71 Further, the potential message priming impact that tailored vaccine education has during pregnancy may boost future uptake of infant vaccines.
Providers in our study asserted the importance of a designated immunization champion. Yet, in contrast to pediatric practices that have designated vaccine advocates who are selected and trained according to professional guidelines (i.e., American Academy of Physicians), the role in obstetrical practices is less structured. Others have suggested that every practice should have an immunization champion who is charged with monitoring implementation of immunizations.72 This champion serves a critical role in establishing the norms within a particular practice, and leads the efforts to improve immunization delivery, assists in ensuring that providers are able to resonate with parents on a personal level.68 Previous studies have shown that immunization champions can improve vaccination rates.73,74 as well as standing orders related to vaccination.75 Future research should seek to determine which staff makes the most effective immunization champion and what sort of training is most appropriate.75
As with any qualitative study, social desirability bias is a concern. Due to the qualitative nature of this study, findings are not intended to be representative of all ob-gyn providers, clinicians, and practice managers. While this study poses limitations, it provides an understanding of factors that may contribute to improved integration of practice and communication approaches associated with improved maternal immunization uptake.
The findings from this study offer important direction for provider communication interventions to improve maternal immunization uptake within ob-gyn practices. Specifically, our work highlights the need for designation and training of immunization champions within ob-gyn practices to address the specific concerns of women who may be reluctant to get influenza and pertussis immunizations during pregnancy. The extent and timing of communication with women holding these views may vary according to location and may benefit from tailored strategies. Finally, although providers are supportive of maternal immunization, they may also benefit from guidance on how to recover costs associated with their immunization programs implemented in practice settings.
Materials and methods
Study design and data collection
We conducted in-depth interviews with a convenience sample of healthcare providers (i.e., physicians, nurse practitioners, midwives) and clinic/practice staff (i.e., nurses, medical assistants, practice managers) from selected urban and suburban ob-gyn practices in Georgia and Colorado in 2015. We carefully selected the Georgia and Colorado sites to capture a diversity of provider experience with an array of racial/ethnic patient demographics, reported maternal vaccine attitudes and beliefs, and similar modes of care delivery. In Georgia, 59.8% of the population is white, 31.2% black/African American, and 9.2% Hispanic/Latino. The median age of the State population is 36 years and approximately 51% of the population is female. In Colorado, 84.3% of the population is white, 4.1% black/African American, and 21.1% Hispanic/Latino. The median age is 36 years and approximately 50% of the population is female.76 We have long-standing relationships with 10 practices (5 sites in Georgia; 5 in Colorado) that facilitated study recruitment. Prior to study implementation, we received IRB approval from Emory University.
Participants
Healthcare providers and clinic/practice staff were eligible if they were a current physician, nurse practicioner, midwife, nurse, medical assistant, or practice manager at a participating ob-gyn practice; they were excluded if they were not currently in one of these roles at a participating ob-gyn office/clinic. All persons were ≥ 18 years of age.
Study procedures
Research staff approached the healthcare providers and clinic/practice staff at the designated locations about participating in an interview at approved recruitment times arranged with the clinic coordinator. We sampled providers and clinic/practice staff until we achieved data saturation; our goal was to accrue 27–45 participants for the study. Interviews ranged 30–40 minutes in duration.
Analyses
The data collected from the interviews were transcribed, and subsequently coded and analyzed using NVivo 11.0 qualitative data analysis software (QSR International). Data were team-based analyzed using the constant comparative approach within the grounded theory process model.77 This approach utilizes both deductive and inductive methods to identify patterns or major themes in the data.78 All interview transcripts were coded according to emerging patterns and these codes were further refined through a series of iterative cycles used in team-based qualitative analysis.
Random samples of transcripts (20%) were cross-coded in two cycles to establish the codebook structure and to determine the extent of intercoder agreement on coding and subsequent definitional refinement. Intercoder reliability was ultimately established by comparing the presence or absence of codes in a subsample of text from each interview. Disagreements in coding resulted in subsequent team-based discussions and codebook refinement, followed by additional coding and adjudication when appropriate. In a third cycle, we established overall agreement between coders at 84.3%, suggesting high overall intercoder reliability consistent with good qualitative research practice.79 Finally, we conducted nodal correlation assessment for validation of coding and thematic convergence using Pearson's R measurement across major codes.80 We included those codes that met high correlation coefficient standards (e.g, R ≥ 0.80) to validate the identified code relationships and to summarize thematic findings.81
Funding Statement
Study funding provided by NIH R01AI110482.
Disclosure of potential conflicts of interest
No conflicts of interest for any of the authors except Dr. Daniel Salmon, who received research support and/or consulting funds from Crucell, Pfizer and/or Merck. Dr. Salmon received additional travel funds and honorarium from the National Foundation of Infectious Diseases (NFID).
Acknowledgments
Special thanks to all of our participants and to the following practices for their help and support during our study: My OB/GYN (Riverdale, GA), Women's Center of Athens (Athens, GA), Southern Crescent Women's Health Care (Fayetteville, GA), MCCG Anderson Health Clinic (Macon, GA), Emory University Clinic Midtown (Atlanta, GA), University of Colorado Hospital OB/GYN (Denver, CO), Women's Health Group (Denver and Longmont, CO), Women's Health Care Associates (Denver, CO), and Red Rocks Ob/Gyn (Denver, CO).
References
- 1.Centers for Disease Control and Prevention Ten great public health achievements–United States, 2001–2010. MMWR Morb Mortal Wkly Rep. 2011;60(19):619–23 [PubMed] [Google Scholar]
- 2.National Vaccine Advisory Committee A pathway to leadership for adult immunization: recommendations of the National Vaccine Advisory Committee: Approved by the National Vaccine Advisory Committee on June 14, 2011. Public Health Rep. 2012;127(Suppl 1):1–42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.US Centers for Disease Control and Prevention Pregnant Women and Flu Vaccination, Internet Panel Survey, United States, November 2016. 2017. [cited 2017July28]; Available from: https://www.cdc.gov/flu/fluvaxview/pregnant-women-nov2016.htm [Google Scholar]
- 4.Centers for Disease Control and Prevention Influenza vaccination coverage among pregnant women: 2011–12 influenza season, United States. MMWR Morb Mortal Wkly Rep. 2012;61:758–763 [PubMed] [Google Scholar]
- 5.Ahluwalia IB, Singleton JA, Jamieson DJ, Rasmussen SA, Harrison L. Seasonal influenza vaccine coverage among pregnant women: pregnancy risk assessment monitoring system. J Womens Health. 2011;20(5):649–651. doi: 10.1089/jwh.2011.2794 [DOI] [PubMed] [Google Scholar]
- 6.CDC Influenza Vaccination Coverage Among Pregnant Women — 2011–12 Influenza Season, United States. MMWR Morb Mortal Wkly Rep. 2012;61(38):758–763 [PubMed] [Google Scholar]
- 7.CDC Influenza vaccination coverage among pregnant women – United States, 2012 – 2013 influenza season. Morb Mortal Wkly Recomm Rep. 2013;62(38):787–92 [PMC free article] [PubMed] [Google Scholar]
- 8.CDC Tdap vaccination coverage among U.S. women who were pregnant any time during August 2011 – April 2012, Internet Panel Survey (Unpublished data). 2012 [Google Scholar]
- 9.Kharbanda EO, Vazquez-Benitez G, Lipkind H, Naleway AL, Klein NP, Cheetham TC, Hambidge SJ, Vellozzi C, Nordin JD. Receipt of pertussis vaccine during pregnancy across 7 Vaccine Safety Datalink Sites. Preventive Medicine. 2014;67(0):316–319 [DOI] [PubMed] [Google Scholar]
- 10.Control, C.f.D. and Prevention Influenza vaccination coverage among pregnant women—United States, 2010–11 influenza season. MMWR. Morbidity and mortality weekly report. 2011;60(32):1078. [PubMed] [Google Scholar]
- 11.US Centers for Disease Control and Prevention Pregnant Women and Tdap Vaccination, Internet Panel Survey, United States, April 2016. 2017. [cited 2017July28] ; Available from: https://www.cdc.gov/vaccines/imz-managers/coverage/adultvaxview/tdap-report-2016.html
- 12.Centers for Disease Control and Prevention Prevention and control of influenza with vaccines: recommendations of the Advisory Committee on Immunization Practices (ACIP)–United States, 2012–13 influenza season. MMWR Morb Mortal Wkly Rep. 2012;61(32):613–8 [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention Updated recommendations for use of tetanus toxoid, reduced diphtheria toxoid and acellular pertussis vaccine (Tdap) in pregnant women and persons who have or anticipate having close contact with an infant aged <12 months — Advisory Committee on Immunization Practices (ACIP), 2011. MMWR Morb Mortal Wkly Rep. 2011;60(41):1424–1426 [PubMed] [Google Scholar]
- 14.Centers for Disease Control and Prevention Updated recommendations for use of tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis vaccine (Tdap) in pregnant women–Advisory Committee on Immunization Practices (ACIP), 2012. MMWR. Morbidity and mortality weekly report. 2013;62(7):131. [PMC free article] [PubMed] [Google Scholar]
- 15.Beigi RH, Wiringa AE, Bailey RR, Assi TM, Lee BY. Economic value of seasonal and pandemic influenza vaccination during pregnancy. Clin Infect Dis. 2009;49(12):1784–92. doi: 10.1086/649013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Moro PL, Tepper NK, Grohskopf LA, Vellozzi C, Broder K. Safety of seasonal influenza and influenza A (H1N1) 2009 monovalent vaccines in pregnancy. Expert Rev Vaccines. 2012;11(8):911–21. doi: 10.1586/erv.12.72 [DOI] [PubMed] [Google Scholar]
- 17.Centers for Disease Control and Prevention Maternal and Infant Outcomes Among Severely Ill Pregnant and Postpartum Women with 2009 Pandemic Influenza A (H1N1) — United States, April 2009–August 2010. MMWR Morb Mortal Wkly Rep. 2011;60(35):1193–1196 [PubMed] [Google Scholar]
- 18.Georgia Department of Health Annual Vaccine Preventable Diseases Surveillance Report – Georgia, 2010. 2010October4; Available from: http://health.state.ga.us/pdfs/epi/vpd/2010%20VPD%20Report.pdf
- 19.Centers for Disease Control and Prevention CDC – Pertussis: Outbreaks. 2013 August 28, 2013. [cited 2014March3] ; Available from: http://www.cdc.gov/pertussis/outbreaks/index.html
- 20.Healy CM, Rench MA, Wootton SH, Castagnini LA. Evaluation of the Impact of a Pertussis Cocooning Program on Infant Pertussis Infection. The Pediatric Infectious Disease Journal. 2015;34(1):22–26. doi: 10.1097/INF.0000000000000486 [DOI] [PubMed] [Google Scholar]
- 21.Housey M, Zhang F, Miller C, Lyon-Callo S, McFadden J, Garcia E, Potter R. Vaccination with tetanus, diphtheria, and acellular pertussis vaccine of pregnant women enrolled in Medicaid–Michigan, 2011–2013. MMWR Morb Mortal Wkly Rep. 2014;63(38):839–42 [PMC free article] [PubMed] [Google Scholar]
- 22.Kharbanda EO, G1 V-B, Lipkind HS, Klein NP, Cheetham TC, Naleway A, Omer SB, Hambidge SJ, Lee GM, Jackson ML, et al.. EValuation of the association of maternal pertussis vaccination with obstetric events and birth outcomes. JAMA. 2014;312(18):1897–1904. doi: 10.1001/jama.2014.14825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kretsinger K, Broder KR, Cortese MM, Joyce MP, Ortega-Sanchez I, Lee GM, Tiwari T, Cohn AC, Slade BA, Iskander JK, Mijalski CM, et al.. Preventing tetanus, diphtheria, and pertussis among adults: use of tetanus toxoid, reduced diphtheria toxoid and acellular pertussis vaccine recommendations of the Advisory Committee on Immunization Practices (ACIP) and recommendation of ACIP, supported by the Healthcare Infection Control Practices Advisory Committee (HICPAC), for use of Tdap among health-care personnel. MMWR Recomm Rep. 2006;55(RR-17):1–37 [PubMed] [Google Scholar]
- 24.Sirkus L, Lukacs S, Branum A. NCHS Data on Pertussis Hospitalization in Young Children. 2010. January 7, 2010 [cited 2013June4] ; Available from: http://www.cdc.gov/nchs/data/hestat/pertussis/pertussis.htm
- 25.Committee on Obstetric Practice ACOG Committee Opinion No. 566: Update on immunization and pregnancy: Tetanus, diphtheria, and pertussis vaccination. Obstet Gynecol. 2013;121(6):1411–4 [DOI] [PubMed] [Google Scholar]
- 26.Omer SB, Goodman D, Steinhoff MC, Rochat R, Klugman KP, Stoll BJ, Ramakrishnan U. Maternal influenza immunization and reduced likelihood of prematurity and small for gestational age births: A retrospective cohort study. PLoS Medicine. 2011;8(5):e1000441. doi: 10.1371/journal.pmed.1000441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Steinhoff MC, Omer SB, Roy E, El Arifeen S, Raqib R, Dodd C, Breiman RF, Zaman K. Neonatal outcomes after influenza immunization during pregnancy: a randomized controlled trial. CMAJ. 2012;184(6):645–653. doi: 10.1503/cmaj.110754 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zaman K, Roy E, Arifeen SE, Rahman M, Raqib R, Wilson E, Omer SB, Shahid NS, Breiman RF, Steinhoff MC. Effectiveness of maternal influenza immunization in mothers and infants. N Engl J Med. 2008;359(15):1555–1564. doi: 10.1056/NEJMoa0708630 [DOI] [PubMed] [Google Scholar]
- 29.Phadke VK, Steinhoff MC, Omer SB, MacDonald NE. Maternal Influenza Immunization and Adverse Birth Outcomes: Using Data and Practice to Inform Theory and Research Design. Am J Epidemiol. 2016;184(11):789–792. doi: 10.1093/aje/kww110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bratton KN, Wardle MT, Orenstein WA, Omer SB. Maternal influenza immunization and birth outcomes of stillbirth and spontaneous abortion: a systematic review and meta-analysis. Clin Infect Dis. 2015;60(5):e11–9. doi: 10.1093/cid/ciu915 [DOI] [PubMed] [Google Scholar]
- 31.Katz J, Englund JA, Steinhoff MC, Khatry SK, Shrestha L, Kuypers J, Mullany LC, Chu HY, LeClerq SC, Kozuki N, et al.. Nutritional status of infants at six months of age following maternal influenza immunization: A randomized placebo-controlled trial in rural Nepal. Vaccine. 2017;35(48 Pt B):6743–6750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sugimura T, Nagai T, Kobayashi H, Ozaki Y, Yamakawa R, Hirata R. Effectiveness of maternal influenza immunization in young infants in Japan. Pediatr Int. 2016;58(8):709–13. doi: 10.1111/ped.12888 [DOI] [PubMed] [Google Scholar]
- 33.Poehling KA, Szilagyi PG, Staat MA, Snively BM, Payne DC, Bridges CB, Chu SY, Light LS, Prill MM, Finelli L, et al.. Impact of maternal immunization on influenza hospitalizations in infants. Am J Obstet Gynecol. 2011;204(6 Suppl 1):S141–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Omer SB, Goodman D, Steinhoff MC, Rochat R, Klugman KP, Stoll BJ, Ramakrishnan U. Maternal influenza immunization and reduced likelihood of prematurity and small for gestational age births: A retrospective cohort study. PLoS Med. 2011;8(5):e1000441. doi: 10.1371/journal.pmed.1000441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Vannice KS, Salmon DA, Shui I, Omer SB, Kissner J, Edwards KM, Sparks R, Dekker CL, Klein NP, Gust DA. Attitudes and beliefs of parents concerned about vaccines: impact of timing of immunization information. Pediatrics. 2011;127(Suppl 1):S120–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Frew PM, Saint-Victor DS, Owens LE, Omer SB. Socioecological and message framing factors influencing maternal influenza immunization among minority women. Vaccine. 2014;32(15):1736–44. doi: 10.1016/j.vaccine.2014.01.030 [DOI] [PubMed] [Google Scholar]
- 37.Frew PM, Kriss JL, Chamberlain AT, Malik F, Chung Y, Cortés M, Omer SB. A randomized trial of maternal influenza immunization decision-making: A test of persuasive messaging models. Hum Vaccin Immunother. 2016;12(8):1989–1996. doi: 10.1080/21645515.2016.1199309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Frew PM, Owens LE, Saint-Victor DS, Benedict S, Zhang S, Omer SB. Factors associated with maternal influenza immunization decision-making. Evidence of immunization history and message framing effects. Hum Vaccin Immunother. 2014;10(9):2576–83. doi: 10.4161/hv.32248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Frew PM, Painter JE, Hixson B, Kulb C, Moore K, del Rio C, Esteves-Jaramillo A, Omer SB. Factors mediating seasonal and influenza A (H1N1) vaccine acceptance among ethnically diverse populations in the urban south. Vaccine. 2012;30(28):4200–8. doi: 10.1016/j.vaccine.2012.04.053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Frew PM, Zhang S, Saint-Victor DS, Schade AC, Benedict S, Banan M, Ren X, Omer SB. Influenza vaccination acceptance among diverse pregnant women and its impact on infant immunization. Hum Vaccin Immunother. 2013;9(12):2591–602. doi: 10.4161/hv.26993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Falter KH, Strikas RA, Barker WH, Brugliera PD, Bandemer CJ, Doggett KB, Williams WW. Curriculum content on vaccine-preventable diseases in U.S. medical schools. Am J Prev Med. 1994;(10 Suppl):4–10 [PubMed] [Google Scholar]
- 42.Strikas RA, Falter KH, Barker WH, Brugliera PD, Bandemer CJ, Doggett KB, Williams WW. Curriculum content on vaccine-preventable diseases in primary care and preventive medicine residency programs in the United States. Am J Prev Med. 1994;(10 Suppl):11–7 [PubMed] [Google Scholar]
- 43.Tan TQ, Bhattacharya L, Gerbie MV. Awareness, perceptions and knowledge of recommended adult vaccines among a nationwide sample of adult primary care providers. J Reprod Med. 2011;56(7–8):301–7 [PubMed] [Google Scholar]
- 44.Leddy MA, Anderson BL, Power ML, Gall S, Gonik B, Schulkin J. Changes in and current status of obstetrician-gynecologists' knowledge, attitudes, and practice regarding immunization. Obstet Gynecol Surv. 2009;64(12):823–9. doi: 10.1097/OGX.0b013e3181c4bbb7 [DOI] [PubMed] [Google Scholar]
- 45.Naleway AL, Smith WJ, Mullooly JP. Delivering influenza vaccine to pregnant women. Epidemiol Rev. 2006;28:47–53. doi: 10.1093/epirev/mxj002 [DOI] [PubMed] [Google Scholar]
- 46.Eppes C, Wu A, Cameron KA, Garcia P, Grobman W. Does obstetrician knowledge regarding influenza increase HINI vaccine acceptance among their pregnant patients? Vaccine. 2012;30(39):5782–4. doi: 10.1016/j.vaccine.2012.06.032 [DOI] [PubMed] [Google Scholar]
- 47.Broughton DE, Beigi RH, Switzer GE, Raker CA, Anderson BL. Obstetric health care workers' attitudes and beliefs regarding influenza vaccination in pregnancy. Obstet Gynecol. 2009;114(5):981–987. doi: 10.1097/AOG.0b013e3181bd89c2 [DOI] [PubMed] [Google Scholar]
- 48.Gonik B, Jones T, Contreras D, Fasano N, Roberts C. The obstetrician-gynecologist's role in vaccine-preventable diseases and immunization. Obstet Gynecol. 2000;96(1):81–4 [DOI] [PubMed] [Google Scholar]
- 49.Chamberlain AT, K2 S, KA3 A, Rosenberg ES, Frew PM, Cortés M, Whitney EA, Berkelman RL, Orenstein WA, Omer SB. Improving influenza and Tdap vaccination during pregnancy: A cluster-randomized trial of a multi-component antenatal vaccine promotion package in late influenza season. Vaccine. 2015;33(30):3571–9. doi: 10.1016/j.vaccine.2015.05.048 [DOI] [PubMed] [Google Scholar]
- 50.Chamberlain AT, Seib K, Ault KA, Rosenberg ES, Frew PM, Cortés M, Whitney EAS, Berkelman RL, Orenstein WA, Omer SB. Improving influenza and Tdap vaccination during pregnancy: a cluster-randomized trial of a multi-component antenatal vaccine promotion package in late influenza season. Under review at Vaccine. Submitted on 01/14/15, 2015 [DOI] [PubMed] [Google Scholar]
- 51.Chamberlain AT, Seib K, Ault KA, Orenstein WA, Frew PM, Malik F, Cortés M, Cota P, Whitney EA, Flowers LC. Factors Associated with Intention to Receive Influenza and Tetanus, Diphtheria, and Acellular Pertussis (Tdap) Vaccines during Pregnancy: A Focus on Vaccine Hesitancy and Perceptions of Disease Severity and Vaccine Safety. PLoS Curr. 2015;7. doi: 10.1371/currents.outbreaks.d37b61beebae5a7a06d40a301cfa819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Barnard JG, Dempsey AF, Brewer SE, Pyrzanowski J, Mazzoni SE, O'Leary ST. Facilitators and barriers to the use of standing orders for vaccination in obstetrics and gynecology settings. Am J Obstet Gynecol. 2017;216(1):69 e1–69 e7. doi: 10.1016/j.ajog.2016.09.096 [DOI] [PubMed] [Google Scholar]
- 53.O'Leary ST, Pyrzanowski J, Brewer SE, Dickinson LM, Dempsey AF. Evidence-based vaccination strategies in obstetrics and gynecology settings: Current practices and methods for assessment. Hum Vaccin Immunother. 2016;12(4):866–71. doi: 10.1080/21645515.2015.1130194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Dempsey AF, Brewer SE, Sevick C, Pyrzanowski J, Mazzoni S, O'Leary ST. Tdap vaccine attitudes and utilization among pregnant women from a high-risk population. Hum Vaccin Immunother. 2016;12(4):872–8. doi: 10.1080/21645515.2015.1094594 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Dempsey AF, Pyrzanowski J, Brewer S, Barnard J, Sevick C, O'Leary ST. Acceptability of using standing orders to deliver human papillomavirus vaccines in the outpatient obstetrician/gynecologist setting. Vaccine. 2015;33(15):1773–9. doi: 10.1016/j.vaccine.2015.02.044 [DOI] [PubMed] [Google Scholar]
- 56.Mazzoni SE, Brewer SE, Pyrzanowski JL, Durfee MJ, Dickinson LM, Barnard JG, Dempsey AF, O'Leary ST. Effect of a multi-modal intervention on immunization rates in obstetrics and gynecology clinics. Am J Obstet Gynecol. 2016;214(5):617 e1–7. doi: 10.1016/j.ajog.2015.11.018 [DOI] [PubMed] [Google Scholar]
- 57.Bluman B, Jarvis-Selinger S, Hotz S. Guidelines implementation: transforming physician/patient interaction through stages of change. J Contin Educ Health Prof. 2007;27(3):188–9. doi: 10.1002/chp.123 [DOI] [PubMed] [Google Scholar]
- 58.Walsh JM, McPhee SJ. A systems model of clinical preventive care: an analysis of factors influencing patient and physician. Health Educ Q. 1992;19(2):157–75. doi: 10.1177/109019819201900202 [DOI] [PubMed] [Google Scholar]
- 59.Petty RE. Creating strong attitudes: two routes to persuasion. NIDA Res Monogr. 1995;155:209–24 [PubMed] [Google Scholar]
- 60.Collins J, Alona I, Tooher R, Marshall H. Increased awareness and health care provider endorsement is required to encourage pregnant women to be vaccinated. Hum Vaccin Immunother. 2014;10(10):2922–9. doi: 10.4161/21645515.2014.971606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Bonville CA, Cibula DA, Domachowske JB, Suryadevara M. Vaccine attitudes and practices among obstetric providers in New York State following the recommendation for pertussis vaccination during pregnancy. Hum Vaccin Immunother. 2015;11(3):713–8. doi: 10.1080/21645515.2015.1011999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Chamberlain AT, K2 S, KA3 A, Rosenberg ES, Frew PM, Cortes M, Whitney EA, Berkelman RL, Orenstein WA, Omer SB. Impact of a multi-component antenatal vaccine promotion package on improving knowledge, attitudes and beliefs about influenza and Tdap vaccination during pregnancy. Hum Vaccin Immunother. 2016;12(8):2017–2024. doi:… [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Nowak GJ, Sheedy K, Bursey K, Smith TM, Basket M. Promoting influenza vaccination: insights from a qualitative meta-analysis of 14 years of influenza-related communications research by U.S. Centers for Disease Control and Prevention (CDC). Vaccine. 2015;33(24):2741–56. doi: 10.1016/j.vaccine.2015.04.064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Stinchfield PK. Practice-proven interventions to increase vaccination rates and broaden the immunization season. Am J Med. 2008;121(7 Suppl 2):S11–21 [DOI] [PubMed] [Google Scholar]
- 65.Omer SB, Salmon DA, Orenstein WA, deHart MP, Halsey N. Vaccine refusal, mandatory immunization, and the risks of vaccine-preventable diseases. N Engl J Med. 2009;360(19):1981–8. doi: 10.1056/NEJMsa0806477 [DOI] [PubMed] [Google Scholar]
- 66.Leask J, Kinnersley P, Jackson C, Cheater F, Bedford H, Rowles G. Communicating with parents about vaccination: a framework for health professionals. BMC pediatrics. 2012;12(1):154. doi: 10.1186/1471-2431-12-154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Wheelock A, Parand A, Rigole B, Thomson A, Miraldo M, Vincent C, Sevdalis N. Socio-psychological factors driving adult vaccination: A qualitative study. PLoS One. 2014;9(12):e113503. doi: 10.1371/journal.pone.0113503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Gowda C, Dempsey AF. The rise (and fall?) of parental vaccine hesitancy. Hum Vaccin Immunother. 2013;9(8):1755–62. doi: 10.4161/hv.25085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Stockwell MS, Fiks AG. Utilizing health information technology to improve vaccine communication and coverage. Hum Vaccin Immunother. 2013;9(8):1802–11. doi: 10.4161/hv.25031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Quinn SCParmerJ, Freimuth VS, Hilyard KM, Musa D, Kim KH. Exploring communication, trust in government, and vaccination intention later in the 2009 H1N1 pandemic: Results of a national survey. Biosecur Bioterror. 2013;11(2):96–106. doi: 10.1089/bsp.2012.0048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Stewart MA. Effective physician-patient communication and health outcomes: A review. CMAJ. 1995;152(9):1423–33 [PMC free article] [PubMed] [Google Scholar]
- 72.Zimmerman RK. Enhancing Engagement of Clinicians in Adult Immunizations: Reflections on a decade and a half of research. Vaccine. 2014;32(52):7040. doi: 10.1016/j.vaccine.2014.10.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Zimmerman RK, Nowalk MP, Lin CJ, Hannibal K, Moehling KK, Huang HH, Matambanadzo A, Troy J, Allred NJ, Gallik G. Cluster randomized trial of a toolkit and early vaccine delivery to improve childhood influenza vaccination rates in primary care. Vaccine. 2014;32(29):3656–63. doi: 10.1016/j.vaccine.2014.04.057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Caskey RN, Macario E, Johnson DC, Hamlish T, Alexander KA. A School-Located Vaccination Adolescent Pilot Initiative in Chicago: Lessons Learned. J Pediatric Infect Dis Soc. 2013;2(3):198–204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Albert SM. Standing orders for influenza and pneumococcal polysaccharide vaccination: Correlates identified in a national survey of US Primary care physicians. BMC family practice. 2012;13(1):22. doi: 10.1186/1471-2296-13-22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.United States Census Bureau 2012–2016 American Community Survey 5-Year Estimates. 2017. [cited 2017December8] ; Available from: http://factfinder.census.gov/bkmk/table/1.0/en/ACS/16_5YR/B01002/0400000US13
- 77.Guest G, MacQueen KM. Handbook for team-based qualitative research. 2008: Lanham, Altamira [Google Scholar]
- 78.Glaser BG. Grounded theory and gender relevance. Health Care Women Int. 2002;23(8):786–93. doi: 10.1080/07399330290112317 [DOI] [PubMed] [Google Scholar]
- 79.Carey JW, Morgan M, Oxtoby MJ. Intercoder agreement in analysis of responses to open-ended interview questions: Examples from tuberculosis research. Cultural Anthropology Methods. 1996;8(3):1–5 [Google Scholar]
- 80.Chen PY, Popovich PM. Correlation: Parametric and nonparametric measures. 2002: Sage [Google Scholar]
- 81.Miles MB, Huberman AM. Qualitative data analysis: An expanded sourcebook. 2nd ed. 1994, Thousand Oaks, CA: Sage [Google Scholar]


