Abstract
Background:
Indo-Gangetic basin is known to have higher incidence of gallbladder cancer. Proximity to River Ganga and high heavy metal in soil exposure have been postulated as risk factors.
Aim:
This study aims to evaluate the geographical pattern of gallbladder cancer from consecutive patient database enrolled in hospital-based cancer registry (HBCR).
Objectives:
To evaluate demographic profile and districtwise/zonewise dispersion of gallbladder cancer cases registered in HBCR from year 2014 to 2016. To evaluate association of carcinoma gallbladder (CaGB) due to proximity of Ganges, districts of high soil arsenic levels and referral bias.
Materials and Methods:
Demographic profile and district-based location of individual consecutive gallbladder cancer patient registered in Regional Cancer Centre from the year 2014 till 2016 were analyzed. Population data from 2011 census and arsenic soil content data from central groundwater body were obtained. Frequency distribution, cross tabulation, and odds ratio were used to analyze risk of CaGB across population subsets in Bihar.
Results:
A total of 1291 consecutive patients of CaGB were registered from 2014 to 2016. Median age at diagnosis was 55 years (range 18–95 years). Male to female ratio was 0.6. Patna (16%) followed by Vaishali (5.8%), Sitamarhi (5%), Madhubani (4.7%), Gaya (4%), and Samastipur (4%) had highest cases. Districts along main central River Ganga (n = 12) and those exposed to high arsenic soil content (n = 15) had higher odds ratio for CaGB, 1.72 (95% confidence interval [CI]: 1.54–1.91, P = 0.001), and 1.45 (95% CI: 1.30–1.62, P = 0.001), respectively. Districts within 100 km radius of our institute had higher gallbladder cancer cases, odds ratio 1.81 (95% CI: 1.62–2.03, P = 0.001), suggesting significant referral bias predominantly contributed by cases registered under Patna and Vaishali districts.
Conclusion:
CaGB is major public health problem in Bihar. Exposure to high soil arsenic levels and proximity to River Ganga are strongly associated with gallbladder cancer. Systematic population-based longitudinal studies are needed to explore above hypothesis.
Keywords: Arsenic heavy metal exposure, gallbladder cancer, Ganga river
Introduction
The incidence of carcinoma gallbladder (CaGB) varies widely across the globe. SEER data estimate an incidence of 1.1 cases per million population across United States of America, while GLOBOCON puts a figure of 1.3% incidence of all cancers and 1.7% cancer mortality across the world.[1,2] In India, Northern and Eastern states stretched across the Indo- Gangetic belt has the highest incidence ranging from most common in Kamrup District, second most common in Dibrugarh, third most common in Delhi, and forth most common in Kolkata among women across these major population-based cancer registries (PBCR).[3,4] Lack of PBCR in two of the most populous states across the Gangetic belt, Uttar Pradesh, and Bihar, makes estimating the incidence of CaGB difficult. However, hospital-based cancer registries (HBCR) in Uttar Pradesh, estimates CaGB as 4.4% of all malignancies and approximate incidence of 4/100,000 population/year.[4,5] There is paucity of data from Bihar, regarding incidence and distribution of CaGB across several districts in this state.[6] We report three consecutive year individual patient data of CaGB cases registered in our tertiary Regional Cancer Centre (RCC) and HBCR in Bihar.
Materials and Methods
We retrieved consecutive individual patient data registered as CaGB from January 2014 to December 2016 (3 years) in our HBCR. Our institute is the only tertiary RCC in Bihar, under the joint control and funding of the Government of India and the Bihar state government equipped with departments of radiotherapy, surgical oncology, medical oncology, gynecologic oncology, and palliative care.
Demographic variables including age, sex, diagnosis, and patient addresses were retrieved and analyzed. Further, patients were grouped into districts they represent as per the information registered in HBCR database. Districtwise distribution of CaGB cases was analyzed with respect to the baseline overall population in each of the 38 districts of Bihar. Information regarding population in each of the districts was assessed through data reported by Census 2011.[7]
To identify and stratify CaGB cases into geographical divisions, all 38 districts were grouped into North, South, East, West, and Central Region.
North region – East Champaran, West Champaran, Araria, Kishanganj, Madhubani, Sheohar, Sitamarhi, Supaul, Darbhanga
West region – Arwal, Bhojpur, Buxar, Gopalgunj, Jehanabad, Kaimur, Muzaffarpur, Saran, Siwan
South Region – Aurangabad, Gaya, Jamui, Nawada, Rohtas
East Region – Banka, Bhagalpur, Khagaria, Katihar, Munger, Madhepura, Purnia, Saharsa
Central Region – Patna, Vaishali, Begusarai, Lakhisarai, Sheikhpura, Nalanda, Samastipur.
Entire study was divided into three broad objectives as below:
To evaluate CaGB cases around districts through which main River Ganga flows: main central River Ganga flows across West to East Bihar before navigating the state of West Bengal. CaGB cases in districts surrounding the main River Ganga, for example, Sivan, Buxar, Saran, Bhojpur, Khagaria, Patna, Vaishali, Begusarai, Munger, Lakhisarai, Bhagalpur, and Katihar (12) were matched with CaGB cases in other, nonGanga vicinity districts. This was further analyzed with respect to baseline exposed population in districts around main river Ganga versus other districts
To evaluate pattern of CaGB cases in districts exposed to higher arsenic soil content: As per data from Central Ground Water Board, Ministry of Water Resources, River Development and Ganga Rejuvenation, Government of India, around 15 districts have high soil arsenic level (above 0.05 mg/L): Begusarai, Bhagalpur, Bhojpur, Buxar, Darbhanga, Katihar, Khagaria, Kishanganj, Lakhisarai, Munger, Patna, Purnia, Samastipur, Saran, and Vaishali. CaGB cases in these 15 districts were plotted against other remaining 23 districts. Further, these CaGB cases in exposed (high arsenic districts) and nonexposed districts were compared with baseline overall population in these districts as per Census 2011 data[7]
To evaluate extent of hospital referral bias with respect to geographical proximity. Our center being in Central Bihar and in the capital city of Patna is likely to receive higher patients from proximate areas. To evaluate extent of hospital referral bias, we divided districts into two zones. Zone 1 (districts within 100 km radius of our Institute, approximate traveling time 3 h) including Patna, Vaishali, Nalanda, Jehanabad, Bhojpur, Saran, Samastipur, and Muzaffarpur and Zone 2 including rest of Bihar districts. We plotted CaGB cases in above two zones with respect to baseline overall population in above zones using Census 2011 data.[7]
Data were analyzed using frequency distribution charts, crosstabs, line diagram, and compound bar diagram using SPSS version 20 (SPSS 20, IBM, Armonk, NY, United States of America). Comparison of carcinoma GB for above all three objectives, i.e., A, B, and C was done using odds ratio with respect to exposed and nonexposed population. This study was reviewed and approved by our Institutional Review Board and Ethics Committee.
Results
A total of 1291 consecutive cases of CaGB were registered in HBCR through our several oncology Outpatient Departments in RCC between January 2014 and December 2016 (3 years). These cases also include cases diagnosed by other parallel departments such as general surgery, gastrointestinal surgery, gastroenterology, and general medicine. Total cases were 250, 455, and 586 reported in the year 2014, 2015, and 2016, respectively. Median age at diagnosis was 55 years with range from 18 to 95 years. Male to female ratio was 0.6 favoring females. Patna (n = 208), Vaishali (n = 75), Sitamarhi (n = 64), Madhubani (n = 61), Saran (n = 56), Samastipur (n = 54), Gaya (n = 54), East Champaran (n = 49), Muzaffarpur (n = 43), Begusarai (n = 42), and Bhojpur (n = 42) were among the top 10 districts in terms of CaGB cases reported in those 3 years [Figure 1].
Figure 1.
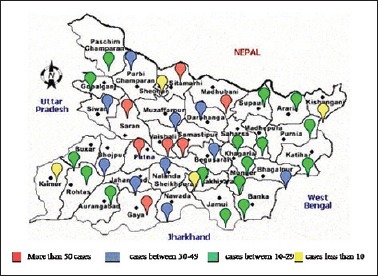
Case distribution pattern across several districts in Bihar
Among geographical regions, central region had the maximum concentration of CaGB cases (n = 432) followed by North (n = 278), West (n = 242), East (n = 191), and South (n = 148). About 28% higher cases were registered in 2016 compared to 2015. Western region showed sharpest rise in terms of CaGB cases reported in the year 2016 compared to the year 2014 and 2015, while cases in central region seem to plateau in the year 2016 with minimal rise compared to other regions reported [Table 1 and Figure 2a, b]. Central region dominated among all other regions registering 37% of all cases in the year 2014, 34% of all cases in the year 2015, and 31% of all cases in the year 2016. Southern region had least of all regions with 9.2% of all cases in the year 2014, 10.5% and 13% of all cases in the year 2015 and 2016, respectively.
Table 1.
Distribution of carcinoma gallbladder cases in different geographical regions with respect to time
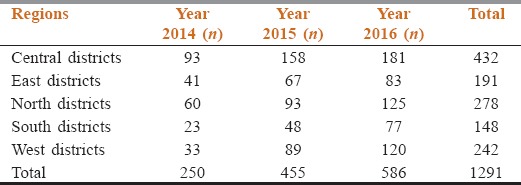
Figure 2.
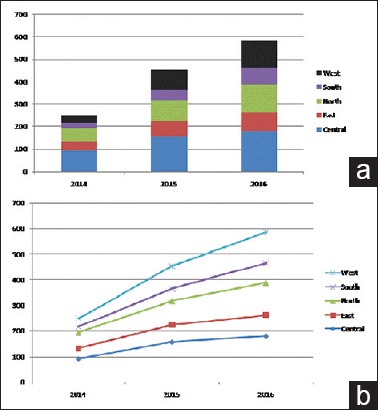
(a and b) Pattern of carcinoma gallbladder in different regions, trend with respect to time
Compared to districts away from central main River Ganga, districts along the River Ganga had significantly higher risk of reporting CaGB with odds ratio of 1.72 (95% confidence interval [CI] - 1.54–1.91), P < 0.0001. Similarly, we also found that districts with high soil level of arsenic (>0.05 mg/dL) had significantly high association with reporting CaGB cases, odds ratio 1.45 (95% CI = 1.30–1.62), P < 0.0001. Our center being the apex tertiary referral RCC situated in the State Capital Patna, we evaluated whether these above factors increase likelihood of higher cases reported from proximal districts due to hospital and proximity bias compared to distant remote districts. We found that districts within 100 km radius had significantly high odds ratio of reporting CaGB cases compared to other distant districts, odds ratio 1.81 (95% CI = 1.62–2.03), P < 0.0001, thus confirming strong bias of reporting CaGB cases favoring proximal districts.
Discussion
Bihar is a state in Eastern India with Patna city being its capital. Bihar is the third most populous state of India with population of 104,099,452, with 89% of people living in rural India.[8] River Ganga divides Bihar into two unequal halves and flows through middle from West to East. Under National Cancer Control Programme with Ministry of Health and Family Welfare (India), RCC was created to cater needs of populace in several distinct geographical regions/states.[9] In Bihar, Indira Gandhi Institute of Medical Sciences has its own and only RCC in Patna. It is tertiary apex RCC with functional radiotherapy, surgical oncology, medical oncology, and gynecologic oncology. Our RCC also has HBCR which gives a fare assessment of magnitude and pattern of cancer care in the state of Bihar.[10]
Indo-Gangetic belt has high incidence of CaGB compared to West, especially in females.[11] Apart from genetic and lifestyle factors, gallstones, obesity, diabetes, heavy metal in water for consumption, mustard oil, and chickpea consumption have been associated as risk factors in population having higher CaGB cases.[12,13,14,15,16,17] Majority of CaGB present in advanced stages, and definitive curable therapy is feasible in 10%–20% of localized disease only.[18] Palliative chemotherapy extends median survival up to 10–12 months with patients ultimately succumbing to disease progression.[19,20] Soil in districts along main river Ganga is known to have higher heavy metal, pesticides, infectious waste, and toxins content.[21] These districts lie downstream of river Ganga which is primary source of water for drinking, washing, and irrigation purposes.[22] Furthermore, higher arsenic content in groundwater and soil has been postulated as strong risk factor for higher CaGB cases in Indo-Gangetic Belt in several studies.[23,24,25,26,27]
In our study, we tried to explore the hypothesis that population living along main river Ganga and in districts with higher soil arsenic levels have higher risk of developing CaGB. We analyzed all consecutive individual patients with CaGB reported in our RCC and registered in HBCR across 38 districts of Bihar over 3 years from January 2014 to December 2016. We assume that our list is fairly comprehensive as CaGB cases seen by other parallel primary disciplines such as general surgery, general medicine, gastrointestinal surgery, medical gastroenterology, and gynecology were also registered under HBCR. When compared with exposed and unexposed background population using 2011 census data in each of the 38 districts of Bihar, districts along central River Ganga and those in higher arsenic soil zone were found to have statistically significant risk of reporting CaGB cases, odds ratio of 1.72 (P < 0.0001), and odds ratio 1.45 (P < 0.0001), respectively, thus strengthening above two hypothesis and association.
Our institute being in state capital and primary referral apex tertiary cancer center had high likelihood of registering cases from proximal districts and hence could have strong referral bias. To evaluate this important variable, we analyzed whether reporting of CaGB cases was higher from districts within 100 km radius of our institute (traveling time <3 h by local transport) compared to rest of Bihar districts. The result came statistically significant with odds ratio 1.81 (P < 0.0001) suggesting strong referral/proximity bias in reporting CaGB cases. In our analysis, each successive year is showing a rise in cases registered as CaGB with 28% higher cases in 2016 compared to 2015. These high registrations may not be only explained by rising incidence of CaGB but also by improvement in healthcare including prompt diagnosis with more widely accessible ultrasonography, better road transportation, improved infrastructure, public awareness, and rising economy.
Being retrospective, our data lack several important demographic diseases and treatment-related variables such as symptoms at presentation, performance status, staging, tumor grade, histology, choice, and intent of therapy. Patna (n = 208) being the state capital registered 2.7 times higher cases of CaGB compared to second district Vaishali (n = 75). It is likely that some patients might have given Patna as their home address rather than their permanent native address due to their business in Patna or some of their relatives residing in State Capital, hence inflating cases registered under Patna. We cannot verify the registered address as true in every case as the data being retrospective with scarce follow-up. All three of our major analyses comparing districts around river Ganga, districts with high soil arsenic, and proximal referral districts had Patna and Vaishali as predominant contributors in groups favoring significant odds ratio. We cannot dissociate or ascertain the extent of contribution of this factor on overall significant association results. By restricting our choice for districts with high arsenic levels (>0.05 mg/dL), we do acknowledge lack of information regarding exact arsenic soil levels as threshold for carcinogenesis; hence, these values can be suboptimal for rational stratification. Similarly, stratification of districts with close proximity to Ganga and otherwise was based on rationale that silt based deposition of unknown toxins, heavy metals are higher along the main river compared to peripheral districts.
Conclusion
CaGB is a significant public health problem along Indo- Gangetic Belt. Population residing along River Ganga and those exposed to high soil arsenic levels have strong association for developing subsequent gallbladder cancer. Districts in Central and North Bihar have higher CaGB cases registered. Among several districts, State capital Patna has highest number of registered cases. Systematic population-based longitudinal studies are needed to confirm above hypothesis and initiate urgent public health measures if found significant to curb rising incidence of gallbladder cancer.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.SEER Database. [Last assessed on 2017 Oct 17]. Available from: https://www.seer.cancer.gov/faststats/selections.php?#Output .
- 2.GLOBOCON data. [Last assessed on 2017 Oct 17]. Available from: http://www.globocan.iarc.fr/Pages/fact_sheets_population.aspx .
- 3.National Centre for Disease Informatics and Research. Release of Reports PBCR and HBCR 2012-2014. [Last assessed on 2017 Oct 17]. Available from: http://www.ncrpindia.org/ALL_NCRP_REPORTS/PBCR_REPORT_2012_2014/ALL_CONTENT/PDF_Printed_Version/Chapter 2_Printed.pdf .
- 4.National Centre for Disease Informatics and Research. Release of Reports PBCR and HBCR 2012-2014. [Last assessed on 2017 Oct 17]. Available from: http://www.ncrpindia.org/ALL_NCRP_REPORTS/PBCR_REPORT_2012_2014/ALL_CONTENT/PDF_Printed_Version/Chapter 7_Printed.pdf .
- 5.Shukla VK, Khandelwal C, Roy SK, Vaidya MP. Primary carcinoma of the gall bladder: A review of a 16-year period at the university hospital. J Surg Oncol. 1985;28:32–5. doi: 10.1002/jso.2930280109. [DOI] [PubMed] [Google Scholar]
- 6.Khan I, Panda N, Banerjee M, Das R. Epidemiological factors in gall bladder cancer in eastern India-a single centre study. Indian J Surg Oncol. 2013;4:67–72. doi: 10.1007/s13193-012-0203-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.The Detail Analysis of Population Census 2011 Published by Govt. Of India for Bihar State. [Last assessed on 2017 Oct 17]. Available from: http://www.census2011.co.in/census/state/districtlist/bihar.html .
- 8.Indian State Census 2011. [Last assessed on 2017 Oct 17]. Available from: http://www.census2011.co.in/states.php .
- 9.Government of India. National Cancer Control Programme. [Last assessed on 2017 Oct 17]. Available from: https://www.web.archive.org/web/20111018014423.;http://www.india.gov.in/sectors/health_family/index.php?id=11 .
- 10.Indian Council of Medical Research, Hospital Based Cancer Registry. [Last assessed on 2017 Oct 17]. Available from: http://www.icmr.nic.in/ncrp/hbcr.pdf .
- 11.Randi G, Franceschi S, La Vecchia C. Gallbladder cancer worldwide: Geographical distribution and risk factors. Int J Cancer. 2006;118:1591–602. doi: 10.1002/ijc.21683. [DOI] [PubMed] [Google Scholar]
- 12.Zatonski WA, Lowenfels AB, Boyle P, Maisonneuve P, Bueno de Mesquita HB, Ghadirian P, et al. Epidemiologic aspects of gallbladder cancer: A case-control study of the SEARCH program of the international agency for research on cancer. J Natl Cancer Inst. 1997;89:1132–8. doi: 10.1093/jnci/89.15.1132. [DOI] [PubMed] [Google Scholar]
- 13.Nandakumar A, Gupta PC, Gangadharan P, Visweswara RN, Parkin DM. Geographic pathology revisited: Development of an atlas of cancer in India. Int J Cancer. 2005;116:740–54. doi: 10.1002/ijc.21109. [DOI] [PubMed] [Google Scholar]
- 14.Dhir V, Mohandas KM. Epidemiology of digestive tract cancers in India IV. Gall bladder and pancreas. Indian J Gastroenterol. 1999;18:24–8. [PubMed] [Google Scholar]
- 15.Prasad RR, Singh JK, Mandal M, Kumar M, Prasad SS. Profile of gall bladder cancer cases in Bihar. Indian J Med Paediatr Oncol. 2005;26:31. [Google Scholar]
- 16.Dixit R, Srivastava P, Basu S, Srivastava P, Mishra PK, Shukla VK, et al. Association of mustard oil as cooking media with carcinoma of the gallbladder. J Gastrointest Cancer. 2013;44:177–81. doi: 10.1007/s12029-012-9458-2. [DOI] [PubMed] [Google Scholar]
- 17.Unisa S, Jagannath P, Dhir V, Khandelwal C, Sarangi L, Roy TK, et al. Population-based study to estimate prevalence and determine risk factors of gallbladder diseases in the rural gangetic basin of north india. HPB (Oxford) 2011;13:117–25. doi: 10.1111/j.1477-2574.2010.00255.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Misra S, Chaturvedi A, Misra NC, Sharma ID. Carcinoma of the gallbladder. Lancet Oncol. 2003;4:167–76. doi: 10.1016/s1470-2045(03)01021-0. [DOI] [PubMed] [Google Scholar]
- 19.Sirohi B, Rastogi S, Singh A, Sheth V, Dawood S, Talole S, et al. Use of gemcitabine-platinum in indian patients with advanced gall bladder cancer. Future Oncol. 2015;11:1191–200. doi: 10.2217/fon.14.295. [DOI] [PubMed] [Google Scholar]
- 20.Ramaswamy A, Ostwal V, Pinninti R, Kannan S, Bhargava P, Nashikkar C, et al. Gemcitabine-cisplatin versus gemcitabine-oxaliplatin doublet chemotherapy in advanced gallbladder cancers: A match pair analysis. J Hepatobiliary Pancreat Sci. 2017;24:262–7. doi: 10.1002/jhbp.439. [DOI] [PubMed] [Google Scholar]
- 21.Uttam RS. Elemental Investigation of River Ganga Water by LIBS. [Last accessed on 2018 Mar 13]. Available from: http://www.indiaenvironmentportal.org.in/files/file/river%20ganga.pdf .
- 22.Dixit R, Shukla VK. Perspectives in Cancer Prevention-Translational Cancer Research. New Delhi: Springer; 2014. Why Is Gallbladder Cancer Common in the Gangetic Belt? pp. 145–51. [Google Scholar]
- 23.Nath A, Vendan PS, Kumar S, Kumar A, Singh JK. Toxicity due to arsenic in Gangetic zone of Patna, India and its linkage with cancer. J Environ Anal Toxicol. 2013;3:2161–525. [Google Scholar]
- 24.Kumar A, Ali M, Rahman SM, Iqubal AM, Anand G, Niraj PK, et al. Ground water arsenic poisoning in “Tilak Rai Ka Hatta” Village of Buxar District, Bihar, India Causing Severe Health Hazards and Hormonal Imbalance. J Environ Anal Toxicol. 2015;5:1. [Google Scholar]
- 25.Kumar, Arun, Ashok Ghosh, and Nandita Singh. The Human Right to Water. Springer, Cham; 2016. “Arsenic in Drinking Water: An Emerging Human Right Challenge in India.”; pp. 55–81. [Google Scholar]
- 26.Shukla VK, Prakash A, Tripathi BD, Reddy DC, Singh S. Biliary heavy metal concentrations in carcinoma of the gall bladder: Case-control study. BMJ. 1998;317:1288–9. doi: 10.1136/bmj.317.7168.1288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chhabra D, Oda K, Jagannath P, Utsunomiya H, Takekoshi S, Nimura Y, et al. Chronic heavy metal exposure and gallbladder cancer risk in India, a comparative study with japan. Asian Pac J Cancer Prev. 2012;13:187–90. doi: 10.7314/apjcp.2012.13.1.187. [DOI] [PubMed] [Google Scholar]


