Summary
Background
In the light of diagnostic and therapeutic advances, patients with a previous myocardial infarction or with a diagnosis of chronic obstructive pulmonary disease are vulnerable and need continuous monitoring over time. These pathological frameworks have a strong impact on the economy and on the status of the population and require effective and low-cost solutions.
Aims
The objective of this clinical trial is to evaluate the efficacy in the short term of a telephone counseling intervention to modify the lifestyles of these two patient populations.
Methods
In May 2015, all the patients included in the study underwent a questionnaire to evaluate their eating and smoking habits and their quality of life. After randomization in two groups, the intervention group received telephone counseling related to the correct lifestyles. The control group did not undergo any intervention. In September-October 2015, the same initial questionnaire was administered to evaluate changes in patients’ behavior.
Results
64 patients were included in the study: 34 were assigned to the intervention group and 30 to the control group. The outcomes evaluated were: quality of life, assessment of eating habits and smoking status. After the telephone counseling, the intervention group (34 persons) showed a significant improvement in the score of adherence to the Mediterranean diet (p = 0.01) and a significant reduction in the percentage of smokers (p = 0.01) compared to the population that did not receive any intervention (30 persons). On the other hand, the changes related to the quality of life questionnaire were not significant.
Conclusions
A single telephone counseling intervention is effective in modifying the lifestyles of patients with a previous myocardial infarction or diagnosed with chronic obstructive pulmonary disease in the short term, reducing their risk profile.
Keywords: Counseling, Tertiary prevention, Chronic disease, Nutrition, Smoke, Quality of life, Chronic obstructive pulmonary disease, Acute myocardial infarction
Introduction
Cardiovascular diseases are the first cause of death in the western world. In 2014 cardiovascular diseases were responsible for 29.5% of all deaths in Italy [1]. These pathological frameworks have a strong impact on the resources of the health system since they are not only the cause of the subject’s death, but often turn into chronic conditions that accompany the individual in the rest of his life and make him/her a vulnerable person. However, there is no effective cure for chronic obstructive pulmonary diseases (COPD) although several treatments are available to control the symptoms and avoid dangerous complications. In both these patient populations it is therefore essential to implement multidisciplinary secondary and tertiary prevention programs to reduce exposure to modifiable risk factors and in order to achieve maximum adherence to the therapeutic program.
In the literature, many epidemiological studies report high inhomogeneities in the incidence rate of cardiovascular diseases in relation to different geographical areas. Compared to the Northern Europe Countries and the United States, there is a lower incidence of coronary heart disease in the Countries of Southern Europe and in particular in those facing the Mediterranean basin such as France, Spain, Greece and Italy [2-4]. This geographical variability has been attributed to environmental factors, lifestyles and different eating habits, which in the Mediterranean Countries traditionally reflect the characteristics of the “Mediterranean Diet”. According to the LYON study, the Mediterranean diet decreases the mortality rate for coronary heart disease by 50% [5]. Other data show that an increase in adherence to the Mediterranean diet may result in a reduction in the overall incidence of cancer or mortality from cancer between 6 and 12% [6]. In fact, it is widely considered a food model to be pursued, both in primary and in secondary prevention, since it is substantially able to change the cardiovascular risk profile towards achieving and maintaining good health and longevity [7, 8]. The Guidelines for a Healthy and Correct Italian Food provide the “nutritional recommendations” that shape the characteristic Mediterranean diet: abundant consumption of fruit and vegetables, cereals, legumes, olive oil, fish, and, in less quantity, of meat, sausages, cheese and derivatives. An ideal dietetic pattern prefers poly and monounsaturated fats, in particular of the oleic acid contained in olive oil, limiting the intake of “trans” and saturated fats and cholesterol [7, 9].
At the same time, the tobacco epidemic is one of the most important public health challenges. The WHO estimates that in the world cigarette smoking kills about 6 million people every year, of which 5 million are smokers or former-smokers. About 50% of current smokers will die from cigarette-related illnesses [10]. Tobacco is a known or probable cause of at least 25 diseases, including chronic obstructive pulmonary disease (COPD) and other chronic lung diseases, oncological diseases, heart diseases and vasculopathies. Among the tumors, there is sufficient scientific evidence with respect to a direct causal relationship between cigarette smoking and tumor of lung, larynx, oral cavity, pharynx, esophagus, pancreas, bladder, cervix, stomach and acute myeloid leukemia [11]. The risk of premature death and the likelihood of developing smoking-related diseases depend on several factors, including the number of years spent smoking, the number of cigarettes daily smoked, the starting and terminating age of smoking, and if the person was already ill at the time of smoking cessation.
Considering the scientific evidences of literature on the important health consequences deriving from modifiable lifestyles, it is necessary to consider the need to actively intervene on these aspects. Particularly interesting for possible health outcomes are the most susceptible populations, i.e. those diagnosed with previous acute myocardial infarction (AMI) or COPD.
Preventive Medicine, by enhancing the factors useful to health and the removal or correction of causes and states of predisposition and/or risk to the disease, cooperates to achieve a state of complete physical, mental and social well-being of the individual and the community. At the same time, it contributes to decrease the costs of the health services, reducing disability and increasing work capacity. In order to achieve this goal, Health Promotion is an effective tool expressly aimed at promoting, modifying or eliminating behaviors capable of influencing the health conditions of individuals and of the population.
The objective of this research study is to estimate, through a pilot randomized clinical trial, the efficacy of a tertiary prevention counseling intervention on patients with AMI and COPD in reducing tobacco use and increasing food behavior and health-related quality of life.
Materials and methods
The study population was made of patients previously involved as cases in a case-control study that investigated the factors associated with the etiopathogenesis of the considered clinical scenery [12]. Patients who accepted to participate in the study were 64: 33 patients included as cases with AMI and 31 patients included as cases with COPD (Fig. 1). All patients included in the study received and signed the informed consent to participate. The study received approval from the Ethics Committee of the Policlinic Umberto I of Rome.
Fig. 1.
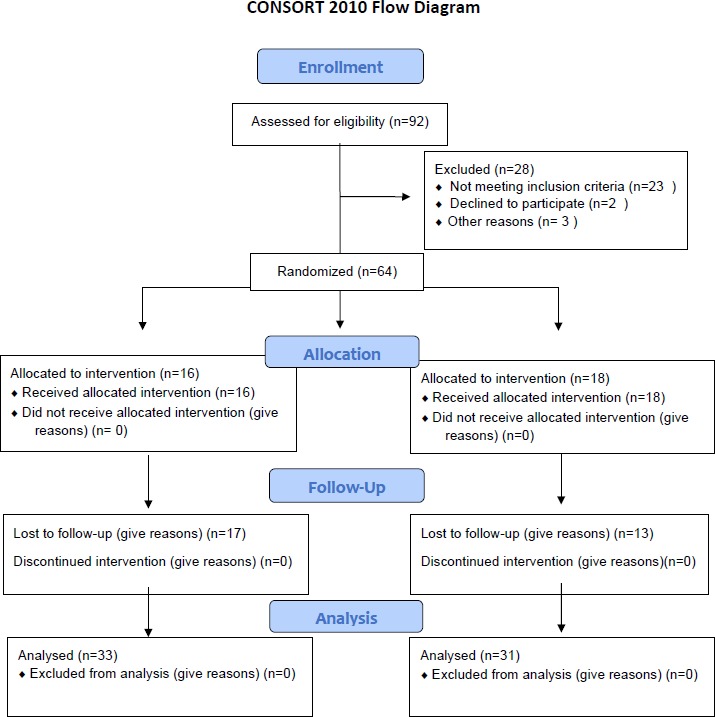
Flow diagram of the participants of the study.
The subjects included in the study as cases with myocardial infarction were patients admitted to the Coronary Units after a first myocardial infarction event (ICD-9 code: 410-14), male and female, aged between 35 and 70, with intact state of consciousness and capacity for judgment.
Concerning the COPD patients, they were admitted to the Respiratory Diseases Unit with an established diagnosis of COPD according to the GOLD Guidelines and classified as COPD, COPD exacerbation, chronic respiratory failure, chronic bronchitis or pulmonary emphysema. The sample included male and female subjects, between the ages of 40 and 80, with intact state of conscience and capacity for judgment.
Patients of each of the two diagnostic categories considered, AMI and COPD, were divided into 4 groups based on exposure to “smoking” and “poor diet” risk factors. For each pathological category were therefore obtained: a group of exposure to both risk factors; a group of exposure to smoking and not to bad diet; a group of exposure to bad diet and not to smoking; a group of non-exposure to any of the two risk factors. Within each of these subsets, the patients were randomly referred to an intervention group or to a control group. The randomization of the subjects was performed using the random numbers tables. Following randomization, 34 patients were assigned to the intervention group and 30 to the control group.
All the study participants in May 2015 were given a questionnaire comprising a registry section gathering information on sex, marital status, number of children, number of family members, educational level and smoking status (current, former or never smoker).
To assess the differences between the two groups at the end of the study, before and after the intervention a questionnaire was administered to all the participants that investigated eating habits (SUN PROJECT questionnaire) and smoking habits (exposure to cigarette smoke), Fagerström’s smoking addiction test and Mondor’s smoking cessation test [13]. Quality of life was measured using the SF-12 questionnaire from which their MCS (Summary of mental components) and their PCS (Physical Component Summary) were calculated [14].
In May 2015, patients who were part of the intervention group were contacted by telephone with the aim of encouraging adherence to the Guidelines for a healthy and correct diet, giving further food advices, answering doubts, questions or clarifications, and promoting cessation of smoking habit.
Patients’ nutrition education interventions took place through counseling activities and training interventions by experts in Food Science: after the assessment of eating habits and the assessment of the degree of adherence to the Mediterranean diet, the health professionals gave provisions regarding food in accordance to the Guidelines for a healthy and correct diet (INRAN) [9, 15].
The interventions on smokers who suffered of heart attack or who have been diagnosed with mild or moderate COPD had the aim to promote the motivation to quit, to inform smokers about the resources available for cessation and to direct the smoker to planned routes. These counseling interventions were structured in the light of the “Clinical Guidelines to encourage the cessation of smoking habits” drawn up by the National Institute of Health which provides a list of suggestions, called the 5 A’s for a good structure:
ASK = ask the subject if he smokes;
ADVISE = information on the effects of smoking and recommend to quit;
ASSESS= define the characteristics of the subject;
ASSIST = verify and implement a therapeutic path to monitor and reinforce cessation;
ARRANGE = implement actions to prevent relapse [16].
In the period between September and October 2015, all the participants were contacted again in order to collect the same data on tobacco smoking, dietary behavior and health-related quality of life.
Results
A descriptive analysis was performed considering the data obtained from the personal data section of the administered questionnaire. The patients who underwent the intervention were 26 males (76.5%) and 8 females (23.5%). Those who were assigned to the control group were 19 males (63.3%) and 11 females (36.7%). Regarding marital status, most patients in the intervention group were married (23 people, 67.6%), 18 patients (52.9%) claimed to have two children and 14 (41.2%) cohabited with two people. The general educational level was medium since 9 patients (26.5%) declared that they only attended elementary schools, 13 patients (38.2%) junior high schools, 7 patients (20.6%) high schools, and only 5 patients (14.7%) held a bachelor’s degree. In the control group, on the other hand, most patients were married (19 people, 63.3%), 11 patients (36.7%) claimed to have three children and 14 (46.7%) lived with two people. In this case, the general educational level was medium-low since 9 patients (30.0%) attended elementary schools, 13 patients (43.3%) middle schools and 8 patients (26.7%) high schools.
In the period before the telephone intervention, the smoking patients who were assigned to the intervention group were 15 (44.1%) while the non-smokers were 19 (55.9%). In the control group, 11 patients (36.7%) were smokers, 19 (63.3%) were non-smokers. Therefore, at the initial randomization, the two groups taken into consideration for the study were very similar, except for the variable “number of children” which did not seem to be crucial for the purposes of the statistical analysis. The results of the descriptive analysis are shown in Table I.
Tab. I.
Baseline socio-demographic characteristics of the patients.
| Variable | Intervention group (%) | Control group (%) | p |
|---|---|---|---|
| SEX Male Female |
26 (76.5%) 8 (23.5%) |
19 (63.3%) 11 (36.7%) |
0.251 |
| CIVIL STATUS Single Married Divorced Widower |
3 (8.8%) 23 (67.6%) 4 (11.8%) 4 (11.8%) |
2 (6.7%) 19 (63.3%) 4 (13.3%) 5 (16.7%) |
0.931 |
| SONS 0 1 2 3 4 5 6 |
3 (8.8%) 4 (11.8%) 18 (52.9%) 2 (5.9%) 4 (11.8%) 2 (5.9%) 1 (2.9%) |
3 (10.0%) 6 (20.0%) 6 (20.0%) 11 (36.7%) 3 (10.0%) 1 (3.3%) 0 (0.0%) |
0.031 |
| COHABITANTS 1 2 3 4 5 6 |
7 (20.6%) 14 (41.2%) 7 (20.6%) 6 (17.6%) 0 (0.0%) 0 (0.0%) |
6 (20.0%) 14 (46.7%) 5 (16.7%) 3 (10.0%) 1 (3.3%) 1 (3.3%) |
0.673 |
| EDUCATIONAL LEVEL Elementary school Junior high school High school Degree |
9 (26.5%) 13 (38.2%) 7 (20.6%) 5 (14.7%) |
9 (30.0%) 13 (43.3%) 8 (26.7%) 0 (0.0%) |
0.184 |
| SMOKING STATUS Yes No |
15 (44.1%) 19 (55.9%) |
11 (36.7%) 19 (63.3%) |
0.545 |
After 4-5 months, in September-October 2015, all the patients included in the study were contacted by telephone to investigate the variations in the answers to the same questionnaires administered before the intervention. All the patients included in the study answered to the follow up questionnaire. The results emerged from the statistical analysis are shown in Table II.
Tab. II.
Results of the trial concerning HR-QoL scales, diet and tobacco use.
| Variable | Intervention group | Control group | P |
|---|---|---|---|
| PCS pre (all) PCS post (all) p |
34.3 (21 - 56.7) 33.3 (21-57.5) 0.877 |
35.8 (20.8 - 59.6) 33.7 (19.5-54.7) 0.514 |
0.476 0.941 |
| AMI pre AMI post p |
40.6 (23.6 - 56.7) 39.8 (24.6 - 57.5) 0.861 |
49.8 (20.8 - 59.6) 38.8 (19.5 - 54.7) 0.022 |
0.276 0.606 |
| COPD pre COPD post p |
32.3 (21 - 41.7) 31.6 (21 - 40.9) 1.00 |
32.1 (24.9 - 42.6) 32.5 (23.9 - 37) 1.00 |
0.890 0.831 |
| MCS pre (all) MCS post (all) p |
40.4 (22.6-59.5) 42.4 (22.5 - 56.2) 0.427 |
35.7 (25.8-66.9) 39.9 (25.8 - 52.5) 0.293 |
0.861 0.213 |
| AMI pre AMI post p |
39.4 (27.9 - 58.6) 42.9 (28.1 - 56.2) 0.134 |
48.2 (32.6 - 66.9) 46.7 (27.8 - 52.5) 0.831 |
0.045 0.901 |
| COPD pre COPD post p |
41.3 (22.6 - 59.5) 42.1 (22.5 - 49.6) 1.00 |
35.9 (25.8 - 46.7) 30.3 (25.8-47) 1.00 |
0.03 < 0.01 |
| DIET SCORE | 7 (3-9) | 5 (3-9) | 0,010 |
| SMOKING STATUS Before After |
44,1% 20,6% |
36,7% 26,7% |
< 0.01 |
Nonparametric tests were used, and median values were taken into account. After the telephone intervention, analyzing the median values of the MCS and PCS, there were no improvements in the quality of life of the patients. The p values of the PCS and MCS variables do not indicate a significance in terms of effectiveness of the telephone intervention (p = 0.941 and p = 0.213, respectively). Analyzing the subgroups of the AMIs and the COPD a significance is shown on the MCS mental score for COPD patients.
Statistical analysis shows positive trends related to patient follow-up in terms of adherence to the Mediterranean diet and cessation of smoking habits. From the results of the collected data can be seen a greater adherence to the Mediterranean diet of the patients undergoing the intervention rather than the patients in the control group. Considering a range from 3 to 9, the medians of the Intervention group and the Control group were different. In fact, the Diet score is 7 in the intervention group and 5 in the control group. P = 0.01 indicates a high validity of the effectiveness of the telephone intervention.
As far as concerns smoking, in the control group the percentage of smokers at the time of admission was 36.7% and that at September follow-up was 26.7%, with a difference of 10.0 %. In the intervention group, the difference has doubled. At zero time, the percentage of patients who declared smoking was 44.1% while following the telephone intervention, the percentage of smokers fell to 20.6%, highlighting a difference between the pre- and post-intervention of 23.5%. Also in this case the p = 0.01 indicates a high significance and therefore the effectiveness of the telephone intervention performed on the patients. In addition to the parameters of the ARR of 26.1% and RRR of 1.96, the NNT equal to 3.8 highlights the effectiveness of the treatment: this value indicates the estimate of the number of patients to be submitted to treatment to obtain a unit of advantage over the comparison treatment.
Discussion
This scientific project is based on the evidence that the chronic patient, and in particular the patient with AMI and with COPD, is called to be an active subject, who must become independent and protagonist of the management of his own condition, together with the healthcare professional. There is evidence that not only pharmaceutical treatment is needed for patients with chronic conditions, while more interest is needed to non-pharmacological lines of treatment [17].
The concept of care comes to detach from the usual imaginary of making a diagnosis, prescribing a therapy and assisting the person in acute. Health promotion interventions are permanent, integrated and patient-centered processes and there is scientific evidence that after an AMI event, being smoker negatively correlates with the individual’s HLR-QoL [18]. The individual must be exposed to sensitization, information, learning and psychological support activities concerning his disease, the therapies and the behaviors to be implemented to prevent complications.
This study shows that, beneath the differences related to quality of life were not relevant, after the telephone counseling the intervention group showed a significant improvement in the score of adherence to the Mediterranean diet and a significant reduction in the percentage of smokers. However, other psychosocial smoking cessation interventions based on behavioral therapeutic approaches and telephone support, showed to be effective at 1 year follow up, in promoting abstinence in patients affected by coronary heart disease [19].
The strengths of this study are represented by the short-term effectiveness demonstrated in modifying the life habits of the patients involved and by the fact that this result was obtained in an economic way, after one single telephone counseling intervention.
Weaknesses are represented by the limited number of the sample population and by the evaluation of the outcomes which is limited to short-term and therefore does not give any information about the permanence of behavioral changes induced in patients. The improvement of lifestyle, although initially difficult to achieve because it aims to modify behavioral aspects deeply rooted in the population, is a process that produces significant changes in the health of the subject. The intervention helps the patient and his family to understand the pathology, to live healthier and improve their quality of life.
Conclusions
The project aims to modify the lifestyles to reduce the incidence of the main chronic-degenerative diseases and decreasing the mortality rate for coronary heart disease. It has shown that even with a single telephone counseling intervention is effectively possible to intervene on the education of the patient in the post-acute period about his illness. It helps to implement the strengthening of the awareness and the ability to choose of the individual through the promotion of good eating habits and the benefits resulting from the cessation of cigarette smoking. This study is a good starting point for carrying out larger studies, with repeated counseling interventions over time and long-term efficacy evaluation. Further fields of investigation could be represented by the evaluation of the outcomes also in terms of health, assessing the differences in the percentages of complications, exacerbations and hospitalizations between a population of patients who received the intervention and a population that did not receive any intervention.
Acknowledgements
No potential conflict of interest relevant to this article was reported.
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Footnotes
Authors’ contributions
GLT, RAC, MC and ELS conducted the literature search, the selection of articles, data extraction and write-up of the manuscript. RS, AF, MM, LA, RS and AM, were involved in the design of the study and revision of the paper.
References
- [1].ISTAT. L’evoluzione della mortalità per causa: le prime 25 cause di morte, ISTAT - www.istat.it/it/archivio/199352
- [2].Keys A, Menotti A, Karvonen MJ, Aravanis C, Blackburn H, Buzina R, Djordjevlc BS, Dontas AS, Fldanza F, Kromhout D, Nedeljkovic S, Punsar S, Seccareccia F, Toshima H. The diet and 15-year death rate in the seven countries study. Am J Epidemiol 1986;124:903-15. [DOI] [PubMed] [Google Scholar]
- [3].Tunstall-Pedoe H, Kuulasmaa K, Mähönen M, Tolonen H, Ruokokoski E, Amouyel P. Contribution of trends in survival and coronary-event rates to changes in coronary heart disease mortality: 10-year results from 37 WHO MONICA project populations. Monitoring trends and determinants in cardiovascular disease. Lancet 1999;353:1547-57. [DOI] [PubMed] [Google Scholar]
- [4].Masiá R, Pena A, Marrugat J, Sala J, Vila J, Pavesi M, Covas M, Aubó C, Elosua R. High prevalence of cardiovascular risk factors in Gerona, Spain, a province with low myocardial infarction incidence. REGICOR Investigators. J Epidemiol Community Health 1998;52:707-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Kris-Etherton P, Eckel RH, Howard BV, St Jeor S, Bazzarre TL. AHA Science Advisory: Lyon Diet Heart Study. Benefits of a Mediterranean-style, National Cholesterol Education Program/American Heart Association Step I dietary pattern on cardiovascular disease. Circulation 2001;103:1823-5. [DOI] [PubMed] [Google Scholar]
- [6].WHO. Regional office for European. Public health action for healthier children and population. The European Health Report 2005. [Google Scholar]
- [7].Trichopoulou A, Kouris-Blazos A, Wahlqvist ML, et al. Diet and overall survival in elderly people. BMJ 1995;311:1457-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Iestra J, Knoops K, Kromhout D, et al. Lifestyle, Mediterranean diet and survival in European post-myocardial infarction patients. Eur J Cardiovasc Prev Rehabil 2006;13:894-900. [DOI] [PubMed] [Google Scholar]
- [9].Linee Guida per una Sana e Corretta Alimentazione Italiana- Istituto Nazionale di Ricerca per gli Alimenti e la Nutrizione, Roma, 2003. [Google Scholar]
- [10].WHO, Report on the Global Tobacco Epidemic, 2015. [Google Scholar]
- [11].Gandini S, Botteri E, Iodice S, Boniol M, Lowenfels AB, Maisonneuve P, Boyle P. Tobacco smoking and cancer: a meta-analysis. Int J Cancer 2008;122:155-64. [DOI] [PubMed] [Google Scholar]
- [12].La Torre G, Saulle R, Di Murro F, Siliquini R, Firenze A, Maurici M, Mannocci A, Colamesta V, Barillà F, Ferrante F, Agati L. Mediterranean diet adherence and synergy with acute myocardial infarction and its determinants: a multicenter case-control study in Italy. PLOS One 2018;13(3):e0193360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Heatherton TF, Kozlowski LT, Frecker RC, Fagerstrom KO. The Fagerstrom Test for nicotine dependence: a revision of the Fagerstrom Tolerance Questionnaire. Br J Addict 1991;86:1119-27. [DOI] [PubMed] [Google Scholar]
- [14].Ware J, Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care 1996;34:220-33. [DOI] [PubMed] [Google Scholar]
- [15].Galbete C, Toledo E, Toledo JB, et al. Mediterranean diet and cognitive function: the SUN project. J Nutr Health Aging 2015;19:305-12. [DOI] [PubMed] [Google Scholar]
- [16].Istituto Superiore di Sanità - Linee guida cliniche per promuovere la cessazione dell’abitudine al fumo. Roma, 2008. [Google Scholar]
- [17].Allam MF, Arjona O. Health promotion or pharmacological treatment for chronic diseases? J Prev Med Hyg 2013;54:11-3. [PMC free article] [PubMed] [Google Scholar]
- [18].Buchanan DM, Arnold SV, Gosch KL, Jones PG, Longmore LS, Spertus JA, Cresci S. Association of smoking status with angina and health-related quality of life after acute myocardial infarction. Circ Cardiovasc Qual Outcomes 2015;8:493-500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Barth J, Critchley J, Bengel J. Psychosocial interventions for smoking cessation in patients with coronary heart disease. Cochrane Database Syst Rev 2008;(1):CD006886. [DOI] [PubMed] [Google Scholar]


