Abstract
BACKGROUND:
Survival rates for children with cancer have significantly increased over the past 35 years. However, adolescents with cancer aged 15 to 19 years have had less progress in survival prolongation compared with younger children, which may be due to lower clinical trial enrollment among adolescents with cancer. To help address this issue, the Centers for Disease Control and Prevention (CDC) convened a series of webinars to identify salient issues and measures to address this problem. This supplement is intended to raise awareness about the unique challenges of clinical trial enrollment among adolescents with cancer.
METHODS:
The CDC convened a workgroup of researchers and health care providers in the field of adolescent and young adult oncology and cancer survivorship to examine the barriers and challenges limiting the participation of adolescents in clinical trials and to define ways to improve on these concerns.
RESULTS:
The workgroup identified 3 distinct issues affecting clinical trial enrollment among adolescents with cancer: (1) many adolescents with cancer are not referred to institutions where clinical trials are offered, (2) there are limited numbers of clinical trials for adolescents with cancer, and (3) psychosocial barriers impede adolescents with cancer from enrolling in clinical trials.
CONCLUSIONS:
Adolescents with cancer have the smallest proportion and least number of patients enrolled in clinical trials in pediatric oncology. Successfully addressing this challenge requires improving referral to existing clinical trials, addressing regulatory barriers to clinical trial enrollment, increasing the number of clinical trials for adolescents, and addressing unique psychosocial barriers to clinical trial enrollment. Pediatrics 2014;133:S85—S90
Keywords: clinical trial, enrollment, adolescent
The increasing survival of children with cancer has been one of the greatest success stories in the practice of medicine during the past half century. Childhood cancer mortality has decreased by >50% from 1975 to 2006.1,2 Much of this substantial improvement in survival is directly attributable to increasing enrollment of children with cancer in clinical trials.2–5 Clinical trials allow more effective therapeutic treatments to be identified and provided to patients with cancer. For many decades, national clinical trials designed for children were primarily focused on children <15 years of age.6 Indeed, the first national clinical trials in the United States were conducted in the mid-1950s in young children with acute lymphoblastic leukemia and Wilms tumor who were predominantly <5 years of age. The focus on younger children has resulted in a lack of clinical trials for older adolescents aged 15 to 19 years of age. The proportion of patients with cancer enrolled in a National Cancer Institute (NCI)-sponsored treatment trial has been shown to decrease with age (Fig 1).7 Although the majority of children under the age of 15 years are enrolled in clinical trials, <20% of adolescents aged 15 to 19 years are enrolled in clinical trials.3–5,7–10 This situation has led to gaps in survival rates between adolescents and younger children for many types of cancer (Fig 2). Across most pediatrictype cancers, children >15 years of age have had less progress in survival prolongation compared with children <15 years of age.11–14 Figure 3 displays the annual observed survival of all invasive cancers in 15- to 19-year-olds and 0- to 14-year-olds from 1975 to 2004. Survival among 15- to 19-year-olds was relatively constant from 1986 to 2002, during which children <15 years of age continued to have improved survival and, by the early 1990s, caught up with 15- to 19-year-olds. Since 2000, 15- to 19-year-olds have had some improvement in overall survival such that both age groups have had similar survival prolongation. The lack of clinical trial enrollment among adolescents with cancer undoubtedly has played a central role in the lack of improved survival in this population. One reason adolescents with cancer are not enrolled in clinical trials is the treatment setting in which they receive care. Adolescents suspected of cancer are referred by primary care physicians to either pediatric or adult oncologists. However, there is increasing evidence that adolescents treated by pediatric oncologists and at NCI-sponsored cancer centers are more likely to be enrolled in a clinical trial. Despite this finding, more adolescents are treated by adult oncologists and referrals to adult oncologists increase with the increasing age of adolescents.15–18 This is shown in Fig 4: with every year of age above 14, the proportion of newly diagnosed patients with cancer referred to the only children’s hospital in the region declined an average of 14% per year, from 85% in 14 year-olds to <5% in 21-year-olds. A small proportion of the age group was referred to the comprehensive cancer center at the region’s academic medical center. The majority remained in private practice, with approximately one-third of these at practices not certified by the American College of Surgeons. Because the treatment setting in which adolescents are referred to receive their cancer workup and treatment is so critical, pediatricians play a key role in shaping the long-term outcomes of adolescents with cancer.
FIGURE 1.
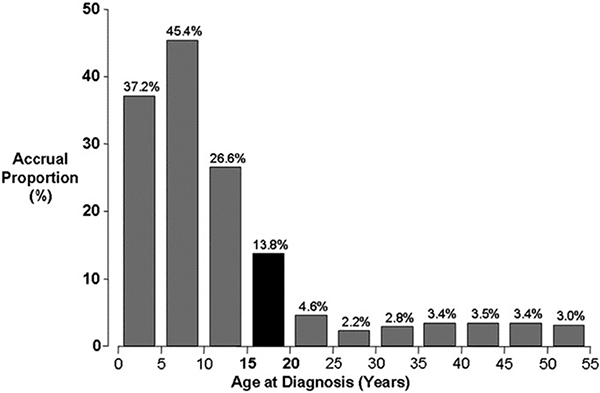
Estimated proportion of patients with cancer entered in NCI-sponsored treatment trials, 1997–2005. The black bar represents patients age 15–19 years with cancer entered in NCI-sponsored treatment trials. Clinical trials accrual data were provided by the Cancer Therapy Evaluation Program, NCI. Population data were obtained from the US Census Bureau.7
FIGURE 2.
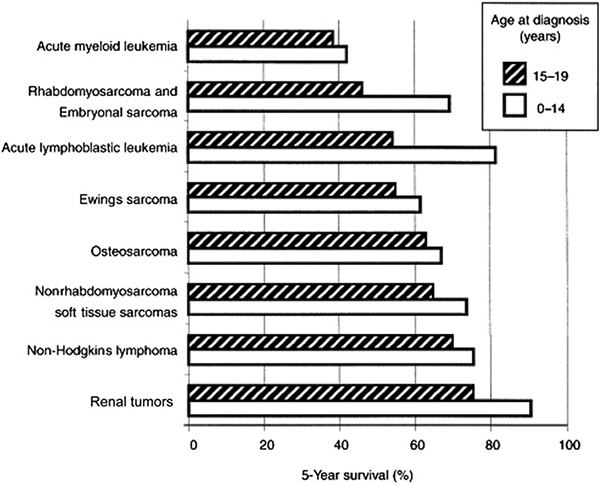
Gap in survival rates for selected cancers in 15- to 19-year-olds versus those in < 15-year-olds.14
FIGURE 3.
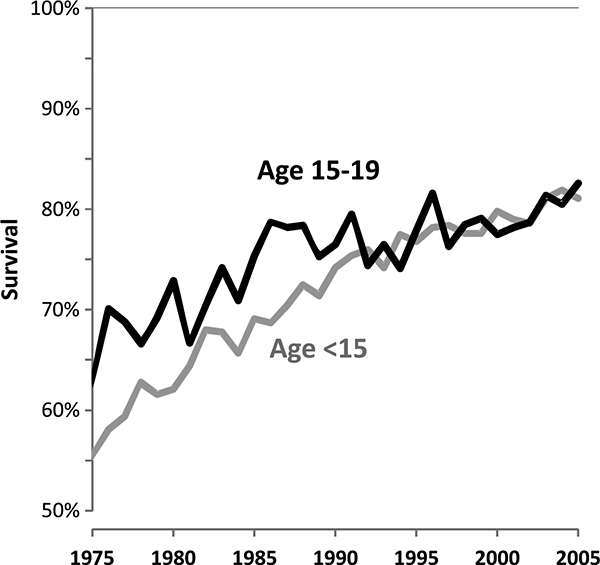
Annual 5-year observed survival for all invasive cancers, 1975–2004: Surveillance, Epidemiology, and End Results.
FIGURE 4.
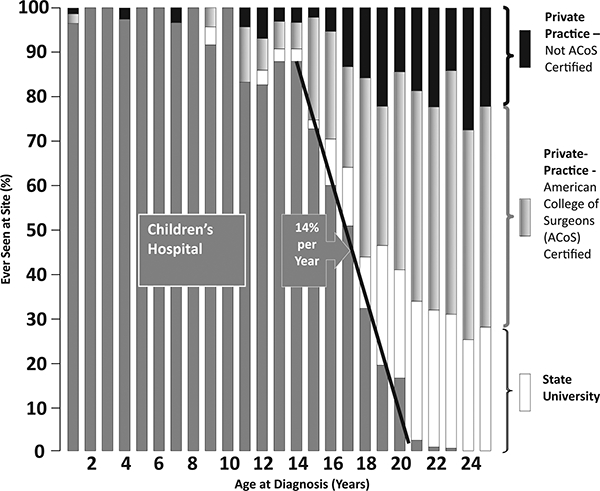
Referral patterns of patients with newly diagnosed cancer before age 25, by age, to the state children’s hospital and the state university adult center. Modified from reference 16.
The Carolyn Price Walker Act of 2008 authorized federal agencies to expand and enhance research, surveillance, and awareness activities related to pediatric cancer, including improving access to clinical trials for children with cancer.19 To ensure that adolescents shared in the improvements in cancer survival seen among younger children, the CDC initiated a project to identify the salient issues and measures to address this problem. We first performed a literature review of the available evidence on this topic. Next, we convened an informal workgroup of leading pediatric and adult oncologists, behavioral scientists, nurses, and researchers from academia and government (Table 1). We then held a series of 3 webinars with the workgroup to define barriers to clinical trial enrollment and to provide recommendations on addressing them. This monograph, which includes a series of articles, is intended to raise awareness among pediatricians, the predominant type of primary care physician caring for adolescents, about the unique challenges of clinical trial enrollment among adolescents with cancer.
Table 1.
Workgroup Members
| Karen Albritton | Cook Children’s Medical Center Fort Worth TX |
| Ronald Barr | McMaster University Hamilton ON |
| Lynda Kwon Beaupin | Roswell Park Cancer Institute, Buffalo NY |
| Archie Bleyer | Oregon Health Science University St. Charles Regional Cancer Center Bend OR |
| Rebecca Block | Oregon Health Science University Portland OR |
| Peter Coccia | University of Nebraska Medical Center Omaha NE |
| Deborah Vollmer Dhalke | Texas A&M, Seton Family of Healthcare, College Station, TX |
| Judy Felgenhauer | Providence Sacred Heart Medical Center & Children’s Hospital, Spokane WA |
| Steven Friedman | National Cancer Institute - Cancer Therapy Evaluation Program, Bethesda MD |
| Abha Gupta | Hospital for Sick Children, Toronto ON |
| Brandon Hayes-Lattin | Oregon Health Science University, Portland OR |
| Casey Flooke | Children’s Hospitals and Clinics of Minnesota, Minneapolis MN |
| Daniel Indelicato | University of Florida, Jacksonville, FL |
| Rebecca Johnson | Seattle Children’s Hospital, Seattle WA |
| Susan Lindemulder | Oregon Health Science University, Portland OR |
| Margo Michaels | Education Network to Advance Clinical Trials (ENACCT), Bethesda MD |
| Nita Seibel | National Cancer Institute - Cancer Therapy Evaluation Program, Bethesda MD |
| Leonard Sender | Children’s Hospital of Orange County, Orange CA |
| Peter Shaw | Children’s Hospital of Pittsburgh, Pittsburgh PA |
| Ashley Wilder Smith | National Cancer Institute, Bethesda MD |
RESULTS
On the basis of 3 workgroup webinars, 3 distinct issues were identified that may explain why adolescents with cancer in the United States have not fared as well as the younger pediatric population:
many adolescents with cancer are not referred to NCI-sponsored institutions where clinical trials are offered;
there are limited numbers of clinical trials for adolescents with cancer and increasing their availability is difficult; and
psychosocial barriers impede adolescents from enrolling in clinical trials.
Webinar 1: “Potential Barriers to Clinical Trial Enrollment Among Adolescent Cancer Patients”
Daniel Indelicato and Archie Bleyer reported the lack of available clinical trials for adolescents. This was illustrated by lymphoma clinical trials among adolescents. Although the incidence of lymphoma is relatively high among adolescent patients compared with other pediatric cancers, there are limited available treatment clinical trials for these patients.20 This situation was also revealed by the University of Pittsburgh Medical Center Cancer Center’s (UPMC-ML’s) and Children’s Hospital of Pittsburgh’s (CHP’s) experience. At UPMC and CHP, the rate of adolescents enrolled in clinical trials was lower than that of the younger pediatric population and may have been due to the lack of available trials at the time of their diagnosis.10
Simply increasing the number of clinical trials for adolescents and young adults (AYAs) is not feasible, as pointed out by Abha Gupta and Daniel Indelicato in this monograph series. As a member of the Children’s Oncology Group Soft Tissue Sarcoma Steering Committee, Gupta recognizes that it is challenging to design clinical trials when survival rates are already high in some diseases, but continued efforts are needed in incorporating AYA-specific aims into cooperative group trials. Although collaboration between pediatric and adult oncology cooperative groups is ideal, the complexities of regulatory barriers may overshadow the pursuit of such partnerships as shown by Judy Felgenhauer, Vice-Chair of the Children’s Oncology Group AYA Steering Committee.
Webinar 2: “Where Are Adolescent Cancer Patients Being Treated and What’s Going on in Their Heads?”
This session focused on the regulatory barriers that exist across different hospital settings and among pediatric and adult hospitals. Adolescents with cancer are often not treated at centers where clinical trials are offered, or if they are, these trials often have an age cutoff to include only those who are >18 years old. Pediatric and adult hospitals, sometimes within the same institution, may have separate in stitutional review boards, hindering enrollment in clinical trials that encompass both adolescents and young adults. The lack of use of a central institutional review board also limits the enrollment of adolescents from different institutions within a study. Unfortunately, there is no easy solution for such instances, and Felgenhauer et al outline some regulatory issues through different patient scenarios.
Despite regulatory issues and a decline in the number of clinical trials available for adolescents, data indicate that even within institutions treating children and adolescents, the latter group has decreased accrual rates onto clinical trials. There seems to be some promise in dedicated AYA programs that many cancer centers have established to help address this issue. At UPMC, it was noted that more AYAs are being treated at UPMC-ML, but those treated at CFIP had a higher enrollment rate in clinical trials.21,22 Since the establishment of the AYA program at UPMC, there has been an increase in the number of young adults 15 to 22 years of age enrolled in a clinical trial. In this monograph, Peter Shaw, head of the AYA program at UPMC, focuses on how to increase the opportunities for adolescents to enroll in studies.
A significant feature of both webinars 1 and 2 was the psychosocial aspect of adolescents. A large part of AYA oncology rests on the recognition that AYAs have psychosocial issues unique to this population. Studies have shown that AYAs with cancer have more distress associated with a cancer diagnosis23,24 compared with younger patients, and adolescent cancer survivors report having a worse quality of life than both survivors of childhood cancer25 or their age-matched healthy peers.26 Flow this affects treatment decisions is unclear, more so when considering whether psychosocial challenges affect AYAs in enrolling in clinical trials. The AYA Health Outcomes and Patient Experience is a population-based cohort study in AYAs with cancer that is supported by the NCI. This longitudinal study included patients with cancer who were 15 to 39 years of age diagnosed between July 2007 and October 2008 and includes addressing clinical trial involvement among AYA patients27 The psychosocial barriers to clinical trial enrollment and adherence are further discussed by Natasha Buchanan in this monograph.
A major clinical trial enrollment barrier identified through the webinarswas the decreased number of referrals of AYAs with cancer to an NCI-sponsored institution. Adolescents are often treated at community hospitals and private oncology practices.16,17 The drop-off in referral rates to a children’s hospital among adolescents over the age of 15 years of age is dramatic and helps explain the decline in enrollment in NCI-sponsored trials. Across most pediatric types of cancers, children >15 years of age generally have lower overall survival rates compared with children <15 years. Karen Albritton and Peter Coccia address this topic in this monograph and provide recommendations on how referral rates can improve.
Webinar 3: Summary
On the basis of discussion from the first 2 webinars, webinar 3, led by workgroup chair Archie Bleyer, focused on identifying key barriers to clinical trial enrollment. One key barrier was that adolescents are not referred to institutions at which clinical trials are offered. A second barrier is the limited number of clinical trials available for adolescents with cancer. Even if adolescents are referred to appropriate treatment settings, there may not be a trial available for those patients and increasing the number of trials is difficult. Psychosocial barriers are a third key obstacle to increasing adolescent enrollment in clinical trials. Addressing these barriers will require increased awareness of these issues among referring physicians, closer collaboration between physicians, and increased research efforts. Efforts to increase awareness about survival trends, empower adolescents and famiIies about treatment choices, and support local efforts focused on AYA cancers are also needed.
CONCLUSIONS
This project revealed that, across all pediatric cancers, adolescents 15 to 19 years of age have poorer outcomes compared with younger patients across disease types and have the smallest proportion and least number of patients enrolled in clinical trials in pediatric oncology.
Since these webinars were held, in 2012, changes are starting to be implemented. As mentioned in Gupta and Indelicato’s report in this monograph, the NCI has introduced a comprehensive plan to transform the previous NCI-sponsored Clinical Trials Cooperative Group Program, which funded several separate organizations conducting cancer treatment trials, into a new consolidated and integrated program referred to as the NCI National Clinical Trials Network. This new program will allow access to clinical trials offered by a number of cooperative oncology groups regardless of which group the treating oncologist may be a member of.
In 2012, the National Comprehensive Cancer Network (NCCN) published the first-ever AYA clinical practice guidelines.28 The NCCN is a not-for-profit alliance of 21 leading cancer centers dedicated to improving the quality and effectiveness of care provided to patients with cancer. The establishment of the NCCN AYA guidelines is instrumental in increasing the awareness among oncologists about AYA cancers and may have an impact on referral patterns of AYA patients.
The barriers identified through this series of webinars are straightforward yet challenging. Successfully addressing these challenges will require improving referral to existing clinical trials, addressing regulatory barriers to clinical trial enrollment, increasing the number of clinical trials for adolescents, and addressing the unique psychosocial barriers to clinical trial enrollment and adherence for adolescents with cancer. Primary care physicians, and in particular pediatricians, play a key role in addressing these challenges. Closer engagement between pediatriciansandthepediatricandadult oncology communities is needed to ensure that adolescents with cancer are referred to physicians and treatment centers that provide access to clinical trials. Collaboration between pediatricians and oncologists is also needed for the long-term well-being of adolescents with cancer.
Acknowledgments
FUNDING: All funding for this project and analysis was provided by the Centers for Disease Control and Prevention.
ABBREVIATIONS
- AYA
adolescents and young adults
- CDC
Centers for Disease Control and Prevention
- CHP
Children’s Hospital of Pittsburgh
- NCCN
National Comprehensive Cancer Network
- NCI
National Cancer Institute
- UPMC-ML
University of Pittsburgh Medical Center Cancer Center
Footnotes
FINANCIAL DISCLOSURE: Dr Bleyer is a consultant for Sigma-Tau Pharmaceuticals and is on its Speakers’ Bureau; and Drs Tai and Beaupin have indicated they have no financial relationships relevant to this article to disclose.
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
The findings and conclusions in this article are those of the author(s) and do not necessarily represent the official position of U.S. Department of Health and Human Services, the Public Health Service, or the Centers for Disease Control and Prevention.
REFERENCES
- 1.Smith MA, Seibel NL, Altekruse SF, et al. Outcomes for children and adolescents with cancer: challenges for the twenty-first century. J Clin Oncol. 2010;28(15):2625–2634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stiller CA, Kroll ME, Pritchard-Jones K. Population survival from childhood cancer in Britain during 1978–2005 by eras of entry to clinical trials. Ann Oncol. 2012;23(9): 2464–2469 [DOI] [PubMed] [Google Scholar]
- 3.Bleyer WA. The U.S. pediatric cancer clinical trials programmes: international implications and the way forward. Eur J Cancer.1997;33(9):1439–1447 [DOI] [PubMed] [Google Scholar]
- 4.Grovas A, Fremgen A, Rauck A, et al. The National Cancer Data Base report on patterns of childhood cancers in the United States. Cancer 1997;80(12):2321–2332 [DOI] [PubMed] [Google Scholar]
- 5.Burke ME, Albritton K, Marina N. Challenges in the recruitment of adolescents and young adults to cancer clinical trials. Cancer 2007;110(11):2385–2393 [DOI] [PubMed] [Google Scholar]
- 6.Bleyer A, Budd T, Montello M. Adolescents and young adults with cancer: the scope of the problem and criticality of clinical trials. Cancer 2006;107(7 suppl): 1645–1655 [DOI] [PubMed] [Google Scholar]
- 7.Bleyer A Adolescent and young adult (AYA) oncology: the first A. Pediatr Hematol Oncol.2007;24(5):325–336 [DOI] [PubMed] [Google Scholar]
- 8.Parsons HM, Harlan LC, Seibel NL, Stevens JL, Keegan TH. Clinical trial participation and time to treatment among adolescents and young adults with cancer: does age at diagnosis or insurance make a difference? J Clin Oncol. 2011;29(30):4045–4053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Krailo MD, Bernstein L, Sullivan-Halley J, Hammond GD. Patterns of enrollment on cooperative group studies: an analysis of trends from the Los Angeles County Cancer Surveillance Program. Cancer. 1993;71(10 suppl): 3325–3330 [DOI] [PubMed] [Google Scholar]
- 10.Shaw PH, Ritchey AK. Different rates of clinical trial enrollment between adolescents and young adults aged 15 to 22 years old and children under 15 years old with cancer at a children’s hospital. J Pediatr Hematol Oncol. 2007;29(12):811–814 [DOI] [PubMed] [Google Scholar]
- 11.Bleyer WA. Cancer in older adolescents and young adults: epidemiology, diagnosis, treatment, survival, and importance of clinical trials. Med Pediatr Oncol. 2002;38(1):1–10 [DOI] [PubMed] [Google Scholar]
- 12.Bleyer A, O’Leary M, Barr R, Ries LAG, eds. Cancer Epidemiology in Older Adolescents and Young Adults 15 to 29 Years of Age: 1975–2000. Bethesda, MD: National Cancer Institute; 2006. NIH Publication 06–5767 [Google Scholar]
- 13.Bleyer A, Viny A, Barr R. Cancer in 15- to 29-year-olds by primary site. Oncologist. 2006;11(6):590–601 [DOI] [PubMed] [Google Scholar]
- 14.Albritton K, Bleyer WA. The management of cancer in the older adolescent. Eur J Cancer. 2003;39(18):2584–2599 [DOI] [PubMed] [Google Scholar]
- 15.Albritton K, Wiggins CL. Adolescents with cancer are not referred to Utah’s pediatric center [abstract 990]. Proc Am Soc Clin Oncol. 2006 [Google Scholar]
- 16.Albritton KH, Wiggins CH, Nelson HE, Weeks JC. Site of oncologic specialty care for older adolescents in Utah. J Clin Oncol. 2007;25(29):4616–4621 [DOI] [PubMed] [Google Scholar]
- 17.Howell DL, Ward KC, Austin HD, Young JL, Woods WG. Access to pediatric cancer care by age, race, and diagnosis, and outcomes of cancer treatment in pediatric and adolescent patients in the state of Georgia. J Clin Oncol. 2007;25(29):4610–4615 [DOI] [PubMed] [Google Scholar]
- 18.Rauck AM, Fremgen AM, Menck HR. Adolescent cancers in the United States: a National Cancer Data Base (NCDB) report. J Pediatr Hematol Oncol. 1999;21(4):310 [Google Scholar]
- 19.Caroline Pryce Walker Conquer Childhood Act of 2008 Congressional Record, 154, 110–706 [Google Scholar]
- 20.Indelicato DJ, Bleyer A. Clinical Trial Availability Compared to Incidence Rates for Adolescent and Young Adult Cancer Patients. Chicago, IL: American Society of Clinical Oncology; 2011 [Google Scholar]
- 21.Shaw P, Boyiadzis M, Tawbi H, et al. Improved clinical trial enrollment in adolescent and young adult (AYA) oncology patients after the establishment of an AYA oncology program uniting pediatric and medical oncology divisions. Cancer. 2012;118(14):3614–3617 [DOI] [PubMed] [Google Scholar]
- 22.Shaw PH, Boyiadzis M, Tawbi H, et al. Improved clinical trial enrollment in adolescent and young adult (AYA) oncology patients after the establishment of an AYA oncology program uniting pediatric and medical oncology divisions. Cancer. 2012;118(14):3614–3617 [DOI] [PubMed] [Google Scholar]
- 23.Carlson LE, Angen M, Cullum J, et al. High levels of untreated distress and fatigue in cancer patients. Br J Cancer. 2004;90(12):2297–2304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Clerici CA, Massimino M, Casanova M, et al. Psychological referral and consultation for adolescents and young adults with cancer treated at pediatric oncology unit. Pediatr Blood Cancer. 2008;51(1):105–109 [DOI] [PubMed] [Google Scholar]
- 25.Kazak AE, Derosa BW, Schwartz LA, et al. Psychological outcomes and health beliefs in adolescent and young adult survivors of childhood cancer and controls. J Clin Oncol. 2010;28(12):2002–2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stam H, Grootenhuis MA, Caron HN, Last BF. Quality of life and current coping in young adult survivors of childhood cancer: positive expectations about the further course of the disease were correlated with better quality of life. Psychooncology. 2006;15(1):31–43 [DOI] [PubMed] [Google Scholar]
- 27.Harlan LC, Lynch CF, Keegan TH, et al. ; AYA HOPE Study Collaborative Group. Recruitment and follow-up of adolescent and young adult cancer survivors: the AYA HOPE Study. J Cancer Surviv. 2011;5(3):305–314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.National Comprehensive Cancer Network. NCCN Guidelines. Available at: www.nccn.org/professionals/physician_gls/f_guide-lines.asp. Accessed April 9, 2014


