Abstract
Background:
Antenatal care (ANC) is one of the basic components where it can provide pregnant women with an expansive scope of well-being, health promotion, and preventive health services. However, still 830 women die every day from preventable pregnancy-related causes, and 99% of these deaths occur in developing countries, out of which 20% of these deaths were from India.
Objectives:
The objective of this study is to explore the factors influencing the utilization of reproductive health services among mothers and to find the association between various factors and utilization of reproductive health services.
Methods:
A community-based cross-sectional study was conducted during January–June 2017 among 160 mothers who had an infant aged <6 months in Mawkyrwat Block, South West Khasi Hills District in Meghalaya. Respondents were selected through simple random sampling, and semi-structured questionnaire was used for data collection. Data were analyzed using SPSS 16.
Results:
Mothers attending four or more antenatal checkups were 10.6%, where 53.5% of the mothers registered their first ANC checkups only by the second trimester and 57.5% preferred home delivery. Nearly 52.9% of the mothers were staying more than 5 km away from the health-care facilities. The usage of family planning methods was very low, i. e., 96.9% of the mothers are not using any of the family planning methods.
Conclusion:
Study finding reveals that the utilization of health-care services was low. Area-specific approaches such as health camps and mobile clinics might result in improved utilization of reproductive health services.
Keywords: Antenatal care services, antenatal care, intranatal care, reproductive health, utilization
Introduction
In India, maternal and child health has remained an integral part of the Family Welfare Programme of India since the time of the First and Second 5-Year Plans (1951–1956 and 1956–1961) when the Government of India took steps to strengthen maternal and child health services. To improve the services, especially for people residing in rural and urban areas, the government has launched the National Health Mission (NHM) in 2005, i.e. to provide access to improved health care at the household level through Accredited Social Health Activist (ASHA) which acts as an interface between the community and the public health system. In some of the areas with limited resources, trained birth attendants (TBAs) help a women to delivered their babies at home.[1]
The NHM envisages achievement of universal access to equitable, affordable, and quality health-care services that are accountable and responsive to people needs.[2] Under the NHM, a wide range of interventions have been ensured for effective health care, in spite of the availability of intervention reductions in maternal mortality and morbidity still remains a challenge. Under the NHM, they have come up with Meghalaya Maternity Benefit Scheme where incentives will be given to the mother with the aim to promote institutional delivery and to bring down maternal mortality.[3]
Preventing death of the mothers during pregnancy and after the childbirth is one of the key interventions to bring down the maternal mortality.[4] In India, maternal mortality ratio (MMR) has declined from 178 deaths/100,000 live births in 2010–2012 to 167 deaths/100,000 live births in 2011–2013 and infant mortality rate of 40 deaths/1000 births in 2013.[4] These indicators will be the backbone of monitoring the progress toward the Sustainable Development Goals 2030 (SDGs), where SDGs target to reduce the global MMR to <70/100,000 live births.[5] The World Health Organization recommends a minimum of four antenatal care (ANC) visits, comprising interventions such as tetanus toxoid (TT) vaccination, iron-folic acid tablets, screening and treatment for infections, and identification of warning signs during pregnancy.[6] The health of mothers and the baby depends on an operational continuum of care with accessible, high-quality care before and during pregnancy, childbirth, and postnatal period.[7]
According to the National Family Health Survey-4 (NFHS-4), in Meghalaya, mothers who had antenatal checkups in the first trimester were 53.3% and mothers who had at least four antenatal checkups were 50%. Mothers who had mother and child protection cards were 93.6%. In national surveys, it has been shown that mothers in West Khasi Hills District who had antenatal checkup in the first trimester were 36.3%, mothers who had at least four antenatal checkups were 40.4%, and mothers who had mother and child protection card were 94%. Mothers accessing modern methods of family planning services were 19.1%, intrauterine device was 2.4%, pills were 10.3%, condoms were 0.9%, and mothers who underwent female sterilization were 5.6%.[8] These data are indicative of the improper utilization of health services in the state. This study had been designed to understand the factors influencing the utilization of health services in the state.
Methods
A community-based cross-sectional study was conducted in Mawkyrwat Block, South West Khasi Hills District, Meghalaya. Mawkyrwat Block has 140 villages, 1 community health center, 2 primary health centers, and 13 subcenters.
The sample size for the study was calculated as 158, based on the NFHS-4 result that 40.4% of the mothers had at least four ANC visits and a nonresponse rate of 10%. Data were collected during January–March 2017.
A two-stage random sampling procedure was adopted for the study. At the first stage, 16 villages in Mawkyrwat Block were selected using simple random sampling technique. A list of all eligible mothers (who were having <6-month-old baby at the time of data collection) was prepared from the birth records maintained by ASHA for the selected villages. In the second stage, 160 eligible mothers were selected randomly from the list. Using a semi-structured questionnaire, face-to-face interviews were conducted among the selected mothers after obtaining the written consent.
Kasturba Medical College and Kasturba Hospital Ethics Committee approved the study protocol, and permission was taken from the District Medical and Health Officer to conduct the study at Mawkyrwat Block.
Data were entered and analyzed using Statistical Package for the Social Sciences version 16.0. The categorical variables were expressed in frequency and percentage and the continuous variable in mean and standard deviation. Chi-square test was performed to measure the association between independent variables and utilization of services. P < 0.05 was considered to be statistically significant.
Results
A total of 160 mothers having babies <6 months were interviewed.
The mean age of the respondents was 27.8 years, and 45.6% were working as clerks, shop owners, or farmers. About 57.5% of the respondents belong to nuclear family. Almost 65% of the respondents had a family income of <Rs. 5000 a month. About 39 (24%) mothers, reported of having financial problems, did not have enough money for transportation to health facilities and cited of wage loss to avail services.
Of 124 (77.5%) mothers who had a previous pregnancy, 99.2% of them were normal delivery, 66.9% were home delivery, 64.5% of the deliveries were conducted by trained birth attendants, and 3.2% has experienced labor difficulty or complications.
During the recent pregnancy, 89.4% of the respondents had <4 ANC visits, and 18.8% of the mother felt that they feel healthy during the pregnancy period and also due to the difficulty in getting transport to visit the health facilities. Almost 53.5% attended their first ANC checkups only by the second trimesters. Of 89.4% of the mothers who attended <4 ANC checkups, three mothers did not have any ANC visits.
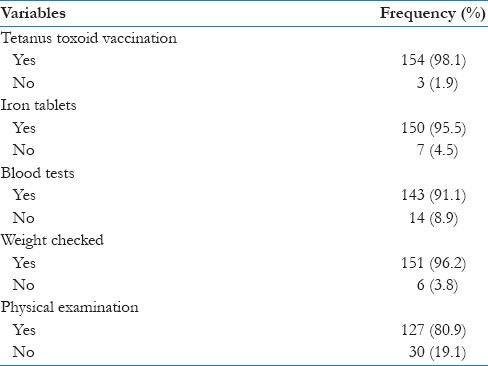
About 98.1% of the mothers received TT vaccination. Almost 95.5% of the study participants took iron tablets, but on further inquiry, it was known that the compliance for the iron tablet was less due to its side effects. Majority of the mothers did blood tests (91.1%), checked the weight gain during pregnancy (96.2%), and also underwent physical examination (80.9%) [Table 1].
Table 1.
Distribution of respondents according to the utilization of antenatal services by during recent antenatal care visits (n=157)
Almost half of the respondents (53.6%) whose residence was more than 5 km from the health facility had gone for <4 antenatal visits.
Majority (57.5%) of the respondents underwent home delivery. The reasons given by the mother for opting home delivery were due to the sudden onset of labor (21.8%), the trust on TBA (12.5%), giving more importance to household work (7.5%), and other reasons (17.5%) such as feeling healthy and shying away from availing the services. The other reasons found were unavailability of doctors at night time as well as during weekends. Based on the observation, mothers could not access much to the health care services as there were no subcenters nearby.
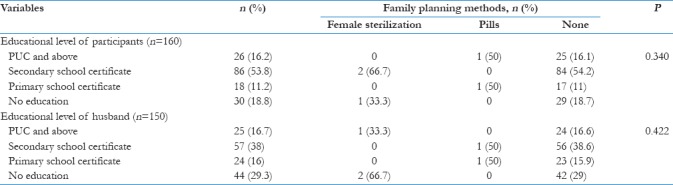
Majority (96.9%) of the respondents were not using any of the family planning methods. The main reasons for not using it were due to the decision taken by the respondents herself (33.12%) and husband decision (15.62%); 15% of respondents were due to the decision taken by her family. This is indicative of the role of family in making decisions related to the health-seeking behavior. Mothers as well as the husbands of the respondents play a major role in making decisions related to the health of the pregnant mothers. It was also observed that both the couples (8.12%) do not want to use any of the family planning methods. The other reasons (25%) for not using any of the family planning methods were presence of male doctors at the health facilities, belief that child was God's gift, and lack of counseling services for family planning, and some of the respondents were about to attain menopause. The findings were indicative that the education of the respondents and husbands does not play much role on the times of antenatal visits as well as the employment status and family income also did not have any significant influence on the antenatal visits done [Table 2]. The family planning methods do not vary with the educational level of the respondents and their spouse [Table 3].
Table 2.
Association between educational level with number of antenatal visits during recent pregnancy
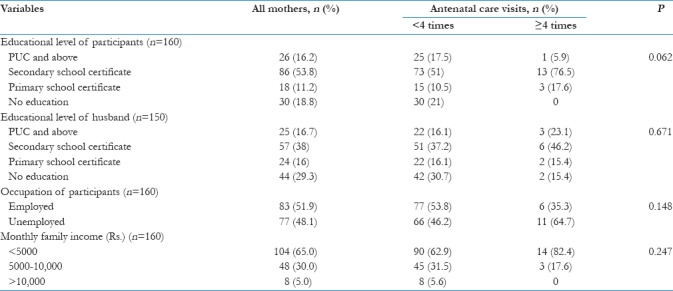
Table 3.
Association between educational level and family planning methods
Discussion
The study revealed that the mothers accessing the health-care services were low. The study findings reveal that the mothers attending the ANC checkups for more than 4 times were low, mothers registered their first ANC checkups only by the second trimester, and they prefer home delivery with the assistance of TBAs. The mothers also responded that they opted for home delivery due to the sudden onset of labor, trust on TBAs, and increased significance for household work. Other reasons being shy to avail services from the male health workers. Similar findings were observed in a study among tribal population where most respondents had attended the ANC for at least one, majority of mothers received their first ANC checkups by the second trimester, and child deliveries occurred at home.[9]
Exploring into the factors almost half of the mothers (52.9%) reported distance to be one of the factors that hinder the mothers in accessing the health-care services. However, distance and transportation together can be factors that contribute to the delay in the registration of pregnancy. A mother has to travel for a long period of time to avail the health-care services due to geographical barriers and lack of proper construction of the road.
The sociodemographic characteristics and ANC visits were not significantly associated with the utilization of health-care services for the ANC visits. One of the studies revealed that occupation as well as education was found to influence the frequency of ANC visits done.[10]
Another important domain drawn out from this study was 96.9% of the mothers who were not using any of the family planning methods. The mothers responded that the reasons for not using any of these methods were due to the decisions taken by the respondents herself and decision taken by husband and parents and other reasons were both the couples did not want to use any of the family planning methods. There are also reasons that contribute such as the presence of male doctors at the health facilities and cultural factors.
This study was attempted to explore factors influencing utilization of services. This study shows that the mother attended the ANC visits for at least once, and most of the mothers opted for home delivery due to certain conditions. Factors such as finance, distance, transportation, familial system, and culture were the reasons that influence the health-seeking behavior.
Conclusion
In spite of the governmental efforts of introducing many financial schemes so as to enhance the number of ANC checkups and to promote institutional delivery, the utilization has been less due to various reasons such as geographical barriers and sociocultural reasons that hinder the mothers in accessing the health-care services which is a matter of concern and needs more attention by the administrators and policymakers.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
I would like to thank Manipal University and NEIGRIHMS, Shillong, for support in carrying out this research.
References
- 1.Agus Y, Horiuchi S. Factors influencing the use of antenatal care in rural west Sumatra, Indonesia. BMC Pregnancy Childbirth. 2012;12:9. doi: 10.1186/1471-2393-12-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vol. 1. Mumbai: International Institute for Population Sciences; 2007. International Institute for Population Sciences and Macro International. National Family Health Survey (NFHS.3), 2005-06: India. [Google Scholar]
- 3.NHM-Governnment of India. [Last accessed on 2017 May 11]. Available from: http://www.nhm.gov.in/nhm.html .
- 4.MMBS. [Last accessed on 2017 May 11]. Available from: http://www.nrhmmeghalaya.nic.in/spip/stateinitiatves/mmbs.html .
- 5.Sustainable Development Goals. Indicators and a Monitoring Framework for the Sustainable Development Goals. [Last accessed on 2017 May 09]. Available from: https://www.suatainabledevelopment.un.org/index.ohp .
- 6.Gupta RK, Shora TN, Verma AK, Jan R. Knowledge regarding antenatal care services, its utilization, and delivery practices in mothers in a rural area of North India. [Last accessed on 2017 May 09];Trop J Med Res. 2015 18:89–94. Available from: http://www.tjmrjournal.org/text.asp?2015/18/2/89/158401 . [Google Scholar]
- 7.Arute JE, Eniojukan JF, Odili VO. Quality of life in pregnant women attending anti-natal clinics in rural and urban areas of delta state. Value Health. 2014;17:A518. doi: 10.1016/j.jval.2014.08.1612. [DOI] [PubMed] [Google Scholar]
- 8.National Family Health Survey. [Last accessed on 2017 May 11]. Available from: http://www.rchiips.org/NFHS/factsheet_NFHS-4.shtml .
- 9.Varma GR, Kusuma YS, Babu BV. Antenatal care service utilization in tribal and rural areas in a South Indian district: An evaluation through mixed methods approach. J Egypt Public Health Assoc. 2011;86:11–5. doi: 10.1097/01.EPX.0000395395.17777.be. [DOI] [PubMed] [Google Scholar]
- 10.Kawungezi PC, AkiiBua D, Aleni C, Chitayi M, Niwaha A, Kazibwe A, et al. Attendance and utilization of antenatal care (ANC) services: Multi-center study in upcountry areas of Uganda. Open J Prev Med. 2015;5:132–42. doi: 10.4236/ojpm.2015.53016. [DOI] [PMC free article] [PubMed] [Google Scholar]


