Abstract
Purpose
To describe a case of interface fluid formation caused by uncontrollable intraocular pressure (IOP) 16 years after laser-assisted in situ keratomileusis (LASIK) surgery secondary to Posner Schlossman Syndrome (PSS).
Observations
After trabeculectomy operation, IOP of the operative eye was back to normal, and the interface fluid refluxed over time.
Conclusions
and importance: Interface Fluid Syndrome can be a potential lifelong complication after LASIK surgery. PSS patients post-LASIK require early IOP control.
Keywords: Interface fluid syndrome, Posner-Schlossman syndrome, Laser-assisted in situ keratomileusis
1. Introduction
Interface fluid syndrome (IFS) is a rare complication following LASIK surgery characterized by fluid collection in the flap interface. It has been reported secondary to raised intraocular pressure (IOP), endothelial decompensation, and uveitis.1, 2, 3 It is commonly reported 1 week to months after LASIK surgery. To our knowledge there have been no publications on IFS due to increased IOP occurring 16 years after LASIK operation triggered by Posner-Schlossman Syndrome (PSS).
2. Case report
A 46-year-old male presented with eye pain and blurred vision in the right eye that he had been experiencing for 1 year. He had undergone successful LASIK operation in both eyes for a myopic refractive error 16 years earlier. The best-corrected visual acuity (BCVA) of the right eye was 20/20. He presented with eye pain and vision impairment in the right eye 6 years later and was diagnosed with PSS by unilateral, nongranulomatous, anterior uveitis accompanied by markedly elevated intraocular pressure. The IOP of the right eye at that time was 36 mmHg by Non-contact Tonometer (NCT), and was treated with steroids and topical β-blocker eye drops. It had been well controlled within 15 days. From then on, PSS recurred almost twice per year, and was successfully treated by the same strategy each time. The bouts of PSS lengthened to nearly 3 months in the past three years. A combination of three types of anti-glaucoma eye drops were used (topical timolol maleate 0.5% twice daily, brimonidine 0.15% thrice daily, travoprost 0.004% once at bedtime) to control the IOP, in addition to steroids to treat the PSS. During these outbreaks, IFS was never found by slit-lamp examination or anterior segment OCT. The PSS ultimately reacted positively to the treatments every time. While, he presented with vision decline one year ago with a diagnosis of PSS, the IOP of the right eye was 20 mmHg. The IOPs of the right eye were from 22 to 45 mmHg during the past year, and edema of the cornea began. OCT examination only showed a thickening of the cornea (Fig. 1). However, the visual acuity of right eye dropped drastically to 4/200 on December 27, 2016. IFS was suspected and confirmed using high-resolution OCT. Edema of the entire cornea was observed, and every layer was involved (Fig. 2A). The clear space here was showed by OCT (Fig. 3A). In consideration of the uncontrollable IOP and formation of the IFS, a trabeculectomy was performed on December 30, 2016.
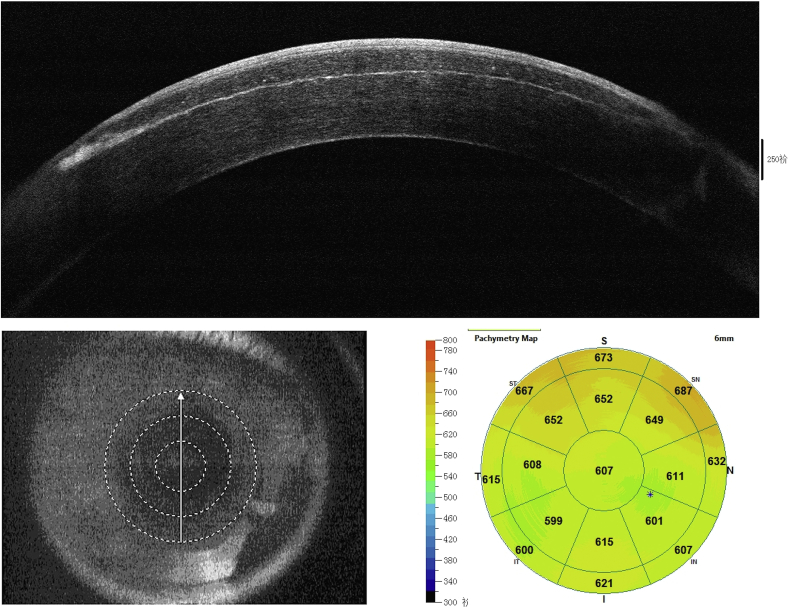
Fig. 1.
Anterior segment OCT shows no separation of the interface. The whole cornea is thickened as detected by Pachymetry Map of the cornea. (The Scanning direction of representative images of OCT in this case report are all from bottom to top; scale bar = 250 μm.) (Check date: 2016-11-5).
Fig. 2.
Representative slit-lamp clinical photographs of different stages of this patient.
A. Slit view of the cornea before operation. A LASIK cornea with moderate (stage 2) IFS that has moderate edematous abnormalities along the interface wound causing a diffuse smudgy interface haze. The whole cornea has edema and epithelium bullae can be found out by careful examination. The pupil size is larger than normal. (Check Date: 2016-12-
26)
B. Cornea still has edema, several tiny folds are observed on the corneal flap interface in the right eye 9 days postoperative. (Check Date: 2017-1-9)
C. Cornea is transparent. The tiny folds, which could be observed previously, have disappeared. The pupil size is back to normal one month postoperative. (Check Date: 2017-2-6).
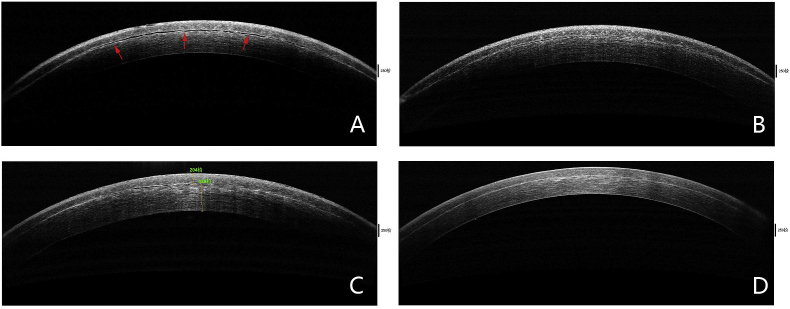
Fig. 3.
Representative high-resolution optical coherence tomography (OCT) images of different stages of this patient.
A. OCT shows focal small fluid space (red arrows) accompanied with cornea edema with each layer involved. (Check Date: 2016-12-26).
B. Interface fluid refluxed, only occasional focal small fluid pockets exist (red arrows) 3 days postoperative. (Check Data: 2017-1-3)
C. OCT scan of the cornea with resolved interface fluid. The flap clings to the stromal bed. However, the cornea still has edema. The flap thickness is 204 μm, and the residual bed is 488 μm. (Check Date: 2017-1-9)
D. Cornea flap is flush to the stromal bed. Interface fluid is totally bumped out. Cornea is transparent again. (Check Date: 2017-2-6). (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
This patient underwent successful trabeculectomy surgery on December 30, 2016. The first day postoperatively, the vision acuity was 20/80 and the IOP of the right eye was 9 mmHg. The cornea flap edema could be observed during the first ten days postoperatively, and gradually diminished from the periphery to center over one week. OCT showed the space between the flap and residual stromal bed shrank over time (Fig. 3B–D). Several tiny folds were observed on the corneal flap interface in the right eye postoperatively, which diminished over two months (Fig. 2C). The IOPs were 8.7 mmHg in the right eye and 14 mmHg in the left eye (as measured by NCT) one month postoperatively. At the time of the most recent measurement, the BCVA of the right eye was 20/25 by pinhole. The endothelial counting was 1600 cells/mm2 in the right eye and 2700 cells/mm2 in the left eye. There were no significant differences in IOP between postoperative months 1 and 3.
3. Discussion
LASIK surgery for myopia is a common refractive surgical procedure. The LASIK flap is known to be an incomplete healing, retaining only 2%–28% of the original tensile strength for more than a decade after surgery.4 Therefore, the potential space between the flap and stroma is constant. It is also the physiological basis of IFS in this case. There are reports about IFS in other types of surgery which have potential space, such as small incision lenticule extraction (SMILE)5 and lamellar keratoplasty.6
Posner-Schlossman Syndrome (PSS), or glaucomatocyclitic crisis, is a unilateral ocular condition characterized by recurrent attacks of non-granulomatous anterior uveitis and raised intraocular pressure that can result in chronic secondary glaucoma. Males of middle age are prone to be affected. Topical steroids combined with topical anti-glaucoma therapies are recommend as a first line treatment in PSS.7 If IOP cannot be controlled medically, surgical treatment should be used.8 In this case, continuously high IOP caused by the incontrollable PSS is the mainly cause of IFS.
IFS is a flap-related complication of LASIK surgery. Clinically, the early stage of IFS is easy to mistake for the dispersed granular appearance of diffuse lamellar keratitis (DLK). The former usually occurs 1 week to months after LASIK surgery, whereas the latter always happens within the first week postoperatively.9 In moderate to severe cases, IFS appears as an optically empty space between the flap and the residual stromal bed. It can be detected with a careful slit-lamp examination and confirmed by high-resolution optical coherence tomography (OCT).10 Dawson et al.11 classified IFS into three stages according to the degree of fluid accumulation in the flap interface. Using this staging system, the right eye in the current case would be categorized as stage 2: moderate to severe swelling of the LASIK interface wound associated with moderate to severe diffuse, smudgy, nongranular interface haze and occasional focal small fluid pockets. The reasons of IFS are summarized as high intraocular pressure (IOP), endothelial cell dysfunction, and uveitis. In this case, the patient experienced all three factors. First, PSS occasionally broke out. Then high IOP attacked the endothelium layer, leading to decreased cell density of the endothelium each time. Uncontrolled PSS triggered constantly high IOP, and the rest of the endothelial cells could not undertake the burden of the IOP. Balance between the endothelial cells and the IOP was lost and humor began to accumulate in the potential space. Fortunately, the interface fluid was gradually absorbed after the anti-glaucoma operation, the space disappeared, and the flap became transparent again. It is interesting in this case that PSS attacked several times without IFS formation. Because of cave persistence, and partial flap detachments, IFS is a common long-term postoperative challenge. In these people in the post-LASIK period, a long-term follow-up after routine LASIK surgery is probably the easiest and most necessary step to prevent IFS.
4. Conclusions
PSS is a relatively rare disease that typically affects males of middle age and its onset cannot be predicted. The group of people who undergo LASIK operation is largely operated on before middle age. So, when PSS occurs post-LASIK, early IOP control is needed, for IFS may be a potential lifelong flap complication in such cases. Anterior OCT is a helpful tool in confirming the diagnosis and is useful for follow-ups to check for resolution of the fluid. Increasing flap adhesive strength while maintaining transparency is a clinical goal.
Acknowledgements and disclosures
Funding
No funding or grant support.
Conflicts of interest
The following authors have no financial disclosures: (Zhe Jia, Shaozhen Zhao, Ruihua Wei, Yue Huang, Chen Zhang, Ruibo Yang).
Authorship
All authors attest that they meet the current ICMJE criteria for Authorship.
Acknowledgements
None.
References
- 1.Shajari M., Rafiezadeh P., Pavlovic I. Management of interface fluid syndrome after LASIK by descemet membrane endothelial keratoplasty in a patient with Fuchs' corneal endothelial dystrophy. J Refract Surg. 2017;33(5):347–350. doi: 10.3928/1081597X-20170210-01. [DOI] [PubMed] [Google Scholar]
- 2.Goto S., Koh S., Toda R. Interface fluid syndrome after laser in situ keratomileusis following herpetic keratouveitis. J Cataract Refract Surg. 2013;39(8):1267–1270. doi: 10.1016/j.jcrs.2013.04.026. [DOI] [PubMed] [Google Scholar]
- 3.Bamashmus M.A., Saleh M.F. Post-LASIK interface fluid syndrome caused by steroid drops. Saudi J Ophthalmol. 2013;27(2):125–128. doi: 10.1016/j.sjopt.2013.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Morgan S.R., Dooley E.P., Kamma-Lorger C., Funderburgh J.L., Funderburgh M.L., Meek K.M. Early wound healing of laser in situ keratomileusis-like flaps after treatment with human corneal stromal stem cells. J Cataract Refract Surg. 2016;42(2):302–309. doi: 10.1016/j.jcrs.2015.09.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zheng K., Han T., Li M. Corneal densitometry changes in a patient with interface fluid syndrome after small incision lenticule extraction. BMC Ophthalmol. 2017;17(1):34. doi: 10.1186/s12886-017-0428-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ramappa M., Bhalekar S., Chaurasia S., Mulay K., Trivedi R.H., Wilson M.E. Presumed allograft stromal rejection after deep anterior lamellar keratoplasty in a boy presenting with interface fluid syndrome. J AAPOS. 2013;17(5):554–557. doi: 10.1016/j.jaapos.2013.06.011. [DOI] [PubMed] [Google Scholar]
- 7.Megaw R., Agarwal P.K. Posner-Schlossman syndrome. Surv Ophthalmol. 2017;62(3):277–285. doi: 10.1016/j.survophthal.2016.12.005. [DOI] [PubMed] [Google Scholar]
- 8.Dinakaran S., Kayarkar V. Trabeculectomy in the management of Posner-Schlossman syndrome. Ophthalmic Surg Laser. 2002;33:321–322. [PubMed] [Google Scholar]
- 9.Tello A., Galvis V., Mendoza B.F. LASIK interface complications: pressure-induced stromal keratitis (PISK), interface fluid syndrome (IFS) and post-LASIK edema-induced Keratopathy (PLEK) Int Ophthalmol Clin. 2016;56(3):185–187. doi: 10.1097/IIO.0000000000000129. [DOI] [PubMed] [Google Scholar]
- 10.Ramos J.L., Zhou S., Yo C. High-resolution imaging of complicated LASIK flap interface fluid syndrome. Ophthalmic Surg Laser Imag. 2008;39:S80–S82. doi: 10.3928/15428877-20080715-04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dawson D.G., Schmack I., Holley G.P., Waring G.O., 3rd, Grossniklaus H.E., Edelhauser H.F. Interface fluid syndrome in human eye bank corneas after LASIK: causes and pathogenesis. Ophthalmology. 2007;114(10):1848–1859. doi: 10.1016/j.ophtha.2007.01.029. [DOI] [PubMed] [Google Scholar]