Abstract
Background & Aims
Epidemiologic analyses of acute and chronic pancreatitis (AP and CP) provide insight into causes and strategies for prevention, and affect allocation of resources to its study and treatment. We sought to determine current and accurate incidences of AP and CP, along with the prevalence of CP, in children and adults in the United States.
Methods
We collected data from the Truven MarketScan Research Databases of commercial inpatient and outpatient insurance claims in the United States from 2007 through 2014 (patients 0–64 years old). We calculated the incidences of AP and CP, and prevalence of CP, based on International Classification of Diseases, Ninth Revision (ICD-9) diagnosis codes. Children were defined as 18 years or younger and adults as 19 to 64 years old.
Results
The incidence of pediatric AP was stable from 2007 through 2014, remaining at 12.3/100,000 persons in 2014. Meanwhile the incidence for adult AP decreased from 123.7/100,000 persons in 2007 to 111.2/100,000 persons in 2014. The incidence of CP decreased over time in children (2.2/100,000 persons in 2007 to 1.9/100,000 persons in 2014) and adults (31.7/100,000 persons in 2007 to 24.7/100,000 persons in 2014). The prevalence of pediatric and adult CP was 5.8/100,000 persons and 91.9/100,000 persons, respectively in 2014. Incidences of AP and CP increased with age; we found little change in incidence during the first decade of life, but linear increases starting in the second decade.
Conclusions
We performed a comprehensive epidemiologic analysis of privately insured non-elderly adults and children with AP and CP in the United States. Changes in gallstone formation, smoking, and alcohol consumption, along with advances in pancreatitis management, may be responsible for the stabilization and even decrease in the incidences of AP and CP.
Keywords: pancreas, inflammation, trends, epidemiology
INTRODUCTION
Globally, pancreatitis occurred in over 17 million individuals in 2013, making it the 35th most common disease/injury in the world, an incidence nearly twice that of acute myocardial infarctions.1 In the United States (U.S.), the annual incidence of acute pancreatitis (AP) is estimated to be approximately 40/100,000 persons, resulting in over 130,000 new cases per year. Chronic pancreatitis (CP) occurs less frequently, reported at about 8/100,000 persons.2 Historically, pancreatitis has been considered primarily an adult disease, strongly associated with alcohol use and gallstones. However, pediatric pancreatitis has received greater attention over the last decade. Based on single academic center studies, the incidence of pediatric AP in the U.S. is reported to be between 3.6 and 13.2 per 100,000 persons annually, increasing in all age groups.3–5 This trend mirrors what has been observed in adults.6–8 These trends have been linked to greater clinical awareness, increased diagnostic testing, and rising prevalence of obesity. In 2012, AP was identified as the number one cause of hospitalization for gastrointestinal diseases in the U.S., costing an estimated $2.6 billion in inpatient costs.9 Beyond its direct monetary impact, pancreatitis has a substantial negative impact on the quality of life of children and adults.10
Previous population studies examining the epidemiology of pancreatitis have used inpatient databases to determine the incidence and prevalence of AP and CP. While the majority of individuals with AP are admitted, those with mild cases may be managed in the outpatient setting. In fact, one study reported that 23% of children with AP were discharged home from the Emergency Department (ED).11 Thus, inpatient data samples do not completely capture all individuals with AP. For CP, this disparity may be even larger, with many individuals primarily receiving outpatient care. To increase the accuracy of epidemiological estimates for AP and CP, examination of both inpatient and outpatient medical services is necessary.
Accurate epidemiological estimates of AP and CP are important in shaping the medical care of this disease. Health care resource allocation, federal and private research funding, and medical provider training priorities are all influenced by disease occurrence. Thus, to provide comprehensive and current epidemiology of pancreatitis in the U.S., we examined the incidences and prevalence of AP and CP in a nationwide employer-based insurance claims database containing inpatient and outpatient encounters. The secondary aim of our study was to perform sub-analysis examining only inpatient data to compare our results to prior studies. Our results provide current epidemiological trends in AP and CP and will help shape the national narrative on pancreatic disease in the U.S.
METHODS
Data source
The data originated from the Truven Health MarketScan Commercial Claims and Encounters (CCAE) database, a subset of the Truven MarketScan Research Database. The CCAE database consists of de-identified outpatient, inpatient, and pharmaceutical claims of approximately 40–50 million enrollees with employer-sponsored coverage each year. Patients in this database include active employees, early retirees, COBRA (Consolidated Omnibus Budget Reconciliation Act) continuees and dependents of ages 0–64 years from all 50 states of the U.S. We analyzed the annual enrollment, inpatient and outpatient claims from 2007–2014.
Participants
Inclusion criteria were enrollees with a diagnosis of AP (ICD-9 577.0) or CP (ICD-9 577.1) between 2007-2014. Four diagnosis codes were reviewed for each line item of both inpatient and outpatient encounters. Data was aggregated from the item line level such that, on any given service date, a patient could have one or more diagnoses of AP and/or CP. Patients were defined as having AP or CP based on the AP or CP diagnosis for that service date. Patients who had both CP and AP diagnoses on the same service date could not be classified concretely and were omitted from the analysis. This resulted in the loss of 0.4% from the original cohort (1,741 patients; 97% adults (0.4% adult cohort) and 3% children (0.4% pediatric cohort)). Years are calculated as the year of the service date. The remaining cohort of patients with AP or CP contained 426,604 people (Figure 1).
Figure 1. Determination of Pediatric and Adult Acute and Chronic Pancreatitis Cohorts.
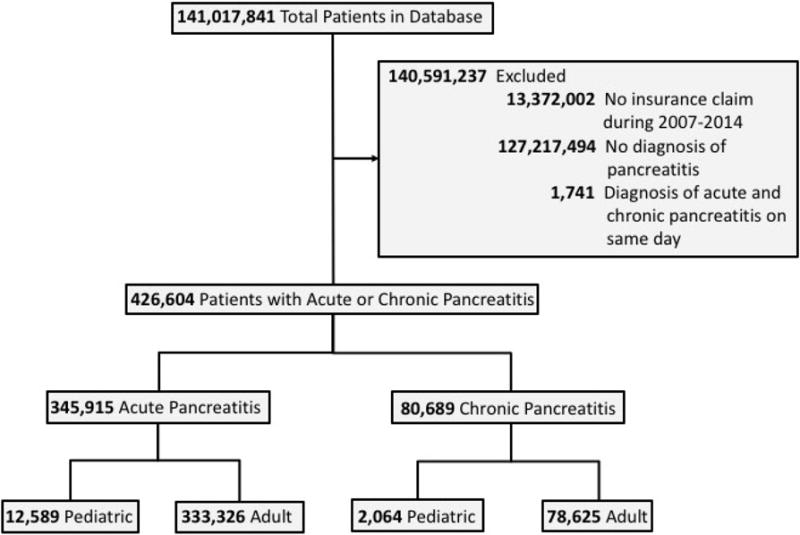
Outpatient and inpatient encounters from 2007–2014 were used from the Truven Health MarketScan Commercial Databases. Using both databases resulted in a total of 141,017,841 unique patients. Patients with AP or CP were identified by their respective ICD-9 diagnosis codes. A subset of patients had dual AP and CP codes on the same day. These represented 0.4% of the pancreatitis cohort and were excluded. These cohorts were further divided into pediatric or adult groups based on age at time of diagnosis.
Design
The cohort was divided into four groups: pediatric AP, pediatric CP, adult AP, and adult CP. Pediatric groups were defined by INSPPIRE criteria,12 with the first episode of AP or CP at 18 years or younger. The adult groups were defined as being 19 to 64 years.
Outcome Measures
The main outcome measures were incidence and prevalence. Incidence was calculated as the number of patients with AP or CP who had not previously been diagnosed as such. The incidence date was determined by the first service date (inpatient or outpatient) with a diagnosis of AP or CP. Incidence rate per year was calculated as the number of patients with their first diagnosis in a given year divided by the number of patients enrolled in the database for that year. Prevalence for CP was calculated as the number of patients with CP prior to a given year divided by the number of patients enrolled in that given year.
Statistical analysis
Comparison of descriptive data between pediatric and adult cohorts was done with STATA using Student’s T-Test. The significance of regression lines was performed with a linear Pearson analysis using SigmaPlot 11. Significance was determined by P<0.05.
RESULTS
Cohort
From 2007-2014, there were 141,017,841 unique patients in the database, with 113,653,591 patients having outpatient encounters and 13,992,248 with inpatient encounters (Figure 1). Patient data came from all 50 states (Figure 2). There was near equal gender distribution (53% female, 47% male) across all years; ages ranged from 0–64 years. Approximately 26.2% of data came from patients 18 years or younger, with 73.8% from those 19 to 64 years. Within the database, AP or CP occurred in 426,604 patients, with 309,436 of those having an outpatient diagnosis and 201,184 an inpatient diagnosis. From this cohort, 14,653 pediatric and 411,951 adult patients had a diagnosis of AP or CP (Table 1). Of those with AP, 12.0% of children and 14.3% of adults went on to have a diagnosis of CP during the study period.
Figure 2. Geographical Distribution of Persons in the Truven Health MarketScan Commercial Databases in the United States in 2014.
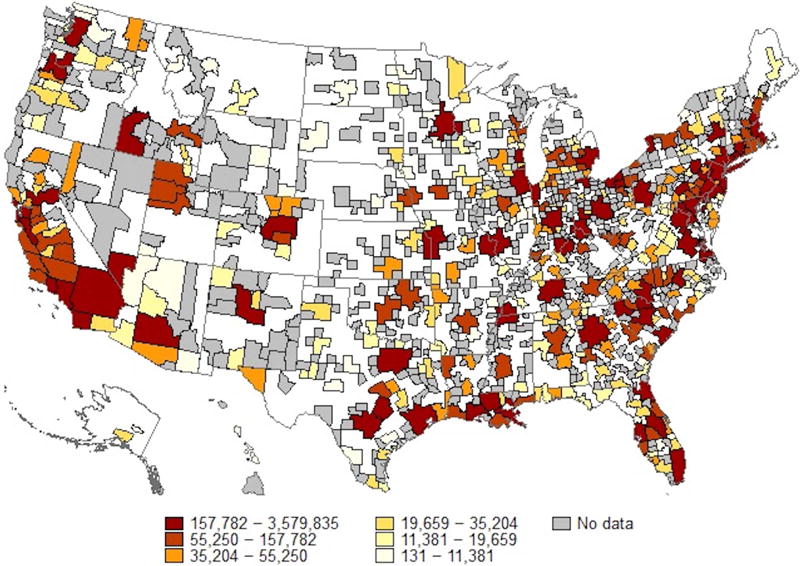
Each color represents the number of persons in the database that are located within each of the defined metropolitan statistical areas (MSA) in 2014. White regions represent rural areas where patients may have been present, but no MSA information exists, whereas grey regions represent places without patient representation in the database in 2014.
Table 1.
Demographics of Pediatric and Adult Pancreatitis Cohorts
| Pediatric | Adult | |||
|---|---|---|---|---|
| Acute Pancreatitis | Chronic Pancreatitis | Acute Pancreatitis | Chronic Pancreatitis | |
| Unique Patients | 12,589 | 2,064 | 333,326 | 78,625 |
| Mean Medical Patient (SD) Visits Per | ||||
| Outpatient | 30.8 (65.0)* | 58.4 (105.6)* | 41.5 (68.7)* | 63.6 (81.8)* |
| Inpatient | 4.5 (12.6)* | 2.6 (11.3)* | 2.9 (6.0)* | 1.4 (6.2)* |
| Mean AP or Visits (SD) CP-Associated | ||||
| Outpatient | 2.2 (13.7) | 7.5 (16.2)* | 2.1 (6.2) | 5.9 (12.8)* |
| Inpatient | 2.1 (4.1)* | 1.3 (4.2)* | 1.9 (3.6)* | 0.7 (3.3)* |
| Mean Length Stay (days) of | 4.5 (13.3)* | 2.7 (6.8)* | 2.6 (6.4)* | 1.4 (6.7)* |
| Mean Age (years) at Diagnosis | 13.4 (4.6) | 13.0 (4.6) | 46.9 (11.8) | 48.5 (11.6) |
| Gender (%) | ||||
| Female | 55% | 55% | 53% | 51% |
| Male | 45% | 45% | 47% | 49% |
| Geographic Region (%) | ||||
| Northeast | 17% | 18% | 18% | 18% |
| North Central (Midwest) | 23% | 22% | 23% | 23% |
| South | 38% | 36% | 41% | 40% |
| West | 19% | 21% | 16% | 16% |
| Unknown | 3% | 3% | 3% | 3% |
| Insurance Type (%) | ||||
| Comprehensive | 1% | 1% | 2% | 3% |
| EPO/PPO | 65% | 65% | 65% | 66% |
| HMO | 14% | 13% | 12% | 11% |
| POS (+/− capitation) | 7% | 7% | 8% | 8% |
| CDHP/HDHP | 7% | 7% | 6% | 6% |
| Other | 6% | 7% | 7% | 6% |
, P< 0.05 comparing Pediatric vs. Adult by Student’s T-test.
AP Incidence
Using these pediatric and adult cohorts, we calculated longitudinal incidences for AP. In adults, AP decreased over time (P=0.044), dropping from 123.7/100,000 persons in 2007 to 111.2/100,000 persons in 2014. In children, there was a steady incidence of AP, ranging from 11.6 to 13.5/100,000 persons per year, with the 2014 incidence being 12.3/100,000 persons (Figure 3A). Given the decline in adult AP incidence, we calculated AP incidence as a function of age to determine if this decline occurred equally at all ages, or was specific to a defined group. AP incidence became greater with advancing age (P<0.0001); it was low and stable during the first decade of life and increased thereafter. The downtrend in AP incidence between 2007 and 2014 was a result of decreased incidence amongst older individuals (Figure 3B).
Figure 3. Trends in the Incidence of Pediatric and Adult Acute Pancreatitis from 2007–2014.
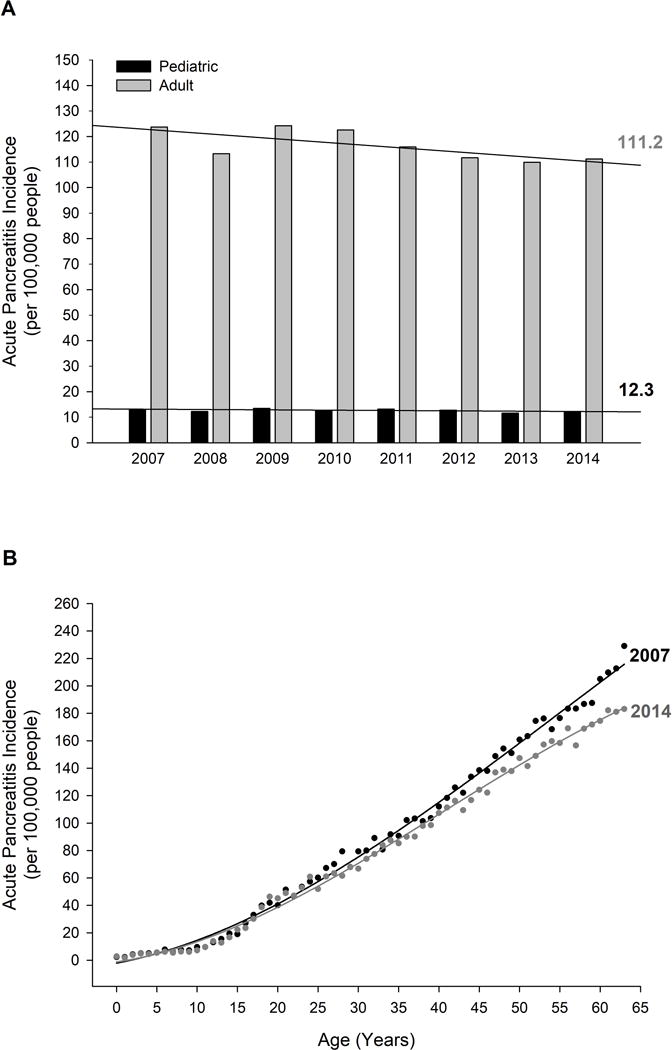
A. Incidence of pediatric (black) or adult (grey) AP for each year from 2007–2014. Lines represent regression trend lines for each group with the incidence for 2014 represented in text. B. Comparison of AP incidence by age between 2007 (black) and 2014 (grey). Circles represent incidence for each age, with the line being the best fit regression line.
To compare our results with prior studies, which only examined inpatient admissions, we performed two separate analyses using only inpatient admissions with AP. In adults, the incidence of AP admission decreased from 65.1/100,000 persons in 2007 to 60.1/100,000 persons in 2014, although this was non-significant over the entire time (P=0.146). However, between 2010–2014, there was a clear and significant decline (P=0.004) (Supplemental Figure 1A). In children, the incidence of AP admission was similar between 2007–2014, ranging from 6.2–7.1/100,000 persons, with a 2014 incidence of 6.4/100,000 persons. Others have also examined AP incidence by measuring the number of inpatient AP admissions from total hospital admissions. In adults, there was a near-significant increasing trend (P=0.055) in AP hospital admissions from 2007-2014, ranging from 291.9-309.3/100,000 admissions. Pediatric AP admissions were similar from 2007-2014, ranging from 40.2-50.3/100,000 admissions, with an incidence of AP admissions amongst all hospital admissions of 42.7/100,000 admissions in 2014 (Supplemental Figure 1B).
CP Incidence and Prevalence
Subsequently, we calculated incidences and prevalence for pediatric and adult CP. As seen in Figure 4A, the incidence of CP in adults significantly decreased from 2007–2014 (P=0.006), with an incidence of 31.7/100,000 persons in 2007 versus 24.7/100,000 persons in 2014. The prevalence of adult CP in 2014 was 91.9/100,000 persons. Similarly, the incidence of pediatric CP significantly decreased from 2007–2014 (P=0.010), decreasing from 2.2–1.9/100,000 persons. Pediatric CP prevalence was 5.8/100,000 persons in 2014 (Figure 4A). Given the decline in CP incidence amongst both children and adults, we calculated age-specific CP incidences. Similar to AP, CP began to steadily increase in the second decade of life and increased with advancing age (P<0.0001). Likewise, the greatest differences in CP incidence between 2007 and 2014 occurred at the most advanced ages (Figure 4B).
Figure 4. Trends in the Incidence of Pediatric and Adult Chronic Pancreatitis from 2007–2014.
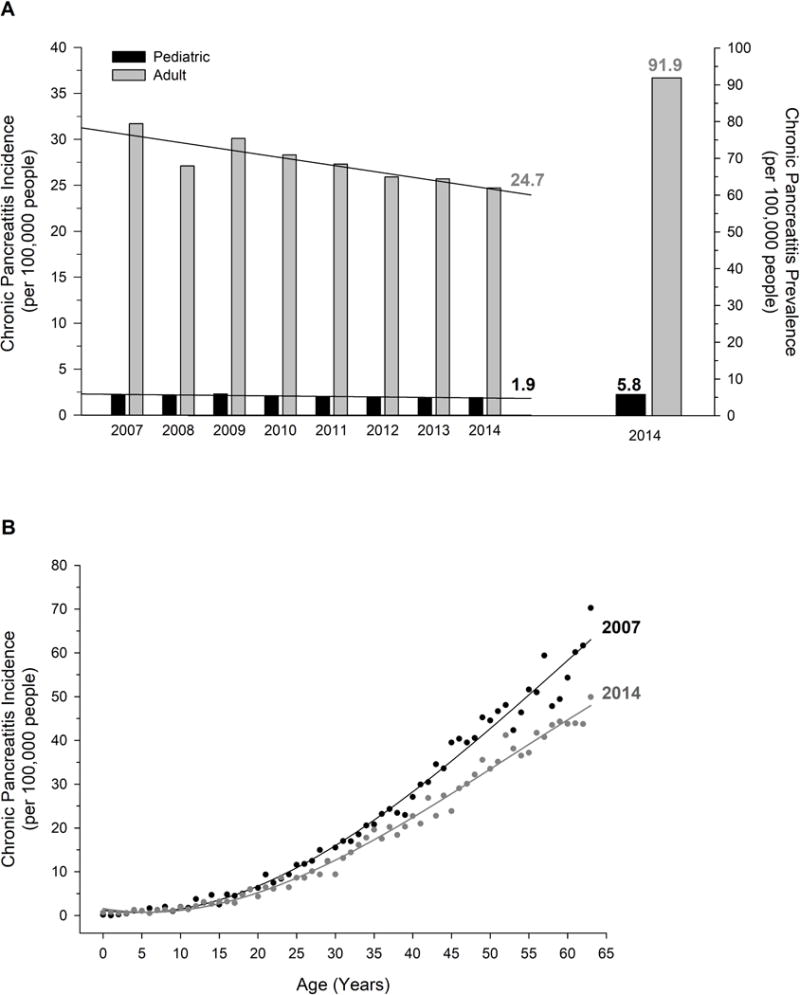
A. Left: Incidence of pediatric (black) or adult (grey) CP for each year from 2007–2014. Lines represent regression trend lines for each group with the incidence for 2014 represented in text. Right: Prevalence of (black) and adult (grey) CP in 2014. B. Comparison of CP incidence by age between 2007 (black) and 2014 (grey). Circles represent incidence for each age, with the line being the best fit regression line.
Similar to AP, we performed a separate analysis of CP incidence using inpatient admissions amongst the general population of total admissions. From 2007-2014, the incidence of adult CP admissions decreased significantly (P=0.046), changing from 7.4/100,000 persons in 2007 to 6.1/100,000 persons in 2014. This decreasing trend was even more prominent from 2009–2014 (P=0.0002). The incidence of pediatric CP admissions ranged from 0.5–0.9/100,000 persons, with a 2014 incidence of 0.5/100,000 persons. This was not significantly different across the entire time period (P=0.632), but was from 2009–2014 (P=0.006) (Supplemental Figure 2A). Analysis of the number of CP admissions amongst all inpatient admissions showed similar trends for both children and adults (Supplemental Figure 2B). The incidence of CP amongst all admissions was 3.5–5.8/100,000 admissions in children (3.5/100,000 in 2014) and 32.7–36.9/100,000 admissions in adults (31.2/100,000 in 2014). These changes were not significant in the pediatric (P=0.429) or adult cohorts (P=0.197). In contrast, there was a significant decline in both pediatric (P=0.009) and adult (P=0.001) CP admissions amongst all hospitalizations during 2009-2014.
DISCUSSION
Over the last several decades multiple studies have examined the occurrence of pancreatitis. However, to date, all epidemiological studies performed in the U.S. have relied solely on inpatient databases. Hospital admission with AP is common due to typical symptoms of anorexia, dehydration, and refractive nausea and pain. Additionally, when nil per os was the mainstay treatment for AP, hospital admission was necessary. However, in the current era of early enteral feeding with pancreatitis, patients with mild cases who can tolerate oral hydration and pain control may be managed as outpatients. A recent Pediatric ED study found that 23% of children with AP were discharged home.13 The problem becomes larger for CP, where the management of chronic pain and nutrition primarily occur in the outpatient setting. Our study is the first to utilize nationwide inpatient and outpatient databases to calculate the incidences and prevalence of AP and CP in the U.S., resulting in increased accuracy of pancreatitis epidemiology.
Acute Pancreatitis
From our comprehensive epidemiological analysis, we found that the incidence of AP was 12.3/100,000 persons in children and 111.2/100,000 persons in non-elderly adults in 2014. Similar to prior studies,2, 14 we observed age-dependent increase in AP, with an increase in incidence occurring at about 10 years of age. We found adult AP to be higher than previously reported. Using only inpatient admissions, Frey et al.15 and Yadav et al.16 estimated AP incidence to be 38.1 and 58.2/100,000 persons, respectively. Our sub-analysis with inpatient admissions resulted in an AP incidence of 60.1/100,000 adults, similar to these prior reports. The inclusion of outpatient encounters likely allowed us to identify individuals with mild, self-limiting AP, managed in an outpatient setting, which may occur in as much as 50% of cases.17
Most pediatric pancreatitis studies report the absolute number of cases in a hospital or region. Until recently, the only other study to calculate population incidence was that by Morinville et al., who reported the number of AP admissions at a single pediatric tertiary care center divided by the estimated hospital catchment area. With this, they found an incidence of 13.2/100,000 children in 2004.18 Recently, Hornung et al. performed a similar study, except examining AP admissions from 2010-2014. They reported an estimated pediatric AP incidence of 6.6/100,000 children in 2014.19 Using inpatient admissions, we found an incidence of pediatric AP to be 6.4/100,000 in 2014, mirroring that of Hornung et al. Since the 1990s and early 2000s, there has been increased awareness about the development of pancreatitis in children (as evidenced by rising amylase and lipase testing18, 20); providers outside of tertiary care academic centers are becoming increasingly comfortable caring for children with uncomplicated AP. Between 2006 and 2011, about half of all ED visits for pediatric AP were at non-teaching hospitals.13 Therefore, it is possible that the Morinville et al. dataset included a concentration of cases due to referral center bias, leading to an overestimation of pediatric AP incidence.
Over the last several decades, the consensus from many epidemiological studies has been that the incidence of adult AP is rising. We are the first to report a decrease in AP incidence, however, others have noted a recent stabilization in AP incidence. There is little data post-2010, but Munigala et al. observed a stabilization in AP hospital discharges from 2009 to 2010, after a steady increase since 1983.21 Likewise, Krishna et al. found minimal change in AP hospital admissions from 2010-2012.22 Many epidemiological studies report AP incidence as the number of AP admissions (discharges) divided by total admissions (discharges), with the outcome being percent AP admissions (discharges). This may reflect actual incidence of AP, but may also be influenced by provider admission practices. In fact, when we looked at the number of AP admissions per 100,000 admissions, we found a near-significant increasing trend in AP admissions, similar to prior studies.
Amongst adults, the number one and two causes for AP are gallstones and alcohol use, respectively. In Allegheny County (Pennsylvania), Yadav et al. showed that gallstone disease constitutes an increasing proportion of AP with advancing age.16 Krishna et al. reported a decrease in the odds ratio of gallstone-related AP in the U.S. between 2002-2005 and 2009-2012.22 Likewise, there was a decrease in biliary procedures performed in the U.S. from 1998-2013.23 With all major U.S. gastroenterological and pancreatology societies advocating for cholecystectomy on index admission (or soon after) for biliary pancreatitis,24–28 a drop in biliary-related AP admissions is expected. The contribution from alcohol consumption is more difficult to interpret. Alcohol consumed per capita in the U.S. has fluctuated over time, dramatically increasing from the 1930s to the early 1980s, declining during the 1980s and early 1990s, and then increasing again from the late 1990s. Since then, the amount of alcohol intake per capita in the U.S. has remained relatively stable. In 2007, per capita ethanol consumption was 2.31 gallons, compared to 2.32 gallons in 2014.29 So, while the last several decades showed an increasing trend in AP, due to changes in risk factors associated with AP, we may now see a stabilization, and even decrease, in this trend.
We did not observe a decrease in pediatric AP. However, it is notable that we also did not see an increase, as previously reported from 1993-2004.18 Rising rates of pediatric AP have been attributed to increasing childhood obesity (thereby increasing gallstone formation), but have also been hypothesized to be related to increased awareness of pediatric pancreatitis.18, 20 While the prevalence of childhood obesity significantly increased from 1999–2014 (13.9% to 17.2%), it remained stable from 2003–2014 (17.1% to 17.2%).30 We are not the only ones to suggest a change in the rising trends of pediatric AP in the U.S. Pant et al. observed a stabilization in pediatric AP-associated ED visits from 2006–201113 and Hornung et al. found no change in pediatric AP admissions at a large, tertiary care pediatric hospital from 2010–2014.19
Chronic Pancreatitis
We found a markedly higher incidence of CP in non-elderly adults than what was previously reported by Yadav et al. in Olmsted County (Minnesota) (4.35/100,000 persons from 1997-2006).31 The discrepancy could be due to our larger patient sample (106 vs. 80,689 cases), differing racial demographics (~86% vs. ~72% White in the U.S.32), or the ability of Yadav et al. to verify a correct diagnosis of CP with actual patient data (as opposed to our reliance on diagnosis coding). However, when examining only inpatient admissions for the entire population, we found a similar CP incidence in 2014 at 6.1/100,000 persons, suggesting that our higher incidence is likely due to the inclusion of outpatient encounters. Given the interrelationship between AP and CP,33 it is not surprising that we also found a decrease in the incidence of CP, although the degree of decline was larger than AP. Alcohol and smoking are the primary identifiable causes of CP in adults. Alcohol use, often accompanied by cigarette smoking, is by itself a risk factor for CP, but together with smoking, imparts an even greater risk. The prevalence of smoking in the U.S. decreased by an estimated 13% between 2007 and 2012, with an associated increase in individuals undertaking smoking cessation.34
We also found the incidence of pediatric CP to be greater than previously reported. There are few population-based studies on CP in children, but both Yadav et al. (0-34 years-old) and Spanier et al. (<20 years-old) found an incidence of 0.5/100,000 persons in Olmsted County and the Netherlands, respectively.7, 31 When we examined the incidence of inpatient admission for CP amongst our total national cohort, we found the incidence of pediatric CP to be similar at 0.5/100,000 children in 2014. Thus, the discrepancy in our studies is likely attributable to our use of outpatient data which, as indicated earlier, is where most CP management occurs. Like adult disease, pediatric CP also showed a statistically significant decrease, although this was numerically less impressive (2.2 to 1.9/100,000 persons). With genetic causes responsible for nearly 75% of pediatric CP cases,35 there is likely to be minimal variation in CP incidence. With the continuum disease model,33 improvements in recurrent AP (RAP) management is expected to decrease the progression of RAP to CP. With our inability to accurately determine RAP from ICD-9 coding, we cannot comment on trends in RAP, however, ongoing longitudinal epidemiological studies on RAP and CP in children and adults should shed light on this.
Limitations
The inherent limitation in the use of a de-identified database is the inability to verify accurate diagnosis coding. This is especially difficult with AP and CP, given that individuals can meet Cambridge criteria for CP and continue to experience AP episodes. This is also problematic when coding for RAP since it is not clearly defined within ICD-9 coding. In ICD-9-CM Sixth Edition, “577.0 Acute Pancreatitis” includes “Pancreatitis: acute (recurrent)”, while “577.1 Chronic Pancreatitis” includes “Pancreatitis: recurrent” and “Pancreatitis: relapsing.” Coding RAP as CP would lead to an overestimation of CP in our study.
While our cohort was a nationwide sample, it did not include those 65 years or older, on Medicaid, or those on non-employer-based insurance plans. Using an employer-based insurance database captures the largest group of individuals in the U.S. under 65 years-old (2014: 47% of children, 59% of adults).36 However, Medicaid makes up the second largest insured group of non-elderly at 22%.36 This sampling bias may be more profound for pediatric pancreatitis where, despite accounting for only 30% of the population, more children were enrolled in Medicaid than adults in 2014 (34,805,500 vs. 27,417,700).37 Additionally, disability and unemployment in CP patients, which was reported to be 27.1% in the NAPS2 study (North American Pancreatitis Study 2),38 may result in increased reliance on Medicaid and/or disability Medicare, leading to an underestimation in the prevalence of CP in our study. With the increasing incidence of AP and CP with advancing age, the omission of individuals 65 years or older also leads to an underestimation in the incidence and prevalence of adult pancreatitis. Future work combining employer-based insurance, Medicaid, and Medicare databases would provide even more thorough coverage and further increase the accuracy of the incidence of pancreatitis in the U.S.
Conclusion
We have provided a comprehensive and current epidemiological analysis of AP and CP in the U.S. for privately insured children and non-elderly adults. With changing human health behaviors and advances in pancreatitis clinical management, we have observed a stabilization, and even a decrease, in the incidences of AP and CP. Despite falling incidences, due to decreased mortality, the prevalence of CP is increasing and CP remains a substantial burden on patients, families, and the U.S. healthcare system.22 Ongoing research into the pathophysiology and management of pancreatitis in children and adults will continue the positive trends in decreasing pancreatic disease.
Supplementary Material
Acknowledgments
Data for this project were accessed using the Stanford Center for Population Health Sciences (PHS) Data Core. The PHS Data Core is supported by a National Institutes of Health (NIH) National Center for Advancing Translational Science Clinical and Translational Science Award (UL1 TR001085) and from Internal Stanford funding. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
We would like to thank Aditi Gupta, MS and Robert Doxey, BS for organizational help with preliminary data analysis, and Walter Park, MD for manuscript review. Funding sources include the Cystic Fibrosis Foundation (SELLER16L0 to Z.M.S.), Stanford University (Women and Sex Differences in Medicine Seed Grant to C.K.), and National Institute of Diabetes and Digestive and Kidney Diseases (DK094868 to K.T.P.).
Grant Support: Funding sources include the Cystic Fibrosis Foundation (SELLER16L0 to Z.M.S.), Stanford University (Women and Sex Differences in Medicine Seed Grant to C.K.), and National Institute of Diabetes and Digestive and Kidney Diseases (DK094868 to K.T.P.).
Abbreviations
- AP
acute pancreatitis
- CP
chronic pancreatitis
- RAP
recurrent acute pancreatitis
- US
United States
- ED
Emergency Department
- ICD-9
International Classification of Diseases
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures: The authors have nothing to disclose.
Author Contributions:
Zachary M. Sellers, MD, PhD: study concept and design, analysis and interpretation of data, statistical analysis, drafting of the manuscript, study supervision.
Donna MacIsaac, MA: acquisition of data, statistical analysis.
Helen Yu, BS: acquisition of data, statistical analysis.
Melody Dehghan, BS: acquisition of data, statistical analysis.
Ke-You Zhang, MD: study concept and design, critical revision of the manuscript for important intellectual content.
Rachel Bensen, MD, MPH: critical revision of the manuscript for important intellectual content.
Jessie J. Wong, PhD: critical revision of the manuscript for important intellectual content.
Cindy Kin, MD, MS: critical revision of the manuscript for important intellectual content, obtained funding.
KT Park, MD, MS: study concept and design, critical revision of the manuscript for important intellectual content, obtained funding, study supervision.
References
- 1.Global Burden of Disease Study C. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;386:743–800. doi: 10.1016/S0140-6736(15)60692-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yadav D, Lowenfels AB. The epidemiology of pancreatitis and pancreatic cancer. Gastroenterology. 2013;144:1252–61. doi: 10.1053/j.gastro.2013.01.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Park A, Latif SU, Shah AU, et al. Changing referral trends of acute pancreatitis in children: A 12-year single-center analysis. J Pediatr Gastroenterol Nutr. 2009;49:316–22. doi: 10.1097/MPG.0b013e31818d7db3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lopez MJ. The changing incidence of acute pancreatitis in children: a single-institution perspective. J Pediatr. 2002;140:622–4. doi: 10.1067/mpd.2002.123880. [DOI] [PubMed] [Google Scholar]
- 5.Sanchez-Ramirez CA, Larrosa-Haro A, Flores-Martinez S, et al. Acute and recurrent pancreatitis in children: etiological factors. Acta Paediatr. 2007;96:534–7. doi: 10.1111/j.1651-2227.2007.00225.x. [DOI] [PubMed] [Google Scholar]
- 6.Yadav D, Lowenfels AB. Trends in the epidemiology of the first attack of acute pancreatitis: a systematic review. Pancreas. 2006;33:323–30. doi: 10.1097/01.mpa.0000236733.31617.52. [DOI] [PubMed] [Google Scholar]
- 7.Spanier B, Bruno MJ, Dijkgraaf MG. Incidence and mortality of acute and chronic pancreatitis in the Netherlands: a nationwide record-linked cohort study for the years 1995–2005. World J Gastroenterol. 2013;19:3018–26. doi: 10.3748/wjg.v19.i20.3018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zheng Y, Zhou Z, Li H, et al. A multicenter study on etiology of acute pancreatitis in Beijing during 5 years. Pancreas. 2015;44:409–14. doi: 10.1097/MPA.0000000000000273. [DOI] [PubMed] [Google Scholar]
- 9.Peery AF, Dellon ES, Lund J, et al. Burden of gastrointestinal disease in the United States: 2012 update. Gastroenterology. 2012;143:1179–87. e1–3. doi: 10.1053/j.gastro.2012.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pezzilli R, Bini L, Fantini L, et al. Quality of life in chronic pancreatitis. World J Gastroenterol. 2006;12:6249–51. doi: 10.3748/wjg.v12.i39.6249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pant C, Deshpande A, Olyaee M, et al. Epidemiology of acute pancreatitis in hospitalized children in the United States from 2000-2009. PLoS One. 2014;9:e95552. doi: 10.1371/journal.pone.0095552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Morinville VD, Husain SZ, Bai H, et al. Definitions of pediatric pancreatitis and survey of present clinical practices. J Pediatr Gastroenterol Nutr. 2012;55:261–5. doi: 10.1097/MPG.0b013e31824f1516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pant C, Deshpande A, Sferra TJ, et al. Emergency department visits for acute pancreatitis in children: results from the Nationwide Emergency Department Sample 2006-2011. J Investig Med. 2015;63:646–8. doi: 10.1097/JIM.0000000000000154. [DOI] [PubMed] [Google Scholar]
- 14.Roberts SE, Morrison-Rees S, John A, et al. The incidence and aetiology of acute pancreatitis across Europe. Pancreatology. 2017;17:155–165. doi: 10.1016/j.pan.2017.01.005. [DOI] [PubMed] [Google Scholar]
- 15.Frey CF, Zhou H, Harvey DJ, et al. The incidence and case-fatality rates of acute biliary, alcoholic, and idiopathic pancreatitis in California, 1994–2001. Pancreas. 2006;33:336–44. doi: 10.1097/01.mpa.0000236727.16370.99. [DOI] [PubMed] [Google Scholar]
- 16.Yadav D, O’Connell M, Papachristou GI. Natural history following the first attack of acute pancreatitis. Am J Gastroenterol. 2012;107:1096–103. doi: 10.1038/ajg.2012.126. [DOI] [PubMed] [Google Scholar]
- 17.Richter JM. Management of Pancreatitis. In: Goroll AH, Mulley AG, editors. Primary Care Medicine: Office Evaluation and Management of the Adult Patient. Sixth. Philadelphia, PA: Lippincott Williams & Wilkins; 2009. pp. 578–581. [Google Scholar]
- 18.Morinville VD, Barmada MM, Lowe ME. Increasing incidence of acute pancreatitis at an American pediatric tertiary care center: is greater awareness among physicians responsible? Pancreas. 2010;39:5–8. doi: 10.1097/MPA.0b013e3181baac47. [DOI] [PubMed] [Google Scholar]
- 19.Hornung L, Kalkwarf HJ, Szabo FK, et al. 48th Meeting of the American Pancreatic Association. Vol. 46. San Diego, CA: Pancreas; 2017. Stabilized Incidence of Pediatric Acute Pancreatitis; pp. 1386–1448. [DOI] [PubMed] [Google Scholar]
- 20.Oracz G, Wejnarska K, Kolodziejczyk E, et al. Pediatric Acute and Chronic Pancreatitis: Increase in Incidence or Increasing Awareness? Pancreas. 2017;46:e55–e56. doi: 10.1097/MPA.0000000000000821. [DOI] [PubMed] [Google Scholar]
- 21.Munigala S, Yadav D. Case-fatality from acute pancreatitis is decreasing but its population mortality shows little change. Pancreatology. 2016;16:542–50. doi: 10.1016/j.pan.2016.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Krishna SG, Kamboj AK, Hart PA, et al. The Changing Epidemiology of Acute Pancreatitis Hospitalizations: A Decade of Trends and the Impact of Chronic Pancreatitis. Pancreas. 2017;46:482–488. doi: 10.1097/MPA.0000000000000783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Huang RJ, Thosani NC, Barakat MT, et al. Evolution in the utilization of biliary interventions in the United States: results of a nationwide longitudinal study from 1998 to 2013. Gastrointest Endosc. 2017 doi: 10.1016/j.gie.2016.12.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tenner S, Baillie J, DeWitt J, et al. American College of Gastroenterology guideline: management of acute pancreatitis. Am J Gastroenterol. 2013;108:1400–15. doi: 10.1038/ajg.2013.218. 1416. [DOI] [PubMed] [Google Scholar]
- 25.Forsmark CE, Baillie J, Practice AGAIC et al. AGA Institute technical review on acute pancreatitis. Gastroenterology. 2007;132:2022–44. doi: 10.1053/j.gastro.2007.03.065. [DOI] [PubMed] [Google Scholar]
- 26.Crockett SD, Wani S, Gardner TB, et al. American Gastroenterological Association Institute Guideline on Initial Management of Acute Pancreatitis. Gastroenterology. 2018 doi: 10.1053/j.gastro.2018.01.032. [DOI] [PubMed] [Google Scholar]
- 27.Working Group IAPAPAAPG. IAP/APA evidence-based guidelines for the management of acute pancreatitis. Pancreatology. 2013;13:e1–15. doi: 10.1016/j.pan.2013.07.063. [DOI] [PubMed] [Google Scholar]
- 28.Abu-El-Haija M, Kumar S, Quiros JA, et al. The Management of Acute Pancreatitis in the Pediatric Population: Clinical Report from the NASPGHAN Pancreas Committee. Journal of Pediatric Gastroenterology and Nutrition. 2017 doi: 10.1097/MPG.0000000000001583. [DOI] [PubMed] [Google Scholar]
- 29.Haughwout S, Slater M. Apparent Per Capita Alcohol Consumption: National, State, and Regional Trends, 1977–2015. 2017 [Google Scholar]
- 30.Ogden CL, Carroll MD, Fryar CD, et al. PRevalence of Obesity Among Adults and Youth: United States, 2011–2014. 2015 [PubMed] [Google Scholar]
- 31.Yadav D, Timmons L, Benson JT, et al. Incidence, prevalence, and survival of chronic pancreatitis: a population-based study. Am J Gastroenterol. 2011;106:2192–9. doi: 10.1038/ajg.2011.328. [DOI] [PubMed] [Google Scholar]
- 32.United States Census Bureau QuickFacts. Race and Hispanic Origin [Google Scholar]
- 33.Whitcomb DC, Frulloni L, Garg P, et al. Chronic pancreatitis: An international draft consensus proposal for a new mechanistic definition. Pancreatology. 2016;16:218–24. doi: 10.1016/j.pan.2016.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pernenkil V, Wyatt T, Akinyemiju T. Trends in smoking and obesity among US adults before, during, and after the great recession and Affordable Care Act roll-out. Prev Med. 2017;102:86–92. doi: 10.1016/j.ypmed.2017.07.001. [DOI] [PubMed] [Google Scholar]
- 35.Kumar S, Ooi CY, Werlin S, et al. Risk Factors Associated With Pediatric Acute Recurrent and Chronic Pancreatitis: Lessons From INSPPIRE. JAMA Pediatr. 2016;170:562–9. doi: 10.1001/jamapediatrics.2015.4955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Health Insurance Coverage of Nonelderly 0-64. 2014 [Google Scholar]
- 37.Medicaid Enrollees by Enrollment Group. 2014 [Google Scholar]
- 38.Machicado JD, Amann ST, Anderson MA, et al. Quality of Life in Chronic Pancreatitis is Determined by Constant Pain, Disability/Unemployment, Current Smoking, and Associated Co-Morbidities. Am J Gastroenterol. 2017;112:633–642. doi: 10.1038/ajg.2017.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


