Abstract
Nonalcoholic fatty liver disease (NAFLD) is the commonest chronic liver disease and affects a considerable proportion of the general population. NAFLD is independently associated with increased risk for cardiovascular events, particularly coronary heart disease. Importantly, even though NAFLD is more prevalent in patients with major cardiovascular risk factors (e.g., type 2 diabetes mellitus, obesity and hypertension), the association between NAFLD and cardiovascular disease appears to be independent of these risk factors. However, NAFLD also appears to increase the risk for ischemic stroke, a leading cause of mortality and long-term disability worldwide. It also appears that nonalcoholic steatohepatitis is more strongly related to the risk of ischemic stroke than isolated hepatic steatosis. Moreover, emerging data suggest that patients with NAFLD experience more severe ischemic stroke and have more unfavorable prognosis after an acute ischemic stroke in terms of functional dependency and short- and long-term mortality. These associations have major public health implications, since ischemic stroke is the second leading cause of death worldwide and an important cause of long-term disability. The aim of the present review is to summarize the current knowledge regarding the relationship between NAFLD and ischemic stroke incidence, severity and outcome. Given these associations, it might be useful to evaluate patients with acute ischemic stroke for the presence of NAFLD and to manage those with NAFLD more aggressively.
Keywords: Nonalcoholic fatty liver disease, Ischemic stroke, Risk, Incidence, Severity, Outcome, Functional dependency
Core tip: Accumulating data suggest that nonalcoholic fatty liver disease (NAFLD) is independently associated with increased risk for ischemic stroke, a leading cause of mortality and long-term disability worldwide. Moreover, emerging evidence shows that patients with NAFLD experience more severe ischemic stroke and have more unfavorable prognosis after an acute ischemic stroke in terms of functional dependency and short- and long-term mortality.
INTRODUCTION
Nonalcoholic fatty liver disease (NAFLD) is the most frequent chronic liver disease, affects approximately 25% of the general population and is the leading cause of abnormal liver function tests[1,2]. Moreover, the prevalence of NAFLD is even higher in elderly subjects and in patients with type 2 diabetes mellitus (T2DM), obesity, hypertension and/or metabolic syndrome[2,3]. Nonalcoholic steatohepatitis (NASH), a more advanced form of NAFLD, is present in up to 10% of adults[4]. NAFLD can progress to cirrhosis, hepatocellular cancer or liver failure, and is a major cause of liver transplantation[3,5].
Several studies showed that NAFLD is a risk factor for cardiovascular disease (CVD)[6,7]. Importantly, even though NAFLD is more prevalent in patients with major cardiovascular risk factors (e.g., T2DM, obesity and hypertension), the association between NAFLD and CVD appears to be independent of these risk factors (Figure 1)[6,7].
Figure 1.
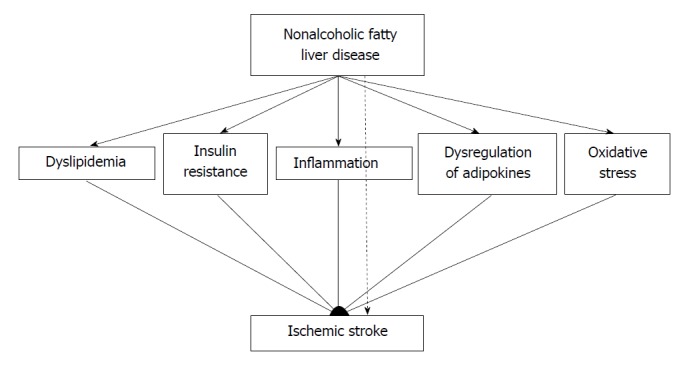
Mechanisms underpinning the association between nonalcoholic fatty liver disease and ischemic stroke (broken line suggests the independent association between nonalcoholic fatty liver disease and ischemic stroke).
In this context, accumulating data suggest that NAFLD is also associated with increased incidence of ischemic stroke. Moreover, emerging evidence suggests that NAFLD might also be related with more severe stroke and with worse outcome of patients with acute ischemic stroke. These associations have major public health implications, since ischemic stroke is the second leading cause of death worldwide and an important cause of long-term disability[8,9]. The aim of the present review is to summarize the current knowledge regarding the relationship between NAFLD and ischemic stroke incidence, severity and outcome.
NAFLD AND INCIDENCE OF ISCHEMIC STROKE
Several studies reported that elevated aminotransferase and g-glutamyltransferase (gGT) levels, which are mostly due to NAFLD, are associated with increased incidence of ischemic stroke (Table 1). In a small case-control study in 103 patients with acute ischemic stroke and 200 controls, alanine or aspartate aminotransferase levels were independently associated with increased odds ratio for ischemic stroke[10]. In a larger prospective study in 6997 men without established CVD or T2DM, gGT levels, a more specific marker of NAFLD, was independently associated with higher risk of ischemic stroke, even in subjects at low- or moderate cardiovascular risk[11]. In EUROSTROKE, a nested-case control study performed in 3 European countries (Finland, Netherlands and United Kingdom), the association between gGT levels and ischemic stroke risk appeared to be stronger in patients without T2DM[12]. Importantly, gGT appears to play a role in atherogenesis[13]. Indeed, gGT has been isolated from atheromatic plaques, macrophages and foam cells[14] and appears to contribute to atherosclerosis by inducing oxidative stress[15]. It was shown than gGT promotes oxidization of low-density lipoprotein and that it plays a crucial role in the catabolism of glutathione and the release of reactive oxygen species[16,17]. In a recent cross-sectional study, NAFLD diagnosed with ultrasonography was associated with increased prevalence of lacunar infarcts in non-obese subjects but not in obese patients[18]. In contrast, in another recent case-cohort study in 572 patients with incident ischemic stroke and 1017 controls, NAFLD defined as fatty liver index > 60 was associated with lower risk in men but there was no association in women[19]. In a meta-analysis of 9 case-control and cohort studies, NAFLD was independently associated with 2.3 times higher risk for ischemic stroke (95%CI: 1.84-2.93)[20]. The strength of this association was comparable in Caucasian and Asian patients[20]. Importantly, this association was independent of traditional cardiovascular risk factors, including dyslipidemia, obesity and T2DM[20].
Table 1.
Major studies that evaluated the association between nonalcoholic fatty liver disease and ischemic stroke
| Ref. | Design | Mean age (yr) | Follow-up | Outcome |
| [7] | Prospective observational study in 1637 healthy Japanese men/women | 47.8 | 2 yr | Higher incidence of CVD including stroke in patients with NAFLD compared with controls |
| [22] | Prospective study in 242 patients admitted with acute stroke | 66 | 2 yr | Increased risk of acute stroke, more severe stroke and worse outcome in patients with NAFLD |
| [11] | Prospective study in 6997 men with no history of CVD or diabetes mellitus | 40-59 | 24 yr | Association between gGT and higher incidence of fatal, major stroke events and total CVD mortality |
| [10] | Cross sectional study in adults with suspected acute stroke | 20-27 | Not applicable | Elevated ALP and ALT levels independently associated with higher risk of acute stroke |
| [12] | Case-control study using data from 3 European cohort studies in 13177 subjects | 40-60 | 3-8 yr | Elevated gGT levels associated with higher risk of stroke |
| [21] | Case-control study in 295 patients with acute stroke and 1942 healthy subjects | 60 | Not applicable | Liver fibrosis was associated with higher incidence of ischemic stroke |
| [20] | Meta analysis of 9 studies that examined relation of NAFLD and stroke | Not reported | Not applicable | Higher risk of ischemic stroke and hemorrhagic stroke in patients with NAFLD |
| [23] | Retrospective study in 306 patients with confirmed brainstem infractions | 65 | Not applicable | Higher incidence of brainstem infracts in patients with NAFLD |
| [24] | Study in 415 patients admitted with acute ischemic stroke | 78.8 | Duration of hospitalization | NAFLD was not associated with stroke severity at admission or outcome during hospitalization |
| [19] | Case-cohort study in 572 patients with stroke and 1017 controls | > 45 | 5.8 yr | Fatty liver index associated with increased risk for ischemic stroke in women and with lower risk in women |
| [20] | Cross-sectional study in 1277 subjects who underwent brain magnetic resonance imaging and abdominal ultrasound during check-up | > 40 yr | Not applicable | NAFLD diagnosed with ultrasonography was associated with increased prevalence of lacunar infarcts in non-obese subjects but not in obese patients |
CVD: Cardiovascular disease; gGT: G-glutamyltransferase; ALP: Alkaline phosphatase; ALT; Alanine aminotransferase; NAFLD: Nonalcoholic fatty liver disease.
It appears that NASH is more strongly related to the risk of ischemic stroke than isolated hepatic steatosis. Indeed, in a case-control study in 295 patients with acute ischemic stroke and 1942 subjects who underwent a health check-up, the degree of liver fibrosis, evaluated with transient elastography, was independently associated with increased stroke risk[21]. In contrast, isolated steatosis was not related with the risk of stroke[21].
NAFLD AND SEVERITY AND OUTCOME OF ISCHEMIC STROKE
There are very few data regarding the impact of NAFLD on the severity and outcome of ischemic stroke (Table 1). In an early prospective study in 200 patients admitted with acute ischemic stroke, NAFLD (defined as elevated aminotransferase levels in the absence of other causes) was present in 42.5% of patients[22]. Patients with NAFLD had more severe stroke at admission and worse functional outcome at discharge[22]. However, patients with NAFLD were more obese, had higher prevalence of T2DM and had higher low-density lip–oprotein cholesterol and triglyceride levels than patients without NAFLD; these differences were not adjusted for in the comparisons of stroke severity and outcome between the 2 groups[22]. In a more recent retrospective study in 306 patients with brainstem infarction, a similar prevalence of NAFLD (defined as elevated aminotransferase levels in the absence of other causes) was reported (42.5%)[23]. Patients with NAFLD had more severe stroke at admission and higher risk for neurological deterioration during hospitalization, independently of other risk factors[23]. In contrast, in a prospective study in 415 consecutive patients with acute ischemic stroke, stroke severity at admission, functional outcome at discharge and in-hospital mortality did not differ between patients with NAFLD (defined as elevated aminotransferase levels without another apparent cause) and those without NAFLD after adjustment for other cardiovascular risk factors[24]. However, only 32 patients (7.7% of the study population) had NAFLD[24]. Therefore, this study might have lacked the power to identify an association between NAFLD and stroke severity and outcome[24].
CONCLUSION
Accumulating data suggest that NAFLD is independently associated with increased risk for ischemic stroke. Moreover, it appears that patients with NAFLD experience more severe stroke and have more adverse functional outcome than patients without NAFLD. Therefore, it might be useful to evaluate patients with acute ischemic stroke for the presence of NAFLD and to manage those with NAFLD more aggressively. It remains to be established whether management of NAFLD will also reduce the risk and improve the outcome of ischemic stroke.
Footnotes
Conflict-of-interest statement: All authors declare no conflict of interest related to this publication.
Manuscript source: Invited manuscript
Peer-review started: March 28, 2018
First decision: April 13, 2018
Article in press: May 31, 2018
Specialty type: Gastroenterology and hepatology
Country of origin: Greece
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P- Reviewer: Abd-Elsalam S, Arslan N, Chen CJ S- Editor: Ji FF L- Editor: A E- Editor: Tan WW
Contributor Information
Stelina Alkagiet, First Propedeutic Department of Internal Medicine, Medical School, Aristotle University of Thessaloniki, AHEPA Hospital, Thessaloniki 54636, Greece.
Achilleas Papagiannis, First Propedeutic Department of Internal Medicine, Medical School, Aristotle University of Thessaloniki, AHEPA Hospital, Thessaloniki 54636, Greece.
Konstantinos Tziomalos, First Propedeutic Department of Internal Medicine, Medical School, Aristotle University of Thessaloniki, AHEPA Hospital, Thessaloniki 54636, Greece. ktziomalos@yahoo.com.
References
- 1.Armstrong MJ, Houlihan DD, Bentham L, Shaw JC, Cramb R, Olliff S, Gill PS, Neuberger JM, Lilford RJ, Newsome PN. Presence and severity of non-alcoholic fatty liver disease in a large prospective primary care cohort. J Hepatol. 2012;56:234–240. doi: 10.1016/j.jhep.2011.03.020. [DOI] [PubMed] [Google Scholar]
- 2.Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease-Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64:73–84. doi: 10.1002/hep.28431. [DOI] [PubMed] [Google Scholar]
- 3.Chalasani N, Younossi Z, Lavine JE, Diehl AM, Brunt EM, Cusi K, Charlton M, Sanyal AJ. The diagnosis and management of non-alcoholic fatty liver disease: practice Guideline by the American Association for the Study of Liver Diseases, American College of Gastroenterology, and the American Gastroenterological Association. Hepatology. 2012;55:2005–2023. doi: 10.1002/hep.25762. [DOI] [PubMed] [Google Scholar]
- 4.Caballería L, Pera G, Arteaga I, Rodríguez L, Alumà A, Morillas RM, de la Ossa N, Díaz A, Expósito C, Miranda D, et al. High Prevalence of Liver Fibrosis Among European Adults With Unknown Liver Disease: A Population-Based Study. Clin Gastroenterol Hepatol. 2018;16:1138–1145.e5. doi: 10.1016/j.cgh.2017.12.048. [DOI] [PubMed] [Google Scholar]
- 5.Bhala N, Angulo P, van der Poorten D, Lee E, Hui JM, Saracco G, Adams LA, Charatcharoenwitthaya P, Topping JH, Bugianesi E, et al. The natural history of nonalcoholic fatty liver disease with advanced fibrosis or cirrhosis: an international collaborative study. Hepatology. 2011;54:1208–1216. doi: 10.1002/hep.24491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Targher G, Bertolini L, Rodella S, Tessari R, Zenari L, Lippi G, Arcaro G. Nonalcoholic fatty liver disease is independently associated with an increased incidence of cardiovascular events in type 2 diabetic patients. Diabetes Care. 2007;30:2119–2121. doi: 10.2337/dc07-0349. [DOI] [PubMed] [Google Scholar]
- 7.Hamaguchi M, Kojima T, Takeda N, Nagata C, Takeda J, Sarui H, Kawahito Y, Yoshida N, Suetsugu A, Kato T, et al. Nonalcoholic fatty liver disease is a novel predictor of cardiovascular disease. World J Gastroenterol. 2007;13:1579–1584. doi: 10.3748/wjg.v13.i10.1579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mendis S, Puska P, Norrving B, editors . Globes Atlas on cardiovascular disease prevention and control. Geneva: World Health Organization; 2011. [Google Scholar]
- 9.Menken M, Munsat TL, Toole JF. The global burden of disease study: implications for neurology. Arch Neurol. 2000;57:418–420. doi: 10.1001/archneur.57.3.418. [DOI] [PubMed] [Google Scholar]
- 10.Ying I, Saposnik G, Vermeulen MJ, Leung A, Ray JG. Nonalcoholic fatty liver disease and acute ischemic stroke. Epidemiology. 2011;22:129–130. doi: 10.1097/EDE.0b013e3181feb50a. [DOI] [PubMed] [Google Scholar]
- 11.Wannamethee SG, Lennon L, Shaper AG. The value of gamma-glutamyltransferase in cardiovascular risk prediction in men without diagnosed cardiovascular disease or diabetes. Atherosclerosis. 2008;201:168–175. doi: 10.1016/j.atherosclerosis.2008.01.019. [DOI] [PubMed] [Google Scholar]
- 12.Bots ML, Salonen JT, Elwood PC, Nikitin Y, Freire de Concalves A, Inzitari D, Sivenius J, Trichopoulou A, Tuomilehto J, Koudstaal PJ, et al. Gamma-glutamyltransferase and risk of stroke: the EUROSTROKE project. J Epidemiol Community Health. 2002;56 Suppl 1:i25–i29. doi: 10.1136/jech.56.suppl_1.i25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Emdin M, Passino C, Franzini M, Paolicchi A, Pompella A. gamma-glutamyltransferase and pathogenesis of cardiovascular diseases. Future Cardiol. 2007;3:263–270. doi: 10.2217/14796678.3.3.263. [DOI] [PubMed] [Google Scholar]
- 14.Franzini M, Corti A, Martinelli B, Del Corso A, Emdin M, Parenti GF, Glauber M, Pompella A, Paolicchi A. Gamma-glutamyltransferase activity in human atherosclerotic plaques-biochemical similarities with the circulating enzyme. Atherosclerosis. 2009;202:119–127. doi: 10.1016/j.atherosclerosis.2008.03.023. [DOI] [PubMed] [Google Scholar]
- 15.Koenig G, Seneff S. Gamma-Glutamyltransferase: A Predictive Biomarker of Cellular Antioxidant Inadequacy and Disease Risk. Dis Markers. 2015;2015:818570. doi: 10.1155/2015/818570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Paolicchi A, Minotti G, Tonarelli P, Tongiani R, De Cesare D, Mezzetti A, Dominici S, Comporti M, Pompella A. Gamma-glutamyl transpeptidase-dependent iron reduction and LDL oxidation--a potential mechanism in atherosclerosis. J Investig Med. 1999;47:151–160. [PubMed] [Google Scholar]
- 17.Stark AA, Zeiger E, Pagano DA. Glutathione metabolism by gamma-glutamyltranspeptidase leads to lipid peroxidation: characterization of the system and relevance to hepatocarcinogenesis. Carcinogenesis. 1993;14:183–189. doi: 10.1093/carcin/14.2.183. [DOI] [PubMed] [Google Scholar]
- 18.Kwak MS, Kim KW, Seo H, Chung GE, Yim JY, Kim D. Non-obese fatty liver disease is associated with lacunar infarct. Liver Int. 2018;38:1292–1299. doi: 10.1111/liv.13663. [DOI] [PubMed] [Google Scholar]
- 19.Alexander KS, Zakai NA, Lidofsky SD, Callas PW, Judd SE, Tracy RP, Cushman M. Non-alcoholic fatty liver disease, liver biomarkers and stroke risk: The Reasons for Geographic and Racial Differences in Stroke cohort. PLoS One. 2018;13:e0194153. doi: 10.1371/journal.pone.0194153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hu J, Xu Y, He Z, Zhang H, Lian X, Zhu T, Liang C, Li J. Increased risk of cerebrovascular accident related to non-alcoholic fatty liver disease: a meta-analysis. Oncotarget. 2017;9:2752–2760. doi: 10.18632/oncotarget.22755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kim SU, Song D, Heo JH, Yoo J, Kim BK, Park JY, Kim DY, Ahn SH, Kim KJ, Han KH, et al. Liver fibrosis assessed with transient elastography is an independent risk factor for ischemic stroke. Atherosclerosis. 2017;260:156–162. doi: 10.1016/j.atherosclerosis.2017.02.005. [DOI] [PubMed] [Google Scholar]
- 22.Abdeldyem SM, Goda T, Khodeir SA, Abou Saif S, Abd-Elsalam S. Nonalcoholic fatty liver disease in patients with acute ischemic stroke is associated with more severe stroke and worse outcome. J Clin Lipidol. 2017;11:915–919. doi: 10.1016/j.jacl.2017.04.115. [DOI] [PubMed] [Google Scholar]
- 23.Li H, Hu B, Wei L, Zhou L, Zhang L, Lin Y, Qin B, Dai Y, Lu Z. Non-alcoholic fatty liver disease is associated with stroke severity and progression of brainstem infarctions. Eur J Neurol. 2018;25:577–e34. doi: 10.1111/ene.13556. [DOI] [PubMed] [Google Scholar]
- 24.Tziomalos K, Giampatzis V, Bouziana SD, Spanou M, Papadopoulou M, Pavlidis A, Kostaki S, Bozikas A, Savopoulos C, Hatzitolios AI. Association between nonalcoholic fatty liver disease and acute ischemic stroke severity and outcome. World J Hepatol. 2013;5:621–626. doi: 10.4254/wjh.v5.i11.621. [DOI] [PMC free article] [PubMed] [Google Scholar]


