Abstract
Aim:
The aim of this study is to assess stress and coping among caregivers of cancer patients on palliative care and to acquire a deeper understanding of their lived experiences.
Materials and Methods:
A mixed method study was conducted among caregivers of cancer patients on palliative care using mixed method approach and triangulation design. Data were gathered using self-administered stress rating scale, brief COPE inventory, and structured interview schedule. Nested sampling technique was adopted. The sample size for quantitative approach was eighty and qualitative approach was eight.
Results:
The results showed that 74% of the participants were females and 30% of them belong to the age group between 51 and 60 years. Fifty-four percent of them belong to Hindu religion and 40% were unemployed. Sixty-two percent of the patients were dependent on caregivers for all activities of daily living. Assessment of stress revealed that 82% of the participants had moderate stress and 18% had severe stress. Participants adopted both negative and positive coping. There was a significant negative correlation (r = −0.722, P = 0.001) between stress and coping. Similar findings were also observed in the phenomenological approach. The theme evolved was “caring companionship to palliative care.”
Conclusion:
Palliative caregiving is stressfull, challenging and can impact the caregiver's physical, emotional, psychological, and social well-being. Understanding lived experiences of caregivers of cancer patients on palliative care is important for the health professionals to improve the support, guidance, and education given to the caregivers of cancer patients on palliative care.
Keywords: Caregivers of cancer patients, coping, mixed method, palliative care, stress
INTRODUCTION
Cancer is one of the leading causes of death globally and was responsible for 8.8 million deaths in 2015. The number of new cases is expected to rise by about 70% over the next two decades.[1] In India, the number of new cancer cases in 2016 was around 14.5 lakhs and the figure is likely to reach 17.3 by 2020.[2] Patients diagnosed with cancer are said to be the most vulnerable group in the society. Cancer affects not only the patients but also his/her entire family. Treating the cancer patient is often an exercise of treating the part if not the whole family of the patient.[3] In addition to causing distress to the patient, it puts financial, personal, social, and health stress on family members. However, in the later stages of life, many people would prefer palliative care and opt to be at home surrounded by their family and friends with support and supervision from palliative care team.[4]
Palliative care is an approach that improves the quality of life of patients and their families facing the problem associated with life-threatening illness by means of early identification, assessment, and treatment of pain by providing physical, psychological, and spiritual care under supervision of palliative team.[5]
The philosophy behind palliative care is to assist patients and their families in achieving the best quality of life surrounded by their loved ones. Palliative caregiving is stressful, multidimensional, and 24-h responsibility, which may be shouldered alone.[6] It is challenging and can impact the caregivers’ physical, emotional, psychological, and economic aspects of life.[7]
Purpose of the study
The purpose of the study was to assess stress and coping among caregivers of cancer patients on palliative care and to acquire a deeper understanding of their lived experiences.
Objectives of the study
The primary objectives of the study were to:
Assess the level of stress among caregivers of cancer patients on palliative care as measured by stress rating scale
Identify the coping adopted by caregivers of cancer patients on palliative care as measured by brief COPE inventory
Explore and describe the lived experience of caregivers of cancer patients on palliative care using a qualitative approach.
The secondary objectives of the study were to:
Determine the relationship between stress and coping adopted by caregivers of cancer patients on palliative care
Elaborate in-depth experiences of caregivers, in relation to the severity of stress experienced during the palliative care.
MATERIALS AND METHODS
This is a mixed method study conducted in selected villages using triangulation design. Both descriptive survey approach and qualitative phenomenological approach were adopted to assess stress, coping, and lived experiences among caregivers of cancer patients on palliative care. The study was conducted between March 1, 2017, and April 30, 2017. Family caregivers of cancer patients on palliative care who had been providing palliative care at home for at least 3 months were included in the study. Paid caregivers and distant relatives were excluded from the study.
Nested sampling technique was adopted for the mixed method, i.e. for descriptive survey approach – to assess stress and coping among caregivers, purposive sampling technique was used. Data were collected from 80 participants. Informed consent was taken after giving participant information sheet and explaining the purpose of the study. Participants who were included in quantitative approach and those who were found to have severe stress on stress rating scale and able to communicate verbally were included in qualitative phenomenological approach using semistructured interview focusing on stress and coping. Data saturation was achieved in qualitative phenomenological approach upon interviewing eight participants. Thus, the sample size for qualitative approach became eight. The quantitative and qualitative data were collected simultaneously by having equal importance on both strands. Administrative permission, institutional ethics committee permission, and CTRI registration were obtained (CTRI/2017/04/008284).
Measures
Data were gathered using self-administered stress rating scale, brief COPE inventory, and structured interview technique. Stress rating scale was a 28-itemed five-point Likert scale with five domains such as physical, psychological, social, economic, and spiritual. The minimum score was 0 and maximum score was 112. The brief COPE inventory was a standardized tool developed by Carver, Scheier, and Weintraub (1997). It was a four-point Likert scale with 28 items. The minimum score was 28 and maximum score was 112. The measuring instruments were validated with nine subject experts in the field of palliative medicine, palliative psychosocial work, palliative care nursing, oncology nursing, psychiatric nursing, and community health nursing. Reliability of stress rating scale was established by administering it among 20 subjects. Reliability coefficient was computed using Cronbach's alpha and it was found reliable (r = 0.83). The reliability of the standardized English version of brief COPE inventory established by Carver (1997) was 0.88. Reliability of the Malayalam-translated brief COPE inventory was established by the researcher using Cronbach's alpha and was found to be 0.93.
Statistical methods
The experiences of eight caregivers of cancer patients on palliative care were gathered and analyzed. Validation of the data was done with participants and subject experts in the field of palliative medicine, medical surgical nursing, community health nursing, and qualitative research. Data collected were analyzed using SPSS version 16.0 for quantitative analysis (SPSS Inc., Chicago, IL, USA) and open code software 4.3 (OPC 4.3) for qualitative analysis (ITS and Epidemiology, University of Umea).
Both quantitative and qualitative data were merged in the area of stress, coping, and the lived experiences at the analytical phase of the continuum. Qualitative data were transcribed and translated to English and were analyzed using steps of Colaizzi's process for phenomenological approach. Extraction of subthemes and categories describing the phenomenon were derived.
RESULTS
Demographic characteristics
Data in Table 1 show that 24 (30%) participants belong to the age group between 51 and 60 years. Seventy-five (93.7%) of them were females. Hindus dominated as far as religion was concerned, i.e. 43 (53.7%). Seventy (87.5%) of them were married and living with spouse. Thirty-eight (47.5%) belonged to nuclear family. With reference to educational qualification, 18 (22.5%) of them were graduates and 4 (5.0%) of them had no formal education. Thirty-two (40.0%) were unemployed or homemakers. Thirty-five (43.7%) participants had monthly income less than Rupees 5000. Thirty-two (40.0%) of the participants were spouses. Major earning member was found to be the patient among 29 (36.2%) of them. Forty-one (51.2%) of them were providing palliative care for 1–3 years. Thirty-six (45.0%) of them received major support to provide palliative care from family and 30 (37.5%) received support from Karunya Fund of Kerala Social Security Mission (KSSM). Fifty (62.4%) patients were dependent for all activities of daily living. Sixty-seven (83.8%) patients were partially dependent and 13 (16.2%) were totally dependent on caregivers.
Table 1.
Frequency and percentage distribution of sample characteristics (n=80)

Description of stress among caregivers of cancer patients on palliative care
The data in Figure 1 show that 66 (82%) of the participants had moderate stress and 14 (18%) had severe stress whereas none had mild stress or no stress.
Figure 1.

The level of stress
Similar findings were also observed in the phenomenological approach. Subjects mentioned that the normal household duties inside and outside the home were shifted to the caregivers, particularly spouses; as a result, the caregivers became extremely busy and felt stress and strain in their daily lives. The subthemes evolved were “living with fear and uncertainty” and “stress and strain.” Participants quoted, “Really it is difficult to sleep…. Every time, some tension is in my mind…. Is he alright? Will he fall? Is he breathing normally? Will anything happen to him? Such tensions are always there….”
Stress among caregivers of cancer patients on palliative care
Data in Table 2 show that minimum score in the psychological domain is 9, maximum is 32, and mean ± standard deviation (SD) is 22.47 ± 5.59, whereas minimum scores in the social domain is 4, maximum is 12, and mean ± SD is 7.21 ± 2.32.
Table 2.
Description of the domain scores of stress among caregivers (n=80)

Similar findings were also observed in the phenomenological approach. The caregivers became extremely busy with responsibilities inside and outside home and felt stress and strain in their daily lives. They experienced physical and emotional strain while providing palliative care which was depicted in subthemes such as financial difficulty, physical and emotional strain, self-neglect, and lack of leisure time.
Participant C said, “A definite income of our family has ceased…. For our necessities, these days we have to depend on other people. My income is hardly sufficient to meet the household expenses. We had a housing loan and educational loan to repay. With both our income, we used manage fairly well. His sudden illness has brought financial crisis in our life.”
Participant E said, “Financially, we are in great trouble because the only income to our family was from agriculture. I am a typical housewife…. All financial aspects was taken care by him…. Our family has no other income…. My husband used to handle all matters with respect to our children, their studies, and all other things pertaining to the financial matters; all these things have been affected greatly…. For our necessities, these days we have to depend on other people.”
Participant F said, “I have pain in my legs and hands …I too have serious problem of backache and hypertension. But, when I see her suffering each moment, all my pain is forgotten.”
Participant E said, “When he is well, I feel alright. But, when he deteriorates or has the pain, I feel disturbed. The worst thing is to see him suffering with pain.”
Participant B said, “Because most of the time I am with my ill son, I do not have time to care for myself. It has been ages since I looked at the mirror. I do not care for myself before, such as putting henna to my hair, polishing my nails, or wearing new cloths. I spend most of my time with him, why should I care about my appearance! I do not care about myself as much as my son's well-being.”
Participant H said, “Last year, I had a fall and fractured my right hand.… I still have pain on that hand. But, when I see him suffering constantly, all my pain just vanishes.”
Participant C said, “For the last 2 years, there has been no leisure time in my life. I am working as a tailor in a readymade garment manufacturing firm. After finishing my routine here, I rush for work. When it happened everything changed, my life has changed; now, it is just with him, and that is all. I haven’t gone anywhere for 1 year leaving home only to visit the nearby temple and workplace.”
Participant F said, “Because most of the time I am with my ill daughter, I do not have time for other leisure activities. A person caring a palliative patient is always busy taking care of the ill person. It has been ages since I have gone out. I spend most of the time with her, How can a mother go out and enjoy leaving her daughter in agony?”
Coping among caregivers
Data presented in Figure 2 show the positive coping adopted by caregivers of cancer patients on palliative care. Data reveal that 66% of them used humor, 90% used religion, 68% utilized planning, and 83% used active coping.
Figure 2.

Positive coping adopted by caregivers of cancer patients on palliative care
Data presented in Figure 3 show the negative coping adopted by caregivers of cancer patients on palliative care. Data reveal that 56% of them used denial, 28% were involved in substance use, 52% used behavioral disengagement, and 66% utilized self-distraction.
Figure 3.
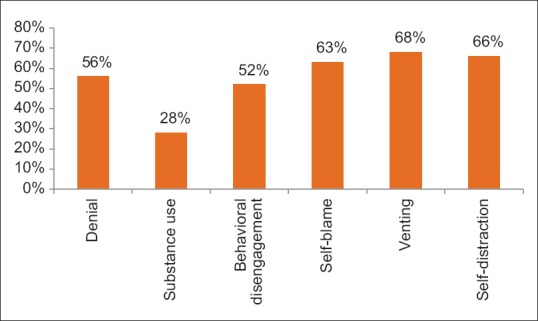
Negative coping adopted by caregivers of cancer patients on palliative care
Similar findings were also observed in the phenomenological approach. The main coping strategies used by caregivers had deep-rooted faith in God and prayers, support from family and friends, support from religious institutions, support from health and palliative team, support from KSSM, and inspiration and motivation from other palliative caregivers and palliative care patients. For many caregivers, their strong faith and belief in God helped them to cope with the distressing situation because they thought that their lives were anchored by God. The following narratives of participants help us to have a better understanding of coping.
Participant A said, “I have learned to overcome it with the help of prayers and blessings of God.”
Participant B said, “Now I have surrendered everything in God's hands. I accept that God has his own plans and everything has its own time. I am hoping that, Allah will take care of everything. I trust in God. It helps a lot to have faith in Allah. I just pray every day for strength to be able to do it. I am praying to Allah for strength and courage. I think it really helped because it gave me peace and inner strength.”
Participant C said, “I became stronger in mind, because I didn’t have another choice. I just grew a lot. I learned to pray a lot. I learned to put myself in God's hands especially when he was going through what he was going through. I am just praying to God to give us strength and guide us through these hurdles of life.
Participant D said, “I think I got help from the faith that I had in God as I knew that he is the only one who could help me. Let what God has planned for me take place…. When I feel really stressed, I pray. It is very helpful. It helps to reduce my worry. God is really protecting us. I firmly believe that it is because of my prayers that at least he is alive till now. I know that God will help me cross that bridge when the time comes…. Please keep us in your prayers.
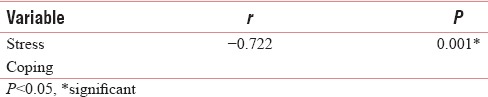
Relationship between the stress and coping adopted by caregivers of cancer patients on palliative care
Since the data were following the normality, Pearson's correlation was computed to assess the relationship between stress and coping.
The data presented in Table 3 show that there is a significant negative correlation (r = −0.722, P = 0.001) between stress and coping adopted by caregivers of cancer patients on palliative care. The study implies that as the stress increases, the coping decreases.
Table 3.
Correlation coefficient computed between stress and coping scores (n=80)
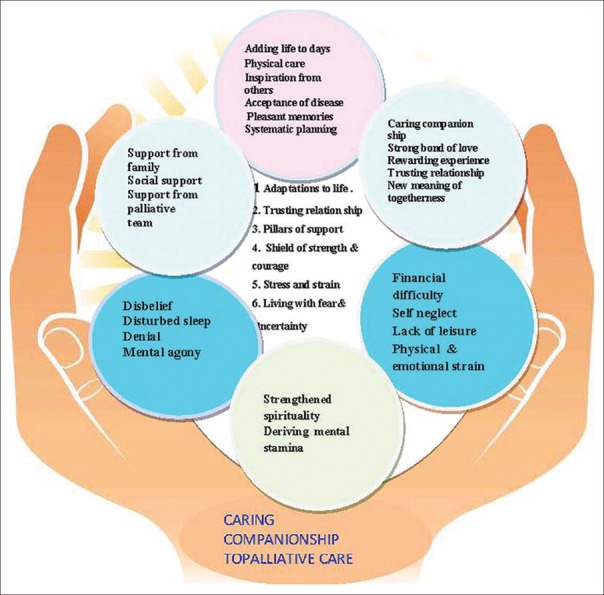
Derivation of qualitative subthemes and themes
The experiences of eight caregivers of cancer patients on palliative care were gathered and analyzed and evolved with six themes and 24 subthemes.
The emerged themes and subthemes are as follows:
-
Adaptation to life
- Adding life to days
- Inspiration from others
- Physical care
- Acceptance of disease
- Pleasant memories
- Systematic planning
-
Pillars of support
- Support from family
- Social support
- Support from health and palliative team
-
Trusting relation ship
- Caring companionship
- Strong bond of love
- Finding new meaning of togetherness
- Rewarding experience
- Trusting relationship with palliative team
-
Shield of strength and courage
- Strengthened spirituality
- Deriving mental stamina
-
Stress and strain
- Financial difficulty
- Physical and emotional strain
- Self-neglect
- Lack of leisure time
-
Living with fear and uncertainty
- Disbelief
- Disturbed sleep
- Denial
- Mental agony.
The phenomenon emerged out of the analysis of the experience was “caring companionship to palliative care.” The model developed to explain the phenomenon is depicted in Figure 4.
Figure 4.
Conceptual model of the phenomenon of lived experiences of caregivers of cancer patients on palliative care
Caregivers of cancer patients on palliative care experience various stressful moments along the pathway of his/her illness. It is a 24-h responsibility which may be shouldered with support from family members, friends, and palliative team. It is challenging and can impact the caregiver's physical, emotional, psychological, and social well-being. However, the caregivers are trying their level best to make the patient as comfortable as possible with the support of family, friends and palliative care team which is represented by supporting hands. These attributes represent themselves as the model for providing caring companionship to palliative care and to add life and cheer to the days of the cancer patient on palliative care.
DISCUSSION
Stress among caregivers of cancer patients on palliative care
The present study findings showed that 82% of the participants had moderate stress and 18% had severe stress whereas none had mild stress or no stress. Similar findings were also observed in the phenomenological approach.
This study findings also revealed that minimum score obtained in physical domain is 9 and maximum is 27 with a mean ± SD of 16.46 ± 3.47, minimum score in the psychological domain is 9 and maximum 32, mean ± SD 22.47 ± 5.59, minimum score in the social domain is 4 and maximum 12, mean ± SD 7.21 ± 2.32, minimum score in the spiritual domain is 9 and maximum 16, mean ± SD 12.81 ± 1.84, and minimum score in the economic domain is 4 and maximum 15, mean ± SD 9.25 ± 2.92.
The present study supports the study conducted among 75 caregivers of cancer patients in Haryana which revealed physical burden with a mean ± SD 9.23 ± 2.55, disruption of family activities with mean ± SD 7.85 ± 2.21, disruption of family leisure with mean ± SD 6.09 ± 2.05, disruption of family interaction with mean ± SD 2.59 ± 1.56, effect on physical health with mean ± SD 2.43 ± 1.41, and effect on mental health with mean ± SD 1.68 ± 0.85.[8]
The present study findings support the findings of the study conducted in Pune. It revealed that the disease has varied impact on the caregiver's health. A large number of caregivers (52%) reported feeling continually tired and exhausted. Lack of sleep was reported by a sizeable number of caregivers (46%). Inability to focus and mental confusion were reported by 46% of caregivers. The study revealed that overall stress level among caregivers is 5.18 ± 0.26 on a scale of 0–10.[9]
Coping among caregivers of cancer patients on palliative care
The present study findings showed that caregivers adopted negative as well as positive coping strategies. Fifty-six percent of them used denial, 28% were involved in substance use, 52% used behavioral disengagement, 63% utilized self-blame, 68% used venting, and 66% utilized self-distraction, whereas 66% of them used humor, 90% used religion, 85% used instrumental support, 68% utilized planning, 88% used emotional support, 80% was involved in positive reframing, 84% used acceptance, and 83% used active coping.
The present study supports the findings of the study conducted to assess family caregiver coping in end-of-life cancer care which revealed that most prominent ways of coping reported by participants were plan full problem-solving, seeking social support, self-controlling, escape avoidance, accepting responsibility, and positive reappraisal.[10]
The present study also supports the findings of a review of literature on stress and coping among breast cancer patients and family caregivers which revealed four predominant coping mechanisms for both patient and family, namely, (a) seeking social support, (b) reliance on God, (c) positive suggestion/attitude or reaffirmation, and (d) acquisition of information and education.[11]
Relationship between stress and coping adopted by caregivers of cancer patients on palliative care
The present study findings revealed that there is a significant negative correlation (r = −0.722, P = 0.005) between stress and coping among caregivers of cancer patients on palliative care.
This study also supports a study conducted to assess the level of burden and coping among caregivers of terminally ill cancer patients at Neiyyur, Kanyakumari. The study findings revealed that 68% of the caregivers had moderate burden and 32% had severe burden. Twenty-two percent of the caregivers had minimal coping and 78% had moderate coping. There was negative correlation between caregivers burden and coping (r = −0.6, P = 0.005).[12]
The present study also supports a cross-sectional study conducted in a pain and palliative care unit in Spain, which revealed that the caregivers utilized mainly the “acceptance” method among the “emotional coping” methods, while cancer patients utilized the dysfunctional coping methods and denial among subgroups. Moreover, a statistically significant difference and negative correlation between the dysfunctional coping scores and anxiety was determined.[13]
Lived experiences among caregivers of cancer patients on palliative care
In the present study, lived experiences among cancer patients on palliative care were evolved with a phenomenon of “caring companionship to palliative care” with six themes namely “adaptation to life,” “pillars of support,” “trusting relationship” “shield of strength and courage,” “stress and strain,” and “living with fear and uncertainty” and 24 subthemes.
Findings of the present study also support the findings of an integrative review conducted in Thailand to describe the findings from Thai studies cancer concerning family caregivers of cancer patients which reported themes pertaining caregiver's experiences comprised of six categories: (a) “being committed for life to spouses,” (b) “enhancing spouse's comfort,” (c) “being a cosufferer,” (d) “ readjusting themselves,” (e) “appreciating people's support,” and (f) “being gratified with self-development and marital life growth.”[14]
This study also confirms the findings of a meta-synthesis study which revealed that caregivers of persons with advanced cancer living in the community experience multiple, concurrent transitions. The types of transitions were reflected in five overlapping themes: (a) environmental, (b) roles and relationships, (c) physical and mental health, (d) spirituality, and (e) priorities. The participants dealt with the transitions through the processes of (a) coming to terms, (b) connecting with others, and (c) redefining normal.[15]
CONCLUSION
Palliative care for cancer patient affects not only the patients but also their caregivers. When giving palliative care to cancer patients, caregivers are confronted with physical and emotional challenges. During palliative care, caregivers assume significant roles to support the patients. Although caregiving becomes a full time job, the caregivers are trying their level best to add life and cheer to the days of cancer patient on palliative care by providing caring companionship.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1. [Last retrieved on 2016 Nov 12]. Available from: http://www.who.int/mediacentre/factsheets/fs402/en/
- 2. [Last retrieved on 2016 Nov 16]. Available from: https://www.cancer.icmr/about-cancer/understanding/statistics .
- 3.Northouse LL, Katapodi MC, Song L, Zhang L, Mood DW. Interventions with family caregivers of cancer patients: Meta-analysis of randomized trials. CA Cancer J Clin. 2010;60:317–39. doi: 10.3322/caac.20081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cannolly J, MIlligan S. Knowledge and skills needed by informal carers to look after terminally ill patients at home. End Life J. 2014;4:1–14. [Google Scholar]
- 5. [Last retrieved on 2016 Dec 12]. Available from: http://www.who.int/cancer/palliative/en/
- 6.Given B, Wyatt G, Given C, Gift A, Sherwood P, Devoss P, et al. Burden and depression among caregivers of patients with cancer. Oncology Nursing Forum. 2004;31:1105–17. doi: 10.1188/04.ONF.1105-1117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. [Last retrieved on 2016 Oct 15]. Available from: http://www.Palliativecare.in/wp-content/uploads/./End-of-Life-Care-IAPC .
- 8.Gupta A, Sharma R. Burden and coping of care givers of physical and mental illness. Delhi Psychiatry J. 2013;16:367–73. [Google Scholar]
- 9.Kulkarni P, Kulkarni P, Ghooi R, Bhatwadekar M, Thatte N, Anavkar V, et al. Stress among care givers: The impact of nursing a relative with cancer. Indian J Palliat Care. 2014;20:31–9. doi: 10.4103/0973-1075.125554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stajduhar K, Barwich D, Fyles G. Family Caregiver Coping in End of Life Cancer Care. Cancer Nursing. 2008;31:77–9. doi: 10.1097/01.NCC.0000305686.36637.b5. [DOI] [PubMed] [Google Scholar]
- 11.Mukwato K, Mweemba M, Makukula M, Makoleka M. Stress and coping mechanisms among breast cancer patients and family caregivers: A review of literature. Med J Sambia. 2010;37:41–6. [Google Scholar]
- 12.Chellappan S, Rajamanikam R. Caregivers’ burden and coping among caregivers’ of terminally ill cancer patients. Int J Nurs Educ Res. 2016;4:41–6. [Google Scholar]
- 13.Aydogan U, Doganer YC, Komurcu S, Ozturk B, Ozet A, Saglam K, et al. Coping attitudes of cancer patients and their caregivers and quality of life of caregivers. Indian J Palliat Care. 2016;22:150–6. doi: 10.4103/0973-1075.179598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Meecharoen W, NorthHouse L, Yupapin S, Monkong S. Family caregivers for cancer patients in Thailand: An integrative review. Sage Open. 2013;10:1–11. [Google Scholar]
- 15.Duggleby W, Parmar J, Nekolaichuk C, Mirhosseini M, Hotslander L, Hudson P, et al. Metasynthesis Study of Family Caregivers of Community Dwelling Persons with Advanced Cancer. Palliative medicine. 2017;31:602–16. doi: 10.1177/0269216316673548. [DOI] [PubMed] [Google Scholar]