Abstract
The scarce research on the effects of moderate alcohol consumption on mental health among older adults suggests a protective effect against depression. We prospectively examined the association between patterns of moderate alcohol consumption, depression and psychological distress, using information from 5,299 community-dwelling older adults from the ELSA and Seniors-ENRICA cohorts. A Mediterranean drinking pattern (MDP) was defined as moderate alcohol intake (<40 g/day for men; <24 g/day for women) with a preference for wine and drinking only with meals. Depression was ascertained with the 10-item Geriatric Depression Scale (GDS-10), a self-report of clinically-diagnosed depression, or being on anti-depressant medication (Seniors-ENRICA); and with the 8-item Center for Epidemiologic Studies Depression Scale (CES-D) (ELSA). Psychological distress was assessed with the General Health Questionnaire-12 (GHQ-12). Compared to never drinkers, moderate drinkers showed comparable scores on the ENRICA-GDS-10 (PRR (95%CI): 1.03 (0.84–1.26)), the ENRICA-GHQ-12 (0.88 (0.73–1.06)), the ELSA-CES-D (0.92 (0.79–1.06)) and the ELSA-GHQ-12 (0.75 (0.55–1.01). The MDP was not associated with the GDS-10 or GHQ-12 scores, or with clinically-diagnosed depression; however drinkers with a preference for wine showed an increased number of psychological distress symptoms (1.31 (1.03–1.66)). In conclusion, we found no consistent protective association between moderate alcohol consumption and depression in older adults.
Introduction
Among older adults, depression is the most common mental illness1. According to the Global Burden of Disease Study, in 2015 the number of Disability Adjusted Life Years (DALYs) for depressive disorders in older adults ranged from 750 per 100,000 among those aged 80 and over to 1050 per 100,000 among those aged 60–652. Depression in these age groups frequently coexists with other chronic diseases, cognitive impairment, and psychosocial problems (i.e., isolation or economic impoverishment). Moreover, depression in older adults is associated with a higher use of healthcare services3, and is a risk factor of physical function limitations4, suicide5, and premature mortality6,7.
Heavy alcohol consumption significantly contributes to the burden of disease in many countries8. Major illnesses associated with alcohol intake include cancers (e.g., malignancies in the oral cavity, pharynx, larynx, esophagus, liver, colon, rectum, female breast)9, cardiovascular diseases (e.g., hypertension, hemorrhagic stroke, atrial fibrillation)8, and gastrointestinal conditions (e.g., alcoholic hepatitis, cirrhosis, pancreatitis)10. Nevertheless, moderate alcohol consumption has been associated with a reduction of some health risks; for instance, compared to non- drinkers, moderate alcohol drinkers display a reduced risk of coronary artery disease11, ischemic stroke11, heart failure11, and type 2 diabetes12.
A large body of research has traditionally documented the deleterious relationship between alcohol abuse and depression13. However, studies have seldom examined the psychological and mental health effects of light to moderate alcohol consumption, and the scarce longitudinal reports have rendered inconsistent results14–19. Thus, the main objective of this work was to examine the prospective association between moderate alcohol intake and depression or psychological distress in two cohorts of community-dwelling older adults: the Seniors-ENRICA (Study on Nutrition and Cardiovascular Risk in Spain) and the ELSA (English Longitudinal Study of Ageing). Given that the effects of alcohol on mental health might be context-specific, analyzing data from these two cohorts may facilitate determining whether any associations found differ between “Mediterranean” countries like Spain, where alcohol is traditionally used as a nutritional element and most drinking occurs during meals, and “Non-Mediterranean” countries like England, where alcohol is consumed in greater amounts and mainly used as a psychotropic-relaxant. In this work we also assessed the impact of the Mediterranean Drinking Pattern (MDP) on depression and psychological distress. The MDP, characterized by moderate alcohol intake, a preference for wine, and drinking only with meals, is the traditional pattern of alcohol consumption in Spain and other regions of the Mediterranean basin20. Previous studies among older adults have reported the MDP to be associated with a reduced risk of functional limitations21, frailty22 and falls23, and with better scores on the Physical Component Summary of the12-item Short Form Health Survey24. However, its effects over mental health are unknown.
Methods
Study population and design
Seniors-ENRICA cohort
This cohort was established during 2008–2010 with individuals selected by multi-stage stratified random sampling from the non-institutionalized Spanish population aged ≥60 years (wave 1)25. For these analyses, we used information from 2,519 subjects participating in wave 2 (2012) and followed through wave 3 (2015)26. In these two waves, information regarding sociodemographic variables, health behaviors and morbidity was collected using a computer assisted telephone interview. There is evidence from Spanish population studies that telephone surveys yield similar distributions of health behaviors and morbidities as face-to-face interviews27,28. In particular, the Spanish telephone-administered geriatric depression scale has shown a high correlation with the validated personal administration of the scale27. An advantage of the telephone-administered geriatric depression scale is that it may increase participation, as depressed individuals are less likely to respond to fac-e-to-face questions on depression27. After telephone interviews, a diet history and a physical exam were performed by trained staff during at-home visits.
From the initial sample of 2,519 participants in 2012, 82 (3.3%) died and 616 (24.5%) were lost to follow-up; thus, in 2015 data on depression and psychological distress came from 1821 individuals. Participants remaining in the study were slightly younger, had higher educational level, fewer comorbidities and lower scores in the GDS and GHQ-12 scales. Never drinkers and ex-drinkers were more likely to be lost to follow-up. All participants gave informed written consent, and the Clinical Research Ethics Committee of the La Paz University Hospital in Madrid approved the study. All methods were performed in accordance with the relevant guidelines and regulations.
ELSA cohort
This cohort comprises people aged ≥50 years living in private households in England29. The present research analyzed data from Waves 0, 1 and 3. As in previous reports30,31, a combination of Wave 0 (drawn from households that had previously responded to the Health Survey from England in 1998, 1999 or 2001) and Wave 1 (which included those households from Wave 0 where at least one member was aged ≥50 years between March 2002 and March 2003), was used to define the baseline sample (n = 11,391). Information from the initial sample was collected using a personal face-to-face Computer Assisted Personal Interview, a nurse visit and a self-completion questionnaire. From the initial sample, we excluded those individuals aged <60 years (n = 4,166).
During follow-up, 241 participants died (3.3%), 1928 (26.7%) refused to participate or could not be contacted, and 488 (6.8%) became ineligible (mainly because they had moved outside of Britain or had been institutionalized). Thus, in 2006–2007, information on depression and physiologic distress was collected from 4,568 participants aged ≥60 years. Participants remaining in the study were more frequently women, younger, had higher educational level, lower tobacco consumption, fewer comorbidities and lower scores in the CES-D. The National Research Ethics Service (MREC/01/2/91) provided the ethical approval for ELSA.
Study variables
Alcohol consumption
In the Seniors-ENRICA study, alcohol consumption was estimated based on a validated diet history, developed from the one used in the EPIC cohort study in Spain32. The diet history collected consumption data for 34 alcoholic beverages and used photographs depicting different glass sizes to help quantify serving sizes. Alcohol content, in grams, was then estimated using standard composition tables. According to the average alcohol intake, participants were classified as (1) never drinkers (this category also included occasional drinkers with average intake close to zero), (2) ex-drinkers (those reporting having stopped drinking for at least a year before the interview), (3) moderate drinkers and 4) heavy drinkers. We set the threshold between moderate and heavy drinking at ≥40 g/day for men and ≥24 g/day for women33. Among drinkers (categories 3 and 4 in the previous classification), a preference for a specific type of alcoholic beverage (wine or other) was acknowledged when more than 80% of alcohol intake was derived from such drink22. According to the consumption of alcohol with meals (lunch or dinner), drinkers (categories 3 and 4) were also classified into three groups: those who drank exclusively during mealtimes, those who drank exclusively outside meal times, and those who drank at any time. Finally, a Mediterranean Drinking Pattern (MDP) was defined as moderate average intake of alcohol (and no binge drinking), with wine preference and alcohol consumption only with meals22.
For the ELSA-cohort analyses, information on alcohol consumption and frequency was derived from Wave 0 but not from Wave 1 because this wave collected information only on the frequency of drinking. According to the average alcohol intake, and having defined 10 grams of pure alcohol as equivalent to an alcohol unit, participants were classified as never drinkers, ex-drinkers, moderate drinkers, and heavy drinkers. The threshold between moderate and heavy drinking was set at 28 units of alcohol/week in men and 21 units/week in women.
Depression
Depression was ascertained with three instruments:
Geriatric Depression Scale (GDS): To assess depressive symptoms, the Seniors-ENRICA study used the 10-item version of the GDS34. Individuals missing ≥2 items were excluded from the analyses. A higher score in the GDS indicates a greater level of depression.
Center for Epidemiologic Studies Depression Scale (CES-D): The ELSA study used the 8-item version of the CES-D)35. A higher score in the CES-D indicates a greater level of depression.
Self-reported depression: In the Seniors-ENRICA study this variable was defined as a positive answer to the question “Has a doctor ever told you that you have depression” or as being on antidepressant medication.
Psychological distress
The Seniors-ENRICA and the ELSA studies used the 12-item version of the General Health Questionnaire (GHQ-12), a screening tool for psychological distress. Individuals missing ≥2 items were excluded from the analyses. Higher scores in the GHQ-12 indicate higher psychological distress.
Other variables
Baseline self-reported data on age, sex, educational status, and tobacco consumption were collected in both cohorts. In the Seniors-ENRICA cohort, information on physical activity (metabolic equivalent-hour/week) and on the number of hours/day spent watching television was assessed using validated questionnaires36,37. In the ELSA study, participants were asked about the frequency (more than once a week, once a week, one to three times a month, or hardly ever/never) of participation in vigorous-, moderate-, and light-intensity activities. An overall measure of physical activity was generated by multiplying activity frequency by the metabolic equivalent value for each type of activity (6 for vigorous-, 3 for moderate-, and 1.5 for light-intensity activities, respectively). In the Seniors-ENRICA, adherence to the Mediterranean diet was captured using the Mediterranean Adherence Screener (MEDAS) index (excluding the alcohol component)38, and energy intake was calculated based on Spanish food composition tables. In both cohorts, baseline weight and height were measured with standard methods. BMI was calculated as (weight in kg)/(height in m)2. Normal weight was defined as a BMI <25, overweight as a BMI 25–29.9, and obesity as a BMI ≥30. Finally, in both cohorts, participants also reported whether they had previously been diagnosed with any of the following diseases: cardiovascular disease (ischemic heart disease, stroke, heart failure), diabetes, chronic lung disease (asthma, chronic bronchitis), and osteomuscular disease (osteoarthritis or arthritis); as well as the number of medications they were taking. In the Seniors-ENRICA, study staff compared self-reported information on medication use with medication packages stored at home.
Statistical analysis
From the initial 1,821 participants in the Seniors-ENRICA cohort, we excluded 200 (11%) subjects with incomplete data on alcohol consumption or potential confounders. Additionally, for analyses on depression we excluded subjects lacking information on the GDS at baseline or follow-up (n = 411; 22.6%). For analyses on psychological distress we excluded individuals with missing data on the GHQ-12 at baseline or follow-up (n = 31; 1.7%). Similarly, from the initial 4,568 participants in the ELSA cohort, 440 (9.6%) subjects were excluded due to incomplete data on alcohol consumption or potential confounders. Also, we excluded individuals with missing information on the CES-D at baseline or follow-up (n = 157; 3.4%) for analyses on depression, and individuals with no data on the GHQ-12 at baseline or follow-up (n = 768; 16.8%) for analyses on psychological distress. Baseline socio-demographic, lifestyle, and clinical characteristics of individuals with and without missing information were similar, although the latter were on average younger, were more likely to be moderate drinkers, and showed a lower prevalence of diabetes and osteomuscular disease.
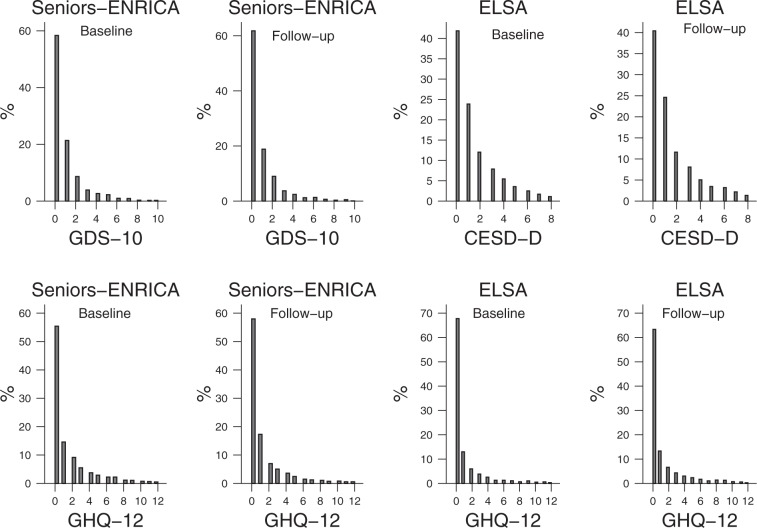
Associations between alcohol consumption and depression or psychological distress were analyzed with generalized regression models because of the highly skewed distribution of the dependent variables (GDS-10, GHQ-12, and CES-D), which mirrored that of count variables (see Fig. 1). To account for over-dispersion and a higher number of zero values than would be expected under the Poisson distribution, we considered using either negative binomial or zero-inflated negative binomial models. Both approaches were compared using Vuong tests which suggested that zero-inflated negative binomial models provided a better fit of the data. Results were expressed as prevalence rate ratios (PRR) and their 95% confidence interval (CI). PRRs in this context represent the percent change in depression and psychological distress scales for one category of alcohol relative to the reference category, holding other variables constant. When the dependent variable was self-reported diagnosed depression, the analyses were performed using Poisson regression with a robust error variance, and results were expressed as Incidence rate ratios (IRR) and their 95% confidence interval.
Figure 1.
Distribution of depression and psychological distress scales in the Seniors-ENRICA and ELSA cohorts, at baseline and at follow-up.
We built three regression models with progressive levels of adjustment. Model 1 adjusted for age, sex, education, and the corresponding baseline values of the dependent variables. Model 2 further adjusted for tobacco consumption, physical activity, BMI, cardiovascular disease, diabetes, chronic lung disease, osteomuscular disease, and cancer in both cohorts. Additionally, the Seniors-ENRICA model 2 adjusted for time watching TV, the MEDAS score, total energy intake, and use of sleeping pills or other central nervous system-acting medications. Analyses of the influence of average alcohol consumption and the MDP were conducted in the total sample, whereas analyses of the influence of beverage preference and drinking with meals were performed only among drinkers. Models for specific drinking habits (i.e. beverage preference, drinking with meals or the MDP) were further adjusted for total alcohol consumption (grams/day).
We conducted separate sensitivity analyses. First, we excluded subjects with baseline cardiovascular disease or cancer as well as participants under anxiolytic, antipsychotic, or antiepileptic medication at baseline. Second, to facilitate comparisons between cohorts, we reran analyses with abstainers (never drinkers and ex-drinkers) as the reference category, and reduced the threshold between moderate and heavy intake to 15 g/day for both genders. Third, we split moderate consumption into two categories: below or above the median average alcohol intake. Fourth, we evaluated the risk of depression as defined by a score above 3 in the CESD or GDS using logistic regression. Finally, we modeled the association between alcohol consumption patterns and changes (defined as difference between follow-up and baseline values) in the GDS-10, GHQ-12, and CES-D, using the VCE (bootstrap) command in Stata to estimate confidence intervals based on 100 resamples (see Supplementary Tables 1 and 2). Our results are presented for both sexes combined because sex-alcohol drinking patterns interactions terms included in regression models failed to reach statistical significance and findings were similar in each sex.
Statistical analyses were performed using Stata®, version 13.1.
Data availability
Data from the Seniors-ENRICA can be accessed upon request to the authors. Data from the ELSA study are available upon request to the UK Data Service
Results
The prevalence of ex-drinkers, moderate drinkers and heavy drinkers at baseline was 7%, 62% and 5% in Seniors-ENRICA, and 5%, 80% and 10% in ELSA, respectively. and Compared to never-drinkers, ex-drinkers were more often male, had higher education, and were more likely to report unhealthy characteristics (obesity, cardiovascular disease, cancer, and use of sleeping pills and other central nervous system-acting medications) (please see Table 1). Both moderate and heavy drinkers were younger, more frequently male, more educated, and, despite lower levels of physical activity, healthier (lower prevalence of obesity, chronic disease, and medication use, and more favorable baseline scores on the GDS-10, GHQ-12 and CESD) (Table 1). According to the GDS (GDS >3) and CESD (CESD >3) scores, at baseline 7.7% (Seniors-ENRICA) and 14.3% (ELSA) of participants had a diagnosis of depression. Similarly, a physician diagnosis of depression was reported at baseline by 7.5% of participants in the Seniors-ENRICA.
Table 1.
Characteristics of the study participants by average alcohol consumption and study cohort.
| Seniors-ENRICA | ELSA | |||||||
|---|---|---|---|---|---|---|---|---|
| Never drinker | Ex-drinker | Moderate drinkera | Heavy drinker | Never drinker | Ex-drinker | Moderate drinkera | Heavy drinker | |
| Female, % | 79.1 | 54.3 | 39.3 | 35.2 | 81.3 | 59.6 | 57.5 | 29.9 |
| Age, years, mean (SD) | 71.9 (5.9) | 72.5 (6.3) | 70.8 (5.8) | 70.6 (5.4) | 69.0 (7.2) | 68.0 (7.2) | 67.0 (7.0) | 65.9 (7.0) |
| Educational level, % | ||||||||
| ≤Primary | 62.9 | 54.3 | 45.2 | 31.0 | 44.8 | 39.4 | 32.7 | 24.6 |
| Secondary | 22.5 | 24.4 | 27.6 | 33.8 | 37.4 | 45.2 | 45.8 | 46.4 |
| University | 14.6 | 21.3 | 27.2 | 35.2 | 17.8 | 15.4 | 21.5 | 29.0 |
| Current smokers, % | 4.7 | 10.6 | 11.4 | 19.7 | 14.6 | 22.9 | 15.1 | 20.6 |
| Physical activity, MET-h/wk, mean (SD) | 64.3 (32.0) | 60.3 (31.8) | 54.9 (29.5) | 49.1 (28.1) | ||||
| Physical activity, % lowest quartile | 16.9 | 17.6 | 25.7 | 30.4 | ||||
| TV viewing, h/wk | 19.4 (10.5) | 20.7 (11.9) | 19.0 (10.2) | 17.2 (8.1) | — | — | — | — |
| MEDAS score, mean (SD)b | 4.1 (1.7) | 4.2 (1.4) | 4.0 (1.6) | 3.5 (1.4) | — | — | — | — |
| Energy intake, kcal/d, mean (SD) | 1873 (401) | 1948 (485) | 2076 (434) | 2614 (1403) | — | — | — | — |
| BMI ≥30 kg/m2, %c | 30.6 | 35.1 | 30.9 | 29.6 | 29.7 | 28.2 | 25.2 | 22.3 |
| Comorbities, % | ||||||||
| Cardiovascular diseased | 7.1 | 9.6 | 5.1 | 4.2 | 12.8 | 23.4 | 13.4 | 11.0 |
| Respiratory disease | 11.2 | 10.6 | 7.7 | 8.5 | 15.5 | 17.6 | 14.2 | 14.6 |
| Osteomuscular disease | 69.5 | 66.0 | 55.0 | 40.9 | 37.9 | 41.5 | 34.4 | 32.8 |
| Diabetes | 16.7 | 23.4 | 15.7 | 15.5 | 8.2 | 6.9 | 4.8 | 4.3 |
| Cancer | 3.7 | 4.3 | 2.1 | 0.0 | 4.6 | 6.9 | 6.5 | 4.6 |
| Sleeping pills, % | 21.4 | 29.8 | 18.6 | 15.5 | ||||
| Other central nervous system-acting drugs,% | 37.6 | 42.6 | 26.7 | 22.5 | — | — | — | — |
| Baseline GDSe scores, mean (SD) | 1.2 (1.8) | 1.5 (2.0) | 0.7 (1.4) | 0.5 (1.1) | — | — | — | — |
| Baseline GHQ-12f scores, mean (SD) | 1.9 (2.8) | 1.9 (2.5) | 1.2 (2.2) | 1.2 (2.0) | 1.4 (2.4) | 1.7 (2.8) | 1.0 (2.2) | 0.9 (1.9) |
| Baseline CES-Dg scores, mean (SD) | — | — | — | — | 2.1 (2.3) | 2.1 (2.1) | 1.4 (1.8) | 1.3 (1.7) |
Data in the table are percentages for categorical variables and means (SD) for continuous variables.
aThe threshold between moderate and heavy drinking is ≥20 g/day in men and ≥10 g/day in women.
bMEDAS: Mediterranean Diet Adherence Screener (range 0–14).
cBMI: Body Mass Index.
dIschemic heart disease, stroke or heart failure.
eGDS: Geriatric Depression Scale-10 item version.
fGHQ-12: General Health Questionnaire-12 item version.
gCES-D Center for Epidemiologic Studies Depression Scale-8 item.
In the Seniors-ENRICA study, drinkers with a preference for wine, who drank only with meals, or who presented a MDP pattern were more likely to be female, slightly older, more physically active, and less frequently obese than their counterparts (Table 2). Those same three types of drinker had a lower prevalence of smoking, higher MEDAS scores, a lower prevalence of respiratory disease, and a higher prevalence of cardiovascular disease, diabetes and osteomuscular disease than their counterparts. The most favorable scores in both the GDS-10 and the GHQ-12 were observed among drinkers with a preference for alcoholic beverages other than wine, those who drank with and outside of meals, and those with no MDP (Table 2).
Table 2.
Characteristics of alcohol drinkers by alcohol consumption patterns in the Seniors-ENRICA cohort.
| Seniors-ENRICA | |||||||
|---|---|---|---|---|---|---|---|
| Beverage preference | Drinking with meals | MDP | |||||
| Other | Wine | With meals | With and outside meals | Without meals | No MDP | MDP | |
| Female, % | 32.5 | 42.6 | 47.6 | 22.5 | 45.2 | 32.4 | 49.5 |
| Age, years, mean (SD) | 70.4 (5.5) | 71.0 (5.9) | 70.1 (5.8) | 70.4 (5.8) | 70.6 (5.3) | 70.5(5.6) | 71.3 (6.0) |
| Educational level, % | |||||||
| ≤Primary | 43.2 | 44.7 | 47.0 | 41.5 | 40.6 | 41.9 | 47.8 |
| Secondary | 27.9 | 28.7 | 27.8 | 27.0 | 31.0 | 27.4 | 29.1 |
| University | 29.9 | 26.6 | 25.2 | 31.5 | 28.4 | 30.7 | 23.1 |
| Current smokers, % | 13.3 | 11.3 | 9.3 | 14.2 | 16.1 | 13.9 | 9.0 |
| Physical activity, METsa *h/wk, mean (SD) | 51.5 (26.8) | 56.1 (30.6) | 56.5 (30.4) | 52.5 (28.9) | 52.1 (26.8) | 52.1 (28.1) | 58.2 (30.9) |
| TV viewing, h/wk, mean (SD) | 19.2 (10.1) | 18.6 (10.1) | 19.5 (10.3) | 18.2 (9.7) | 17.9 (10.2) | 18.6 (9.8) | 19.3 (10.6) |
| MEDASb score, mean (SD) | 3.9 (1.5) | 4.0 (1.6) | 4.1 (1.6) | 3.9 (1.5) | 3.9 (1.6) | 3.9 (1.5) | 4.1 (1.6) |
| Energy intake, kcal/d, mean (SD) | 2172 (646) | 2085 (542) | 2034 (429) | 2244 (658) | 2115 (768) | 2183 (653) | 2010 (430) |
| BMIc ≥30 kg/m2, % | 33.7 | 29.2 | 30.7 | 30.9 | 31.0 | 32.6 | 28.0 |
| Comorbities, % | |||||||
| Cardiovascular diseased | 5.0 | 5.1 | 5.4 | 5.1 | 3.9 | 4.6 | 5.7 |
| Respiratory disease | 8.6 | 7.3 | 7.2 | 7.4 | 10.3 | 8.6 | 6.5 |
| Osteomuscular disease | 50.0 | 56.1 | 59.4 | 45.3 | 54.2 | 48.9 | 62.0 |
| Diabetes | 14.5 | 16.3 | 16.7 | 14.8 | 14.2 | 14.2 | 17.9 |
| Cancer | 1.8 | 2.0 | 2.1 | 1.6 | 1.9 | 1.7 | 2.2 |
| Sleeping pills, % | 16.6 | 19.4 | 19.2 | 14.8 | 23.2 | 17.2 | 20.4 |
| Other central nervous system-acting drugs,% | 24.9 | 27.2 | 27.8 | 21.2 | 32.3 | 25.0 | 28.5 |
| Baseline GDS-10e scores, mean (SD) | 0.6 (1.3) | 0.8 (1.4) | 0.8 (1.4) | 0.6 (1.1) | 0.8 (1.6) | 0.7 (1.3) | 0.8 (1.4) |
| Baseline GHQ-12f scores, mean (SD) | 1.1 (2.2) | 1.3 (2.2) | 1.3 (2.2) | 0.9 (1.9) | 1.6 (2.6) | 1.2 (2.2) | 1.3 (2.2) |
Data in the table are percentages for categorical variables and means and standard deviations (SD) for continuous variables.
aMDP Mediterranean drinking pattern.
bMETs: Metabolic Equivalents of Task.
cMEDAS: Mediterranean Diet Adherence Screener (range 0–14).
dBMI: Body Mass Index.
eIschemic heart disease, stroke or heart failure.
fGDS: Geriatric Depression Scale-10 item version.
gGHQ-12: General Health Questionnaire-12 item version.
The distributions of the GDS-10, CES-D, and GHQ-12 scores at baseline and at follow-up can be observed in Fig. 1. As aforementioned, the most common score in all scales was zero and distributions were all highly skewed to the right. After a 2.8 (ENRICA) and a 7.4-year-mean follow-up (ELSA), 4% and 10% of participants developed incident depression (GDS or CESD scores >3), respectively. Table 3 displays the results for the prospective association between alcohol consumption patterns and follow-up GDS-10 and GHQ-12 scores in the Seniors-ENRICA study. Compared to never-drinkers, moderate alcohol consumers showed similar scores in the GDS-10 (PRR: 1.03; 95%CI: 0.84–1.26) and GHQ-12 (PRR: 0.88; 95%CI: 0.73–1.06). Alcohol consumption patterns, including the MDP, were not associated with GDS-10 or GHQ-12 scores. However, it is worth noting that drinkers with a wine preference showed a non-statistically significant increased number of psychological distress symptoms (PRR: 1.31; 95%CI: 1.03–1.66).
Table 3.
Prospective association between alcohol consumption patterns and Geriatric Depression Scale (GDS) and the General Health Questionnaire-12 (GHQ-12) scores for older adults followed-up for 2.8 years; Seniors-ENRICA cohort study.
| GDS | GHQ-12 | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | Model 1 PRR (95% CI) | Model 2 PRR (95% CI) | n | % | Model 1 PRR (95% CI) | Model 2 PRR (95% CI) | ||
| Average alcohol consumption | 1200 | Average alcohol consumption | 1428 | ||||||
| Never drinker | 315 | 26.2 | Ref. | Ref. | Never drinker (n = 383) | 383 | 26.8 | Ref. | Ref. |
| Ex-drinker | 78 | 6.5 | 0.88 (0.57–1.34) | 0.97 (0.69–1.37) | Ex-drinker (n = 94) | 94 | 6.6 | 1.13 (0.82–1.57) | 1.11 (0.82–1.51) |
| Moderate drinker | 746 | 62.2 | 0.99 (0.77–1.28) | 1.03 (0.84–1.26) | Moderate drinker (n = 880) | 880 | 61.6 | 0.91 (0.75–1.12) | 0.88 (0.73–1.06) |
| Heavy drinker | 61 | 5.1 | 0.65 (0.27–1.53) | 0.88 (0.56–1.36) | Heavy drinker (n = 71) | 71 | 5.0 | 0.68 (0.42–1.09) | 0.70 (0.45–1.08) |
| Beverage preference | 807 | Beverage preference | 951 | ||||||
| Other | 285 | 35.3 | Ref. | Ref. | Other | 338 | 33.5 | Ref. | Ref. |
| Wine | 522 | 64.7 | 0.97 (0.74–1.29) | 1.17 (0.91–1.50) | Wine | 613 | 64.5 | 1.31 (0.98–1.74) | 1.31 (1.03–1.66) |
| Drinking with meals | 807 | Drinking with meals | 951 | ||||||
| Only with meals | 409 | 50.7 | Ref. | Ref. | Only with meals | 485 | 51.0 | Ref. | Ref. |
| With and outside of meals | 261 | 32.3 | 0.81 (0.53–1.25) | 0.91 (0.67–1.22) | With and outside of meals | 311 | 32.7 | 0.96 (0.70–1.31) | 0.90 (0.67–1.19) |
| Only without meals | 137 | 17.0 | 0.87 (0.52–1.45) | 0.84 (0.61–1.18) | Only without meals | 155 | 16.3 | 1.09 (0.76–1.56) | 0.91 (0.66–1.25) |
| Mediterranean drinking pattern (MDP) a | 1200 | Mediterranean drinking pattern (MDP) a | 1428 | ||||||
| Never drinker | 315 | 26.2 | Ref. | Ref. | Never drinker | 383 | 26.8 | Ref. | Ref. |
| Ex-drinker | 78 | 6.5 | 0.90 (0.60–1.36) | 0.96 (0.68–1.35) | Ex-drinker | 94 | 6.6 | 1.13 (0.81–1.57) | 1.10 (0.81–1.50) |
| Drinker with no MDP | 746 | 62.2 | 0.92 (0.67–1.26) | 0.97 (0.75–1.26) | Drinker with no MDP | 583 | 40.8 | 0.89 (0.68–1.15) | 0.88 (0.70–1.13) |
| Drinker with MDP | 61 | 5.1 | 1.08 (0.81–1.43) | 1.15 (0.91–1.46) | Drinker with MDP | 368 | 25.8 | 1.02 (0.80–1.31) | 0.98 (0.78–1.23) |
PRR: Prevalence rate ratio; CI: Confidence interval.
aModerate alcohol consumption with preference for wine and drinking only with meals.
Model 1: Adjusted for the age, sex, educational level (≤primary, secondary, university) and baseline: Geriatric Depression Scale or General Health Questionnaire −12 scores.
Model 2: Additionally adjusted for: tobacco smoking (never/former/current), physical activity (MET-h/week), time watching TV (h/week), MEDAS index (excluding alcohol), total energy intake (Kcal/day), Body Mass Index (≤25, 25–29.9, ≥30 kg/m2), cardiovascular disease, respiratory disease, osteo-muscular disease, diabetes, cancer, sleeping pills and central nervous system-acting medications.
Models for specific drinking habits (i.e. beverage preference, drinking with meals or the MDP) were further adjusted for average alcohol consumption (grams/day).
In the Seniors-ENRICA, we found no evidence of an association between moderate alcohol intake (IRR: 1.14; 95%CI: 0.57–2.29) or the MDP (IRR: 1.84; 95%CI: 0.80–4.25) and incidence of self-reported depression (defined as a physician-diagnosis of depression or as being on antidepressant medication) (Supplementary Table 3). Results for heavy drinking, beverage preference, or drinking with meals and self-reported depression could not be interpreted due to a low number of incident self-reported depression cases (Supplementary Table 3).
Results for the prospective association between average alcohol consumption and follow-up CES-D and GHQ-12 scores in the ELSA cohort can be found in Table 4. Compared to never drinkers, both moderate and heavy drinkers showed similar percent changes in depression and psychologic wellbeing scales. In this sense, the PRR (95%CI) for CESD-D was 0.92 (0.79–1.06) in moderate drinkers, and 1.00 (0.84–1.20) in heavy drinkers; the corresponding results for the GHQ-12 were 0.75 (0.55–1.01) and 0.84 (0.58–1.21), respectively.
Table 4.
Prospective association between average alcohol consumption and Center for Epidemiologic Studies Depression Scale (CES-D) and the General Health Questionnaire-12 (GHQ-12) scores for older adults followed-up for 7.4 years; English Longitudinal Study of Ageing (ELSA).
| CESD | GHQ-12 | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | Model 1 PRR (95% CI) | Model 2 PRR (95% CI) | n | % | Model 1 PRR (95% CI) | Model 2 PRR (95% CI) | ||
| Average alcohol consumption | 3971 | Average alcohol consumption | 3360 | ||||||
| Never drinker | 219 | 5.5 | Ref. | Ref. | Never drinker | 161 | 4.8 | Ref. | Ref. |
| Ex-drinker | 188 | 4.7 | 1.16 (0.96–1.41) | 1.11 (0.91–1.35) | Ex-drinker | 156 | 4.6 | 0.87 (0.59–1.30) | 0.81 (0.54–1.21) |
| Moderate drinker | 3146 | 79.2 | 0.95 (0.83–1.09) | 0.92 (0.79–1.06) | Moderate drinker | 2688 | 80.0 | 0.77 (0.57–1.04) | 0.75 (0.55–1.01) |
| Heavy drinker | 418 | 10.5 | 1.05 (0.88–1.26) | 1.00 (0.84–1.20) | Heavy drinker | 355 | 10.6 | 0.88 (0.61–1.27) | 0.84 (0.58–1.21) |
PRR: Prevalence rate ratios; CI: Confidence interval.
Model 1: Adjusted for the age, sex, educational level (≤primary, secondary, university) and baseline CESD scores or GHQ-12 scores.
Model 2: Adjusted additionally for tobacco smoking (never/former/current), physical activity, BMI (≤25, 25–29.9, ≥30 kg/m2), cardiovascular disease, respiratory disease, osteomuscular disease, diabetes, and cancer.
Sensitivity analyses yielded similar results to those presented in the main tables (data not shown).
Discussion
Overall, we found no consistent protective association between moderate alcohol consumption and depression in older adults. Moreover, in the Seniors-ENRICA cohort, adherence to certain alcohol consumption patterns such as drinking only with meals or the MDP failed to show an association with either of the studied mental health outcomes. However, results showed some non-significant tendency to a lower risk of depression (Spanish sample) and psychological distress (both samples) associated with heavy drinking, which should be further investigated in studies with a larger number of heavy drinkers.
Previous research on the link between moderate alcohol intake and mental health in adults has yielded inconsistent results. In the National Psychiatric Morbidity Survey in England, which followed 2,413 adults for 18 months, moderate drinking (defined as drinking <21 or <14 units/week in men or women, respectively, or having an AUDIT score <8 points), showed no association with incident anxiety or depression (measured with the Clinical Interview Schedule-Revised instrument) when compared to abstaining17. By contrast, Norway’s Nord-Trøndelag Health Survey of 38,930 individuals with a mean age of 48 years, ascertained that low-to-moderate drinkers had a lower risk of case-level anxiety and depression (based on Hospital Anxiety and Depression Rating Scale) than non-drinkers (self-reported abstainers and non-abstainers currently consuming no alcohol). Unfortunately, the study’s partial cross-sectional design hindered drawing causal inference39. Also, a Spanish cohort study of 13,619 university graduates (mean age: 38 years) followed for 10 years showed that female – but not male- moderate drinkers (5–15 g/day) were less likely to self-report suffering from depression than abstainers15. However, a study of midlife alcohol consumption of the Whitehall II cohort of British civil servants, concluded that there was no association between drinking patterns, including a moderate (<40 g/day) one, and risk of depression. The 28-year follow-up study consisted of 7,478 men and women between the ages of 35 and 55 years and depression was assessed by the GHQ-3040. More recently, results based on 3,201 individuals aged 18–65 years, who were primary care attenders in the WHO collaborative study of Psychological Problems in General Health Care, suggested a possible protective effect of moderate (defined as AUDIT <8 points) drinking in the risk of developing a new onset of depression and generalized anxiety disorder (GAD)14.
To our knowledge only one study has focused on older adults. Gea et al. followed 5,505 high-risk men and women (55 to 80 y) from the PREDIMED Trial. Unlike the WHO collaborative study, participants in PREDIMED were initially free of depression or a history of depression, and did not have any history of alcohol-related problems. After 7 years of follow-up, moderate drinkers (5–15 g/day) of both genders were less likely to self-report a diagnosis of depression than abstainers16. Specifically, wine consumption in the range of 2–7 drinks/week decreased the risk of incident depression in this population16. Results in our study using abstainers (never drinkers and ex-drinkers) as the reference category or changing the threshold between moderate and heavy intake to 15 g/day showed no association between moderate alcohol intake and depression. A partial explanation for the discrepant results between the PREDIMED study and ours might be that participants in the PREDIMED trial were primary-care patients participating in an intensive group-based health education intervention; thus, we speculate that the intervention-related social support very likely geared towards a greater adherence to a Mediterranean diet (including moderate drinking)41, received by PREDIMED participants may have contributed to a lower depression risk42. Moreover, greater adherence to a healthy diet also reduces the incidence of cardiovascular disease, diabetes and other chronic diseases which, in turn, are strong risk factors or triggers for depression.
In some cases, differences between clinic-based studies14,16 -which found a protective association between moderate alcohol intake and mental health- and studies in community samples40 which did not find such association (i.e. ours), could be partially explained by the self-medication hypothesis, whereby alcohol intake is used to ameliorate mental and other health problems; this phenomenon could operate more strongly in clinical than community samples due to their worse health status.
Our work has several strengths compared to published research. First, unlike previous studies14–16, we distinguished between never drinkers and ex-drinkers. Since ex-drinkers might have quit drinking due to ill health, including depression, studies incorporating ex-drinkers in the reference category may overestimate the protective effect of moderate alcohol drinking on depression. Second, we adjusted our analyses for a larger number of lifestyle and morbidity variables than previous reports14,15,17. Third, as far as we are aware of, this is the first study to provide detailed analyses on the association between different patterns of moderate alcohol consumption, including the MDP, and mental health outcomes16. Fourth, we used a validated diet history to estimate alcohol consumption in the Seniors-ENRICA cohort. In fact, the Pearson correlation coefficient between alcohol consumption data from the diet history and seven 24-h recalls over the course of one year was a satisfactory 0.6532. Finally, we obtained consistent results using two cohorts characterized by different patterns of alcohol consumption and different follow-up periods. This is important because it suggests that the association, or lack thereof, between moderate alcohol intake and depression does not differ by cultural and social context, i.e., it may be similar in “wet and “dry” countries. Additionally, the ELSA 7.4-year mean follow-up suggests that the failure to detect an association is not due to failing to follow individuals “long enough to see an effect”.
The main limitation of the study was that alcohol consumption was self-reported with the corresponding risk of recall error and social desirability bias. It is known that questions on alcohol habits are commonly subject to under-reporting, particularly among heavy drinkers43. In this sense, although numbers were similar to those reported in previous population-based studies44,45, the percentage of heavy drinkers in our cohorts was rather low (5% in Spain and 10% in the UK). In any case, there is evidence that telephone interviews are less affected by social desirability bias than personal interviews. Second, we lacked repeated measurements of alcohol intake during follow-up to update the information on exposure to alcohol. Third, although we used validated depression and psychological distress scales, these were not confirmed by a clinical diagnosis. Thus, we cannot rule out the existence of diagnostic bias, which effect on these results remains unknown. However, in the Seniors-ENRICA, were we had information on previous physician-diagnoses of depression or being under antidepressant treatment (which was confirmed against drug packages at home), we observed a similar prevalence of depression either using this information or the GDS scale. Fourth, our results may not be generalizable to institutionalized older adults. Finally, in both cohorts we observed an association between heavy drinking and decreased number of psychological distress symptoms approaching statistical significance. However, the small number of heavy drinkers in this cohort makes these results unreliable.
Conclusions
Our results do not support the presence of a protective effect derived from moderate alcohol consumption in general, and wine in particular, on the risk of developing depression or psychological distress among older adults. Given the inconsistency in this literature on the general population and the scarce research on older adults, future research should assess whether and how changes in alcohol consumption patterns affect depression risk using repeated measures of alcohol intake and clinical diagnoses of depression in this vulnerable population.
Electronic supplementary material
Supplementary Information - Prospective association between alcohol consumption patterns and the risk of self-reported incident depression in older adults
Acknowledgements
This work was supported by grant no. 02/2014 from the Plan Nacional sobre Drogas (Ministry of Health of Spain). Additional support was obtained from FIS grants nos. 12/1166 and 16/609 (Instituto de Salud Carlos III, State Secretary of R + D + I and FEDER/FSE); the FRAILOMIC Initiative (European Union FP7 grant agreement 305483-2); the Ageing Trajectories of Health: Longitudinal Opportunities and Synergies (ATHLOS) project (European Union H2020 grant agreement 635316); and the CIBER of Epidemiology and Public Health (CIBERESP). ELSA waves have been funded jointly by UK government departments and the National Institute on Aging, in the USA. The funding agencies had no role in study design, data analysis, interpretation of results, manuscript preparation or in the decision to submit this manuscript for publication. Dr. Laclaustra was supported by Agencia Aragonesa para la Investigación y Desarrollo (ARAID).
Author Contributions
E.G.E. and F.R.A. conceived the study. E.G.E. performed the statistical analyses. E.G.E. drafted the initial document. All authors reviewed the manuscript for important intellectual content. All authors had full access to all of the data (including statistical reports and tables) in the study and can take responsibility for the integrity of the data and the accuracy of the data analysis.
Competing Interests
The authors declare no competing interests.
Footnotes
Electronic supplementary material
Supplementary information accompanies this paper at 10.1038/s41598-018-29985-4.
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Alexopoulos GS. Depression in the elderly. Lancet. 2005;365:1961–1970. doi: 10.1016/S0140-6736(05)66665-2. [DOI] [PubMed] [Google Scholar]
- 2.Institute for Health Metrics and Evaluation. GBD Compare Data Visualization. Seattle, WA: IHME, University of Washington; http://vizhub.healthdata.org/gbd-compare (2017).
- 3.Katon WJ, Lin E, Russo J, Unutzer J. Increased medical costs of a population-based sample of depressed elderly patients. Arch Gen Psychiatry. 2003;60:897–903. doi: 10.1001/archpsyc.60.9.897. [DOI] [PubMed] [Google Scholar]
- 4.Penninx BW, Leveille S, Ferrucci L, van Eijk JT, Guralnik JM. Exploring the effect of depression on physical disability: longitudinal evidence from the established populations for epidemiologic studies of the elderly. Am J Public Health. 1999;89:1346–1352. doi: 10.2105/AJPH.89.9.1346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wright PP, Thorpe CW. Triple Threat Among the Elderly: Depression, Suicide Risk, and Handguns. J Emerg Nurs. 2016;42:14–18. doi: 10.1016/j.jen.2015.01.010. [DOI] [PubMed] [Google Scholar]
- 6.Covinsky KE, et al. Depressive symptoms and 3-year mortality in older hospitalized medical patients. Ann Intern Med. 1999;130:563–569. doi: 10.7326/0003-4819-130-7-199904060-00004. [DOI] [PubMed] [Google Scholar]
- 7.Sutcliffe C, et al. Depressed mood, cognitive impairment, and survival in older people admitted to care homes in England. Am J Geriatr Psychiatry. 2007;15:708–715. doi: 10.1097/JGP.0b013e3180381537. [DOI] [PubMed] [Google Scholar]
- 8.World Health Organization. Global status report on alcohol and health 2014. Geneva: Department of Mental Health and Substance Dependence World Health Organization. http://wwwwho int/substance_abuse/publications/global_alcohol_report/en/ (2017).
- 9.Baan R, et al. Carcinogenicity of alcoholic beverages. Lancet Oncol. 2007;8:292–293. doi: 10.1016/S1470-2045(07)70099-2. [DOI] [PubMed] [Google Scholar]
- 10.Parry CD, Patra J, Rehm J. Alcohol consumption and non-communicable diseases: epidemiology and policy implications. Addiction. 2011;106:1718–1724. doi: 10.1111/j.1360-0443.2011.03605.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Klatsky AL. Alcohol and cardiovascular diseases: where do we stand today? J Intern Med. 2015;278:238–250. doi: 10.1111/joim.12390. [DOI] [PubMed] [Google Scholar]
- 12.Li XH, Yu FF, Zhou YH, He J. Association between alcohol consumption and the risk of incident type 2 diabetes: a systematic review and dose-response meta-analysis. Am J Clin Nutr. 2016;103:818–829. doi: 10.3945/ajcn.115.114389. [DOI] [PubMed] [Google Scholar]
- 13.Sullivan LE, Fiellin DA, O’Connor PG. The prevalence and impact of alcohol problems in major depression: a systematic review. Am J Med. 2005;118:330–341. doi: 10.1016/j.amjmed.2005.01.007. [DOI] [PubMed] [Google Scholar]
- 14.Bellos S, et al. Longitudinal association between different levels of alcohol consumption and a new onset of depression and generalized anxiety disorder: Results from an international study in primary care. Psychiatry Res. 2016;243:30–34. doi: 10.1016/j.psychres.2016.05.049. [DOI] [PubMed] [Google Scholar]
- 15.Gea A, et al. A longitudinal assessment of alcohol intake and incident depression: the SUN project. BMC Public Health. 2012;12:954. doi: 10.1186/1471-2458-12-954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gea A, et al. Alcohol intake, wine consumption and the development of depression: the PREDIMED study. BMC Med. 2013;11:192. doi: 10.1186/1741-7015-11-192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Haynes JC, et al. Alcohol consumption as a risk factor for anxiety and depression: results from the longitudinal follow-up of the National Psychiatric Morbidity Survey. Br J Psychiatry. 2005;187:544–551. doi: 10.1192/bjp.187.6.544. [DOI] [PubMed] [Google Scholar]
- 18.Brennan PL, SooHoo S, Lemke S, Schutte KK. Alcohol Use Predicts 10-Year Depressive Symptom Trajectories in the Health and Retirement Study. J Aging Health. 2016;28:911–932. doi: 10.1177/0898264315615837. [DOI] [PubMed] [Google Scholar]
- 19.Paulson D, et al. The relationship between moderate alcohol consumption, depressive symptomatology, and C-reactive protein: the Health and Retirement Study. Int J Geriatr Psychiatry. 2018;2:316–324. doi: 10.1002/gps.4746. [DOI] [PubMed] [Google Scholar]
- 20.Willett WC, et al. Mediterranean diet pyramid: a cultural model for healthy eating. Am J Clin Nutr. 1995;61:1402S–1406S. doi: 10.1093/ajcn/61.6.1402S. [DOI] [PubMed] [Google Scholar]
- 21.Leon-Munoz LM, Guallar-Castillon P, Garcia-Esquinas E, Galan I, Rodriguez-Artalejo F. Alcohol drinking patterns and risk of functional limitations in two cohorts of older adults. Clin Nutr. 2016;36:831–838. doi: 10.1016/j.clnu.2016.05.005. [DOI] [PubMed] [Google Scholar]
- 22.Ortola R, et al. Patterns of Alcohol Consumption and Risk of Frailty in Community-dwelling Older Adults. J Gerontol A Biol Sci Med Sci. 2016;71:251–258. doi: 10.1093/gerona/glv125. [DOI] [PubMed] [Google Scholar]
- 23.Ortola R, et al. Patterns of alcohol consumption and risk of falls in older adults: a prospective cohort study. Osteoporos Int. 2017;28:3143–3152. doi: 10.1007/s00198-017-4157-2. [DOI] [PubMed] [Google Scholar]
- 24.Ortola R, Garcia-Esquinas E, Galan I, Rodriguez-Artalejo F. Patterns of alcohol consumption and health-related quality of life in older adults. Drug Alcohol Depend. 2016;159:166–173. doi: 10.1016/j.drugalcdep.2015.12.012. [DOI] [PubMed] [Google Scholar]
- 25.Rodriguez-Artalejo F, et al. Rationale and methods of the study on nutrition and cardiovascular risk in Spain (ENRICA) Rev Esp Cardiol. 2011;64:876–882. doi: 10.1016/j.recesp.2011.05.019. [DOI] [PubMed] [Google Scholar]
- 26.Campanini, M. z., Guallar-Castellón, P., Rodríguez-Artalejo, F. & López-García, E. Mediterranean Diet and Changes in Sleep Duration and Indicators of Sleep Quality in Older Adults. Sleep 40 (2017). [DOI] [PubMed]
- 27.Carrete P, et al. Validation of a telephone-administered geriatric depression scale in a hispanic elderly population. J Gen Intern Med. 2001;16:446–450. doi: 10.1046/j.1525-1497.2001.016007446.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Galan I, Rodriguez-Artalejo F, Zorrilla B. Telephone versus face-to-face household interviews in the assessment of health behaviors and preventive practices. Gac Sanit. 2004;18:440–450. doi: 10.1016/S0213-9111(04)72031-2. [DOI] [PubMed] [Google Scholar]
- 29.Steptoe A, Breeze E, Banks J, Nazroo J. Cohort profile: the English longitudinal study of ageing. Int J Epidemiol. 2013;42:1640–1648. doi: 10.1093/ije/dys168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Frisher M, et al. Is alcohol consumption in older adults associated with poor self-rated health? Cross-sectional and longitudinal analyses from the English Longitudinal Study of Ageing. BMC Public Health. 2015;15:703. doi: 10.1186/s12889-015-1993-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shankar A, McMunn A, Steptoe A. Health-related behaviors in older adults relationships with socioeconomic status. Am J Prev Med. 2010;38:39–46. doi: 10.1016/j.amepre.2009.08.026. [DOI] [PubMed] [Google Scholar]
- 32.Guallar-Castillon P, et al. Validity and reproducibility of a Spanish dietary history. PLoS One. 2014;9:e86074. doi: 10.1371/journal.pone.0086074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.World Health Organization. International guide for monitoring alcohol consumption and related harm. Geneva: Department of Mental Health and Substance Dependence World Health Organization. Available at: http://whqlibdoc.who.int/hq/2000/WHO_MSD_MSB_00.4.pdf (2017).
- 34.Yesavage JA, Brink TL, Rose TL. Development and validation of a geriatric depression rating scale: a preliminary report. J Psych Res. 1983;17:27. doi: 10.1016/0022-3956(82)90033-4. [DOI] [PubMed] [Google Scholar]
- 35.Radloff. The CES-D Scale: A Self-Report Depression Scale for Resarch in the General Population. Applied Psychological Measurement. 1, 385–401 (1977).
- 36.Martinez-Gonzalez MA, Lopez-Fontana C, Varo JJ, Sanchez-Villegas A, Martinez JA. Validation of the Spanish version of the physical activity questionnaire used in the Nurses’ Health Study and the Health Professionals’ Follow-up Study. Public Health Nutr. 2005;8:920–927. doi: 10.1079/PHN2005745. [DOI] [PubMed] [Google Scholar]
- 37.Pols MA, et al. Estimation of reproducibility and relative validity of the questions included in the EPIC Physical Activity Questionnaire. Int J Epidemiol. 1997;26:S181–S189. doi: 10.1093/ije/26.suppl_1.S181. [DOI] [PubMed] [Google Scholar]
- 38.Schroder H, et al. A short screener is valid for assessing Mediterranean diet adherence among older Spanish men and women. J Nutr. 2011;141:1140–1145. doi: 10.3945/jn.110.135566. [DOI] [PubMed] [Google Scholar]
- 39.Skogen JC, Harvey SB, Henderson M, Stordal E, Mykletun A. Anxiety and depression among abstainers and low-level alcohol consumers. The Nord-Trondelag Health Study. Addiction. 2009;104:1519–1529. doi: 10.1111/j.1360-0443.2009.02659.x. [DOI] [PubMed] [Google Scholar]
- 40.Bell S, Britton A. Drinking pattern during midlife and risk of developing depression during 28 years of follow-up: A prospective cohort study. Drug Alcohol Depend. 2015;155:111–117. doi: 10.1016/j.drugalcdep.2015.08.008. [DOI] [PubMed] [Google Scholar]
- 41.Sanchez-Villegas A, et al. Mediterranean dietary pattern and depression: the PREDIMED randomized trial. BMC Med. 2013;11:208. doi: 10.1186/1741-7015-11-208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Prince MJ, Harwood RH, Blizard RA, Thomas A, Mann AH. Social support deficits, loneliness and life events as risk factors for depression in old age. The Gospel Oak Project VI. Psychol Med. 1997;27:323–332. doi: 10.1017/S0033291796004485. [DOI] [PubMed] [Google Scholar]
- 43.Midanik L. The validity of self-reported alcohol consumption and alcohol problems: a literature review. Br J Addict. 1982;77:357–382. doi: 10.1111/j.1360-0443.1982.tb02469.x. [DOI] [PubMed] [Google Scholar]
- 44.Galan I, Gonzalez MJ, Valencia-Martin JL. Alcohol drinking patterns in Spain: a country in transition. Rev Esp Salud Publica. 2014;88:529–540. doi: 10.4321/S1135-57272014000400007. [DOI] [PubMed] [Google Scholar]
- 45.NHS. Statistics on Alcohol. England, 2017. NHS Digital. 3-5-0017.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Information - Prospective association between alcohol consumption patterns and the risk of self-reported incident depression in older adults
Data Availability Statement
Data from the Seniors-ENRICA can be accessed upon request to the authors. Data from the ELSA study are available upon request to the UK Data Service