Abstract
L-tyrosine supplementation may provide benefit to nemaline myopathy (NM) patients, however previous studies are inconclusive, with no elevation of L-tyrosine levels in blood or tissue reported. We evaluated the ability of L-tyrosine treatments to improve skeletal muscle function in all three published animal models of NM caused by dominant skeletal muscle α-actin (ACTA1) mutations. Highest safe L-tyrosine concentrations were determined for dosing water and feed of wildtype zebrafish and mice respectively. NM TgACTA1D286G-eGFP zebrafish treated with 10 μM L-tyrosine from 24 hours to 6 days post fertilization displayed no improvement in swimming distance. NM TgACTA1D286G mice consuming 2% L-tyrosine supplemented feed from preconception had significant elevations in free L-tyrosine levels in sera (57%) and quadriceps muscle (45%) when examined at 6–7 weeks old. However indicators of skeletal muscle integrity (voluntary exercise, bodyweight, rotarod performance) were not improved. Additionally no benefit on the mechanical properties, energy metabolism, or atrophy of skeletal muscles of 6–7 month old TgACTA1D286G and KIActa1H40Y mice eventuated from consuming a 2% L-tyrosine supplemented diet for 4 weeks. Therefore this study yields important information on aspects of the clinical utility of L-tyrosine for ACTA1 NM.
Introduction
Tyrosine is a non-essential amino acid that serves as a precursor for several biologically active substances including the brain catecholamine neurotransmitters norepinephrine (NE) and dopamine. Tyrosine may be derived from the diet or via the enzymatic action of phenylalanine hydroxylase on phenylalanine present in the liver, leading to the production of L-tyrosine (the biologically active form of tyrosine1). In humans, oral ingestion of L-tyrosine can improve stress-induced cognitive and behavioural deficits1,2. Additionally, acute L-tyrosine ingestion is thought to enhance performance via improvements to aerobic power, cognitive performance, neurotransmitter synthesis, and stress related exercise3. L-tyrosine treatment in rodents can reduce deficits in locomotor activity in old mice following cold water stress, alter stress-related changes in aggression in young mice4, and can protect against both neurochemical and behavioural effects induced by various states of stress5,6.
Dietary supplementation with L-tyrosine may have therapeutic application for patients with the skeletal muscle disorder nemaline myopathy (NM)7–9. NM is a mainly congenital-onset disorder producing weakened skeletal muscles that contain the characteristic pathological features nemaline bodies10. However no correlation has been shown to exist between the prevalence of nemaline bodies and the degree of skeletal muscle weakness11,12. Twelve different genes can cause NM13–15, with a significant proportion of all NM-causing mutations being within the skeletal muscle α-actin gene, ACTA113. The majority of patients with ACTA1-NM have a severe phenotype leading to death within the first year of life16. At present, no curative treatment exists, highlighting the importance to thoroughly test plausible therapies and for potential novel therapeutic approaches to be identified and investigated.
Daily supplementation of L-tyrosine by an adult male and his 7-year-old son (both with NM) resulted in improved body strength (father), decreased pharyngeal secretions (son), and improved general stamina (both)7. After 10 days of L-tyrosine withdrawal, both patients reported reversion to previous clinical conditions, suggesting the improved conditions resulted from L-tyrosine administration7. A subsequent small trial contained 5 genetically undefined NM patients (4 infants, 1 adolescent with childhood onset) receiving between 250 to 3000 mg/d of powdered or capsule L-tyrosine for 2 to 5 months9. Within 72 h on the L-tyrosine regime, all infants displayed initial improvements in “sialorrhoea, skeletal muscle strength and energy levels”9. Additionally, L-tyrosine (250 mg/d) from 3 months of age was reported to produce marked reduction in oral secretions and improvement in skeletal muscle strength in a severely affected NM patient, however the patient died at 4 months with sudden cardiorespiratory failure17.
A murine model of NM due to an Acta1 mutation (KIActa1H40Y) was orally dosed via syringe with L-tyrosine (25 mg/d) for 4 weeks, from 4 weeks of age18. This study concluded that L-tyrosine supplementation alleviated mobility deficits and skeletal muscle pathologies characteristic of KIActa1H40Y mice. However, the study did not address modulatory effects of the L-tyrosine dosing on the early lethality of male mice, nor did it report the sera or tissue levels of L-tyrosine.
Due to the limited, albeit promising data from the few patient studies and the single NM mouse model report, we aimed to comprehensively assess one aspect of the reported therapeutic benefit of dietary supplementation of L-tyrosine, skeletal muscle function. To do so, we chose three dominant NM animal models, each with a missense ACTA1 mutation resulting in an amino acid substitution (a mouse and a zebrafish model with p.D286G; a mouse model with p.H40Y). In addition to each of these models being suitable animal models of ACTA1-NM, they also have characterised deficits in skeletal muscle function ideal for robust assessment of any improvement due to L-tyrosine. Initially, we evaluated different levels of L-tyrosine supplementation in wildtype (WT) zebrafish and mice to identify the highest safe L-tyrosine concentration to dose our NM models. We determined L-tyrosine levels in sera and skeletal muscles of treated mice using this dose, to ensure this supplementation resulted in a significant L-tyrosine increase in the relevant tissues. We tested different L-tyrosine treatment regimes on the dominant ACTA1-NM zebrafish and mouse models, and evaluated potential effects on skeletal muscle function using physiological assays and parameters of voluntary exercise.
Results
L-tyrosine treatment at higher concentrations can result in deleterious side effects in WT zebrafish
A pilot range-finding experiment with WT zebrafish was performed to determine the maximal non-toxic L-tyrosine dose for treatment. Concentrations ranged from 0.1 μM to 10 mM and the survival, heart rate and locomotion of the zebrafish were recorded. Whilst there was a trend between decreasing concentrations of L-tyrosine and resting heart rate, we observed a significant increase in resting heart rate for zebrafish treated with 0.1 μM and 1 μM, suggesting that L-tyrosine was eliciting a biological effect in the fish. The experimental dose for L-tyrosine treatment was determined at 10 μM since zebrafish treated with higher concentrations showed significantly reduced survival and swimming performance compared to water treated control fish (Fig. 1).
Figure 1.
Toxicity analyses for L-tyrosine treatment of WT zebrafish. (A) Percentage survival, and (B) resting heart rate in beats per minute (bpm) of zebrafish treated with increasing L-tyrosine concentrations (from 0.1 μM to 10 mM) or H2O (used as a control). Error bars represent ± s.e.m. for four independent experiments with 30 zebrafish per experiment for survival assays and 10 zebrafish per experiment for heart rate assays, *p < 0.05, **p < 0.01 compared to H20 treatment. (C) Normalised distance travelled by 6 dpf zebrafish treated with increasing L-tyrosine concentrations (from 0.1 μM to 1 mM) or H2O. Error bars represent ± s.e.m. for four independent experiments with 19–24 zebrafish per dose per experiment. **p < 0.01.
L-tyrosine addition does not improve the swimming performance of TgACTA1D286G-eGFP zebrafish
TgACTA1D286G-eGFP zebrafish and their WT siblings (not carrying the ACTA1D286G-eGFP cassette) were maintained from 1 day post fertilisation (dpf) in E3 media treated with either 10 μM L-tyrosine or H2O until 6 dpf when their swimming performance was assessed. As expected, a significant reduction in distance travelled was observed in water treated TgACTA1D286G-eGFP fish compared to control WT siblings (TgACTA1D286G-eGFP = 0.861 ± 0.021, n = 112; WT siblings = 1.00 ± 0.073, n = 127, p < 0.01). This deficit in swimming distance in TgACTA1D286G-eGFP zebrafish was not ameliorated by the L-tyrosine treatment (water treated = 0.861 ± 0.021, n = 112; tyrosine treated = 0.831 ± 0.082, n = 126; Fig. 2).
Figure 2.

L-tyrosine treatment of TgACTA1D286G-eGFP zebrafish. Normalised distance travelled by 6 dpf TgACTA1D286G-eGFP and WT sibling control zebrafish treated with 10 μM L-tyrosine or H2O. Error bars represent ± s.e.m for five independent experiments with n = 238 for TgACTA1D286G-eGFP, n = 168 WT siblings, 16–39 zebrafish per treatment, per genotype, per experiment. *p < 0.05, **p < 0.01.
WT mice receiving 4% and 8% L-tyrosine supplemented diets after birth display deleterious side effects, whereas mice receiving a 2% L-tyrosine supplemented diet from pre-conception do not
A safety dosing study for L-tyrosine (0, 2, 4 or 8%) supplemented to normal mouse feed (normally 0.7% L-tyrosine) was performed with WT (FVB/NJArc) mice. We observed deleterious outcomes for mice maintained on both the 4% and 8% L-tyrosine supplemented diets. For mice eating the 8% supplemented feed, one dam lost her entire first litter (not necessarily abnormal) then took longer than usual to again become pregnant. She successfully produced a litter of 6 pups, however when the pups were >1 week of age, they were all found dead, a finding out of the ordinary. The second dam receiving the 8% L-tyrosine supplemented feed produced her first and only litter with 2 pups. These pups appeared smaller than usual at the time of wean and were therefore given soft feed located at the base of the cage. Shortly after wean one of the pups was observed to not be moving despite breathing normally and appearing well at an early check that same day. He was therefore sacrificed. Both pups were determined to be ~50% of the weight of WT mice fed the standard diet.
A total of 30 pups were born to the dams receiving the 4% L-tyrosine supplemented feed. Many of these pups, and their mothers, appeared generally dishevelled with ruffled fur. Most pups were found missing on postnatal day 17 (presumably died and were then eaten by the dams or their siblings) with only 6 pups surviving beyond this age (80% mortality). The surviving mice had decreased bodyweight compared to age-matched mice on the control diet (4% L = tyrosine, 11.5 ± 1.7 g, n = 6; control diet, 15.4 ± 1.4 g, n = 9, p = 0.0004).
Due to the animal welfare concerns surrounding these findings, the 4% and 8% L-tyrosine supplemented diets were not further pursued. No detrimental side effects were overtly noticeable for the dams with the 2% L-tyrosine supplemented diet or their resulting offspring (n = 17), with all pups surviving beyond wean age and appearing by eye to be similar to those born to mice on the regular diet. Therefore this dose was subsequently evaluated for therapeutic benefit in the two NM mouse models, with the dosing regime being either from pre-conception or commencing at 5 to 6 months of age. Our measurements of average daily feed consumption in adult NM mice indicated that mice continued to eat the same amount of feed once receiving the L-tyrosine supplementation as there was no change in the weight of feed consumed during the 4 week exposure to the 2% L-tyrosine supplemented diet relative to when mice were receiving the normal diet (~3 g/day and ~4.5 g/day consumed for the KIActa1H40Y and the TgACTA1D286G mice respectively).
Normal feed supplemented with 2% L-tyrosine significantly elevates levels of L-tyrosine in sera and skeletal muscle of TgACTA1D286G mice
We assayed samples from TgACTA1D286G mice receiving the 2% L-tyrosine supplemented feed compared to untreated mice on the control diet and determined that the freely detectable levels of L-tyrosine were significantly elevated in both the sera (untreated mice = 52.7 ± 7.8 nmol/ml, treated mice = 83.0 ± 13.9 nmol/ml, p < 0.01) and quadriceps femoris muscle (untreated mice = 0.089 ± 0.021 nmol/mg, treated mice = 0.129 ± 0.032 nmol/mg, p < 0.05; Fig. 3).
Figure 3.
Levels of free L-tyrosine in sera and quadriceps femoris of TgACTA1D286G mice. The concentration of free L-tyrosine was quantified via LC/MS in (A) sera samples (untreated, n = 4; L-tyrosine, n = 8), and (B) quadriceps femoris muscles (untreated, n = 6; L-tyrosine, n = 11) of 6-week old TgACTA1D286G mice receiving a 2% L-tyrosine supplemented diet from preconception compared to those fed control diets. Each data point represents an individual mouse ± s.d. *p < 0.05, **p < 0.01.
Total bodyweight and hindlimb skeletal muscles volume are not increased in L-tyrosine treated ACTA1-NM mice
At 6 weeks of age there was no improvement in overall bodyweight of male or female TgACTA1D286G mice treated from pre-conception (Fig. 4A). To the contrary, a significant decrease in total bodyweight was detected in L-tyrosine treated male mice compared to untreated TgACTA1D286G mice (Fig. 4A). Likewise, reduced total bodyweight was not negated at 6–7 months for ACTA1-NM mice from either mouse model treated for 1 month (TgACTA1D286G treated = 32.8 ± 4.4 g; untreated = 34.6 ± 2.7 g and KIActa1H40Y treated = 22.6 ± 1.7 g; untreated = 23.8 ± 2.4 g; Fig. 4B). Additionally, at this older age the hindlimb muscles volume was not different between treated and untreated mice for both models (Fig. 4C).
Figure 4.
Total body mass and hindlimb muscles volume for NM mice treated with a 2% L-tyrosine supplemented diet. Total body mass was determined in 6-week old TgACTA1D286G mice (A) (untreated = 10 males, 12 females; L-tyrosine = 14 males, 17 females) receiving a 2% L-tyrosine supplemented diet or an untreated diet, as well as C57BL/6 J mice (untreated = 22 males, 14 females). (B) Total body mass of 6–7 month old mice. TgACTA1D286G (untreated = 9 males, L-tyrosine = 8 males); KIActa1H40Y (untreated = 13 females, L-tyrosine = 13 females). (C) Hindlimb muscles volume for mice: male 6–7 month old TgACTA1D286G (untreated = 8; L-tyrosine = 7), female KIActa1H40Y (untreated = 13; L-tyrosine = 13). Each data point represents an individual mouse ± s.d. *p < 0.05, ***p < 0.001.
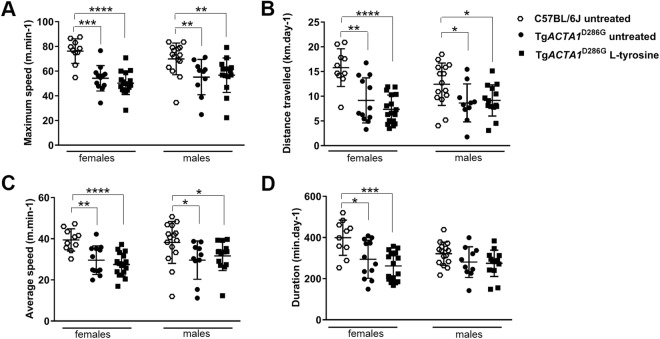
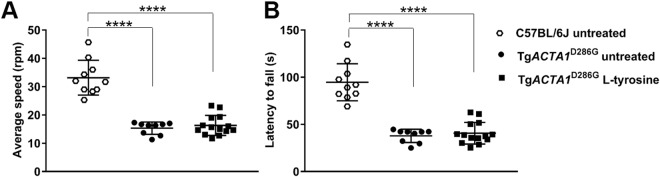
L-tyrosine treatment does not improve the voluntary running wheel or rotarod performance of TgACTA1D286G mice
As per Ravenscroft et al., (2011), the voluntary running wheel and rotarod performances of TgACTA1D286G mice are impaired compared to WT mice. TgACTA1D286G mice treated from prior to conception did not exhibit any significant improvement for any voluntary running wheel activity parameters relative to untreated mice of the same sex (Fig. 5). Similarly, none of the rotarod measurements were significantly improved for treated versus untreated male TgACTA1D286G mice (Fig. 6).
Figure 5.
Voluntary running wheel activity in 6-week old TgACTA1D286G mice receiving a 2% L-tyrosine supplemented diet from preconception compared to TgACTA1D286G and WT C57BL/6 J mice fed an untreated diet. Parameters of voluntary running wheel performance measured included (A) maximum speed (m/min), (B) distance travelled (km/d), (C) average speed (m/min), and (D) duration spent running (min/d). Untreated TgACTA1D286G mice (10 males, 12 females), L-tyrosine treated TgACTA1D286G mice (14 males, 17 females), untreated WT C57BL/6 J mice (15 males, 10 females). Each data point represents an individual mouse average calculated over days 4, 5, and 6 of voluntary wheel access ± s.d. *p < 0.05, **p < 0.01, ***p < 0.001.
Figure 6.
Accelerated rotarod performance in TgACTA1D286G and C57BL/6 J male mice. Performance on an accelerated rotarod apparatus was determined in 6-week old TgACTA1D286G male mice receiving a 2% L-tyrosine supplemented diet (n = 14) compared to TgACTA1D286G (n = 9) and C57BL/6 J (n = 10) mice fed untreated diets. (A) Average speed at fall (rpm), and (B) latency to fall (s). Each data point represents the average of 3 attempts by an individual mouse ± s.d. ****p < 0.0001.
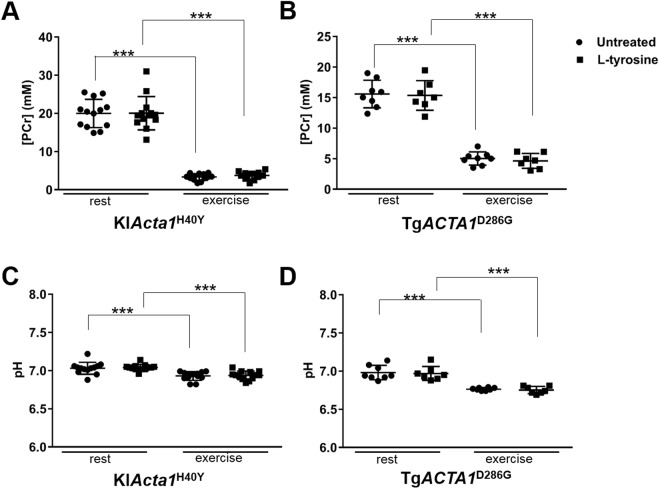
Mechanical performance and metabolism of skeletal muscles in TgACTA1D286G and KIActa1H40Y mice are not increased by L-tyrosine treatment
Absolute maximal force at 6–7 months of age was unchanged for the two NM mouse models after 1 month of treatment (Fig. 7A,B). Force production during the fatiguing protocol was comparable for the treated and untreated mice for each model (Fig. 7C,D). Consequently, the fatigue index (TgACTA1D286G treated = 0.22 ± 0.07; untreated = 0.22 ± 0.08 and KIActa1H40Y treated = 0.35 ± 0.13; untreated = 0.38 ± 0.11) and measures of resting energy metabolism ([PCr] and pHi; Fig. 8) were similar for both treatment groups for each model. During exercise, PCr consumption and pH variations were also similar between the treated and untreated mice for each model (Fig. 8).
Figure 7.
In vivo gastrocnemius skeletal muscle performance of TgACTA1D286G and KIActa1H40Y mice. Absolute maximal force production (A,B) and force production during the stimulation protocol (C,D) from 6–7 month old TgACTA1D286G (B,D) and KIActa1H40Y (A,C) mice fed either an untreated diet or a diet supplemented with 2% L-tyrosine for one month. TgACTA1D286G (untreated = 8 males, L-tyrosine = 7 males,); KIActa1H40Y (untreated = 13 females, L-tyrosine = 13 females). For (A,B) each data point represents an individual mouse ± s.d. Data points for parts (C,D) are represented by the mean force for 5 contractions of all mice in each diet group ± s.d. ***p < 0.001 (significantly different from first five contractions), which demonstrates the effect of time on muscle force performance during exercise.
Figure 8.
Changes in gastrocnemius PCr and pH during the exercise stimulation in TgACTA1D286G and KIActa1H40Y mice. [PCr] (A,B) and pH (C,D) for hindlimb skeletal muscles from 6–7 month old TgACTA1D286G (B,D) and KIActa1H40Y (A,C) mice fed either an untreated diet or supplemented with a 2% L-tyrosine diet, at rest versus at the end of the exercise stimulation protocol. The [PCr] and pH values significantly differed between rest and exercised states for each strain, however there was no significant difference detected due to L-tyrosine treatment. TgACTA1D286G (untreated = 8 males, L-tyrosine = 7 males); KIActa1H40Y (untreated = 13 females, L-tyrosine = 13 females). Each data point represents an individual mouse value expressed as mean ± s.d. ***p < 0.001.
Discussion
Prior reports of L-tyrosine supplementation to NM patients describe potential positive effects of improved skeletal muscle strength, decreased pharyngeal/oral secretions, and increased stamina/energy levels7,9,17, but lacked sufficient numbers for statistical evaluation. There are a very small number of patients (usually only one individual) with a particular mutation in any of the twelve NM genes, including nebulin and skeletal muscle α-actin, the two most common NM genes. Therefore animal models provide a means to thoroughly investigate a possible therapeutic in multiple individuals with the same genetic composition. The purpose of this study was to thoroughly evaluate the therapeutic usefulness of L-tyrosine supplementation on one of these previously reported potential benefits, skeletal muscle function, using three dominant ACTA1-NM animal models and multiple measures. We utilised one zebrafish (TgACTA1D286G-eGFP) and two mouse (TgACTA1D286G and KIACTA1H40Y) models, encompassing all known laboratory animal models of dominant ACTA1-NM. Nguyen et al.18 previously investigated the delivery of L-tyrosine to the KIACTA1H40Y NM mouse model. In terms of skeletal muscle function, the methodology used by Nguyen et al.18 produced an improvement in the number of ambulations over 20 mins after ten days of treatment, but no improvement after one month of treatment. Conversely, forearm strength was not increased after the shorter treatment period, but was after one month of L-tyrosine treatment. A reduction in weakened eye muscles of KIACTA1H40Y mice was also detected after one month of treatment18.
Our L-tyrosine dosing regimes only partially overlapped with Nguyen et al., and were carefully chosen based on our aim to provide the best prospect of detecting a correction of skeletal muscle dysfunction due to ACTA1-NM. As such, one hypothesis we made was that the highest safe dose of L-tyrosine for both zebrafish and mouse would have the maximum likelihood of improving skeletal muscle dysfunction of the respective NM animal models. Therefore, we established the greatest dose of L-tyrosine that could be delivered without overt detriment to WT zebrafish or mice.
We first investigated the safety of increased L-tyrosine levels for WT zebrafish and determined that higher concentrations of L-tyrosine significantly reduced survival and swimming performance. These findings suggest that the potential toxicity of high L-tyrosine dosing should be considered for humans supplementing with this amino acid, for whatever therapeutic reason. For the zebrafish aspect of our study, we utilised the highest concentration of L-tyrosine that did not produce these negative outcomes (10 μM). Nevertheless, the L-tyrosine treated TgACTA1D286G-eGFP zebrafish did not exhibit any improvement in the usually impaired swimming performance (distance travelled). Similarly, treated WT fish did not demonstrate any benefit of L-tyrosine supplementation on this parameter, suggesting no increase in the function of normal skeletal muscle.
Secondly, we supplemented regular mouse feed with 3 levels of L-tyrosine to determine the highest safe dose for WT mice. We chose the delivery method to be via feed to allow for a more sustained L-tyrosine dose, and a route that could be delivered to mouse pups in utero and in the postnatal phase (treatment timing described more below). The addition of both 4% and 8% L-tyrosine was associated with deleterious side effects in WT mouse mothers as well as their pups, when the feed was supplemented from pre-conception. Our pilot toxicity study in mice was not exhaustive or extensive, yet resulted in high mortality rates for two conditions. These adverse findings with the 4% and 8% doses, especially in combination with the findings from the zebrafish toxicity analysis, provide sufficient reason to highlight possible caution for humans receiving high doses of L-tyrosine.
Tyrosine related toxicity, deleterious effects and weight loss has been previously reported in the literature19–24. A potential explanation for the deleterious effects observed in mice receiving higher doses of L-tyrosine may be due to L-tyrosine being a precursor for brain catecholamines. Previous mouse studies report direct correlations between aggressive activity and brain catecholamines in mice25 with the effects proposed due to the prevention of NE depletion1. Aggressive behaviour, defined by the number of territorial-induced attacks, was reported in previously unstressed rodents receiving a diet supplemented with 4% L-tyrosine when they were later put under stress4. The authors postulated a reciprocal relationship between dopamine and NE plus serotonin for the facilitation of aggressive behaviour and suggested that aggressive behaviour may be related to lower brain NE and serotonin levels relative to dopamine4. Aggression by the mother may have been the cause of death for some of the mouse pups on the 4% and 8% supplemented doses in our study.
As no overtly deleterious side effects were seen with 2% L-tyrosine dietary supplementation to WT mice, this dose was pursued for the efficacy studies with the ACTA1-NM mouse models. The 2% L-tyrosine dose significantly increased the free L-tyrosine levels in sera (>55%) and quadriceps muscle (45%) of treated mice. Other studies determined serum tyrosine levels in rats receiving either a 2% or 5% casein diet for 14 days (of 40 ± 3 nmol/ml and 86 ± 8 nmol/ml respectively)26. The level of sera L-tyrosine detected in untreated TgACTA1D286G mice (52.7 ± 7.8 nmol/ml) in this study is in accordance with these previous reports. A paucity of data exist for free L-tyrosine levels in rodent skeletal muscles, although baseline levels of L-tyrosine in other tissues (retina, 0.25 nmol/mg; hypothalamus, 0.55 nmol/mg) have been established for rats26. The mean value for L-tyrosine in quadriceps muscle of untreated mice we determined (0.089 ± 0.021 nmol.mg−1) was less than these levels.
We performed a two-pronged investigation with the 2% L-tyrosine supplemented feed and the NM mouse models, to evaluate pre-birth versus later-onset treatment. We reasoned that if the pre-birth experimental arm established breeding mice on the diet fortified with the highest safe L-tyrosine level and continued the diet through the postnatal and post-wean periods, all offspring conceived would receive the greatest dose and duration of L-tyrosine exposure. Amino acids are known to cross the epithelium of the placental barrier by active transport via specific transporters in syncytiotrophoblast plasma membranes27, and are readily detectable in murine breast milk28. Consequently, this L-tyrosine regime would presumably provide the best possible opportunity for prevention/improvement of the skeletal muscle phenotypes attributed to their NM disease if L-tyrosine were therapeutic for this parameter. A well-known example whereby taking supplements prenatally/throughout gestation has significant therapeutic effects is folic acid in the prevention of neural tube defects such as spina bifida29. TgACTA1D286G mice treated with the pre-birth 2% L-tyrosine supplementation regime until 7 weeks of age demonstrated no improvement in bodyweight, voluntary exercise and rotarod capacity deficits previously reported for this NM model30. In fact, L-tyrosine treated 7 week old male TgACTA1D286G mice weighed significantly less than untreated male mice, perhaps indicative of a negative consequence of the treatment.
Our second experimental arm with the murine NM models assessed the 2% L-tyrosine dose but with a delivery regime that started in older mice at 5 to 6 months of age and continued for one month. This time point was one at which the disease phenotype was manifesting in both NM mouse models. This experimental arm was included to determine whether a later onset treatment could be efficacious, although our hypothesis was that earlier treatment commencement would provide optimal therapeutic opportunity. The treatment duration of one month is the same that Nguyen et al. previously reported for the successful treatment of KIActa1H40Y mice18. However, unlike Nguyen et al., we did not detect significant improvements in any skeletal muscle function we measured in response to dietary treatment with 2% L-tyrosine for same KIActa1H40Y model previously tested, or for the TgACTA1D286G model.
Potential factors that may account for the discrepancies between the findings from the Nguyen et al. study and the results described here are the different methods of L-tyrosine delivery, and how the disease phenotype was measured. Our main dosing methodology was determined with the rationale of using (i) the highest safe dose of L-tyrosine, and (ii) the earliest delivery commencement. In mice, the 2% L-tyrosine dose supplemented to feed significantly increased the free L-tyrosine levels in sera (>55%) and quadriceps muscle (45%) of treated mice, confirming our dosing regime was effective at increasing tyrosine levels.
As Nguyen et al. did not report L-tyrosine levels in sera or skeletal muscles from KIActa1H40Y mice given 25 mg/d of L-tyrosine via syringe directly into the mouth, we are not able to provide a direct comparison as to the effectiveness of the different dosing routes in raising L-tyrosine levels across the two studies. However the dose of L-tyrosine delivered to the mice appears approximately equivalent. We calculated that mice consuming the 2% L-tyrosine supplemented feed would have received a dose ranging from ~60–90 mg/d (based on the daily intake of 3–4.5 g/d for adult ACTA1-NM mice that we determined, which fits with the published murine average daily food consumption range of adolescent mice being from 3.1–6.3 g/d)31. Moreover, if we normalise this dose intake to bodyweight using the average weight for mice (35 g) that were treated at 6 months of age, this equates to 0.17–0.25% of total bodyweight. Nguyen et al. reported a similar dose intake of 0.16% of total bodyweight (based on an average weight of 15 g and mice receiving 25 mg/d), and therefore the daily intake of L-tyrosine for the KIActa1H40Y mice was similar in the two studies, however was more sustained in the current investigations.
Our study thoroughly assessed the function of skeletal muscle in the zebrafish and mouse models to determine any improvement of impaired function due to NM after L-tyrosine treatment. For mice, we evaluated the ability to voluntary exercise over a consecutive 6-day period, rotarod performance (indicative of grip strength, balance and motor coordination), in vivo gastrocnemius muscle force production, magnetic resonance spectroscopy and metabolism of muscle. Contrastingly, in the previous assessment of L-tyrosine delivery to KIActa1H40Y mice the number of ambulations over a 20-minute period, forearm strength and the horizontal and vertical eyelid separation were measured as the indicators of skeletal muscle function18. Our study also assessed bodyweight, and hindlimb muscle volume by magnetic resonance imaging, indicative of skeletal muscle integrity. Finally, we did not determine the percentage of skeletal muscle fibres with nemaline bodies, as the lack of association of these pathological features with skeletal muscle function and disease severity in patients is well documented11,12. With the extensive range of functional tests performed in this study, it is extremely likely that any benefit in skeletal muscle function as a result of the L-tyrosine treatment regimes would have been detected.
In conclusion, we determined the highest safe concentrations of L-tyrosine for dosing WT zebrafish (water) and mice (dietary supplementation), noting greater concentrations had deleterious effects. The dose and delivery methodology evaluated in the dominant ACTA1-NM mouse models significantly increased the free L-tyrosine levels in the sera and quadriceps of TgACTA1D286G mice. Nevertheless, the maximal safe doses utilised had no positive effect on a range of functional parameters of skeletal muscles for TgACTA1D286G-eGFP zebrafish when added from 24 hpf, nor for the ACTA1-NM mice when added continuously from pre-conception (TgACTA1D286G), or for one month from 5 to 6 months of age (TgACTA1D286G and KIActa1H40Y). The amassed data from our multi-pronged evaluation study demonstrate that supplementation of L-tyrosine using the regimes we trialled did not have therapeutic impact on skeletal muscle function in ACTA1-NM animal models. Nevertheless, our study does not exclude the potential that L-tyrosine might (i) improve skeletal muscle functions impaired by NM, when delivered via different treatment regimes, (ii) reduce other symptoms (such as oral secretions and the ability to swallow) that could provide assistance to patients, and (iii) have benefit for other genetic causes of NM. However, our findings highlight the imperative to further pursue novel therapies for ACTA1-NM.
Methods
Animal ethics statement
All animal experiments were performed in agreement with the guidelines of the respective countries (National Health and Medical Research Council of Australia, French guidelines for animal care, European convention for the protection of vertebrate animals used for experimental purposes, and institutional guidelines). Institutional approval was granted from the respective animal ethics committees (Animal Resources Centre, Monash University, Aix-Marseille University).
Zebrafish NM model, TgACTA1D286G-eGFP)
Zebrafish were maintained according to standard protocols32. Zebrafish strains used were Tg(βAct:loxP-mCherry-pA-loxP:Hs.ACTA1D286G-eGFP) and Tg(Actc1b:iCre)33. Crossing of these strains results in the Tg(βAct:loxP-mCherrypA-loxP:Hs.ACTA1D286G-eGFP) strain, shortened to TgACTA1D286G-eGFP. For tyrosine treatment of the zebrafish NM model, Tg(βAct:loxP-mCherry-pA-loxP:Hs.ACTA1D286G-eGFP) fish were crossed with Tg(Actc1b:iCre) fish and their progeny were sorted for eGFP and mCherry fluorescence as per33. TgACTA1D286G-eGFP fish as well as their control WT siblings (consisting of Tg(Actc1b:iCre) and Tg(βAct:loxP-mCherry-pA-loxP:Hs.ACTA1D286G-eGFP) fish) were treated from 24 hpf until 6 dpf with 10μM L-tyrosine disodium salt hydrate or H2O supplemented embryo media, with the media changed daily.
L-tyrosine dosing of the zebrafish NM model
For toxicology testing, 30 WT Tübingen zebrafish were placed in E3 embryo media and treated with increasing doses from 0.1 μM to 10 mM of L-tyrosine disodium salt hydrate (T1145, Sigma, Australia) dissolved in H2O. Zebrafish were treated from 24 hpf until 6 dpf. Supplemented embryo media was made fresh and changed daily. Zebrafish were monitored for survival and heart rate as indicators of toxicity. For controls, H2O was added to the embryo media instead of L-tyrosine. Four independent treatments were performed for each experiment with 30 fish per treatment.
Zebrafish swimming assays and resting heart rate determination
The resting heart rates were measured at 2 dpf by counting the number of heart beats in 10 sec. Heart rate measurements were performed in triplicate with 10 fish per experiment. Assay of swimming ability, as well as the subsequent data analyses performed on 6 dpf WT zebrafish treated with increasing doses of L-tyrosine, TgACTA1D286G-eGFP and their control WT siblings treated with 10 μM L-tyrosine were as per34. Total voluntary distance travelled in a 10-minute period in the dark was measured in mm using zebraboxes (Viewpoint Life Sciences). The values for wild type zebrafish treated with increasing doses of L-tyrosine were normalised to the average of the H2O treated fish in the same replicate. TgACTA1D286G-eGFP and their control WT siblings were normalised to the average of a pooled sample of H2O treated Tg(βAct:loxP-mCherry-pA-loxP:Hs.ACTA1D286G-eGFP) and Tg(Actc1b:iCre) fish in the same replicate, since there was no significant difference in the locomotion observed between these two control groups.
For swimming assays on WT zebrafish, four independent treatments were performed per experiment with 24 fish per treatment. For swimming assays on TgACTA1D286G-eGFP and their control WT siblingS (consisting of a pooled sample of Tg(βAct:loxP-mCherry-pA-loxP:Hs.ACTA1D286G-eGFP) and Tg(Actc1b:iCre) fish), five independent treatments were performed per experiment with 16–39 fish per treatment (238 TgACTA1D286G-eGFP fish in total). Based on the pooled SD of the tyrosine and water treated TgACTA1D286G-eGFP fish this gave us 0.8 power at 0.05 significance to detect an improvement of 52%. For heart rate and swimming assays all treatments were blinded and randomized to avoid experimental bias. Once the testing and analyses were completed the treatments groups were revealed.
Mouse NM models TgACTA1D286G and KIACTA1H40Y and control mouse lines
The NM mouse models used were the TgACTA1D286G+/+ (abbreviated to TgACTA1D286G)30 and KIActa1H40Y+/− (abbreviated to KIActa1H40Y)18 lines. WT mouse strains were used for the initial L-tyrosine safety dosing study (FVB/NJArc), and as a statistical comparison for the TgACTA1D286G line (C57BL/6 J; the closest background strain).
Dietary L-tyrosine dosing of the NM mouse models
Mouse feed (Speciality Feeds, Glen Forrest, Australia, basal L-tyrosine level of 0.7%; SAFE, Augy, France; basal L-tyrosine level of 0.45%) contained all nutritional dietary parameters either meeting or exceeding the maintenance guidelines for rats and mice outlined by the National Research Council (US)35. Prior to evaluating the efficacy of L-tyrosine treatment, we conducted a pilot study with normal mice to compare the Australian standard feed (containing 0.7% L-tyrosine) to the same feed supplemented with an additional 2%, 4% or 8% L-tyrosine. Breeding pairs were established on their respective ad libitum diets so that all offspring mice were conceived and maintained on these until they were sacrificed at ~7 weeks of age.
Once the 2% L-tyrosine supplemented feed was established as the highest safe concentration of those tested, two dosing regimes were evaluated for their modulation of skeletal muscle disease phenotype. One regime commenced from pre-conception (e.g. dosing of breeding pairs) and continued until sacrifice at 7 weeks of age (TgACTA1D286G mice: regular ‘untreated’ feed, n = 14 males, 17 females; 2% L-tyrosine supplemented ‘treated’ feed, n = 10 males, 12 females). The other regime commenced when mice were 5 to 6 months of age and continued for 4 weeks upon which mice were tested (TgACTA1D286G male mice: treated, n = 7; untreated, n = 8; KIActa1H40Y female mice: treated, n = 13; untreated, n = 13). Average weekly feed intake per cage was determined by weighing feed each week for 3 or more weeks prior to addition of the L-tyrosine supplemented feed and then for every week during the 4-week exposure to the treatment. An average daily weight of feed consumed per mouse was then calculated.
Quantification of L-tyrosine levels in plasma and skeletal muscles of NM mouse models
Blood was collected from L-tyrosine treated and non-treated mice via cardiac puncture at euthanasia at ~7 weeks of age. Immediately afterwards, quadriceps femoris muscles were excised, snap frozen in liquid nitrogen and stored at −80 °C. The free L-tyrosine concentration was determined using liquid chromatography/mass spectrometry (LC/MS; University of Western Australia, Centre for Metabolomics, Perth, Australia). Quadriceps femoris samples were thawed from storage at −80 °C and weighed prior to being homogenised with ceramic beads in 500 µl of 0.2 M perchloric acid36. Sample clean up and derivatization was performed on 100 µl of either muscle lysate or sera using an EZfaast™ Kit (Phenomenex). Then 0.1 µl of sample was applied to an Agilent 1290 UPLC coupled to a 6560 QQQ for the measurement of free L-tyrosine. The EZ:faast AAA-MS 4 μ column 250 × 2.0 mm provided with the kit was used and the acquisition method of the kit was followed. The internal standard was homophenylalanine. Data were acquired in positive ion mode and the transition for L-tyrosine was 396–136.
Bodyweight of NM mouse models
Male 6-week old TgACTA1D286G mice treated from pre-conception were weighed prior to individually being housed with access to Low-Profile Wireless Running Wheels (Med Associates Inc, USA) for 6 consecutive days. For both TgACTA1D286G and KIActa1H40Y mice, bodyweight was measured after 1 month of exposure to the 2% L-tyrosine supplemented diet or to the normal diet.
Voluntary running wheel analyses and rotarod assessment of TgACTA1D286G mice
The daily distance travelled, daily time spent running (summary of 1 min intervals in which at least one wheel revolution was recorded), average speed and maximum speed values were calculated. The mean values for all wheel activity traits on days 4, 5 and 6 were used for data analyses. At ~6 weeks of age, male TgACTA1D286G mice treated from pre-conception were acclimatised to the rotarod on the day prior to testing by placing mice onto the rotarod at a constant slow speed of 4 rpm for 2 minutes. The following day, mice were tested with placement on the rotarod at 4 rpm, with the rotarod gradually increased speed over 3 minutes until it reached a maximum value of 60 rpm. The test concluded after the mice had fallen off the rotarod. Each mouse was assessed three times on the same day, being allowed at least 10 minutes to rest in between assessments. The latency (time to fall from the rod) and the speed of the rotarod when the mice fell off were recorded for each test. Data were expressed as the averaged value across the three tests.
Magnetic resonance (MR) and force output measurement in TgACTA1D286G and KIActa1H40Y mice
MR investigations of TgACTA1D286G male mice treated for 4 weeks from 6–7 months of age were performed in a 4.7-Tesla (T) horizontal superconducting magnet (47/30 Biospec Avance, Bruker, Ettingen, Germany) equipped with a Bruker 120 mm BGA12SL (200 mT/m) gradient insert. Investigations of similarly treated 6–7 months of age KIActa1H40Y female mice were performed at 11.75 T on a vertical Bruker Avance 500 MHz.89 mm−1 wide-bore imager (Bruker, Ettlingen, Germany), equipped with high-performance actively shielded gradients (1 T/m maximum gradient strength, 9 kT.m−1.s−1 maximum slew rate) and interfaced with Paravision 5.1. A transmit/receive volume RF coil (birdcage, diameter Ø = 3 cm, homogenous length L = 5 cm, Micro 2.5 Probe, Bruker, Ettlingen, Germany) was used for image acquisition.
Mice were anaesthetized and individually placed supine in a home-built cradle specially designed for the strictly non-invasive functional investigation of the left hindlimb muscles. A home-built facemask was incorporated into the cradle and was used to maintain prolonged anesthesia throughout the experiment. The hindlimb was centered inside a 1H imaging coil and the belly of the gastrocnemius muscle was located above a 31P-magnetic resonance spectroscopy (MRS) surface coil. The foot was positioned on the pedal of the ergometer with a 90° flexion ankle joint. Skeletal muscle contractions were achieved by transcutaneous electrical stimulation using two rod-shaped surface electrodes integrated in the cradle and connected to an electrical stimulator (type 215/T; Hugo Sachs Elektronik-Harvard Apparatus GmbH, March-Hugstetten, Germany). One electrode was placed at the heel level and the other one was located just above the knee joint. Isometric force was measured with a home-built ergometer consisting of a foot pedal coupled to a force transducer. The analog electrical signal from the force transducer was amplified with a home-built amplifier (Operational amplifier AD620; Analog Devices, Norwood, MA, USA), converted to a digital signal, monitored and recorded on a personal computer using the Powerlab 35/series system (AD Instruments, Oxford, United Kingdom).
High-resolution MR images (MRI) were acquired at rest to obtain information about anatomy (i.e. hindlimb muscles volume). For the TgACTA1D286G mice ten contiguous axial slices (thickness = 1 mm), covering the region from the knee to the ankle, were acquired at rest using a spin echo sequence (echo time (TE) = 18.2 ms; repetition time (TR) = 1000 ms; number of repetition (NEX) = 2; field of view (FOV) = 30 × 30 mm; matrix size = 256 × 256; acquisition time = 8 min 32 s). For the KIActa1H40Y mice fifteen contiguous axial slices (thickness = 0.5 mm), covering the region from the knee to the ankle, were acquired at rest using a gradient echo sequence (TE = 1.5 ms; TR = 189 ms; NEX = 16; FOV = 20 × 20 mm; matrix size = 128 × 128; acquisition time = 6 min 27 s). Images were analyzed with FSLview (FMRIB, Oxford, MS). Regions of interest (ROI) were drawn in the two slices located on the proximal and distal parts of the hindlimb by manually tracing the border of the anatomic cross sectional area of the whole hindlimb muscles. Thereafter, the segmentations of the missing intermediate slices were automatically interpolated37. The volume of the hindlimb muscles was calculated (mm3) as the sum of the volume of the six consecutive largest slices for the TgACTA1D286G mice or of the nine consecutive largest slices for the KIActa1H40Y mice.
For the measurement of force output, non-invasive transcutaneous electrical stimulation was first elicited with square-wave pulses (0.5 ms duration) on the gastrocnemius muscle of 6–7 month old mice after 4 weeks of dietary treatment. The individual maximal stimulation intensity was determined by progressively increasing the stimulus intensity until there was no further peak twitch force increase. Plantar flexion force was assessed in response to a 100 Hz tetanic stimulation (duration = 0.75 s) and during a fatigue protocol (80 contractions; 40 Hz; 1.5 s on, 6 s off). The peak force of each contraction was measured. Regarding the fatigue protocol, the corresponding tetanic force was averaged every 5 contractions. A fatigue index corresponding to the ratio between the last five and the first five contractions was determined. The resulting force was divided by the volume of the corresponding hindlimb muscles (see above) in order to obtain specific force (in mN.mm−3).
MRS evaluation and metabolic analyses of skeletal muscles from TgACTA1D286G and KIActa1H40Y mice
Metabolic changes were investigated using 31P-MRS at rest and during the fatiguing protocol. Spectra from the gastrocnemius region were continuously acquired at rest and throughout the fatigue protocol. A total of 497 free induction decays (FID) were acquired (TR = 2 s). Data were processed using proprietary software developed using IDL (Interactive Data Language, Research System, Inc., Boulder, CO, USA). The first 180 FID were acquired at rest and summed together. The next 317 FID were acquired during the stimulation period and summed together. Relative concentrations of high-energy phosphate metabolites (phosphocreatine (PCr), inorganic phosphate (Pi) and ATP) were obtained by a time-domain fitting routine using the AMARES-MRUI Fortran code and appropriate prior knowledge of the ATP multiplets. Intracellular pH (pH) was calculated from the chemical shift of the Pi signal relative to PCr38.
Statistics
Statistical analyses for experiments in TgACTA1D286G mice and zebrafish were performed using GraphPad Prism 7. All phenotypic traits measured were tested using a nonparametric t-test (Mann-Whitney) or a two-way ANOVA. Unequal variances were assumed and all data were tested for normal distribution and passed using D’Agnostino and Perron’s test for Gaussian distribution. All reported sample sizes were powered to detect statistically significant differences in all parameters measured.
Statistical analyses for experiments with 6–7 month-old TgACTA1D286G and KIActa1H40Y mice were performed with the Statistica software version 9 (StatSoft, Tulsa, OK, USA). Normality was checked using a Kolmogorov-Smirnov test. Two-factor (group x contraction number) analysis of variance (ANOVA) with repeated measures on contraction number were used to compare force production. When a main effect or a significant interaction was found, Tukey’s HSD post-hoc analysis was used. One-way ANOVA was used to compare PCr consumption, Pi production and pHi. Unpaired t-tests were used for bodyweight, skeletal muscles volume, fatigue index and maximal force comparison. For all mice data shown, values are presented as the mean ± standard deviation, with the mean ± standard error being reported for all data collected in zebrafish.
Acknowledgements
We thank the staff at the Animal Resources Centre. Some analysis for this study was performed by the Centre for Microscopy, Characterisation and Analysis (Metabolomics Australia) and was supported by infrastructure funding from the Western Australian State Government in partnership with the Australian Federal Government, through the National Collaborative Research Infrastructure Strategy (NCRIS). This study was funded by the Association Française contre les Myopathies (trampoline grant #18207, JG), and by the Auism Foundation (NL). KN was supported by an Australian Research Council Future Fellowship (FT100100734), NL a National Health and Medical Research Council (NHMRC) Principal Research Fellowship (APP1002147), AM an Australian Postgraduate Award, and TS an MDA Development Grant (APP381325) and an AFM Postdoctoral Fellowship (APP19853). The creation of the TgACTA1D286G-eGFP zebrafish model was supported by NHMRC project grant APP1010110.
Author Contributions
All author (s) reviewed the manuscript and figures. Conceptualization: A.M., C.G., T.S., N.L., R.B., J.G., K.N.; methodology: A.M., C.G., T.S., C.V., A.O., D.H., R.B., J.G., K.N.; experimental investigation: A.M., C.G., T.S., E.M., D.H.; formal analysis: A.M., C.G., T.S., A.O., J.G.; writing – original draft preparation: A.M., C.G., T.S., J.G., K.N.; writing – review and editing: A.M., C.G., T.S., E.M., C.V., A.O., D.H., D.B., N.L., R.B., J.G., K.N.; Figure preparation- Figures 1–2 T.S., R.B.; Figures 3, 5, 6 A.M., K.N., Figure 4 A.M., K.N., C.S., J.G., Figures 7–8 C.S., J.G.: funding acquisition: T.S., N.L., R.B., J.G., K.N.
Competing Interests
The authors declare no competing interests.
Footnotes
Adriana M. Messineo, Charlotte Gineste, and Tamar E. Sztal contributed equally to this work.
Robert J. Bryson-Richardson, Julien Gondin and Kristen J. Nowak jointly supervised this work.
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Deijen, J. Tyrosine in Nutritional Neuroscience (ed. Prasad, C.) 363–382 (CRC Press, 2005).
- 2.Banderet LE, Lieberman HR. Treatment with tyrosine, a neurotransmitter precursor, reduces environmental stress in humans. Brain Res Bull. 1989;22:759–762. doi: 10.1016/0361-9230(89)90096-8. [DOI] [PubMed] [Google Scholar]
- 3.Luckose F, Pandey MC, Radhakrishna K. Effects of amino acid derivatives on physical, mental, and physiological activities. Crit Rev Food Sci Nutr. 2015;55:1793–1807. doi: 10.1080/10408398.2012.708368. [DOI] [PubMed] [Google Scholar]
- 4.Brady K, Brown JW, Thurmond JB. Behavioral and neurochemical effects of dietary tyrosine in young and aged mice following cold-swim stress. Pharmacol Biochem Behav. 1980;12:667–674. doi: 10.1016/0091-3057(80)90146-X. [DOI] [PubMed] [Google Scholar]
- 5.Lehnert H, Reinstein DK, Strowbridge BW, Wurtman RJ. Neurochemical and behavioral consequences of acute, uncontrollable stress: effects of dietary tyrosine. Brain Res. 1984;303:215–223. doi: 10.1016/0006-8993(84)91207-1. [DOI] [PubMed] [Google Scholar]
- 6.Kabuki Y, Mizobe Y, Yamada S, Furuse M. Dietary l-tyrosine alleviates the behavioral alterations induced by social isolation stress in mice. Brain Res Bull. 2009;80:389–396. doi: 10.1016/j.brainresbull.2009.08.014. [DOI] [PubMed] [Google Scholar]
- 7.Kalita D. A new treatment for congenital nonprogressive nemaline myopathy. J Orthomol Med. 1989;4:5. [Google Scholar]
- 8.Wallgren-Pettersson C, Laing NG. 109th ENMC International Workshop: 5th workshop on nemaline myopathy, 11th-13th October 2002, Naarden, The Netherlands. Neuromuscul Disord. 2003;13:501–507. doi: 10.1016/S0960-8966(03)00007-5. [DOI] [PubMed] [Google Scholar]
- 9.Ryan MM, et al. Dietary L-tyrosine supplementation in nemaline myopathy. J Child Neurol. 2008;23:609–613. doi: 10.1177/0883073807309794. [DOI] [PubMed] [Google Scholar]
- 10.Shy GM, Engel WK, Somers JE, Wanko T. Nemaline Myopathy. A New congenital myopathy. Brain. 1963;86:793–810. doi: 10.1093/brain/86.4.793. [DOI] [PubMed] [Google Scholar]
- 11.Agrawal PB, et al. Heterogeneity of nemaline myopathy cases with skeletal muscle alpha-actin gene mutations. Ann Neurol. 2004;56:86–96. doi: 10.1002/ana.20157. [DOI] [PubMed] [Google Scholar]
- 12.Ryan MM, et al. Clinical course correlates poorly with muscle pathology in nemaline myopathy. Neurology. 2003;60:665–673. doi: 10.1212/01.WNL.0000046585.81304.BC. [DOI] [PubMed] [Google Scholar]
- 13.Nowak, K. J., Davis, M. R., Wallgren-Pettersson, C., Lamont, P. J. & Laing, N. G. Clinical utility gene card for: Nemaline myopathy - update 2015. Eur J Hum Genet23, 10.1038/ejhg.2015.12 (2015). [DOI] [PMC free article] [PubMed]
- 14.Malfatti E, et al. A premature stop codon in MYO18B is associated with severe nemaline myopathy with cardiomyopathy. J Neuromuscul Dis. 2015;2:219–227. doi: 10.3233/JND-150085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Miyatake S, et al. Biallelic mutations in MYPN, encoding myopalladin, are associated with childhood-onset, slowly progressive nemaline myopathy. Am J Hum Genet. 2017;100:169–178. doi: 10.1016/j.ajhg.2016.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nowak KJ, Ravenscroft G, Laing NG. Skeletal muscle alpha-actin diseases (actinopathies): pathology and mechanisms. Acta Neuropathol. 2013;125:19–32. doi: 10.1007/s00401-012-1019-z. [DOI] [PubMed] [Google Scholar]
- 17.Olukman O, Calkavur S, Diniz G, Unalp A, Atlihan F. Nemaline myopathy in a newborn infant: a rare muscle disorder. Neurol Neurochir Pol. 2013;47:493–498. doi: 10.5114/ninp.2013.38229. [DOI] [PubMed] [Google Scholar]
- 18.Nguyen MA, et al. Hypertrophy and dietary tyrosine ameliorate the phenotypes of a mouse model of severe nemaline myopathy. Brain. 2011;134:3516–3529. doi: 10.1093/brain/awr274. [DOI] [PubMed] [Google Scholar]
- 19.Boctor AM, Harper AE. Tyrosine toxicity in the rat: effect of high intake of p-hydroxyphenylpyruvic acid and of force-feeding high tyrosine diet. J Nutrition. 1968;95:535–540. doi: 10.1093/jn/95.4.535. [DOI] [PubMed] [Google Scholar]
- 20.Alam SQ, Becker RV, Stucki WP, Rogers QR, Harper AE. Effect of threonine on the toxicity of excess tyrosine and cataract formation in the rat. J Nutrition. 1966;89:91–96. doi: 10.1093/jn/89.1.91. [DOI] [PubMed] [Google Scholar]
- 21.Shibui Y, Manabe Y, Kodama T, Gonsho A. 13-week repeated dose toxicity study of L-tyrosine in rats by daily oral administration. Food Chem Toxicol. 2016;87:55–64. doi: 10.1016/j.fct.2015.11.017. [DOI] [PubMed] [Google Scholar]
- 22.Lewis SA, Lyon IC, Elliott RB. Outcome of pregnancy in the rat with mild hyperphenylalaninaemia and hypertyrosinaemia: implications for the management of “human maternal PKU”. J Inherit Metab Dis. 1985;8:113–117. doi: 10.1007/BF01819292. [DOI] [PubMed] [Google Scholar]
- 23.Muramatsu K, Arito T, Tsuda H. Effect of individual amino acid supplements on the toxicity of excess tyrosine in rats. J Nutr Sci Vitaminol. 1976;22:397–403. doi: 10.3177/jnsv.22.397. [DOI] [PubMed] [Google Scholar]
- 24.Muramatsu K, Takei M, Nakamura K. Effect of dietary protein on tyrosine toxicity in the rat. J Nutrition. 1975;105:439–446. doi: 10.1093/jn/105.4.439. [DOI] [PubMed] [Google Scholar]
- 25.Thurmond JB, Brown JW. Effect of brain monoamine precursors on stress-induced behavioral and neurochemical changes in aged mice. Brain Res. 1984;296:93–102. doi: 10.1016/0006-8993(84)90514-6. [DOI] [PubMed] [Google Scholar]
- 26.Fernstrom MH, Fernstrom JD. Effect of chronic protein ingestion on rat central nervous system tyrosine levels and in vivo tyrosine hydroxylation rate. Brain Res. 1995;672:97–103. doi: 10.1016/0006-8993(94)01342-F. [DOI] [PubMed] [Google Scholar]
- 27.Jansson T. Amino acid transporters in the human placenta. Pediatr Res. 2001;49:141–147. doi: 10.1203/00006450-200102000-00003. [DOI] [PubMed] [Google Scholar]
- 28.Rassin DK, Sturman JA, Guall GE. Taurine and other free amino acids in milk of man and other mammals. Early Hum Dev. 1978;2:1–13. doi: 10.1016/0378-3782(78)90048-8. [DOI] [PubMed] [Google Scholar]
- 29.MRC Vitamin Study Research Group Prevention of neural tube effects: Results of the Medical Research Council Vitamin Study. Lancet. 1991;338:131–137. doi: 10.1016/0140-6736(91)90133-A. [DOI] [PubMed] [Google Scholar]
- 30.Ravenscroft G, et al. Mouse models of dominant ACTA1 disease recapitulate human disease and provide insight into therapies. Brain. 2011;134:1101–1115. doi: 10.1093/brain/awr004. [DOI] [PubMed] [Google Scholar]
- 31.Bachmanov AA, Reed DR, Beauchamp GK, Tordoff MG. Food intake, water intake, and drinking spout side preference of 28 mouse strains. Behavior Genetics. 2002;32:435–443. doi: 10.1023/A:1020884312053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Westerfield, M. The Zebrafish Book. A Guide for the Laboratory Use of Zebrafish (Danio rerio). 5 edn, (University of Oregon Press, 2007).
- 33.Sztal TE, et al. Zebrafish models for nemaline myopathy reveal a spectrum of nemaline bodies contributing to reduced muscle function. Acta Neuropathol. 2015;130:389–406. doi: 10.1007/s00401-015-1430-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sztal, T. E., Ruparelia, A. A., Williams, C. & Bryson-Richardson, R. J. Using touch-evoked response and locomotion assays to assess muscle performance and function in zebrafish. J Vis Exp, 10.3791/54431 (2016). [DOI] [PMC free article] [PubMed]
- 35.National Research Council (US) Committee for the update of the guide for the care and use of laboratory animals. Guide for the Care and Use of Laboratory Animals. 8th edn, (National Academies Press, 2011). [PubMed]
- 36.Hamasu K, et al. L-proline is a sedative regulator of acute stress in the brain of neonatal chicks. Amino Acids. 2009;37:377–382. doi: 10.1007/s00726-008-0164-0. [DOI] [PubMed] [Google Scholar]
- 37.Ogier, A., Sdika, M., Fouré, A., Le Troter, A. & Bendahan, D. Individual muscle segmentation in MR Images: a 3D propagation through 2D non-linear registration approaches in 39th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (Jeju Island, Korea, 2017). [DOI] [PubMed]
- 38.Moon RB, Richards JH. Determination of intracellular pH by 31P magnetic resonance. J Biol Chem. 1973;248:7276–7278. [PubMed] [Google Scholar]