Abstract
May-Thurner syndrome (MTS) or iliac vein compression syndrome is an uncommon cause of deep venous thrombosis (DVT) of the lower limb occurring, especially on the left side. It occurs due to compression of the left common iliac vein by the right common iliac artery and occurs predominantly in young females. The awareness of such a presentation is essential to guide therapy. We report one such unusual case of acute-onset DVT of the left lower limb due to MTS.
Keywords: Deep vein thrombosis, iliac vein compression, May-Thurner syndrome
INTRODUCTION
The clinical prevalence of May-Thurner syndrome (MTS) related DVT is very low. This could be because usually the diagnostic work up is halted once DVT is confirmed. Failure to correct the anatomic substrate of MTS could lead to DVT recurrence and additional complications including pulmonary embolism. We report one such unusual case of acute-onset DVT due to MTS.
CASE REPORT
A 57-year-old female with medical history of diabetes and hypertension was transferred to our facility with complaints of high-grade fever for the past 3 days. There was no other significant associated history to explain the probable cause of fever except that she had a history of fall about 2 weeks ago. She had taken initial treatment at a primary health center and was ambulating well at home. On arrival at the emergency room, she was conscious and oriented, febrile, hypotensive, and with minimal respiratory distress. An initial diagnosis of sepsis due to the unknown source was considered and managed per protocol with fluid resuscitation, cultures, and imaging to identify the potential source and broad-spectrum antibiotics. Complete hemogram revealed leukocytosis with toxic neutrophil granulation. Renal, liver, and coagulation panels were within normal limits. Electrocardiogram revealed right axis deviation, S1Q3T3 pattern, and echocardiography did not suggest right heart strain. Lower limb venous Doppler and compression ultrasound did not show any evidence of lower limb deep venous thrombosis (DVT). Computer tomography (CT) pulmonary angiogram was performed which ruled out pulmonary embolism (PE), and she was initiated on unfractionated heparin for DVT prophylaxis.
Blood cultures grew methicillin-sensitive Staphylococcus aureus (MSSA), and the antibiotic was appropriately de-escalated, and the patient was gradually improving. Rest of the cultures did not reveal any bacterial growth and screening for tropical infections was also negative. CT abdomen revealed a fracture of body of D8 vertebra. In view of MSSA bacteremia, transesophageal echocardiography was performed which did not show any features of infective endocarditis.
Subsequently, during the course in hospital, she developed acute left lower limb swelling with pain and redness. Repeat venous Doppler of the left lower limb revealed acute DVT extending from the left internal iliac vein to popliteal vein. Repeat coagulation profile was normal, hemogram showed normal platelet count, and peripheral smear did not reveal any abnormality. Connective tissue and vasculitis workup were negative. Therapeutic anticoagulation with intravenous heparin infusion was initiated.
Magnetic resonance imaging of the spine showed moderate wedging of T8 and T11 vertebral body with no evidence of cord edema or mass. There was compression of the left common iliac vein by the right common iliac artery with acute thrombus in the left common iliac vein, and these features were consistent with May-Thurner syndrome (MTS) [Figure 1a]. A Catheter-based thrombolysis followed by venous stenting was suggested by the vascular surgeon. However, patient's relatives did not consent for the procedure. It was decided in consensus with the cardiologist and vascular surgeon to place a filter in the inferior vena cava (IVC) to prevent PE. Long-term anticoagulation with factor Xa inhibitor (Rivaroxaban) was initiated and continued. She was afebrile and stable at discharge and remained asymptomatic during subsequent follow-up after a month.
Figure 1.
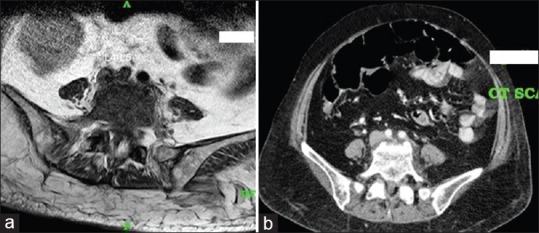
(a) Magnetic resonance imaging and (b) computed tomography images showing compression of the left common iliac vein by the right common iliac artery at its origin against the lumbar spine
DISCUSSION
MTS, which is also alternatively called as iliac vein compression syndrome or Cockett syndrome is one of the rare causes of deep vein thrombosis occurring exclusively in the left lower limb.[1] It was first described in 1957 and has been seen in individuals predisposed with May-Thurner anatomy (MTA) [Figure 1b]. This is an unusual anatomical variation leading to the compression of the left common iliac vein by the right common iliac artery against lumbar spine.[2] It has been noted that the prevalence of MTA is higher as compared to MTS itself.[3] The exact threshold at which compression triggers symptomatic DVT is still unknown.[4] However, one study had reported that the DVT was more likely when the vein compression was >70%.[5] Risk factors precipitating MTS includes trauma, prolonged immobilization, dehydration, multiple pregnancies, postpartum, oral contraceptive therapy, and febrile illness.[6]
MTS usually presents in the second or third decade of life and is more commonly seen in women; however, there are a few reports of such occurrence in the elderly age group.[7] Our patient was a middle-aged female who presented with acute febrile illness and was being evaluated for possible sepsis. In view of strong clinical suspicion of PE, she was promptly investigated. Lower limb Doppler examination along with CT pulmonary angiogram was negative. Later during hospitalization, our patient developed acute DVT of the left lower limb while on unfractionated heparin for DVT prophylaxis.
She was extensively evaluated for the probable cause of acute DVT developing in the critical care unit with all workup being inconclusive. Furthermore, she had MSSA bacteremia, and as part of source identification, imaging studies were done, which incidentally revealed that the left common internal iliac vein was thrombosed and compressed by the right common iliac artery against the lumbar vertebrae. Therapeutic anticoagulation was then initiated immediately to prevent new or propagation of thrombus. However, the definitive management of MTS is aimed at (a) resolution of thrombus if acute or subacute, (b) recanalization of occluded venous segments, and (c) maintenance of the patency of the iliac vein by balloon dilatation and stent placement. Endovascular management remains the first-line treatment for MTS.[8] The only indication of open surgery is a failure of endovascular therapy. Our patient was offered catheter-based thrombolysis followed by stenting, but the relatives did not consent for the same and therapeutic anticoagulation was continued.
Finally, the incidence of PE in patients with MTS is low, and there are only a few case reports of MTS which presented with acute PE.[9] Although the routine use of IVC filter is not recommended by the guidelines, we offered IVC filter for our patient due to the presence of high clot burden and to prevent the development of acute PE.
CONCLUSION
MTS is a unique cause of acute DVT occurring, especially in the left lower limb. Awareness of such a condition not only helps in better diagnosis but also plan appropriate endovascular management which improves the patient outcome.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Cockett FB, Thomas ML. The iliac compression syndrome. Br J Surg. 1965;52:816–21. doi: 10.1002/bjs.1800521028. [DOI] [PubMed] [Google Scholar]
- 2.May R, Thurner J. The cause of the predominantly sinistral occurrence of thrombosis of the pelvic veins. Angiology. 1957;8:419–27. doi: 10.1177/000331975700800505. [DOI] [PubMed] [Google Scholar]
- 3.Chamarthy RM, Patrick S, Mathew A, Mark A, Sanjeeva PK. Evolving concepts in the diagnosis and management of May–Thurner syndrome. J Clin Interv Radiol. 2016;1:23–30. [Google Scholar]
- 4.Birn J, Vedantham S. May-Thurner syndrome and other obstructive iliac vein lesions: Meaning, myth, and mystery. Vasc Med. 2015;20:74–83. doi: 10.1177/1358863X14560429. [DOI] [PubMed] [Google Scholar]
- 5.Narayan A, Eng J, Carmi L, McGrane S, Ahmed M, Sharrett AR, et al. Iliac vein compression as risk factor for left- versus right-sided deep venous thrombosis: Case-control study. Radiology. 2012;265:949–57. doi: 10.1148/radiol.12111580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Patel NH, Stookey KR, Ketcham DB, Cragg AH. Endovascular management of acute extensive iliofemoral deep venous thrombosis caused by May-Thurner syndrome. J Vasc Interv Radiol. 2000;11:1297–302. doi: 10.1016/s1051-0443(07)61304-9. [DOI] [PubMed] [Google Scholar]
- 7.Sahnan K, Chris PY, Robert HT, Kaji S. A rare case of May-Thurner like syndrome in an elderly female. Case rep Intern Med. 2014;1:19. [Google Scholar]
- 8.Meissner MH, Gloviczki P, Comerota AJ, Dalsing MC, Eklof BG, Gillespie DL, et al. Early thrombus removal strategies for acute deep venous thrombosis: Clinical practice guidelines of the society for vascular surgery and the American venous forum. J Vasc Surg. 2012;55:1449–62. doi: 10.1016/j.jvs.2011.12.081. [DOI] [PubMed] [Google Scholar]
- 9.Fasanya AA, LaCapra G. May-Thurner syndrome with pulmonary embolism as the first presentation rather than deep vein thrombosis. Cureus. 2016;8:e509. doi: 10.7759/cureus.509. [DOI] [PMC free article] [PubMed] [Google Scholar]


