ABSTRACT
Despite vaccines benefits, parent's vaccine hesitancy is growing. Health locus of control (HLOC) may affect decision making regarding child vaccinations. The aim of this study was to investigate the relationship between parents' HLOC and compliance with routine childhood immunization programs. A cross-sectional survey was conducted among 731 parents of children aged 3–4 years. Internal HLOC, powerful others and chance HLOC (dimensions of external HLOC), reliability of information sources, and attitudes towards vaccines were measured. Path analysis was conducted to explore direct and indirect associations between HLOC and vaccination's compliance. The results show that High powerful others HLOC has a direct association with vaccination compliance (ß = 0.23, p < 0.001). High internal and chance HLOC have indirect associations through parents' attitudes regarding vaccines. Perceived reliability of information sources was associated with not complying with vaccines (ß = −0.07, p < 0.05). For conclusions, Interaction between internal and external HLOC may explain vaccination compliance. Decreasing levels of chance HLOC and increasing powerful others HLOC may increase levels of compliance with childhood vaccinations.
KEYWORDS: childhood vaccinations, internal/external locus of control, vaccine's attitudes
Introduction
“Vaccine hesitancy” is a broad concept that represents a heterogeneous group of parents who vaccinate their children but have doubts and concerns regarding a vaccine's necessity and safety.1-4 The term was coined about 15 years ago3 and vaccine hesitancy exists among a large percentage of parents.5 These parents may choose to vaccinate with only a selected list of vaccines; delay or refuse some vaccines; or even comply with all recommended vaccines, but with ambivalent feelings towards their choice. This lack of confidence in vaccines stems especially from fear of possible associated adverse events.3 Vaccine hesitant parents are a larger group compered to parents who refuse all vaccines.5 Opel et al.5 found that 33% of parents defined themselves as vaccine hesitant, and higher scores of vaccines hesitancy were associated with lower rates of vaccinated children.
Understanding parents who are vaccine hesitant is important in order to prevent a decline in vaccine coverage. There is a need among public health organizations to tailor suitable intervention programs to encourage hesitant parents to vaccinate their children3,5-9
In Israel, the National Immunization Program (INIP) includes vaccines against 13 diseases. The INIP is non-mandatory and free of charge for every child residing in Israel. The vaccines are administered in Mother-Child Health Clinics (MCHC) located all over the country. Overall, vaccine coverage is 90% but occasionally, Israel experiences outbreaks of vaccine-preventable diseases such as measles, in small communities with low vaccine coverage.10-11
Health locus of control
Health locus of control (HLOC) refers to the individual's perceptions of the importance of factors governing his or her own health or illness. Individuals may believe that they can positively influence their own health if they make a decision in an active and independent manner according to their wishes and needs. These perceptions are defined as internal factors. In contrast, others may believe that their health depends upon external factors such as God, chance, or other people such as their doctors. This may influence more passive health behavior because these factors are external to the individual and he or she has lower influence on them.12-14
HLOC is recognized as one of the factors that can explain health promotion behavior.14-19 Studies have found inconsistent results: Grotz et al.15 found that high internal HLOC is associated with health promotion behavior whereas Steptoe & Wardle20 found that high external HLOC, particularly belief in powerful others, may explain preventive and health promotion behavior. Other studies suggest that HLOC is a complex issue and only interaction between internal and external factors can explain one's health behavior.21 Wallston22 emphasizes that perception of HLOC depends on the situation, that it is a general orientation of health behavior, and that each individual will behave differently in each situation.
In this study, we use the definition of HLOC provided by Wallston, Wallston &DeVellis,23 which refers to three dimensions: internal LOC, belief in chance LOC and belief in powerful others LOC (The latter two represent an external HLOC).
Internal LOC refers to the extent to which individuals believe in their own ability to influence their health status. Chance LOC refers to the extent to which individuals believe that their health status is a matter of fate or luck. Powerful others LOC refers to the extent to which individuals believe that their health status is determined by other people such as their physicians or nurses. Internal LOC, chance LOC, and powerful others LOC are three parallel dimensions and are independent of each other.22
Internal or external HLOC may be a factor influencing vaccine hesitancy; however, no studies have investigated these associations directly. A few studies have looked at HLOC and compliance with childhood vaccinations as a marginal behavior in general health preventive behavior, such as regular visits at the doctor.4,24
Studies explored that beliefs and attitudes regarding vaccines, influences parents' decision-making.1,7,25-26 In addition, few studies suggested that beliefs and attitudes regarding vaccines are mediating variables between sociodemographic status, and vaccination27 and HLOC beliefs mediated the association between socioeconomic status and self-rated health.28
Drawing on these studies, the theoretical model for the current study (Fig. 1) assumes: (1) a direct association between socioeconomic variables and the three HLOC dimensions and compliance with routine childhood vaccinations; (2) beliefs and attitudes regarding vaccines mediate the association between socioeconomic variables, HLOC, and compliance with childhood vaccinations.
Figure 1.
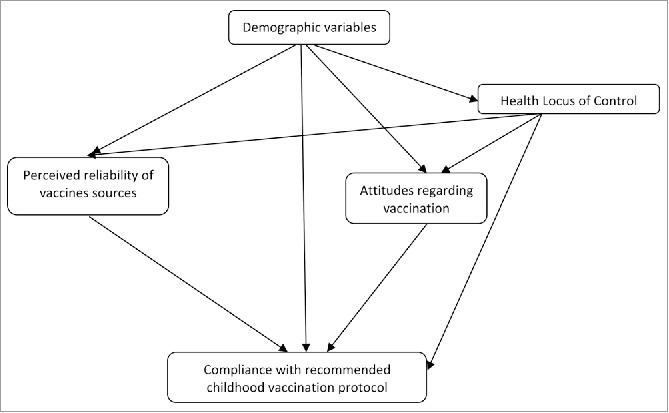
Theoretical model: Relationship between demographic variables, health locus of control attitudes, and beliefs regarding vaccination and compliance.
Aim
The primary goals of this study were to assess the relationship between the three HLOC dimensions and parental compliance with recommended vaccinations, and to determine how beliefs and attitudes regarding vaccines mediate the relationship.
Results
Two groups of parents were interviewed: 309 parents of children who had not completed one or more of the vaccinations recommended (the study group) and 422 parents of children who had completed the recommended vaccinations (the control group).
Socioeconomic characteristics
Parents of the study group had higher levels of education and income compared with the control group (χ2 = 32.43, p < 0.001, χ2 = 6.39, p < 0.001), included more Jews (χ2 = 32.63, p < 0.001) and older parents (38.58 vs. 36.17 years, p < .001). No significant difference was found between the groups in terms of number of children.
Health locus of control
A MANOVA test revealed that internal HLOC was significantly higher among participants with above average income (F = 10.26, p < 0.01). Chance HLOC was significantly higher among participants with a non-academic education (F = 21.02, p < 0.001), Muslims (F = 8.04, p < 0.01) and participants with average or lower income (F = 19.60, p < 0.001). Powerful others HLOC was significantly higher among those with a non-academic education (F = 23.62, p < 0.001) and Muslims (F = 63.84, p < 0.001) (Table 1). In addition, younger parents reported perception of higher powerful others HLOC (F = 2.04, p < 0.01) (not in the table). No other significant differences were found.
Table 1.
Participant level of health locus of control by socioeconomics variables (MANOVA).
| Health Powerful others locus of control | Health Chance locus of control | Health Internal locus of control | ||
|---|---|---|---|---|
| Variable (n) | M (SD) | M (SD) | M (SD) | |
| Education | Not academic (240) | 3.13 (0.84) | 2.40 (0.72) | 2.87 (0.74) |
| Academic (248) | 3.23 (0.77) | 2.15 (0.65) | 2.59 (0.69) | |
| p≤ | 0.09 | 0.001 | 0.001 | |
| Religion | Jewish (636) | 3.22 (0.79) | 2.21 (0.69) | 2.69 (0.71) |
| Muslims (90) | 3.06 (0.80) | 2.43 (0.61) | 3.23 (0.49) | |
| p≤ | 0.07 | 0.01 | 0.001 | |
| Income | Average or Lower (295) | 3.08 (0.85) | 2.37 (0.69) | 2.69 (0.76) |
| Above Average (344) | 3.28 (0.73) | 2.13 (0.67) | 2.60 (0.67) | |
| p≤ | 0.01 | 0.001 | 0.11 |
A MANOVA test revealed that internal HLOC and powerful others HLOC among parents of the study group were significantly lower than the control group (3.00 vs. 3.34, p < 0.001; 2.25 vs. 3.00, p<0.001). Chance HLOC was significantly higher among parents of the study group than parents at the control group (2.34 vs. 2.16, p < 0.001) (Table 2).
Table 2.
Participants' locus of control, beliefs, and attitudes by parent groups (MANOVA).
| Completed Vaccination Protocol | Did Not Complete Vaccination Protocol | F | p< | |
|---|---|---|---|---|
| Variable | M (SD) | M (SD) | ||
| Internal health locus of control | 3.34(0.72) | 3.00 (0.81) | 8.66 | 0.001 |
| chance health locus of control | 2.16 (0.66) | 2.34 (0.71) | 6.48 | 0.001 |
| Powerful others health locus of control | 3.00 (0.56) | 2.25 (0.69) | 18.23 | 0.001 |
| Pro vaccine attitudes | 3.49 (0.52) | 2.78 (0.76) | 220.27 | 0.001 |
| Anti-vaccine attitudes | 2.25 (0.75) | 3.01 (0.75) | 183.31 | 0.001 |
| Mandatory vaccine attitudes | 2.42 (0.93) | 3.30 (0.75) | 20.10 | 0.001 |
| Perceived Reliability of: | ||||
| Formal Information Sources | 2.95 (0.59) | 2.61 (0.63) | 55.51 | 0.001 |
| Informal Information Sources | 1.96 (0.95) | 2.51 (0.86) | 62.29 | 0.001 |
Attitudes and beliefs
In comparison to the control group, parents of the study group had significantly lower Pro VA scores (2.78 vs. 3.49, p < 0.001), significantly higher Anti VA scores (3.01 vs. 2.25, p < 0.001), and significantly higher Mandatory VA scores (3.30 vs 2.42, p < 0.001). Parents in the study group considered formal information sources to be less reliable than their counterparts in the control group (2.61 vs. 2.95, p < 0.001), and they perceived the informal information sources that oppose vaccinations as more reliable than the parents in the control group (2.51 vs. 1.96, p < 0.001; Table 2).
Mediating variables
A path analysis (Fig. 2 and Table 3) found that decisions regarding vaccination were significantly and directly explained by parents' education level (ß = −0.12, p < 0.001), powerful other HLOC (ß = 0.23, p < 0.001), Pro VA (ß = 0.11, p < 0.01), Anti VA (ß = −0.15, p < .0001), Mandatory VA (ß = −0.17, p < 0.001), and perceived reliability of unofficial information sources that oppose vaccinations (ß = −0.07, p < 0.05). In other words, the absence of academic education, high level of powerful other HLOC, high positive attitudes regarding vaccination, weak negative attitudes regarding vaccination, weak negative attitudes regarding mandatory vaccination, and considering unofficial information sources that oppose vaccinations as unreliable increase the likelihood that parents will complete their children's vaccinations.
Figure 2.
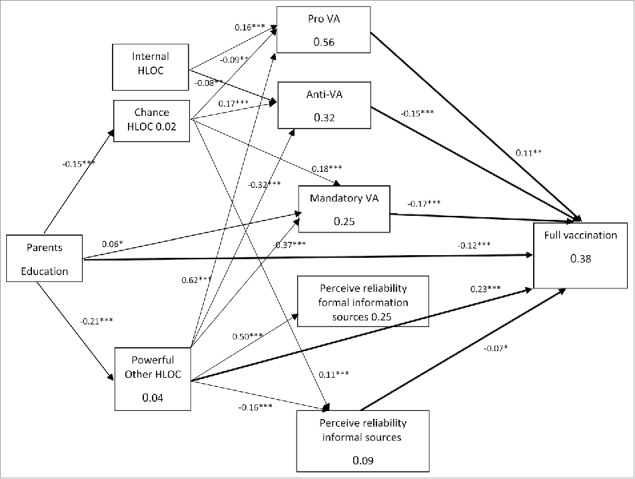
Path diagram model: direct and mediating variables association between parent's education, health locus of control, attitudes, and beliefs regarding vaccination. Values on the arrows were correlation coefficients (ß) and values in the boxes were the R2. Thick line = direct association. Model fitness: χ2(52) = 64.20, p = .119, NFI = .980, NNFI = .991, CFI = .996, RMSEA = .018.
Table 3.
Relationship of the parent's education, health locus of control, attitudes, and beliefs regarding compliance with vaccinations (path analysis).
| Dependent Variable | Independent Variable | B | S.E. | β | R2 |
|---|---|---|---|---|---|
| Internal LOC | Parent's Education | — | — | — | — |
| Chance LOC | Parent's Education | −0.22 | 0.05 | −0.15*** | 0.02 |
| Powerful others LOC | Parent's Education | −0.32 | 0.05 | −0.21*** | 0.04 |
| Pro VA | Internal LOC | 0.15 | 0.02 | 0.16*** | 0.56 |
| Chance LOC | −0.10 | 0.03 | −0.09*** | ||
| Powerful others LOC | 0.62 | 0.03 | 0.62*** | ||
| Anti-VA | Internal LOC | −0.09 | 0.03 | −0.08** | 0.32 |
| Chance LOC | 0.20 | 0.04 | 0.17*** | ||
| Powerful others LOC | −0.38 | 0.04 | −0.32*** | ||
| Mandatory VA | Parent's Education | 0.13 | 0.06 | 0.06* | 0.25 |
| Chance LOC | 0.25 | 0.05 | 0.18*** | ||
| Powerful others LOC | −0.49 | 0.05 | −0.37*** | ||
| Perceived Reliance on Formal Info Sources | Powerful others LOC | 0.44 | 0.03 | 0.50*** | 0.25 |
| Perceived Reliance on Informal Info Sources | Chance LOC | 0.08 | 0.02 | 0.11** | 0.09 |
| Powerful others LOC | −0.11 | 0.03 | −0.16*** | ||
| Decision to Vaccinate | Parent's Education | −0.13 | .03 | −0.12*** | 0.38 |
| Powerful others LOC | 0.16 | 0.03 | 0.23*** | ||
| Pro VA | .008 | .003 | 0.11* | ||
| Anti-VA | −0.09 | 0.02 | −0.15*** | ||
| Mandatory VA | −0.09 | 0.02 | −0.17*** | ||
| Perceived Reliance on Informal Info Sources | −0.07 | 0.03 | −0.07* |
p < 0.05,
p < 0.01,
p < .001; LOC— locus of control; VA— vaccination attitudes.
Parent's age, income, and religion did not have a direct effect on the completion of vaccinations. Only the absence of academic education was found to have a direct and independent effect on parents' decisions to complete childhood vaccinations. Only powerful others HLOC had a direct effect on completion of vaccination protocol.
Internal HLOC and chance HOCL were found to have an indirect effect, mediated through other variables on completion of the vaccination protocol. Findings of the Sobel test (Table 4) reveal that Pro VA, Anti VA, Mandatory VA, and perceived reliability of informal information sources that oppose vaccination acted as mediators for internal HLOC, chance HLOC, and parents' compliance with vaccination. In addition to the direct effect, powerful others HLOC affected an indirect path for compliance with vaccinations by the mediating variables.
Table 4.
Results of Sobel tests for significant relationships with the mediating variables: Parents' attitudes towards vaccination and perceived reliance on information sources (N = 731).
| Independent Variable | Mediating Variable | Sobel | S.E. |
|---|---|---|---|
| Internal LOC | Pro VA | 8.86*** | 0.013 |
| Anti-VA | 7.06*** | 0.11 | |
| Chance LOC | Pro VA | −6.91*** | 0.10 |
| Anti-VA | −6.23*** | 0.10 | |
| Mandatory VA | −5.98*** | 0.11 | |
| Reliance on Informal Sources | *3.36*** | 0.14 | |
| Powerful others LOC | Pro VA | 4.77*** | 0.16 |
| Anti-VA | 6.28*** | 0.10 | |
| Mandatory VA | 4.09*** | 0.19 | |
| Reliance on Informal Sources | 3.84*** | 0.13 |
p < 0.001.
LOC— locus of control.
VA— vaccination attitudes.
The model based on the pathway analysis (Fig. 2) was found to have a good fit with the theoretical model according to the following criteria: χ2(52) = 64.20, p = 0.119, NFI = 0.980, NNFI = .991, CFI = 0.996, RMSEA = 0.018.
Discussion
The path analysis indicates two major pathways between HLOC and compliance with recommended vaccinations:
-
1.
A direct path between powerful others HLOC and compliance with vaccinations;
-
2.
An indirect path between internal and chance HLOC through mediating variables leading to compliance with vaccinations.
To our knowledge, this is the first study that examines the relationship between HLOC and child's vaccination as the main outcome. The findings in the current study emphasized the complexity of HLOC: interaction between the three dimensions of HLOC may explain an individual's health behavior.13,21,29-31 In the current study, internal LOC, chance HLOC and powerful others HLOC explain full compliance with childhood vaccination directly and through mediating factors. Powerful others HLOC predicts direct compliance with childhood vaccinations, but an indirect path can explain this phenomenon as well. For example, internal HLOC might follow this path: as Internal HLOC increases, positive attitudes regarding vaccinations increases and negative attitudes regarding vaccinations decrease, leading to a higher probability of full vaccination (Fig. 2).
For not compliant with childhood vaccination, chance HLOC might follow this path: as chance HLOC increases, positive attitudes regarding vaccinations decrease but negative attitudes regarding vaccinations, attitudes against mandatory vaccinations, and reliability of informal sources that opposed vaccinations increase, leading to lower levels of children's vaccinations (Fig. 2).
The current study found that powerful others HLOC can directly predict compliance with vaccinations. Few studies have investigated the association between HLOC and compliance with vaccinations, and then only as part of health prevention behaviors. Tinsley & Holtgrave24 found that high internal HLOC among mothers of infants is a predicting factor to complete a child's visiting at physician clinics and vaccinations according to recommendations. The study did not find a significant association between perception of powerful others HLOC and use of preventive health services.
In general, studies found that orientation of high internal HLOC encourages compliance with preventive medicine such as: measles immunization,32 taking vitamins and iron among pregnant women,33 and prevention of children's caries.34 Nevertheless, some studies found no association between high internal HLOC and health outcomes. One result repeated consistently: high chance HLOC is a factor that has a negative influence on a healthy life styles.20,34-35 Similarly, in the current study, parents with high chance HLOC vaccinated their children less, but chance HLOC cannot directly explain complete vaccinations but through intermediary variables such as: low pro VA or high anti VA and mandatory VA.
The current study found that beliefs and attitudes regarding vaccinations were directly and positively associated with parent compliance with vaccinations. This finding has been well documented in the literature.1,25-26 Yet, the current study found that beliefs and attitudes regarding vaccinations are mediating variables between all three dimensions of HLOC and completing vaccinations. As far as we know, no study has examined these relationships. One study27 found that positive attitudes towards vaccinations and a sense of control (not LOC) are mediating factors between socioeconomic variables and compliance with childhood vaccinations. The current study supports this finding. An example of one possible path may be: academic education of the parent is associated with low perception of powerful others HLOC, associated with high anti-vaccination attitudes, and therefore, uncompleted children vaccines (Fig. 2).
The current study found that formal information sources regarding vaccines were associated with high powerful others HLOC, but no relation was found with completing vaccinations. This finding supports previous literature.36-38 At the other end of the spectrum, according to the current study, is the high degree of reliability attributed to informal sources regarding vaccinations and that variable's impact on completion of vaccinations. This variable only mediates the association between chance HLOC and vaccinations. It appears that for parents who did not comply with vaccination protocol, the perceived reliability of internet-based information sources that opposes vaccination is greater than that of formal information sources.39
The current study has several limitations. As an observational cross-sectional study, causal relationships could not be inferred. Nevertheless, the path analysis enabled the construction of a causation model,40 as presented in Fig. 2. In addition, the study was performed when the children were three to four years old, so it is possible that the parents did not remember exactly what they felt and thought when their children were one or two years, when the vaccines were administered. For this reason, we collected the children's vaccine status from their medical records.
The strength of this study is in adding the variable health locus of control as part of the determinants that can influence parents in their decision to vaccinate their child. In order to support parents who, hesitate to vaccinate their child, it is important to encourage and develop parents' trust in health care professionals. From a public health perspective, there may be a paradox: On the one hand, we are interested in parents who vaccinated their children with full understanding of the importance of vaccinations, in their safety and necessity. On the other hand, we are not interested in parents who have “blind faith” in nurses or doctors who care for them.7 We aspire to the public with the ability to make a sophisticated medical decision, based on professional and reliable information. Therefore, it is important to deepen the parents' knowledge of vaccines in order to prevent passivity or ignorance regarding the vaccinations of their child. Actions to strengthen the public's confidence in the professional health care include actions at the micro and macro levels. Micro-level activities include enriching knowledge among medical staff and providing practical tools, based on a positive attitude37 and effective communication with the parent, to cope properly with parents' hesitation in vaccinations or parents who refuse to one or all vaccines.47 The medical staff should be able to tailor a specific intervention program to vaccine hesitate parents according to their needs.2,5 In the macro level, policymaker should use sophistical social media to engagement with web media and informal sources of vaccinations in order to encourage the public trust in medical staff. Programs for the general public that engage in critical reading of informal medical information on websites, will increase the public's trust in the medical establishment. As this study suggested, such programs may act as a balance between chance HLOC and powerful others HLOC and to encourage hesitate parents to vaccinate their children.
In conclusion, this study provides evidence that parents with high levels of powerful others HLOC and high levels of pro-vaccination attitudes are most likely to vaccinate their children. Parents with high levels of chance HLOC are most likely not to vaccinate their children, a mediating factor might be high levels of anti-vaccination attitude.
Parents with high levels of internal HLOC are most likely to vaccinate their children through mediating factors such as high levels of pro-vaccination attitude and low anti-vaccination attitude.
This study highlights the importance of health LOC as having an impact on parents' decision-making regarding their child's vaccination. At the same time, parents' attitudes to vaccines are highly important as mediating factors between the health LOC and the decision on whether to vaccinate the child. Encouraging public trust in public health teams, as well as strengthening positive attitudes on vaccines, will encourage vaccination, particularly among parents who are vaccines hesitate.
Materials and methods
Study sample
This was a stratified case-control study with a retrospective cohort.41-42 The participants were recruited from parents of infants born in 2009 registered at MCHC clinics from north and central Israel. These clinics included about 13% of all births in 2009. MCHCs offer a variety of preventive health services for mother and child, including childhood vaccination. The MCHCs serve Israel's entire population. Data regarding the completion of vaccinations, as well as contact information were retrieved from the medical files at each relevant MCHC.
Two groups of children were identified
-
(1)
children who had not completed at least one of three childhood vaccinations by the age of two: three parts of the hepatitis B vaccination (HBV-3), four parts of the diphtheria-tetanus-pertussis vaccination (DTaP-4), and vaccination against mumps, measles, and rubella (MMR-1). These vaccinations are routinely administered during the first year of life and are considered core vaccination protocol. We examined whether children completed each vaccine by receiving all doses. Children who did not receive the last dose of the vaccine series were defined as children who did not fully vaccinate according to their age, whether or not they received the first doses of the vaccine series.
-
(2)
a control group of children who had completed the three vaccinations by the age of two. Each group was randomly sampled and a telephone interview was conducted with one of the parents.
The telephone interviews were conducted between December 2012 and March 2013.
Measures
Health locus of control
The measure of HLOC was based on the Multidimensional Health Locus of Control (MHLC) questionnaire developed by Wallston, Wallston & Devellis.23 MHLC assesses internal LOC, chance LOC and powerful others LOC to predict health-related behavior. The questionnaire was adapted to reflect the topic of childhood vaccinations, while remaining as faithful as possible to the original wording. For example, question for internal HLOC: “When my child is ill, I have the power to make him well again; question for cance HLOC: ”I often feel that no matter how many vaccines my child might get, if he is going be ill, he will be'; and for powerful others HLOC: ” If my child regularly visit the Mother-Child Health Clinic, my child is less likely to have health problems”. The questionnaire included 18 items ranked on a Likert scale, ranging from 1 = “not agree at all” to 4 = “very much agree”.
We tested content validity of the questionnaire according to 4 opinions from professionals in four different fields: social epidemiology, public health and vaccinations, child medicine (MD), and statistics. The questionnaire was reworded according to their recommendations until we reach a final version of the scales. Cronbach's alpha for internal LOC was 0.68; for chance LOC 0.70; and for powerful others 0.77.
Beliefs and attitudes towards vaccination and sources of information
These measures were based on the questionnaire from Salmon et al.,43 which was adapted to refer to parents of infants. Three groups of attitudes were examined:
(a) pro-vaccine attitudes (Pro VA), for example: “To what extent do you agree that vaccinations were proven safe before it was decided to administer them to children?”; (b) anti-vaccine attitudes (Anti VA), for example: “To what extent do you agree that vaccinations can cause attention deficit disorder, chronic illness, or autism?”; (c) attitudes regarding mandatory vaccination (Mandatory VA), for example: “To what extent do you agree that mandatory administration of vaccinations goes against freedom of choice?”. Answers were recorded on a Likert scale, ranging from 1 = “completely disagree” to 4 = “completely agree”. The higher scores suggest high pro- or anti vaccination attitudes in questions “a” and “b” and higher disagreement with mandatory vaccinations in questions “c”. Cronbach's alpha was 0.84, 0.80, and 0.79, respectively.
Beliefs in reliability of information sources regarding vaccines were divided into two groups: (a) formal sources of information, for example: “To what extent do you perceive the MCHC nurses as reliable?” and (b) informal sources of information, for example: “To what extent do you perceive the internet sites that oppose vaccination as reliable?” A Likert scale was provided, ranging from 1 = “completely reliable” and 4 = “completely unreliable”. Cronbach's alpha was 0.83 and 0.64, respectively.
Demographic characteristics
These characteristics included age, educational level (academic and nonacademic), number of children in the family, religion (Jewish, Muslim), and household income level. The average income in Israel in 2011 was 12,100 NIS and was stated in the questionnaire. The respondent was asked to report if his or her income was below average, average, or above average.
Statistical analysis
We used the χ2 and MANOVA tests to identify significant differences between the two parent groups regarding socioeconomic variables, health LOC dimensions, and variables related to beliefs and attitudes about vaccines. Path analysis was conducted to test the fit of the theoretical model and to analyze the mediating variables.44 To examine the model's fit (goodness of fit), the χ2 test, the non-normed fit index (NNFI), the normed fit index (NFI), and the root mean square error of approximation (RMSEA) with comparative fit index (CFI) were calculated. For the χ2 test, a p-value>0.05 indicated a nonsignificant difference between the theoretical model and the calculated (equations) statistical model, suggesting a good fit. On the NNFI, NFI, and CFI tests, p-values >0.95 and a p-value < 0.05 on the RMSEA test were considered indicative of a good model. Regression coefficient (ß) with p-value < 0.05 tested the associations between the variables. The significance of the mediating variables was performed by the Sobel test.45-46 Analyses were performed using SPSS version 21. The AMOSE software package version 22 was used for the path analysis.
Funding Statement
This work was supported by Israel National Institute for Health Policy Research (IL) source (2012/149/R). This work was supported by funding from the Israel National Institute for Health Policy Research. Grant number 2012/149/R.
Disclosure of potential conflicts of interest
No potential conflicts of interest were disclosed.
Ethical approval
The study was approved by the Ethics Committee for Studies with Human Participants at the University of Haifa.
References
- 1.Larson HJ, Jarret C, Eckersberger E, Smith DMD, Paterson P. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: a systematic review of published literature, 2007–2012. Vaccine. 2014;32:2150–9 doi: 10.1016/j.vaccine.2014.01.081. PMID:24598724. [DOI] [PubMed] [Google Scholar]
- 2.Velan B. Vaccine hesitancy as self-determination: an Israeli perspective. Isr J Health Policy Res. 2016;5:13. doi: 10.1186/s13584-016-0071-x. PMID:27051517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.ECDC Meeting report. Individual decision- making and childhood vaccination. 24 may 2013. Stockholm, Sweden: Available at: https://ecdc.europa.eu/sites/portal/files/media/en/publications/Publications/vaccination-individual-decision-making-and-childhood-vaccination.pdf. [Google Scholar]
- 4.Gesser-Edelsburg A, Shir-Raz Y, Green MS. Why do parents who usually vaccinate their children hesitate or refuse? General good vs. individual risk. J Risk Res. 2016;19:405–24. doi: 10.1080/13669877.2014.983947. [DOI] [Google Scholar]
- 5.Opel DJ, Taylor JA, Mangione-Smith R, Solomon C, Zhao C, Catz S, Martin D. Validity and reliability of a survey to identify vaccine-hesitant parents. Vaccine. 2012;29:6598–605. doi: 10.1016/j.vaccine.2011.06.115. [DOI] [PubMed] [Google Scholar]
- 6.Levitsky LL. Childhood immunization and chronic illness. New Engl J Med. 2004;350:1380–2. doi: 10.1056/NEJMp048034. PMID:15070785. [DOI] [PubMed] [Google Scholar]
- 7.Hobson-West P. “Trusting blindly can be the biggest risk of all”: organized resistance to childhood vaccination in the UK. Sociol Health Ill. 2007;29:198–215. doi: 10.1111/j.1467-9566.2007.00544.x. [DOI] [PubMed] [Google Scholar]
- 8.Byington CL. Vaccines: can transparency increase confidence and reduce hesitancy? Pediatrics. 2014;134:377–9. doi: 10.1542/peds.2014-1494. PMID:25086161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gust DA, Strine TW, Maurice E, Smith P, Yusuf H, Wilkinson M, Battaglia M, Wright R, Schwartz B. Underimmunization among children: effects of vaccine safety concerns on immunization status. Pediatrics. 2004;114(1):e16–22. doi: 10.1542/peds.114.1.e16. PMID:15231968. [DOI] [PubMed] [Google Scholar]
- 10.Anis A. Vaccine coverage report among children born 2009, report number 15628314, 27/2/2014. Jerusalem: Minister of health. [Google Scholar]
- 11.Vaysblay A. Israel national immunization program. Jerusalem: Knesset Israel; 2008. [Google Scholar]
- 12.Wallston BS, Wallston KA. Locus of control and health: A review of the literature. Health Educ Monogr. 1978;6:107–17. doi: 10.1177/109019817800600102. PMID:357347. [DOI] [PubMed] [Google Scholar]
- 13.Ahmedani BK, Peterson EL, Wells KE, Rand CS, Williams LK. Asthma medication adherence: the role of God and other health locus of control factors. Ann Allerg Asthma Im. 2013;110(2):75–9. doi: 10.1016/j.anai.2012.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Norman P, Bennett P, Smith S, Murphy A. Health locus of control and health behavior. J Health Psychol. 1998;3(2):71–180. doi: 10.1177/135910539800300202. PMID:22021344. [DOI] [PubMed] [Google Scholar]
- 15.Grotz M, Hapke U, Lampert T, Eiester H. Health locus of control and health behavior: results from a nationally representative survey psychology. Health Med. 2011;16(2):129–40. doi: 10.1080/13548506.2010.521570. [DOI] [PubMed] [Google Scholar]
- 16.Cobb-Clark D, Kassenboehmer SC, Schurer S. Healthy habits: the connection between diet, exercise, and locos of control. J Econ Behav Organ. 2014;98:1–28 doi: 10.1016/j.jebo.2013.10.011. [DOI] [Google Scholar]
- 17.Omeje O, Nebo C. The influence of locus control on adherence to treatment Regimen among Hypertensive patient. Patient Prefer Adher. 2011;5:141–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Armitage CJ. The relationship between multidimensional health locus of control and perceived behavioral control: How are distal perceptions of control related to proximal perceptions of control?. Psycho Health. 2003;18(6):723–38. doi: 10.1080/0887044031000141216. [DOI] [Google Scholar]
- 19.Holt CL, Clark EM, Kreuter MW, Rubio DM. Spiritual health locus of control and breast cancer beliefs among urban African American women. Health Psychol. 2003;22(3):294. doi: 10.1037/0278-6133.22.3.294. PMID:12790257. [DOI] [PubMed] [Google Scholar]
- 20.Steptoe A, Wardle J. Locus of control and health behavior revisited: a multivariate analysis of young adults from 18 countries. Brit J Psychol. 2001;92:659–72. doi: 10.1348/000712601162400. PMID:11762867. [DOI] [PubMed] [Google Scholar]
- 21.O'Hea EL, Grothe KB, Bodenlos JS, White MA, Brantley PJ. Predicting medical Regimen Adherence: The interaction of health locus of control beliefs. J Health Psychol. 2005;10(5):705–17. doi: 10.1177/1359105305055330. PMID:16033792. [DOI] [PubMed] [Google Scholar]
- 22.Wallston KA. The validity of the multidimensional health locus of control. J Health Psychol. 2005;10(4):623–31. doi: 10.1177/1359105305055304. PMID:16033784. [DOI] [PubMed] [Google Scholar]
- 23.Wallston KA, Wallston BS, DeVellis R. Development of the multidimensional health locus of control (MHLC) scales. Health Educ Behav. 1978;6:160–70. [DOI] [PubMed] [Google Scholar]
- 24.Tinsley BJ, Holtgrave DR. Maternal health locus of control beliefs, utilization of childhood preventive health services, and infant health. Dev Behavioral Pediatrics. 1989;10(5):236–41. doi: 10.1097/00004703-198910000-00003. [DOI] [PubMed] [Google Scholar]
- 25.Evans M, Stoddart H, Condon L, Freeman E, Grizzell M, Mullen R. Parents' perspectives on the MMR immunization: a focus group study. Br J Gen Prac. 2001;51:904–10. [PMC free article] [PubMed] [Google Scholar]
- 26.Anglillo IF, Ricciardi G, Rossi P, Pantisano P, Langiano E, Pavia M. Mothers and vaccination: knowledge, attitudes and behavior in Italy. Bull World Health Organization. 1999;77(3):224–9. [PMC free article] [PubMed] [Google Scholar]
- 27.Prislin R, Dyer J, Blakely CH, Johonson CD. Immunization status and sociodemographic characteristics: The mediating role of beliefs, attitudes, and perceived control. Am J Public Health. 1998;88(12):1821–6. doi: 10.2105/AJPH.88.12.1821. PMID:9842380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Poortinga W, Dunstan FD, Fone DL. Health locus of control beliefs and socio-economic differences in self-rated health. Prev Med. 2008;46:374–80. doi: 10.1016/j.ypmed.2007.11.015. PMID:18177930. [DOI] [PubMed] [Google Scholar]
- 29.Janowaki K, Kurpas D, Kusz J, Mroczek B, Jedynak T. Health-related behavior, profile of health locus of control and acceptance of illness on patient suffering from chronic somatic diseases. Plos One. 2013;8(5):e63920. doi: 10.1371/journal.pone.0063920. PMID:23675516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sonntage U, Esch T, Hagen L, Renneberg B, Braun V, Heintze C. Locus of control, self-efficacy and attribution tendencies in obese patients – implication for primary care consultations. Med Sci Monitor. 2010;16(7):cr330–335. [PubMed] [Google Scholar]
- 31.Lau RR. Origins of health locus of control beliefs. J Pers Soc Psycho. 1982;2:322–34. doi: 10.1037/0022-3514.42.2.322. [DOI] [PubMed] [Google Scholar]
- 32.Weitkunat R, Markuzzi A, Vogel S, Schlipkoter U, Koch H, Meywe G, Ferring D. Psychological factors associated with the uptake of measles immunization. J health psychol. 1998;3(2):273–84. doi: 10.1177/135910539800300210. PMID:22021365. [DOI] [PubMed] [Google Scholar]
- 33.Haslam C, Lawrence W, Haefeli K. Intention to breastfeed and other important health-related behavior and beliefs during pregnancy. Fam Prac. 2003;20(5):528–30. doi: 10.1093/fampra/cmg506. [DOI] [PubMed] [Google Scholar]
- 34.Duijster D, Loveren C, Dusseldorp E, Verrips GHW. Modelling community, family, and individual determinants of childhood dental caries. Eur J Oral Sci. 2014;122:125–33. doi: 10.1111/eos.12118. PMID:24524246. [DOI] [PubMed] [Google Scholar]
- 35.Leganger A, Kraft P. Control constructs: do they mediate the relation between educational attainment and health behavior? J Health Psychol. 2003;8(3):361–72. doi: 10.1177/13591053030083006. PMID:14670214. [DOI] [PubMed] [Google Scholar]
- 36.Austvoll-Dahlgen A, Helseth S. What informs parents' decision making about childhood vaccinations? J Adv Nurs. 2010;66:2421–30. doi: 10.1111/j.1365-2648.2010.05403.x. PMID:20722796. [DOI] [PubMed] [Google Scholar]
- 37.Danchin M, Nolan TA. Positive approach to patents with concern about vaccination for the family physician. Aust Fam Physician. 2014;43:690–4. PMID:25286425. [PubMed] [Google Scholar]
- 38.Amit-Aharon A, Nehama H, Rishpon S, Baron-Epel O. Parents with high levels of communicative and critical health literacy are less likely to vaccinate their children. Patient Educ Couns. 2017;100:768–75. doi: 10.1016/j.pec.2016.11.016. PMID:27914735. [DOI] [PubMed] [Google Scholar]
- 39.Kata A. A postmodern Pandora's box: anti-vaccination misinformation on the internet. Vaccine. 2010;28:1709–16. doi: 10.1016/j.vaccine.2009.12.022. PMID:20045099. [DOI] [PubMed] [Google Scholar]
- 40.Wu AD, Zumbo BD. Understanding and using mediators and moderators. Soc Indic Res. 2008;87:367–92. doi: 10.1007/s11205-007-9143-1. [DOI] [Google Scholar]
- 41.Wacholder S, McLaughlin J, Silveman DT, Mandel JS. Selection of controls in case-control studies, part 1: principles. Am J Epidemiol. 1992;135:1019–28. Available from: Institute for Vaccine Safety Johns Hopkins Bloombery School of Public Health, www.vaccinesafety.edu. doi: 10.1093/oxfordjournals.aje.a116396. PMID:1595688. [DOI] [PubMed] [Google Scholar]
- 42.Ernester VL. Nested case – control studies. Prev Med. 1997;23:587–90. doi: 10.1006/pmed.1994.1093. [DOI] [PubMed] [Google Scholar]
- 43.Salmon DA, Moulton LH, Omer SB, Chace LM, Klassen A, Talebian P, Halsey NA. Knowledge, attitudes, and beliefs of school nurses and personnel and associations with nonmedical immunization exemptions. Pediatrics. 2004;113:e552–e9. doi: 10.1542/peds.113.6.e552. PMID:15173536. [DOI] [PubMed] [Google Scholar]
- 44.Preacher K, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav Res Methods. 2008;40:879–91. doi: 10.3758/BRM.40.3.879. PMID:18697684. [DOI] [PubMed] [Google Scholar]
- 45.Imai K, Keele L, Tingley DA. General approach to causal mediation analysis. Psychol Methods. 2010;15:309–34. doi: 10.1037/a0020761. PMID:20954780. [DOI] [PubMed] [Google Scholar]
- 46.MacKinnon DP, Dwyer JH. Estimating mediated effects in prevention studies. Evaluation Rev. 1993;17:144–58. doi: 10.1177/0193841X9301700202. [DOI] [Google Scholar]
- 47.Leask J, Kinnersley P, Jackson C, Cheater F, Bedford H, Rowles G. Communicating with parents about vaccination: a framework for health professionals. BMC Pediatrics. 2012;12:154–64. doi: 10.1186/1471-2431-12-154. PMID:22998654. [DOI] [PMC free article] [PubMed] [Google Scholar]


