Abstract
Background
There are numerous reports on cage subsidence after ACDF; however, few studies have identified its risk factors. The current study aimed to identify risk factors for cage subsidence after ACDF using the PEEK cage packed with local autobone implant with plate and provides evidence for surgical decision-making.
Material/Methods
We retrospectively reviewed 77 patients with OPLL who underwent 1/2-level ACDF using the PEEK cage packed with local autobone implant with plate from March 2013 to December 2015. Implant subsidence was defined as the decrease in interbody height at the final follow-up compared to that measured on the first postoperative day ≥2 mm. Intervertebral fusion was evaluated on the basis of no motion across the fusion site and the presence of trabeculae between bone and implant in the X-rays. Multivariate logistic regression analysis was used to identify the risk factors for cage subsidence.
Results
In comparing the end-plate removal group with the end-plate preservation group, we found that the fusion rate (removal group, 35.90%; preservation group, 10.50%) and the change of IH (P=0.011) were significantly different during the first 6 weeks after surgery. Advanced age (OR=1.34, 95% CI=1.04–1.24, P=0.004), end-plate removal (OR=11.84, 95% CI=2.91–48.28, P=0.001), and nonunion within 6 weeks after surgery (OR=22.67, 95% CI=2.36–217.67, P=0.007) played an important role in predicting cage subsidence.
Conclusions
These findings suggest that advanced age, end-plate removal, and nonunion within 6 weeks after surgery are risk factors for the cage subsidence after ACDF using the PEEK cage packed with local autobone implant with plate in patients with OPLL.
MeSH Keywords: Ossification of Posterior Longitudinal Ligament, Risk Factors, Spine
Background
Cervical spondylosis is a chronic degenerative process of the cervical spine, which is generally caused by the disc herniation, bone spur formation, and ossified ligament [1]. Previous studies showed that cervical spondylosis was closely related to age [1–3]. However, based on clinical imaging data, we found the prevalence of cervical spondylosis tended to be higher in younger patients. Cervical ossification of posterior longitudinal ligament (OPLL) is recognized as an important cause of cervical spondylosis [4]. When conservative treatment fails, surgery is considered. The approaches include anterior, posterior, and posterior-anterior surgery. Anterior cervical discectomy and fusion (ACDF) procedure is theoretically feasible to use in treating cervical massive OPLL [4,5]. Cage subsidence is a postoperative complication after ACDF surgery. Previous studies reported that the incidence of cage subsidence varied significantly [6,7]. The decrease of the foraminal volume, cervical spine instability, and loss of segmental lordosis resulting from cage subsidence can lead to adjacent segment degeneration, which is a concern [8–10]. Nevertheless, few studies have identified the risk factors for cage subsidence, and such factors could influence surgical programs. The mission of this study was to identify the risk factors of cage subsidence in patients with OPLL after ACDF procedure and to provide evidence for surgical decision-making.
Material and Methods
This study was approved by the Institutional Ethics Board of the 3rd Hospital of Hebei Medical University and the methods were carried out in accordance with approved guidelines. Since this was a retrospective study, informed consent was not required.
A total of 77 patients with single-level or 2-level cervical OPLL who underwent ACDF surgery were enrolled in this study from March 2013 to December 2015 at the Department of Spine Surgery. The inclusion criteria were: 1) diagnosis of cervical spondylosis myelopathy caused by OPLL (Figure 1); 2) high-signal intensity of the spinal cord on T2-weighted magnetic resonance imaging (MRI); 3) the lesion does not exceed 2 segments; 4) the OPLL can be removed directly by the anterior approach; and 5) ≥24-month follow-up period. The exclusion criteria were: 1) spinal tumors or infectious spondylitis; 2) patients who have had cervical surgery; and 3) incomplete imaging data. The enrolled patients included 38 men and 39 women and the average age at surgery was 58.1 years. The mean follow-up period was 33.4 months (range, 24 to 57 months). All patients in our department were recommended to be reviewed at 6 weeks and 6 months after surgery and then annually at the outpatient clinic. Patients received plain radiographs to assess the fusion condition on the first postoperative day and at each follow-up visit. The degree of postoperative symptom recovery was assessed by comparison of preoperative and postoperative Japanese Orthopedic Association score (JOA) and the Neck Disability Index score (NDI)
Figure 1.
A 54-year-old female patient complained of numbness of both hands and difficulty walking for 2 years. Plain radiological examination (A) and preoperative CT image showed a hill-shaped OPLL from C4 to C5 ≥50% (B, C). MRI demonstrated spinal cord compression at C4/5 (D).
Radiological evaluation
We collected histories from all patients. Physical examination, plain radiographs in anterior-posterior and lateral views, computed tomography (CT), and MRI were conventionally performed. The decrease of the interbody height at the final follow-up compared to that measured on the first postoperative day ≥2 mm was defined as cage subsidence [11]. Interbody height (IH) was measured by lateral radiograph as the distance between the middle points of the superior end-plate of the upper vertebral body and the inferior end-plate of the lower vertebral body (Figure 2A). Intervertebral fusion was evaluated on the basis of no motion across the fusion site on the flexion-extension lateral radiographs and the presence of trabeculae between the bone and the implant in the X-rays. The cervical sagittal curvature was defined as the angle between the upper end-plate of C2 and the lower end-plate of C7. Cobb angle was measured between the upper and lower end-plate that were most inclined on standing lateral X-rays.
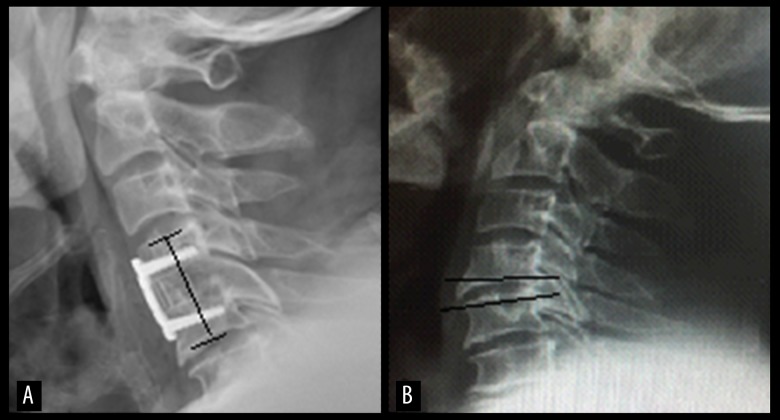
Figure 2.
The IH was measured by lateral radiograph as the distance between the middle points of the superior end-plate of the upper vertebral body and the inferior end-plate of the lower vertebral body (A); A total of 2–3 mm was removed, including cartilage and cortical bone (B).
Surgical technique
The ACDF procedure involved a right transverse incision. An optimal cage was prepared after removal of the end-plate (including cartilage and cortical bone), degenerative intervertebral disc, and the ossified posterior longitudinal ligament. During the operation, the endplates were removed with a curette or burr to enlarge the space of operation and to obtain adequate decompression (Figure 2B). For original stabilization, a laboratory cage was used to select the appropriate cage size. The polyetheretherketone (PEEK) cage packed with local autobone was implanted into the intervertebral space. The anterior margin of the cage was consistent with the anterior edge of the vertebra. Then, a titanium plate was fixed to the vertebral body with proper screws. All patients were recommended to stay in bed for 1 day and to wear a cervical collar for 3 weeks after surgery.
Statistical analysis
SPSS software (version 21.0; SPSS Inc., Chicago, IL, USA) was used for statistical analysis. Quantitative date among the different groups were assessed by the t test or the Mann–Whitney U test, as appropriate. When statistically significant differences occurred, we performed multiple comparisons. Factors with P-value <0.05 in univariate analysis were selected into the multivariate logistic model. Multivariate logistic regression analysis was performed to identify the risk factors for early cage subsidence. Adjusted 95% confidence intervals (CIs), odds ratios (ORs), and P-values are presented with their respective predictors. P-values <0.05 were considered statistically significant.
Results
At T1, statistically significant differences could be discovered. The fusion rate of end-plate preservation group and end-plate removal group was 4 patients (10.5%) and 14 patients (35.9%), respectively; the fusion rate in the single-segment group and in the 2-segment group was 13 patients (28.90%) and 5 patients (15.6%), respectively. At T2, the result showed that the difference of fusion rate was narrowing. Fusion rate was 100% in every group at the final follow-up. This dynamic change indicated that cage subsidence occurred in the course of intervertebral fusion (Table 1). The cage subsidence was statistically significant from T0 to the T1 (P=0.011) in the end-plate preservation group (1.35±0.58) and in the end-plate removal group (2.32±1.48). Cage subsidence in the fusion group and nonunion group at 6 weeks after surgery was 1.36±0.85 and 1.99±1.29, respectively, which was statistically significant (P<0.05). However, there was no significant difference from T1 to T3(P>0.05) in the change of cage subsidence (Table 2).
Table 1.
Fusion rate at different time points after surgery.
| T1 | T2 | T3 | ||||
|---|---|---|---|---|---|---|
| Number | Percentage | Number | Percentage | Number | Percentage | |
| End-plate | ||||||
| Preservation | 4 | 10.50% | 33 | 86.80% | 38 | 100% |
| Removal | 14 | 35.90% | 38 | 97.40% | 39 | 100% |
| Segment | ||||||
| Single | 13 | 28.90% | 43 | 95.60% | 45 | 100% |
| Two | 5 | 15.60% | 28 | 87.50% | 32 | 100% |
| Total | 18 | 23.40% | 71 | 92.20% | 77 | 100% |
T1 stands for 6 weeks after surgery; T2 stands for 6 months after surgery; T3 stands for final follow-up.
Table 2.
The effect of end-plate and early fusion on the change of IH.
| From T0 to T1 | From T1 to T3 | |
|---|---|---|
| End-plate | ||
| Preservation | 1.35±0.58 | 0.49±0.56 |
| Removal | 2.32±1.48 | 0.6±0.71 |
| P-value | 0.011 | 0.529 |
| Fusion | ||
| Yes | 1.36±0.85 | 0.42±0.3 |
| No | 1.99±1.29 | 0.59±0.71 |
| P-value | 0.046 | 0.246 |
T0 stands for the first postoperative day; T1 stands for 6 weeks after surgery; T3 stands for final follow-up. IH – interbody height.
Compared the group of cage subsidence <2 mm with the group of cage subsidence ≥2 mm, there were statistically significant differences, which included higher average age (P=0.002) and end-plate removal (P=0.01) and nonunion at the first 6 weeks after surgery (P=0.03) (Table 3). In multivariate logistic regression analysis, age (OR=1.34, 95% CI=1.04–1.24, P=0.004), end-plate removal (OR=11.84, 95% CI=2.91–48.28, P=0.001), and nonunion within 6 weeks after surgery (OR=22.67, 95% CI=2.36–217.67, P=0.007) were independently associated with implant subsidence (Table 4).
Table 3.
Comparison of patient characteristics between the subsidence <2 mm group and ≥2 mm group.
| Variable | Subsidence <2 mm (n=54) | Subsidence ≥2 mm (n=23) | P-value |
|---|---|---|---|
| Age at surgery (years) | 56.1±7.5 | 62.8±7.6 | 0.002 |
| Sex | 0.502 | ||
| Male | 28 | 10 | |
| Female | 26 | 13 | |
| BMI (kg m−2) | 25.3±3.1 | 24.6±4.3 | 0.409 |
| Hemorrhage during operation (ml) | 263±149.3 | 302.2±179.3 | 0.323 |
| Fusion rate at 6 weeks after surgery | 17 (31.5%) | 1 (4.3%) | 0.03 |
| Preoperative C2–C7 Cobb | 12.38±9.2 | 11.84±10.0 | 0.815 |
| Postoperative C2–C7 Cobb | 12.31±6.44 | 14.52±7.2 | 0.189 |
| End-plate | 0.01 | ||
| Preservation | 32 | 6 | |
| Removal | 22 | 17 | |
| Segment | 0.778 | ||
| Single | 31 | 14 | |
| Two | 23 | 9 | |
| Duration of symptoms (months) | 10.9±3.7 | 10.7±5.1 | 0.85 |
| Smoking | 0.103 | ||
| Yes | 25 | 6 | |
| No | 29 | 17 |
BMI – body mass index.
Table 4.
Risk factors for the cage subsidence: multiple logistic regression analysis.
| Variable | Odds radio | 95% confidence interval | P-value |
|---|---|---|---|
| Age at surgery(years) | 1.34 | 1.04–1.24 | 0.004 |
| End-plate removal | 11.84 | 2.91–48.28 | 0.001 |
| Nonunion within 6 weeks after surgery | 22.67 | 2.36–217.67 | 0.007 |
The final follow-up JOA scores and NDI scores of each group were higher than the corresponding scores preoperatively (P<0.001). This demonstrated that the postoperative symptoms of patients were significantly improved. However, the JOA scores and the NDI scores were not significantly different between the end-plate preservation group and end-plate removal group at the final follow-up (P>0.05), and the same results were found for single or double segments as well (Table 5).
Table 5.
Evaluation of the end-plate and segment for outcome by JOA and NDI.
| JOA score | NDI score | |||
|---|---|---|---|---|
| Preoperative | Final follow-up | Preoperative | Final follow-up | |
| End-plate | ||||
| Preservation | 8.47±1.61 | 14.21±1.68* | 24.95±5.18 | 7.18±3.38* |
| Removal | 9.12±1.74 | 14.05±1.32* | 24.67±5.29 | 6.3±2.36* |
| P-value | 0.093 | 0.326 | 0.87 | 0.265 |
| Segment | ||||
| Single | 8.79±1.80 | 14.14±1.47* | 25.69±5.43 | 6.98±2.89* |
| Two | 8.81±1.56 | 14.11±1.55* | 23.57±4.68 | 6.41±2.98* |
| P-value | 0.950 | 0.992 | 0.141 | 0.287 |
Contrastive study between preoperative and final follow-up P<0.001
Discussion
Traditionally, surgical intervention is recommended when patients are diagnosed with OPLL showing high sign on T2-weighted magnetic resonance imaging (MRI) at the narrowest level of the spinal cord. However, the optimal approach for cervical myelopathy caused by OPLL is controversial. The posterior approach can generate an indirect decompression resulting from the posterior float of the spinal cord, which is safer than the anterior approach, but it restricts the recovery of damaged nerves to a certain extent [12–14]. The risk of postoperative disease progression, failure to correct cervical kyphosis, and poor consequences in K-line negative patients are the disadvantages of posterior surgery [15].
The ACDF can remove an ossified ligament that compresses spinal cord directly to obtain better outcomes for patients with hill-shaped ossification or occupying ratio ≥60% [16]. In spite of increased technical difficulty and higher complication rates, anterior surgery is related to good outcomes when OPLL occupies >50% to 60% of the canal [17]. The decision to use either the anterior or posterior approach mainly depends on the number of levels (1–2 levels, anterior; more than 2 levels, posterior) in our department. In this study, we selected patients who underwent anterior surgery due to localized OPLL, which consisted of a single lesion referring to 1 vertebral level or interspace.
Some studies have shown that the occurrence of cage subsidence was associated with various factors, including the size and contact surface ratio of cage and bone density [18,19]. However, Suh et al. [20] reported that substrate density and footprint area contribute to cage subsidence. In addition, Marino [21] found that the thickness of the resected end-plate also had a significant impact on cage subsidence after posterior lumbar interbody fusion. Hakało et al. [22] reported that there are 2 stages in the process of subsidence: an original stage and a final one. The rapid increase of subsidence took place in the original stage. The last stage of the subsidence is relatively long and ends in a clinical environment when interbody bone fusion is performed and new bone is formed [23]. Similarly, our results showed that the duration of cage subsidence could be short, which is attributable to the intervertebral fusion. Nevertheless, the association between cage subsidence and clinical outcome is controversial. Recent studies found that there were no statistically significant differences between cage subsidence and clinical outcome. The hardware failure may be attributable to excessive subsidence [24]. Young et al. [25] reported that there were no statistically significant differences between cage subsidence and clinical outcome. Similarly, our study indicated that removal of the end-plate and the number of involved segments did not significantly affect postoperative recovery according to the JOA scores and the NDI scores, which indirectly supports this view as well.
The effect of the end-plate on interbody fusion is unclear. Park et al. [26] reported that destruction of the cartilage end-plate is an important factor increasing subsidence after ACDF with a stand-alone cage. In our study, compared with the end-plate preservation group, patients with end-plate removal had higher fusion rates (35.90%) but also had higher occurrence of cage subsidence (2.32±1.48) in the first 6 weeks after surgery. However, this difference narrowed significantly at the final follow-up. Therefore, the close association between cage subsidence and end-plate removal only found in the early postoperative period. From our perspective, end-plate removal accelerated cage subsidence and early postoperative fusion hinders cage subsidence. Patient sex, BMI, duration of symptoms, hemorrhage during operation, number of involved segments, postoperative Cobb angle, and smoking status were not identified as predictors in this study.
In the present multivariate logistic regression analysis, nonunion within 6 weeks after surgery and advanced age was risk factors of cage subsidence, in addition to end-plate removal. However, Yang et al. [27] found that differences in the incidence of cage subsidence were not statistically significant between the nonunion and union groups. Our results showed that nonunion within 6 weeks after surgery is an important predictor of cage subsidence, but nonunion from 6 weeks after surgery to the last follow-up did not greatly affect cage subsidence. The different results were due to Yang’s focus on the distinction between immediate postoperative and final follow-up. In fact, his results are consistent with ours. Jeong et al. [26] found that subsidence is a risk factor of nonunion. We believe that nonunion within 6 weeks after surgery and cage subsidence are mutually causative and affect each other.
Although Jeong did not explicitly state that advanced age is a risk factor for subsidence, he stated that surgeons should evaluate bone mineral density in all patients before surgery to predict the risk of cage subsidence [26]. Multivariate logistic analysis demonstrated that advanced age was a risk factor in our study. This may be because the normal physiological curvature of the cervical spine of the elderly has changed, which led to long-term abnormal stress and caused cage subsidence. In addition, osteoporosis associated with the normal ageing process and increased risk of underlying poor nutrition also have negative influences on cage subsidence. Hence, surgeons should counsel the elderly to have good nutrition and to treat minimize osteoporosis after surgery to prevent cage subsidence.
There were a series of limitations that needed to be considered regarding our study. Firstly, it was a single-center study and the number of cervical spondylosis with OPLL was limited, so the findings cannot be generalized beyond the studied cases. Secondly, we achieved a minimum follow-up of 24 months, which is a distinct drawback of this study; the present findings cannot be interpreted as long-term results. Finally, fusion rates might be overestimated because our study evaluated fusion by simple X-ray. Due to these limitations, our findings require further validation in studies with larger patient samples and longer follow-up.
Conclusions
In a relatively small sample of patients with OPLL, risk factors for cage subsidence after ACDF using the PEEK cage packed with local autobone implant with plate were advanced age, end-plate removal, and nonunion within 6 weeks after surgery. Because cage subsidence can trigger complications, even the failure of hardware, a better understanding of the significance of risk factors can help surgeons develop more effective and appropriate surgical schemes.
Footnotes
Source of support: Departmental sources
References
- 1.Wang C, Tian F, Zhou Y, et al. The incidence of cervical spondylosis decreases with aging in the elderly and increases with aging in the young and adult population: A hospital-based clinical analysis. Clin Interv Aging. 2016;11:47–53. doi: 10.2147/CIA.S93118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nagashima H, Dokai T, Hashiguchi H. Clinical features and surgical outcomes of cervical spondylotic myelopathy in patients aged 80 years or older: A multi-center retrospective study. Eur Spine J. 2011;20(Suppl 2):240–46. doi: 10.1007/s00586-010-1672-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hayashi H, Okada K, Hamada M, et al. Etiologic factors of myelopathy. A radiographic evaluation of the aging changes in the cervical spine. Clin Orthop Relat Res. 1987;214:200–9. [PubMed] [Google Scholar]
- 4.Iwasaki M, Okuda S, Miyauchi A, Sakaura H. Surgical strategy for cervical myelopathy due to ossification of the posterior longitudinal ligament: Part 1: Clinical results and limitations of laminoplasty. Spine. 2007;32(Suppl 6):647–53. doi: 10.1097/01.brs.0000257560.91147.86. [DOI] [PubMed] [Google Scholar]
- 5.Wang X, Chen D, Yuan W, et al. Anterior surgery in selective patients with massive ossification of posterior longitudinal ligament of cervical spine: technical note. Eur Spine J. 2012;21(Suppl 2):314–21. doi: 10.1007/s00586-011-1996-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Barsa P, Suchomel P. Factors affecting sagittal malalignment due to cage subsidence in standalone cage assisted anterior cervical fusion. Eur Spine J. 2007;16(Suppl 9):1395–400. doi: 10.1007/s00586-006-0284-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hacker RJ, Cauthen JC, Gilbert TJ, Griffith SL. A prospective randomized multicenter clinical evaluation of an anterior cervical fusion cage. Spine. 2000;25:2646–54. doi: 10.1097/00007632-200010150-00017. [DOI] [PubMed] [Google Scholar]
- 8.Bartels RH, Donk R, van Azn RD. Height of cervical foramina afer anterior discectomy and implantation of a carbonfber cage. J Neurosurg. 2001;95(Suppl 1):40–42. doi: 10.3171/spi.2001.95.1.0040. [DOI] [PubMed] [Google Scholar]
- 9.Ha SK, Park JY, Kim SH, et al. Radiologic assessment of subsidence in stand-alone cervical polyetheretherketone (PEEK) cage. J Korean Neurosurg Soc. 2008;44(6):370–74. doi: 10.3340/jkns.2008.44.6.370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Katsuura A, Hukuda S, Saruhashi Y, Mori K. Kyphotic malalignment after anterior cervical fusion is one of the factors promoting the degenerative process in adjacent intervertebral levels. Eur Spine J. 2001;10(4):320–24. doi: 10.1007/s005860000243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Park JI, Cho DC, Kim KT, et al. Anterior cervical discectomy and fusion using a stand-alone polyetheretherketone cage packed with local autobone: Assessment of bone fusion and subsidence. J Korean Neurosurg Soc. 2013;54(3):189–93. doi: 10.3340/jkns.2013.54.3.189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Iwasaki M, Kawaguchi Y, Kimura T, Yonenobu K. Long-term results of expansive laminoplasty for ossification of the posterior longitudinal ligament of the cervical spine: More than 10 years follow up. J Neurosurg. 2002;96(Suppl 2):180–89. [PubMed] [Google Scholar]
- 13.Denaro V, Longo UG, Berton A, et al. Cervical spondylotic myelopathy: The relevance of the spinal cord back shift after posterior multilevel decompression. A systematic review. Eur Spine J. 2015;24(Suppl 7):832–41. doi: 10.1007/s00586-015-4299-x. [DOI] [PubMed] [Google Scholar]
- 14.Xia G, Tian R, Xu T, et al. Spinal posterior movement after posterior cervical decompression surgery: Clinical findings and factors affecting postoperative functional recovery. Orthopedics. 2011;34(Suppl 12):e911–18. doi: 10.3928/01477447-20111021-03. [DOI] [PubMed] [Google Scholar]
- 15.Fujiyoshi T, Yamazaki M, Kawabe J, et al. A new concept for making decisions regarding the surgical approach for cervical ossification of the posterior longitudinal ligament: The K-line. Spine (Phila Pa 1976) 2008;33(26):E990–93. doi: 10.1097/BRS.0b013e318188b300. [DOI] [PubMed] [Google Scholar]
- 16.Iwasaki M, Okuda S, Miyauchi A, Sakaura H. Surgical strategy for cervical myelopathy due to ossification of the posterior longitudinal ligament: Part 2: Advantages of anterior decompression and fusion over laminoplasty. Spine. 2007;32(Suppl 6):654–60. doi: 10.1097/01.brs.0000257566.91177.cb. [DOI] [PubMed] [Google Scholar]
- 17.An HS, Al-Shihabi L, Kurd M. Surgical treatment for ossification of the posterior longitudinal ligament in the cervical spine. J Am Acad Orthop Surg. 2014;22(7):420–29. doi: 10.5435/JAAOS-22-07-420. [DOI] [PubMed] [Google Scholar]
- 18.Liu W, Hu L, Wang J, et al. Comparison of zero-profile anchored spacer versus plate-cage construct in treatment of cervical spondylosis with regard to clinical outcomes and incidence of major complications: A meta-analysis. Ther Clin Risk Manag. 2015;11:1437–47. doi: 10.2147/TCRM.S92511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nemoto O, Kitada A, Naitou S, et al. Stand-alone anchored cage versus cage with plating for single-level anterior cervical discectomy and fusion: A prospective, randomized, controlled study with a 2-year follow-up. Eur J Orthop Surg Traumatol. 2015;25(Suppl 1):S127–34. doi: 10.1007/s00590-014-1547-4. [DOI] [PubMed] [Google Scholar]
- 20.Suh PB, Puttlitz C, Lewis C, et al. The effect of cervical interbody cage morphology, material composition, and substrate density on cage subsidence. J Am Acad Orthop Surg. 2017;25(Suppl 2):160–68. doi: 10.5435/JAAOS-D-16-00390. [DOI] [PubMed] [Google Scholar]
- 21.Marino JF. Subsidence of metal interbody cage after posterior lumbar interbody fusion with pedicle screw fixation. Orthopedics. 2010;33(Suppl 4):226–27. doi: 10.3928/01477447-20100225-32. [DOI] [PubMed] [Google Scholar]
- 22.Hakało J, Pezowicz C, Wronski J, et al. The process of subsidence after cervical stabilizations by cage alone, cage with plate and plate-cage. A biomechanical comparative study. Neurol Neurochir Pol. 2007;41(5):411–16. [PubMed] [Google Scholar]
- 23.Hakało J, Ciupik L, Łabedzka A, et al. Biomechanical characteristic of bone fusion in presence of stabilizer. Acta Bioengineering Biomechanics. 2001;3(Suppl 1):97–103. [Google Scholar]
- 24.Lee CH, Kim KJ, Hyun SJ, et al. Subsidence as of 12 months after single-level anterior cervical inter-body fusion. Is it related to clinical outcomes? Acta Neurochir (Wien) 2015;157(6):1063–68. doi: 10.1007/s00701-015-2388-6. [DOI] [PubMed] [Google Scholar]
- 25.Joung YI, Oh SH, Ko Y, et al. Subsidence of cylindrical cage (AMSLU™Cage): Postoperative 1 year follow-up of the cervical anterior interbody fusion. J Korean Neurosurg Soc. 2007;42(5):367–70. doi: 10.3340/jkns.2007.42.5.367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Park JI, Cho DC, Kim KT, et al. Anterior cervical discectomy and fusion using a stand-alone polyetheretherketone cage packed with local autobone: Assessment of bone fusion and subsidence. J Korean Neurosurg Soc. 2013;54(3):189–93. doi: 10.3340/jkns.2013.54.3.189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yang JJ, Chang HY, Chang BS, et al. Subsidence and nonunion after anterior cervical interbody fusion using a stand-alone polyetheretherketone (PEEK) cage. Spine J. 2010;10(9):16–23. doi: 10.4055/cios.2011.3.1.16. [DOI] [PMC free article] [PubMed] [Google Scholar]