Abstract
Introduction:
Utilization of recommended antenatal care (ANC) throughout the pregnancy period is a proven healthy behavior in reducing maternal mortalities and morbidities. The objective of this study is to identify the demand side factors that are associated with the recommended utilization of ANC services among adolescents and adult women in Bangladesh.
Method:
This study utilized cross-sectional data from latest Bangladesh Demographic and Health Survey 2014. Data of a total of 4626 adolescents and adult women were analyzed. Bivariate and multivariate analyses were performed for identifying the significant determining factors associated with the ANC services utilization.
Results:
Approximately, 32% adult and 30% adolescent women utilized the recommended ANC care. The higher educated adolescents and adult women were 8.08 times (P < .001) and 2.98 times (P < .001) more likely to receive 4 or more ANC, respectively, compared to uneducated women. The richest quintile showed higher tendency to utilize optimum ANC services and had 2.70 times (P < .05) and 6.51 times (P < .001) more likelihood to receive optimal ANC services for adolescent and adult groups, respectively, compared to poorest quintile.
Conclusion:
Other than education and income, several other factors including mass -media, place of residence, working status, and geographical variations were significantly associated with recommended ANC. These findings might help health-care programmers and policy makers for initiating appropriate policy and programs for ensuring optimal ANC coverage for all. Ensuring adequate ANC regardless of economic status and residence of pregnant women could guarantee universal maternal health-care coverage as devoted to a national strategic guideline.
Keywords: antenatal care, determinants, pregnant women, service utilization, bangladesh
Introduction
Utilization of recommended antenatal care (ANC) throughout the pregnancy period is a proven healthy behavior in reducing maternal mortalities and morbidities as well as to promote safe motherhood with improved maternal health outcome.1 Pregnancy-related complications triggered an estimated 358 000 deaths of women each year globally and mostly occurred in resource-poor settings, where maternal health-care services (MHS) utilization are considerably low and inadequate, and approximately 6 000 deaths occurred in Bangladesh.2-4 Latest Sustainable Development Goals focused to reduce the 70 maternal death per 100 000 livebirths globally within 2030.5 Bangladesh government has set a target to reduce the maternal mortality ratio from 176 to 105 per 100 000 livebirths by 20216; therefore, it is crucial for ensuring access of MHS to all pregnant women so that pregnancy-related mortality and morbidity could be reduced.7 The World Health Organization recommended to utilize at least 4 ANC visits to avoid probable pregnancy-related complications during prenatal period.8,9 Despite relatively high rates of utilizing overall ANC and better access to health facilities, the optimum number of ANC utilization (at least 4 ANC) remains low (31.2%) in Bangladesh.10,11,12 The optimum ANC coverage is even not uniformly distributed across the socioeconomic strata of the populations.12 The utilization of recommended ANC services often depends upon the availability, affordability, and quality of services; social structure; cultural beliefs as well as individual’s and household’s characteristics of the end users.13-15 Optimum ANC services could contribute to reduce maternal morbidities, mortalities, complications at birth, risk of low birth weights (<2500 g), and preterm births.16-18 There are various factors that had proven effects on ANC services utilization and often expressed as socioeconomic, demographic, and accessibility factors19 and factors related to women’s perceived quality of MHS.20
Although a number of literatures are available related to maternal health-care-related utilization and pregnancy-related outcomes, the information concerning maternal age-specific factors for ANC utilization is limited in Bangladesh context.2,7,11,16,21 Therefore, proper understanding about the various demand side factors across age groups is necessary to inform policy which might help to take proper actions to strengthen the ANC services and betterment of maternal health. The objective of this study is to identify the demand side factors that are associated with the recommended utilization of ANC services among adolescents and adult women in Bangladesh by analyzing a nationally representative data set.
Methods
Study Design
This study used latest Bangladesh Demographic and Health Survey (BDHS) 2014 data, a cross-sectional survey, based on nationally representative sample of women in childbearing age. The BDHS sample was collected using 2-stage stratified cluster sampling procedure of household. A total of 18 245 ever-married women aged 15 to 49 years were identified for the survey, and among them 17 963 respondents were interviewed, yielding a response rate was 98%. Details of sampling and data collection methods are described elsewhere.22 The information in respect to ANC was collected from all women who gave birth within the 3 years preceding the survey. In women with a history of giving more than 1 live birth preceding the 3 years of survey, only data regarding the most recent live birth were collected in the BDHS survey. For capturing age-specific variation, we considered 2 age-groups, adolescents and adult women; while women aged 15 to 19 years were considered as adolescent, those aged 20 or 20 plus were treated as adult.21,23 The inclusion criteria was (1) married at the time of survey, (2) aged between 15 and 49 years, and (3) had their most recent births within the 3 years preceding the survey. Finally, a total of 4626 women met the abovementioned criteria for inclusion, 970 were found to be adolescent women and the remaining 3656 were adults.
Statistical Analysis
Bivariate and multivariate analyses were performed for identifying factors associated with the utilization of ANC. Bivariate analyses were accomplished to examine the association between utilization of ANC and various socioeconomic and demographic characteristics of the households. The independent variables were maternal age (15-19 years and 20 or more years), women and husbands education (no education, primary, secondary, and higher), place of residence (urban and rural), household size (≤5 members per households and >5 members per households), mass media exposure (no/yes), number of children (1, 2 to 3, and 4 or more), working status (not working and working), administrative divisions (Sylhet, Barisal, Chittagong, Rajshahi, Dhaka, Khulna, and Rangpur), and economic status of the household (poorest, poorer, middle, richer, and richest) based on earlier literatures. Socioeconomic status was measured by wealth index using principle components analysis.12 In this analysis, we considered the number of ANC visits as the primary outcome variable which was recoded as “0” for no ANC, “1” for less than 4 ANC, and “2” for 4 or more ANCs. Multiple linear logistic regression was applied to assess the differential factors affecting utilization of recommended ANC service. The significant associations were measured at 5% α level (P < .05). Three groups were considered: women who did not utilize ANC care (n = 992), those who utilized less than 4 ANCs (n = 2187), and women who utilized optimal (ie, 4 and more) ANC care (n = 1447). The χ2 test of independence was used and measured in terms of P value. The findings were presented in terms of odds ratios (ORs) with 95% confidence interval (CI). All the analysis was performed using the statistical package Stata/SE 13.0.
Ethics Approval and Consent to Participate
The study analyzed a publicly available DHS data set by taking consent from the MEASURE DHS program office. Demographic and Health Survey (DHS) followed standardized data collection procedures. According to the DHS, written informed consent was obtained from women enrolled in the survey.
Results
Distribution of Maternal and Sociodemographic Characteristics
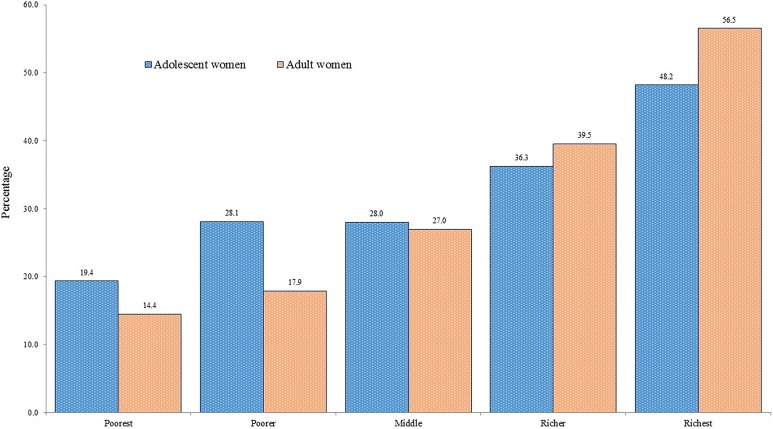
Table 1 shows the sociodemographic and socioeconomic characteristics of the participants. The average age of the women was 24.58 years (standard deviation [SD] 5.75), while the mean age of adolescent and adult women was17.75 and 26.38 years, respectively. Among both age-groups, the majority of the respondents (adolescent 58% and adult 45%) had completed secondary education and lived in rural areas (77% and 73%). The household size was also almost similar in both age-groups (Table 1). A majority (61.78%) of women in both the groups watched television and listened to radio almost regularly. Most of the women were unemployed, and only 15% adolescents and 26% of adult women were employed. Our results indicated that only 32% adult and 30% adolescent mother utilized the recommended (4 and more) ANC services (Table 2). We found that, the poorest women were more vulnerable for utilizing recommended ANC services (for both the groups), while the upper 2 quintiles (richer and richest) frequently utilized the optimal care (Figure 1).
Table 1.
Distribution of Sociodemographic and Maternal Characteristics Among Married Adolescent and Adult Women.
| Background Characteristic | 15-19 Years, n (%) | 20 Years or More, n (%) | Total, N (%) |
|---|---|---|---|
| Age, years | |||
| Mean age, mean (SD) | 17.75 (1.17) | 26.38 (5.08) | 24.58 (5.75) |
| Women’s education | |||
| No education | 47 (04.81) | 607 (16.61) | 654 (14.13) |
| Primary | 304 (31.27) | 990 (27.07) | 1293 (27.95) |
| Secondary | 563 (58.01) | 1644 (44.99) | 2208 (47.72) |
| Higher | 57 (05.90) | 414 (11.33) | 471 (10.19) |
| Husband education | |||
| No education | 171 (17.64) | 933 (25.51) | 1104 (23.86) |
| Primary | 377 (38.85) | 1009 (27.60) | 1386 (29.96) |
| Secondary | 344 (35.46) | 1125 (30.79) | 1470 (31.77) |
| Higher | 78 (08.05) | 589 (16.10) | 667 (14.41) |
| Place of residence | |||
| Urban | 227 (23.42) | 982 (26.86) | 1209 (26.14) |
| Rural | 743 (76.58) | 2673 (73.14) | 3417 (73.86) |
| Household size | |||
| ≤5 members per households | 494 (50.90) | 1897 (51.90) | 2391 (51.69) |
| >5 members per households | 476 (49.10) | 1758 (48.10) | 2235 (48.31) |
| Mass media exposure (TV/Radio) | |||
| No exposure | 380 (39.18) | 1388 (37.96) | 1768 (38.22) |
| Exposure | 590 (60.82) | 2268 (62.04) | 2858 (61.78) |
| Number of children | |||
| One | 876 (90.28) | 970 (26.54) | 1846 (39.91) |
| Two to three | 94 (09.66) | 2046 (55.98) | 2140 (46.26) |
| Four and more | 01 (00.06) | 639 (17.48) | 639 (13.82) |
| Working status | |||
| Not working | 825 (85.05) | 2706 (74.01) | 3531 (76.33) |
| Working | 145 (14.95) | 950 (25.99) | 1095 (23.67) |
| Division | |||
| Sylhet | 73 (07.51) | 355 (09.72) | 428 (09.25) |
| Barisal | 58 (05.99) | 210 (05.74) | 268 (05.79) |
| Chittagong | 198 (20.42) | 813 (22.23) | 1011 (21.85) |
| Rajshahi | 105 (10.78) | 360 (09.84) | 464 (10.04) |
| Dhaka | 332 (34.21) | 1302 (35.63) | 1635 (35.33) |
| Khulna | 83 (08.57) | 288 (07.89) | 371 (08.03) |
| Rangpur | 121 (12.54) | 328 (08.96) | 449 (09.71) |
| Wealth index | |||
| Poorest | 223 (22.97) | 779 (21.31) | 1002 (21.65) |
| Poorer | 192 (22.97) | 684 (21.31) | 876 (18.93) |
| Middle | 225 (22.97) | 656 (17.96) | 882 (19.06) |
| Richer | 200 (20.64) | 755 (20.64) | 955 (20.64) |
| Richest | 130 (13.36) | 782 (21.40) | 912 (19.71) |
| Total, N | 970 | 3656 | 4626 |
Table 2.
Bivariate Distribution of Antenatal Care (ANC)-Seeking Behavior of Pregnant Women.
| Variable | Frequency of ANC, n (%) | χ2 | P Value | ||
|---|---|---|---|---|---|
| No ANC, n = 992 | Less Than 4 times, n = 2187 | Four times or more, n = 1447 | |||
| Maternal age, years | |||||
| 15-19 years | 187 (19.23) | 488 (50.32) | 295 (30.45) | 5.710 | .058 |
| 20 years or more | 805 (22.02) | 1699 (46.47) | 1152 (31.51) | ||
| Women’s education | |||||
| No education | 281 (42.96) | 281 (42.94) | 92 (14.10) | 631.671 | <.001 |
| Primary | 394 (30.50) | 632 (48.85) | 267 (20.66) | ||
| Secondary | 295 (13.34) | 1102 (49.96) | 810 (36.70) | ||
| Higher | 22 (04.62) | 172 (36.41) | 278 (58.96) | ||
| Husband education | |||||
| No education | 406 (36.78) | 510 (46.18) | 188 (17.04) | 537.403 | <.001 |
| Primary | 359 (25.92) | 672 (48.52) | 354 (25.56) | ||
| Secondary | 194 (13.20) | 747 (50.81) | 529 (36.00) | ||
| Higher | 33 (04.88) | 258 (38.74) | 376 (56.38) | ||
| Place of residence | |||||
| Urban | 127 (10.46) | 530 (43.80) | 553 (45.74) | 228.664 | <.001 |
| Rural | 865 (25.32) | 1657 (48.51) | 894 (26.17) | ||
| Household size | |||||
| ≤5 members per households | 482 (20.16) | 1128 (47.16) | 781 (32.68) | 6.939 | .031 |
| >5 members per households | 510 (22.80) | 1059 (47.40) | 666 (29.80) | ||
| Mass media exposure (TV/Radio) | |||||
| No exposure | 642 (36.28) | 826 (46.72) | 300 (16.99) | 495.079 | <.001 |
| Exposure | 350 (12.25) | 1361 (47.62) | 1147 (40.13) | ||
| Number of children | |||||
| One | 284 (15.35) | 883 (47.81) | 680 (36.84) | 187.425 | <.001 |
| Two to three | 455 (21.27) | 1018 (47.56) | 667 (31.17) | ||
| Four or more | 253 (39.56) | 286 (44.79) | 100 (15.65) | ||
| Working status | |||||
| Not working | 727 (20.58) | 1662 (47.06) | 1143 (32.36) | 6.581 | .037 |
| Working | 265 (24.2) | 525 (47.97) | 304 (27.82) | ||
| Division | |||||
| Sylhet | 161 (37.53) | 183 (42.65) | 85 (19.82) | 192.942 | <.001 |
| Barisal | 72 (26.85) | 130 (48.51) | 66 (24.64) | ||
| Chittagong | 257 (25.43) | 494 (48.93) | 259 (25.64) | ||
| Rajshahi | 113 (24.20) | 228 (49.08) | 124 (26.71) | ||
| Dhaka | 263 (16.11) | 789 (48.28) | 582 (35.61) | ||
| Khulna | 42 (11.30) | 184 (49.56) | 145 (39.14) | ||
| Rangpur | 84 (18.78) | 179 (39.82) | 186 (41.40) | ||
| Wealth index | |||||
| Poorest | 426 (42.53) | 420 (41.94) | 156 (15.53) | 734.862 | <.001 |
| Poorer | 261 (29.85) | 438 (50.04) | 176 (20.11) | ||
| Middle | 164 (18.59) | 478 (54.16) | 240 (27.25) | ||
| Richer | 99 (10.34) | 485 (50.82) | 371 (38.83) | ||
| Richest | 42 (04.54) | 366 (40.12) | 504 (55.34) | ||
Figure 1.
Proportion of recommended antenatal care (ANC) among adolescent and adult mother across wealth quintile.
Association of Factors Using Bivariate Analysis
Table 2 shows the percentage of women who utilized the ANC services by selected background characteristics. No significant difference was found between these 2 age-groups considering ANC service utilization, while most of the women in both the groups utilized less then optimum ANC services. However, the utilization of ANC services significantly varied with women’s educational attainment (P < .001). Among the enabling factors, husband’s education seemed to be an important determinant of utilizing ANC services in receiving optimum number of ANCs (P < .001). Similarly, significant relationship was also observed among working status of women, exposure of mass media, number of children, wealth status, and across administrative division of the country concerning the extent of ANC utilization (P < .001).
Association of Factors Using Multivariate Analysis
Findings from multivariate analysis of at least 4 ANC utilizations are presented in Table 3. The results showed that a number of factors such as womens’ education, husbands’ education (adult only), place of resident (only adolescent), mass media exposure, working status of pregnant women (adolescent), number of children (adult), administrative divisions and wealth quintiles were found to be significant determinants of the utilization of ANC services. Our results demonstrated that womens’ educational attainment is a significant positive determining factor for utilizing recommended ANC services. The higher and secondary educated adolescent women were 8.08 times (95% CI: 1.99-32.85; P < .001) and 3.56 times (95% CI: 1.81-7.03; P < .001) more likely to utilize recommended ANC services than the adolescent women who had no formal education. For adult women, those who had higher and secondary education were 2.98 times (95% CI: 1.58-5.62; P < .001) and 1.86 times (95% CI: 1.41-2.46; P < .001) more likely to receive 4 or more ANCs compare to women who had no academic education. Husbands’ education level was also found to be a significant factor for influencing 4 ANC services for their spouse. Adult women who had educated husband up to higher and secondary level were 2.33 times (95% CI:1.41-3.86; P < .001) and 1.47 times (95% CI: 1.12 -1.92; P < .01) more likely to utilize recommended ANC care compared to those whose husband had no formal education. The urban adolescent women were 1.82 times (95% CI: 1.12-2.93; P < .05) more likely to take at least 4 ANCs than the rural adolescents. Such association was not observed among adult women. The mass media was found to be an important determinant for receiving recommended ANC in pregnant women. Adolescent and adult women were 1.62 times (95% CI: 1.09-2.42; P < .05) and 1.56 times (95% CI: 1.26 -1.94; P < .001) more likely to receive recommended ANC compared to those who were not exposed to any mass media. Our results observed a negative association between occupational status and optimum care for adolescent (adjusted odds ratio [AOR]: 0.58; 95% CI: 0.36-0.93; P < .05). Adult women who had experienced first delivery were 1.53 times (95% CI: 1.14-2.06; P < .01) more likely to receive 4 or more ANC services than those who had a history of giving birth for 4 times or more. The administrative division was also found to be an influencing factor in utilizing recommended ANC services. Adolescents living in Rangpur division had the highest likelihood (AOR: 3.52; 95% CI: 1.80-6.89; P < .001) to receive at least 4 ANC services compared to Sylhet division and for the adult women, the highest likelihood (AOR: 3.22; 95% CI: 2.18-4.74; P < .001) was observed in Khulna division. The disparity across economic status on utilization of recommended ANC services was found prominent among both the groups. The adolescent and adult women who belonged to richest quintile utilized recommended care 2.70 times (95% CI: 1.05-6.99; P < .05) and 6.51 times (95% CI: 3.98-10.64; P < .001) more likely compared to poorest quintile.
Table 3.
Multiple Logistic Regression Model Based on the Frequency of Recommended ANC Visit Among Adolescents and Adult Women.
| Variable | Model I | Model II |
|---|---|---|
| 15-19 years old, AOR, (95% CI) | 20 years or more, AOR, (95% CI) | |
| Women’s education | ||
| No education (ref) | 1.00 | 1.00 |
| Primary | 1.89 (0.97-3.67) | 1.29a (1.02 -1.65) |
| Secondary | 3.56b (1.81-7.03) | 1.86b (1.41-2.46) |
| Higher | 8.08b (1.99-32.85) | 2.98b (1.58-5.62) |
| Husband education | ||
| No education (ref) | 1.00 | 1.00 |
| Primary | 0.91 (0.57 -1.45) | 1.06 (0.85 -1.32) |
| Secondary | 1.70 (0.96-3.02) | 1.47c (1.12 -1.92) |
| Higher | 1.27 (0.51-3.18) | 2.33b (1.41-3.86) |
| Place of residence | ||
| Urban | 1.82a (1.12-2.93) | 1.10 (0.87 -1.40) |
| Rural (ref) | 1.00 | 1.00 |
| Household size | ||
| ≤5 members per households | 0.86 (0.60 -1.24) | 1.18 (0.97 -1.43) |
| >5 members per households | 1.00 | 1.00 |
| Mass media exposure (TV/Radio) | ||
| No exposure (ref) | 1.00 | 1.00 |
| Exposure | 1.62a (1.09-2.42) | 1.56b (1.26 -1.94) |
| Working status | ||
| Not working (ref) | 1.00 | 1.00 |
| Working | 0.58a (0.36-0.93) | 0.98 (0.8 -1.21) |
| Number of children | ||
| One | 1.11 (0.64 -1.91) | 1.53c (1.14-2.06) |
| Two to three | - | 1.13 (0.89 -1.44) |
| Four or more (ref) | 1.00 | 1.00 |
| Division | ||
| Sylhet (ref) | 1.00 | 1.00 |
| Barisal | 1.57 (0.85-2.93) | 1.44a (1.05 -1.98) |
| Chittagong | 1.55 (0.85-2.82) | 1.06 (0.80 -1.40) |
| Rajshahi | 2.29c (1.18-4.43) | 1.43a (1.03 -1.99) |
| Dhaka | 1.75 (0.93-3.28) | 2.06b (1.51-2.82) |
| Khulna | 2.49c (1.21-5.11) | 3.22b (2.18-4.74) |
| Rangpur | 3.52b (1.80-6.89) | 2.12b (1.51-2.98) |
| Wealth index | ||
| Poorest (ref) | 1.00 | 1.00 |
| Poorer | 1.09 (0.68 -1.76) | 1.34a (1.06 -1.70) |
| Middle | 1.36 (0.8-2.31) | 1.74b (1.32-2.30) |
| Richer | 1.49 (0.78-2.83) | 2.96b (2.13-4.10) |
| Richest | 2.70a (1.05-6.99) | 6.51b (3.98-10.64) |
| Mean VIF value | 2.72 |
Abbreviations: ANC, antenatal care; AOR, adjusted odds ratio; CI, confidence interval; ref, Reference; SD, standard deviation; VIF, variance inflation factor.
a P < .05.
b P < .001.
c P < .01.
Discussion
The maternal mortality rate has decreased over the past few years in Bangladesh, and the rate of utilizing recommended ANC services is increasing (26% in 2011 and 31.2% in 2014); however, the utilization was not equally distributed across the societies.22 Further, a number of pregnant women still do not utilize the recommended ANC visits, and even utilization pattern often varied along with age of the women. This study identified the factors that were significantly associated with the utilization of recommended ANC services among adolescents and adult women in Bangladesh.
Our study found that both age-groups received almost same proportion (31%) of recommended ANC services. Among the 69 countries tracked by countdown to 2015 observed the median coverage rate of recommended ANC is approximately 55% which was comparatively higher than Bangladesh24,25; thus, more innovative approach should be introduced to increase the recommended ANC coverage in Bangladesh. Our study demonstrated that education is a significant positive factor for utilizing optimum ANC coverage in both the groups. Several studies reported similar findings where education was a proven factor for recommended ANC services.26-28 This might be due to the fact that educated women have more knowledge about self-care with self-dependency,29 usually hold more household decision-making power, and also have greater awareness of the benefits of recommended ANC services and the adverse effects of pregnancy-related complications.30 This study showed that women living in urban areas received more recommended ANC services than rural. Among the adolescent women, urban residents utilized more recommended ANC than the rural women. The transportation barrier and other supply side constraints (eg, facility availability, health personnel, and diagnostic laboratory test results) might be the reasons behind these disparities.31,32 A study of similar setting found that urban women received recommended ANC services which was 1.46 times higher than the rural women.33 However, we did not find any significant association between household size and recommended ANC services. Inconsistent with our study, another study observed that a household having less than 3 children were 8 times more likely to utilize ANC than the larger households.34
Mass media plays an effective role for utilization of optimal MHS.35 Our study found a positive significant association between mass media exposure and receiving recommended ANC services for both adolescents and adult women. Similar findings were also observed in southwestern Uganda.36 Working status of women had negative impact on recommended care, as those who were employed utilized lower number of ANCs than for nonworking women. It might be due to busy working hours or limited opportunity for investing time to receive ANC care than nonworking women. No such association was found among adult women. Among adult women, those who gave birth for the first time were found to have a higher tendency of utilizing recommended ANC services. It might be due to more importance about first pregnancy or limited knowledge about common general symptoms of pregnancy, which led to utilize more ANC services.37 Our study also found variations in utilizing recommended ANC services among the administrative regions of Bangladesh. Women from Rangpur and Khulna region were more likely to have 4 or more ANC visits than women from Sylhet region. Both demand and supply side barrier such as limited knowledge, transports, and affordability issues might be responsible, as it is difficult to get accessibility to ANC services in more remote and hard-to-reach areas in Sylhet region.38 We also observed that the adolescents from Rangpur region received significantly higher number of recommended ANC services, which may be because of implementing a large number of maternal health programs among economically impoverished regions of Bangladesh.39 Nevertheless, utilization of recommended ANC services in Khulna region was higher among adult women than the Sylhet division. The reason for divisional differences is often unclear and needs further investigation.40 Our findings indicated that household wealth index is a crucial determinant of receiving ANC services. Both adolescent and adult women utilized significantly higher recommended ANC services than women from poorest households. A study conducted among 32 low-income countries including Bangladesh found that the women belongs to richest household utilized 4.25 times higher attendance for ANC than the poorest women which is in line with this study.41 An earlier study observed that women belonged to a wealthiest household had 10.86 times more likelihood to receive optimal ANC services than the poorest household women.40 Higher utilization of ANC among women in the wealthiest households suggests that affordability could be an important issue in ANC service utilization. Further, the richest families are educated, have greater independence, and greater access to health care. Although Bangladesh government provides almost free MHSs, several studies reported that hidden costs to families (such as user fee) may induce poorer families to seek care from unqualified providers.40,42
There are several limitations of this study. The study design, a cross-sectional nature as well as women’s own perception and local context could not be answered through this quantitative data. The study is limited by the fact that is based on recall of measures used in the survey. However, study findings can be generalized at the national level as the study gathered data from a nationally representative household demographic and health survey that provided a more accurate picture of recommended ANC care utilization across adolescent and adult women.
Conclusion
The study observed several independent variables such as educational and wealth status, residential status, mass media exposure, number of children, and even the administrative divisions are associated with recommended ANC care. These findings might help health-care programmers and policy makers to initiate appropriate policy and programs for ensuring optimal ANC coverage for all. Ensuring adequate ANC regardless of economic status and residence of pregnant women could guarantee universal maternal health-care coverage as devoted to a national strategic guideline.
Author Biographies
Nausad Ali, Health Economics and Public health researcher, icddr,b Bangladesh.
Marufa Sultana, Health economist and assistant scientist, icddr,b and PhD Fellow at Deakin University, Australia.
Nurnabi Sheikh, Health Economics and Public health researcher, icddr,b Bangladesh.
Raisul Akram, Health Economics and Public health researcher, icddr,b Bangladesh.
Rashidul Alam Mahumud, Health Economics and Public health researcher and PhD Fellow University of Southern Queensland, Toowoomba, Australia.
Muhammad Asaduzzaman, Public health researcher, Laboratory Sciences and Services Division, icddr,b Dhaka, Bangladesh.
Abdur Razzaque Sarker, Health economist and assistant scientist, icddr,b and PhD Fellow at University of Strathclyde, United Kingdom.
Footnotes
Authors’ Note: Muhammad Asaduzzaman is now affiliated to Laboratory Sciences and Services Division, icddr,b Dhaka Bangladesh. Abdur Razzaque Sarker is now affiliated to Health Economics and Financing Research, icddr,b Dhaka Bangladesh.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Abdur Razzaque Sarker  http://orcid.org/0000-0002-2022-7590
http://orcid.org/0000-0002-2022-7590
References
- 1. Amponsah EN, Senadza B, Arthur E. Determinants of utilization of antenatal care services in developing countries Recent evidence from Ghana. Afric J Econom Manage Stud. 2013;4(1):58–73. doi:10.1108/20400701311303159. [Google Scholar]
- 2. Farah S, Karim M. Determinants of utilization of antenatal care services in rural area of Bangladesh. Bangl Med J. 2015;44(2):67–71. [Google Scholar]
- 3. Say L, Chou D, Gemmill A, et al. Global causes of maternal death: a WHO systematic analysis. 2006;2:323–333. doi:10.1016/S2214-109X(14)70227-X. [DOI] [PubMed] [Google Scholar]
- 4. Sultana M, Mahumud RA, Ali N, et al. The effectiveness of introducing Group Prenatal Care (GPC) in selected health facilities in a district of Bangladesh: study protocol. BMC Preg Childb. 2017;17(1):48 doi:10.1186/s12884-017-1227-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Alkema L, Chou D, Hogan D, et al. ; United Nations Maternal Mortality Estimation Inter-Agency Group Collobrators and technical advisory Group. Global, regional, and national levels and trends in maternal mortality between 1990 and 2015, with scenario-based projections to 2030: a systematic analysis by the UN Maternal Mortality Estimation Inter-Agency Group. Lancet. 2016;387(10017):462–474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. MOHFW. Health Bulletin 2016. Dhaka, Bangladesh; 2016. http://www.dghs.gov.bd (accessed on January 10, 2018). [Google Scholar]
- 7. Mahara G, Asweto C, Cao K, Alzain AM, Sebastian A. Utilization of ANC and PNC services in nepal: a multivariate analysis based on nepal demographic health survey 2001 and 2006. Am J Health Res. 2015;3(6):318–327. doi:10.11648/j.ajhr.20150306.11. [Google Scholar]
- 8. World Health Organization (WHO). Integrated Management of Pregnancy and Child Birth: Standard of Maternal and Neonatal Care. Geneva, Switzerland: Department of Making Pregnancy Safer; 2007. [Google Scholar]
- 9. Majrooh MA, Hasnain S, Akram J, Siddiqui A, Memon ZA. Coverage and quality of antenatal care provided at primary health care facilities in the “Punjab” province of “Pakistan.” PLoS One. 2014;9(11):e0113390 doi:10.1371/journal.pone. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ministry of Health and Family Welfare(MOHFW). National Strategy for Maternal Health. Dhaka, Bagladesh: MOHFW; 2001. [Google Scholar]
- 11. Pulok MH, Sabah N, Uddin J, Enemark U. Progress in the utilization of antenatal and delivery care services in Bangladesh: where does the equity gap lie? BMC Pregnancy Childbirth. 2016;16(1):200 doi:10.1186/s12884-016-0970-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. NIPORT. Bangladesh Demographic and Health Survey 2014. Dhaka, Bangladesh, and Rockville, Maryland, USA: NIPORT, Mitra and Associates, and ICF International; 2016. [Google Scholar]
- 13. Chakraborty N, Islam MA, Chowdhury RI, Bari W. Utilisation of postnatal care in Bangladesh: evidence from a longitudinal study. Health Soc Care Community. 2002;10(6):492–502. [DOI] [PubMed] [Google Scholar]
- 14. Kabir M, Iliyasu Z, Abubakar I, Sani AA. Determinants of utilization of antenatal care services in Kumbotso village, Northern Nigeria. Trop Doct. 2005;35(2):110–111. [DOI] [PubMed] [Google Scholar]
- 15. Kulmala T, Vaahtera M, Rannikko J, et al. The relationship between antenatal risk characteristics, place of delivery and adverse delivery outcome in rural Malawi. Acta Obstet Gynecol Scand. 2000;79(11):984–990. [PubMed] [Google Scholar]
- 16. Tuladhar H, Dhakal N. Impact of antenatal care on maternal and perinatal utcome: a study at nepal medical college teaching hospital. Nepal J Obstetr Gynaecol. 2012;6(2):37–43. doi:10.3126/njog.v6i2.6755. [Google Scholar]
- 17. Yakoob M, Menezes EV, Soomro T, Haws RA, Darmstadt GL, Bhutta ZA. Reducing stillbirths: behavioural and nutritional interventions before and during pregnancy. BMC Pregnancy Childbirth. 2009;9(Suppl 1):S3 doi:10.1186/1471-2393-9-S1-S3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Ha BT, Tac PV, Duc DM, Duong DT, Thi LM. Factors associated with four or more antenatal care services among pregnant women: a cross-sectional survey in eight South Central Coast provinces of Vietnam. Int J Womens Health. 2015;7:699–706. doi:10.2147/IJWH.S87276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Ye Y, Yoshida Y, Harun-Or-Rashid M, Sakamoto J. Factors affecting the utilization of antenatal care services among women in Kham District, Xiengkhouang province, Lao PDR. Nagoya J Med Sci. 2010;72(1-2):23–33. [PMC free article] [PubMed] [Google Scholar]
- 20. Yakong VN, Rush KL, Bassett-Smith J, Bottorff JL, Robinson C. Women’s experiences of seeking reproductive health care in rural Ghana: challenges for maternal health service utilization. J Adv Nurs. 2010;66(11):2431–2441. doi:10.1111/j.1365-2648.2010.05404.x. [DOI] [PubMed] [Google Scholar]
- 21. Kingston D, Heaman M, Fell D, Chalmers B; Maternity Experiences Study Group of the Canadian Perinatal Survelliance System, Public Health Agency of Canada. Comparison of adolescent, young adult, and adult women’s maternity experiences and practices. Pediatrics. 2012;129(5): e1228–e1237. doi:10.1542/peds.2011-1447. [DOI] [PubMed] [Google Scholar]
- 22. National Institute of Population Research and Training (NIPORT), Mitra and Associates and II 2016. Bangladesh Demographic and Health Survey 2014. Dhaka, Bangladesh, and Rockville, Maryland, USA: NIPORT, Mitra and Associates, and ICF International; 2014. [Google Scholar]
- 23. World Health Organization (WHO). Women and Health: Today’s Evidence Tomorrow’s Agenda. World Health Organization (WHO); 2009, http://www.who.int/gender-equity-rights/knowledge/9789241563857/en/ (accessed on January 10, 2017). [Google Scholar]
- 24. Requejo JH, Bryce J, Barros AJ, et al. Countdown to 2015 and beyond: fulfi lling the health agenda for women and children. Lancet. 2015;385(9966):466–476. doi:10.1016/S0140-6736(14)60925-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Gupta S, Yamada G, Mpembeni R, et al. Factors associated with four or more antenatal care visits and its decline among pregnant women in Tanzania between 1999 and 2010. PLoS One. 2014;9(7):1–13. doi:10.1371/journal.pone.0101893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Jahan M, Jahan E. Socio-demographic determinants influencing antenatal care seeking behaviour among women in Bangladesh: an application of factor analysis. Community Med and Public Health. 2016;3(4):925–930. doi: doi.org/10.18203/2394-6040. [Google Scholar]
- 27. Anwar I, Nababan HY, Mostari S, Rahman A, Khan JA. Trends and inequities in use of maternal health care services in Bangladesh, 1991-2011. PloS one. 2015;10(3):e0120309 doi:10.1371/journal.pone.0120309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Joshi C, Torvaldsen S, Hodgson R, Hayen A. Factors associated with the use and quality of antenatal care in Nepal: a population-based study using the demographic and health survey data. BMC Pregnancy Childbirth. 2014;14:94 doi:10.1186/1471-2393-14-94 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Jejeebhoy S. Women’s education, autonomy, and reproductive behaviour: experience from developing countries OUPCatalogue. Oxford, UK: Clarendon Press; 1996:28. [Google Scholar]
- 30. Acharya DR, Bell JS, Simkhada P, van Teijlingen ER, Regmi PR. Women’s autonomy in household decision-making: a demographic study in Nepal. Reprod Health. 2010;7(1):15 doi:10.1186/1742-4755-7-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Khatri RB, Dangi TP, Gautam R, Shrestha KN, Homer CSE. Barriers to utilization of childbirth services of a rural birthing center in Nepal: a qualitative study. PLoS One. 2017;12(5):1–20. doi:10.1371/journal.pone.0177602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Matthews Z, Channon A, Neal S, Osrin D, Madise N, Stones W. Examining the “Urban advantage” in maternal health care in developing countries. PLoS Med. 2010;7(9):1–7. doi:10.1371/journal.pmed.1000327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Rahman A, Nisha MK, Begum T, Ahmed S, Alam N, Anwar I. Trends, determinants and inequities of 4 + ANC utilisation in Bangladesh. J Health Popul Nutr. 2017;36(2):1–8. doi:10.1186/s41043-016-0078-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Abosse Z, Woldie M, Ololo S. Factors influencing antenatal care service utilization in hadiya zone. Ethiop J Health Sci. 2010;20(2):75–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Grilli R, Ramsay C, Minozzi S. Mass media interventions: effects on health services. Utilisation. 2002;(1). doi:10.1002/14651858.CD000389. [DOI] [PubMed] [Google Scholar]
- 36. Asp G, Pettersson KO, Sandberg J, Kabakyenga J, Agardh A. Associations between mass media exposure and birth preparedness among women in southwestern Uganda: a community-based survey. Global Health Action. 2014;7(1):1–7. doi:10.3402/gha.v7.22904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Adhikari T, Sahu D, Nair S, Saha KB, Sharma RK, Pandey A. Factors associated with utilization of antenatal care services among tribal women: a study of selected states. Indian J Med Res. 2016;144(1):58–66. doi:10.4103/0971-5916.193284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Government of the People’s Republic of Bangladesh (GoB). National Strategy for Water and Sanitation Hard to Reach Areas of Bangladesh. Dhaka, Bangladesh: Government of the People’s Republic of Bangladesh (GoB; ); 2011. [Google Scholar]
- 39. Bangladesh Bureau of Statistics (BBS). Report of the household income & expenditure survey 2010. Dhaka, Bangladesh: New Panama Printing Press, BBS, Statistics division, Ministry of Planning, The Government of the People’s Republic of Bangladesh. Bangladesh: Bangladesh Bureau of Statistics (BBS; ); 2011: 1–583. [Google Scholar]
- 40. Rahman MM, Rahman MM, Tareque MI, Ferdos J, Jesmin SS. Maternal pregnancy intention and professional antenatal care utilization in Bangladesh: a nationwide population-based survey. PLoS One. 2016;11(6):1–15. doi:10.1371/journal.pone.0157760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Guliani H, Sepehri A, Serieux J. Determinants of prenatal care use: evidence from 32 low-income countries across Asia, Sub-Saharan Africa and Latin America. Health Policy Plan. 2014;29(5):589–602. doi:10.1093/heapol/czt045. [DOI] [PubMed] [Google Scholar]
- 42. Chandrasiri J, Anuranga C, Wickramasinghe R. and RPR-E. The Impact of Out-of-Pocket Expenditures on Poverty and Inequalities in Use of Maternal and Child Health Services in Bangladesh: Evidence from the Household Income and Expenditure Surveys 2000– 2010 RETA–6515 Country Brief. Manila: Asian Development Bank; 2012:1–8. [Google Scholar]