Abstract
Background and Objectives:
Sexual health disorders are an important but less researched public health issue in India. We aimed to estimate the prevalence of sexual health disorders and their associated factors among adult men in a rural community of Haryana, India.
Materials and Methods:
A community-based cross-sectional study was conducted among adult men aged 18–60 years using a multistage stratified random sampling. Information pertaining to sociodemographic characteristics, lifestyle and sexual practices, and self-reported sexual problems were collected. Sexual health disorders were defined based on International Statistical Classification of Diseases-10 classification of mental and behavioral disorders. Step-wise logistic regression was carried out to identify factors independently associated with sexual disorders.
Results:
At least one sexual health disorder was reported by 81% of the men. The most commonly reported disorder was self-perceived defect in semen (64.4%), followed by loss of libido (21%), masturbation guilt (20.8%), erectile dysfunction (5%), and premature ejaculation (4.6%). Factors significantly associated with sexual health disorders among all men were being never married (odds ratio = 2.04; 95% confidence interval: 1.51, 2.77), smoking (1.57; 1.16, 2.14), cannabis use (4.20; 1.68, 10.48), diabetes (2.40; 1.22, 4.73), and hypertension (3.17; 1.12, 8.92).
Interpretation and Conclusions:
A high burden of sexual health disorders was identified among the rural men. Wider recognition of this issue is needed among the health-care providers and policymakers.
Keywords: India, prevalence, rural, sexual health disorders
Introduction
Sexual health is an indispensable dimension of good health. Poor sexual health, either psychological or pathological, can seriously affect the quality of life of adolescent and adult men.[1] It is also a poorly recognized public health problem in India and elsewhere.[1,2] In India, general practitioners, who are the first point of contact for health care, are trained inadequately to deal with common sexual health problems.[3] Furthermore, access to experts such as urologists, sexologists, and andrologists is available only to men living in urban areas, where there is a high concentration of tertiary care hospitals and specialists.[4] This health-care vacuum has led to a thriving business for quacks who take advantage of the ignorance and the fear of patients.[5,6,7,8] In India, the concepts of sexuality are woven into the very fabric of everyday life and the disorders of sex are often stigmatized and considered shameful, which prevent timely and appropriate treatment.[9] Traditional Indian Systems of Medicine (ISM), has a well-developed epistemology based on the teachings handed down from generation to generation. These concepts do not often agree with modern medicine, but they have a strong presence in the common man's understanding and have greatly influenced their lexicon. This gives rise to the concept of culture-bound syndromes, which are defined as a symptom cluster influenced by cultural factors and individual perceptions, rather than being a recognizable biochemical or physical alteration according to modern medical systems.[10] There is evidence that patients suffering from sex-related symptoms often prefer practitioners of ISM more than allopathic doctors.[11]
Many recent studies from India have reported on the prevalence of sexual health disorders among various study populations.[12,13] However, some studies conducted among adult men attending hospital clinics have reported a lower prevalence.[14,15] Apart from the estimation of burden, a few studies have also explored the risk factors associated with sexual health disorders. Among the lifestyle factors, smoking, tobacco chewing, alcohol dependence, and opioid dependence have been implicated.[16,17,18] Diabetes mellitus,[19] psychiatric disorders,[20,21,22,23] and coronary artery disease[24] were common comorbidities associated with different sexual health disorders. Erectile dysfunction (ED) has also been found to be related to poor marital and sexual satisfaction in a study done in Northern India.[25]
Despite the importance of this issue as outlined above, in India, there is very little data about the burden of sexual health disorders from community-based studies, unlike some Western countries where some data are available.[26,27] There is a lack of clear understanding of factors that influence the occurrence of sexual health disorders in the Indian context, especially substance abuse which has been shown to be significantly associated with sexual disorders.[16,17,18] In India, studies on sexual health disorders are largely limited to hospital settings.[15,28] Therefore, we planned this community-based study with the objective to estimate the prevalence of various sexual health disorders and their associated factors among adult men residing in a rural community of Haryana, India.
Materials and Methods
Study setting and study population
The study was conducted in the villages of the Ballabgarh block of Faridabad, Haryana, that form the catchment area for the Comprehensive Rural Health Services Project, Centre for Community Medicine, All India Institute of Medical Sciences (AIIMS), New Delhi.[29] Sociodemographic details and other health-related information of population residing in these villages is maintained in a computerized Health Management Information System (HMIS). The sampling frame for this community-based cross-sectional study included all adult men aged 18–60 years in the study area.
Sample size and sampling strategy
The minimum required sample size was calculated for an assumed prevalence of sexual health disorders of 53%,[6] a precision of 5%, a design effect of 2.25, and a nonresponse rate of 20%. The required sample size was calculated as 1120. The design effect was used to take into account the clustering effect of the complex multistage sampling strategy that we employed. In the first stage, we randomly selected three villages from a total of 28 villages. In the second stage, participants in the three selected villages were randomly selected from among the eligible population using a software-based random selection procedure using the HMIS database. The sampling frame included all adults in the eligible age group who were residing in the study area for the past 6 months. Those who were unable to respond to questions due to problems of comprehension or sickness and those unwilling to give consent were excluded from the study. The data collection period was June–July 2014.
Study instruments
The survey instrument was a pretested interview schedule, which included questions on sociodemographic characteristics, lifestyle and sexual practices, and self-reported sexual problems. The interview schedule was prepared by three authors (VS, AKS, and RSA) drawing from previous similar studies to meet the objectives of the study. A small focus group discussion with young adults of the study area was conducted to refine the interview schedule and answering options. The English version was translated to Hindi and back translated to check for consistency of meaning.
Data collection procedure
Qualified male social workers, who were aware of local customs but did not belong to the study villages carried out the data collection. These social workers were middle-aged married men who were trained to show empathy if the situation demanded and interviews were carried out in settings of privacy, so as to ensure valid responses. Data collection was supervised on a weekly basis by RSA. The participants were given sufficient time to come out with the problems they had and before the interview began they were assured of the confidentiality of their information. Data collection forms were stored under lock and key on daily basis by VS. Sufficient care was taken to ensure that the information gathered was not shared with anyone else.
Operational definitions
Current sexual health disorder
Symptoms/disorders present at the time of interview or within 6 months of the interview were considered to be current disorders.
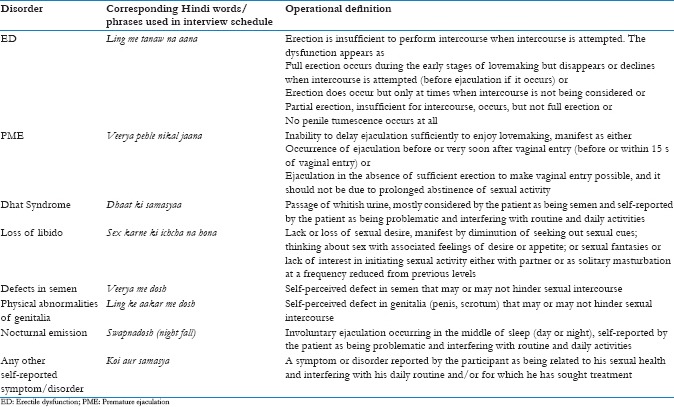
Sexual health disorders (ED, premature ejaculation, Dhat syndrome, loss of libido, defects in semen, physical abnormalities of external genitalia, nocturnal emission, and others conditions) based on the International Statistical Classification of Diseases-10 classification of mental and behavioral disorders, diagnostic criteria for research were the main outcome measures for this study.[30] [Box 1]. All symptoms and diseases were self-reported and no clinical examination was carried out. Data on the past sexual health disorders were not collected in this study.
Box 1.
Operational definitions of sexual health disorders included in this study
Statistical analysis
Descriptive analysis was done and the results were presented as percentages with 95% confidence intervals (CI). Prevalences of various sexual health disorders were stratified according to age (18–30 years and >30 years) and marital status (ever married and never married). Bivariate analysis was done to delineate the factors associated with sexual health disorders. Step-wise logistic regression was carried out to identify factors that were independently associated with the outcomes. Those variables which had a P < 0.25 in the bivariate analysis were included in the multivariable regression. Associations were reported in terms of unadjusted and adjusted odds ratios and 95% CI. A P < 0.05 was considered to be statistically significant. All analyses were done in Stata 12 (Stata Corp, College Station, Texas, USA). Data analysis was done by RSA and AL.
Ethical issues
Ethical clearance was obtained from the Institute Ethics Committee, AIIMS, New Delhi (Reference letter number; IEC/NP-278/2012). All the participants were provided with a participant information sheet and written informed consent was obtained. Participants needing treatment were referred to the subdistrict hospital, Ballabgarh, for counseling and further management by qualified specialists.
Results
Sociodemographic characteristics
Of the 1120 randomly selected men, 894 took part in the study giving a nonresponse rate was 20.2%. The proportion of nonresponse was higher among those aged >30 years as compared to those aged 18–30 years (32.7% vs. 6.5%). The two main reasons for nonresponse were locked house/inability to contact even after two house visits (17%) and refusal to participate in the study (3%). In the final sample, 60% of the men were below 30 years of age, most (76.3%) were educated up to high school or above and about two-thirds of men were currently married [Table 1].
Table 1.
Characteristics of the study participants
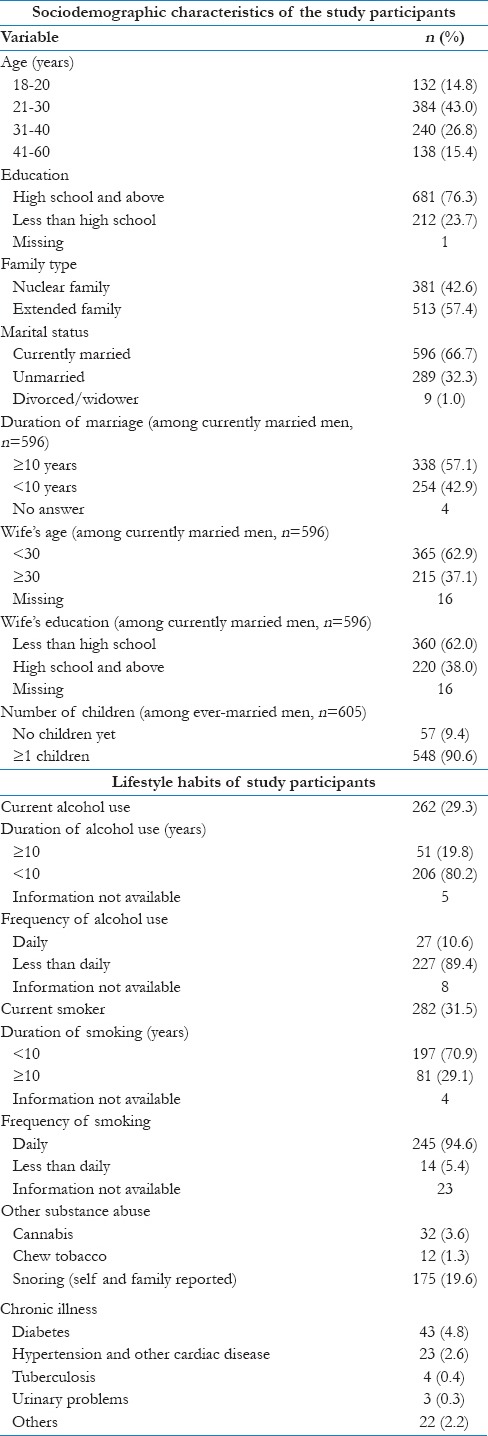
Lifestyle practices
Nearly one-third of the men were current smokers (31.5%) and 29.3% were current alcohol consumers. Among the comorbidities reported, diabetes was the most common (4.8%), followed by hypertension (2.3%) [Table 1].
Prevalence of self-reported sexual health disorders
About 81% of the men reported currently experiencing at least one sexual health disorder. Three or more sexual health disorders were present in 14%. About two-thirds reported to have a self-perceived defect in semen. Other commonly reported disorders were loss of libido (21%) and masturbation guilt (21%). Other problems such as nocturnal emission (13.6%), inability to retract foreskin (5.1%), ED (5.0%), Dhat syndrome (4.8%), and premature ejaculation (4.6%) were less commonly reported. The prevalences of loss of libido (29.6% vs. 3.1%) and ED (6.8% vs. 1.4) were significantly higher in the ever-married group, whereas the prevalences of nocturnal emission (30.4% vs. 5.6%) and inability to retract foreskin (12.1% vs. 1.8%) were significantly higher in the never married group. Presence of at least one sexual health problem was reported by 78.8% of ever-married men, whereas it was 86.5% in never-married men and the difference was statistically significant (P < 0.05) [Table 2].
Table 2.
Prevalence of sexual health disorders (overall and stratified by marital status and age)
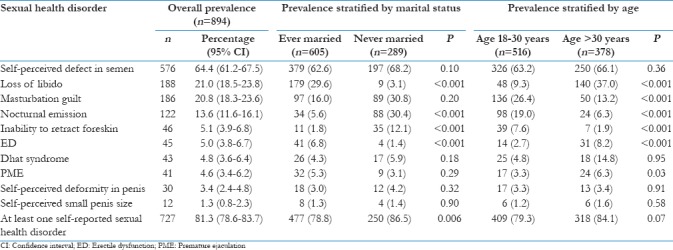
Stratification of the prevalence of sexual health disorders by age showed that loss of libido (37.0% vs. 9.3%), ED (7.6% vs. 1.9%), and premature ejaculation (6.3% vs. 3.3%) were higher among those aged >30 years, whereas masturbation guilt (26.4% vs. 13.2%), nocturnal emission (19.0% vs. 6.3%), and inability to retract foreskin (7.6% vs. 1.9%) were more common among those aged 18–30 years [Table 2].
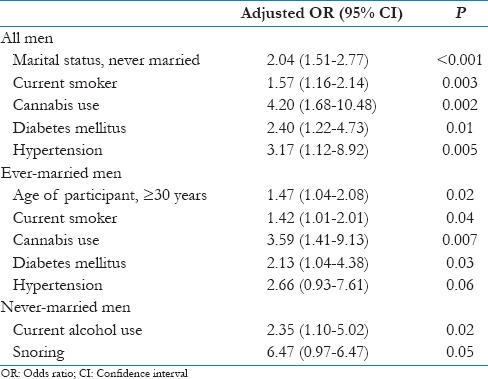
Factors associated with sexual health disorders
Bivariate analysis revealed that a number of factors were associated with the increased odds of having a sexual health disorder. Multivariable logistic regression for all men showed that being never married, current smoking, cannabis use, diabetes, and hypertension were associated with the presence of a sexual health disorder [Table 3]. However, it was seen from the bivariate analysis that ever-married men were more likely to report ED and PME, whereas never-married men were more likely to report other sexual health disorders. Since the type of disorder varied according to the marital status, which was also a function of age, we conducted separate logistic regressions for ever- and never-married men. Among ever-married men, factors significantly associated with having a sexual health disorder were age ≥30 years, current smoking, cannabis use, diabetes, and hypertension. Among never-married men, current alcohol use and snoring were associated with the presence of a sexual health disorder [Table 3].
Table 3.
Factors independently associated with sexual health disorders stratified by marital status - step-wise logistic regression
Discussion
This community-based study conducted among a random sample of men aged 18–60 years in rural Haryana found that there is a huge burden of sexual health disorders among the rural men in this part of the country. The burden of sexual disorders was higher among never-married men as compared to the ever-married men.
Prevalence of sexual health disorders – comparison with Indian studies
In a community-based study done in Mumbai, PME (16.1%) was the most common self-reported sexual health problems.[7] The prevalence of PME in their study was almost three times that reported in our study. This difference was probably due to the difference in the sociodemographic characteristics of the participants, who were all married men aged 21–40 years with a lower mean educational status. On the other hand, recent hospital-based study from Southern India has reported the prevalences of ED and PME to be 48% and 43%, respectively.[12] However, in another study, the prevalences of PME and ED were found to be 18% and 17%, respectively.[15] Hospital-based studies tend to overestimate the burden of a particular sexual disorder such as ED or PME because their study population consists of a self-selected group that seeks care for their perceived sexual health problems. Furthermore, these patients tend to seek care for those conditions that are severe, disabling, and affect their day-to-day life. Therefore, estimating the prevalence of sexual health disorders from hospital-based studies would lead to spuriously high results.
Prevalence of sexual health disorders – comparison with global studies
Since there is a paucity of community-based studies in India, we compared our results with the community-based studies done outside India. These studies have reported a higher prevalence for individual disorders such as ED and PME when compared to the current study.[27,31] A higher reported prevalence in these studies was probably due to their study population being older than that of our study.
Correlates of sexual health disorders
It has been very well documented that diabetes, hypertension, and lifestyle practices such as smoking and alcohol consumption are associated with various sexual health problems.[19,31,32] Similarly, we also found that sexual health problems were significantly associated with the presence of diabetes, hypertension, or any chronic illness. It was also seen that current smokers and cannabis consumers were more likely to report sexual health problems than those without such habits.
Multifactorial etiology of sexual health disorders
Apart from medical causes and addictions, sexual health disorders are frequently associated with false beliefs and misconceptions. Because of the social inhibition and taboos associated with sex and its discussion, doubts related to sexual health are not frequently addressed by peers or friends, who themselves are not well informed on these matters, and therefore, the misconceptions just linger on and spread through the social network.[12] Even when the decision is taken to seek care beyond the friend circle, it is frequently sought from local unqualified quacks because they are easily accessibility.[7,12] Sometimes, even physicians are not adequately trained to manage sexual health disorders.[3] This adds to the worsening of the problems by delaying diagnosis of genuine cases who require expert care, propagating misconceptions, and affecting the overall quality of life, which then transforms into a vicious cycle of poor psychological health in turn affecting sexual health.
It is clear from the above-mentioned points that most sexual disorders have a multifactorial etiology including medical causes, addictions, lack of awareness, social stigma, and poor health seeking behavior. Hence, a multipronged approach is required to address the burden of sexual health disorders in the community.
Strengths and limitations
To the best of our knowledge, this is among one of the very few community-based studies that have exclusively explored the prevalence of sexual health disorders among men in North India. This study has explored the sexual health problems of men who were sexually naïve, which have not been adequately reported hitherto.
However, there are a number of limitations that have to be considered. First, a number of factors such as low testosterone level, higher body mass index, psychiatric disorders, prostate disorders, and dyslipidemia have been documented as risk factors for sexual disorders, but we could not explore these in this study due to scope limitations. Second, due to the differential and higher nonresponse rate (32.7%) among participants aged more than 30 years, the final age composition of the participants was not representative of the source population, which might affect the estimate of the overall prevalence. Third, another cause for the underestimation of the true burden may be the taboos surrounding sex and sexual health in rural communities of India, leading to a social desirability bias. A confidential polling booth method, which has been found to have greater utility in eliciting unbiased results in such sensitive issues, would have been useful. Fourth, we were not able to cover the entire spectrum of sexual health disorders in the current study, for example, conditions such as orgasmic dysfunction, sexual aversion, and excessive sexual drive have not been assessed. Fifth, only self-reported information was collected and no clinical examination was performed due to practical and logistic reasons, and therefore, it was not possible to differentiate between pathological and psychological ED.
Future directions of the study
It is clear from the discussion that a major proportion of sexual health disorders reported by these men have a psychological etiology. This strengthens the argument in favor of integrating the care of sexual health disorders under the ambit of the mental health program in India. It is well know that the mental health program, in India, is plagued by a shortage of trained psychiatrists even in urban areas, and therefore, primary care physicians, ISM practitioners, and paramedical staffs such as clinical psychologists could be trained for identifying and treating common sexual health disorders with a system of referral reserved for complicated cases. There is a great need to educate the population from a relatively young age about sexuality and reproductive health, which is currently lacking in India. A number of avenues are available to promote sexual health education but integrating this into the school curriculum may be an easy and effective public health approach. Although only men were included in the study, women are also equally likely to suffer from sexual health issues and future studies should focus on them. The presence of such a high burden of sexual health problems could be a cause of mental stress, marital discord, and poor quality of life that needs exploration in the future studies.
Conclusions
There was a high burden of sexual health disorders among adult men in this rural community of Haryana. Wider recognition of this issue is needed among health-care providers and policymakers.
Recommendations
Training of primary health-care providers, general physicians, and family physicians on the early recognition and proper treatment and/or referral of patients with sexual complaints would go a long way in reducing the unnecessary burden of poor health due to sexual health disorders. Family and primary care physicians have a pivotal role in recognizing sexual health problems during consultation for other conditions in an opportunistic manner. Sexual health problems, unlike other disease conditions, carry a lot of taboo and social inhibition-related factors that prevent their effective management. Hence, the findings of this study are very relevant in context with family medicine or primary care practice in India.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We acknowledge the staff members of subdistrict hospital, Ballabgarh, who facilitated data collection.
References
- 1.Flynn KE, Lin L, Bruner DW, Cyranowski JM, Hahn EA, Jeffery DD, et al. Sexual satisfaction and the importance of sexual health to quality of life throughout the life course of U.S. adults. J Sex Med. 2016;13:1642–50. doi: 10.1016/j.jsxm.2016.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Balon R. Burden of sexual dysfunction. J Sex Marital Ther. 2017;43:49–55. doi: 10.1080/0092623X.2015.1113597. [DOI] [PubMed] [Google Scholar]
- 3.Bharat S, Mahendra VS. Meeting the sexual and reproductive health needs of people living with HIV: Challenges for health care providers. Reprod Health Matters. 2007;15:93–112. doi: 10.1016/S0968-8080(07)29030-5. [DOI] [PubMed] [Google Scholar]
- 4.Deo MG. Doctor population ratio for India – The reality. Indian J Med Res. 2013;137:632–5. [PMC free article] [PubMed] [Google Scholar]
- 5.Das J, Mohpal A. Socioeconomic status and quality of care in rural India: New evidence from provider and household surveys. Health Aff (Millwood) 2016;35:1764–73. doi: 10.1377/hlthaff.2016.0558. [DOI] [PubMed] [Google Scholar]
- 6.Schensul SL, Mekki-Berrada A, Nastasi B, Saggurti N, Verma RK. Healing traditions and men's sexual health in Mumbai, India: The realities of practiced medicine in urban poor communities. Soc Sci Med. 2006;62:2774–85. doi: 10.1016/j.socscimed.2005.11.003. [DOI] [PubMed] [Google Scholar]
- 7.Schensul SL, Verma RK, Nastasi BK. Responding to men's sexual concerns: Research and intervention in slum communities in Mumbai, India. [Last accessed on 2017 Mar 31];Int J Mens Health. 2004 3:197–220. Available from: http://www.mensstudies.info/OJS/index.php/IJMH/article/view/448 . [Google Scholar]
- 8.Verma RK, Sharma S, Singh R, Rangaiyan G, Pelto PJ. Beliefs concerning sexual health problems and treatment seeking among men in an Indian slum community. Cult Health Sex. 2003;5:265–76. [Google Scholar]
- 9.Chakraborty K, Thakurata RG. Indian concepts on sexuality. Indian J Psychiatry. 2013;55:S250–5. doi: 10.4103/0019-5545.105546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Levine RE, Gaw AC. Culture-bound syndromes. Psychiatr Clin North Am. 1995;18:523–36. [PubMed] [Google Scholar]
- 11.Pulla P. Are India's quacks the answer to its shortage of doctors? BMJ. 2016;352:i291. doi: 10.1136/bmj.i291. [DOI] [PubMed] [Google Scholar]
- 12.Thangadurai P, Gopalakrishnan R, Kuruvilla A, Jacob KS, Abraham VJ, Prasad J, et al. Sexual dysfunction among men in secondary care in Southern India: Nature, prevalence, clinical features and explanatory models. Natl Med J India. 2014;27:198–201. [PubMed] [Google Scholar]
- 13.Nair MK, Leena ML, George B, Thankachi Y, Russell PS. ARSH 2: Reproductive and sexual health knowledge, attitude and practices: Comparison among boys and girls (10-24 y) Indian J Pediatr. 2013;80(Suppl 2):S199–202. doi: 10.1007/s12098-013-1139-z. [DOI] [PubMed] [Google Scholar]
- 14.Kar N, Koola MM. A pilot survey of sexual functioning and preferences in a sample of English-speaking adults from a small South Indian town. J Sex Med. 2007;4:1254–61. doi: 10.1111/j.1743-6109.2007.00543.x. [DOI] [PubMed] [Google Scholar]
- 15.Kendurkar A, Kaur B, Agarwal AK, Singh H, Agarwal V. Profile of adult patients attending a marriage and sex clinic in India. Int J Soc Psychiatry. 2008;54:486–93. doi: 10.1177/0020764008090795. [DOI] [PubMed] [Google Scholar]
- 16.Kumar S, Murarka S, Mishra VV, Gautam AK. Environmental & lifestyle factors in deterioration of male reproductive health. Indian J Med Res. 2014;140(Suppl S1):29–35. [PMC free article] [PubMed] [Google Scholar]
- 17.Pendharkar S, Mattoo SK, Grover S. Sexual dysfunctions in alcohol-dependent men: A study from North India. Indian J Med Res. 2016;144:393–9. doi: 10.4103/0971-5916.198681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Venkatesh K, Mattoo SK, Grover S. Sexual dysfunction in men seeking treatment for opioid dependence: A study from India. J Sex Med. 2014;11:2055–64. doi: 10.1111/jsm.12588. [DOI] [PubMed] [Google Scholar]
- 19.Dan A, Chakraborty K, Mondal M, Neogi R, Chatterjee S, Makhal M, et al. Erectile dysfunction in patients with diabetes mellitus: Its magnitude, predictors and their bio-psycho-social interaction: A study from a developing country. Asian J Psychiatr. 2014;7:58–65. doi: 10.1016/j.ajp.2013.10.012. [DOI] [PubMed] [Google Scholar]
- 20.Rajkumar RP, Kumaran AK. Depression and anxiety in men with sexual dysfunction: A retrospective study. Compr Psychiatry. 2015;60:114–8. doi: 10.1016/j.comppsych.2015.03.001. [DOI] [PubMed] [Google Scholar]
- 21.Grover S, Avasthi A, Gupta S, Dan A, Neogi R, Behere PB, et al. Comorbidity in patients with Dhat syndrome: A nationwide multicentric study. J Sex Med. 2015;12:1398–401. doi: 10.1111/jsm.12899. [DOI] [PubMed] [Google Scholar]
- 22.Dhikav V, Aggarwal N, Gupta S, Jadhavi R, Singh K. Depression in Dhat syndrome. J Sex Med. 2008;5:841–4. doi: 10.1111/j.1743-6109.2007.00481.x. [DOI] [PubMed] [Google Scholar]
- 23.Grover S, Gupta S, Mehra A, Avasthi A. Comorbidity, knowledge and attitude towards sex among patients with Dhat syndrome: A retrospective study. Asian J Psychiatr. 2015;17:50–5. doi: 10.1016/j.ajp.2015.07.002. [DOI] [PubMed] [Google Scholar]
- 24.Kumar J, Bhatia T, Kapoor A, Ranjan P, Srivastava A, Sinha A, et al. Erectile dysfunction precedes and is associated with severity of coronary artery disease among Asian Indians. J Sex Med. 2013;10:1372–9. doi: 10.1111/jsm.12041. [DOI] [PubMed] [Google Scholar]
- 25.Avasthi A, Grover S, Kaur R, Prakash O, Kulhara P. Impact of nonorganic erectile dysfunction on spouses: A study from India. J Sex Med. 2010;7:3666–74. doi: 10.1111/j.1743-6109.2009.01647.x. [DOI] [PubMed] [Google Scholar]
- 26.Corona G, Lee DM, Forti G, O’Connor DB, Maggi M, O’Neill TW, et al. Age-related changes in general and sexual health in middle-aged and older men: Results from the European Male Ageing Study (EMAS) J Sex Med. 2010;7:1362–80. doi: 10.1111/j.1743-6109.2009.01601.x. [DOI] [PubMed] [Google Scholar]
- 27.Teles AG, Carreira M, Alarcão V, Sociol D, Aragüés JM, Lopes L, et al. Prevalence, severity, and risk factors for erectile dysfunction in a representative sample of 3,548 Portuguese men aged 40 to 69 years attending primary healthcare centers: Results of the Portuguese erectile dysfunction study. J Sex Med. 2008;5:1317–24. doi: 10.1111/j.1743-6109.2007.00745.x. [DOI] [PubMed] [Google Scholar]
- 28.Verma KK, Khaitan BK, Singh OP. The frequency of sexual dysfunctions in patients attending a sex therapy clinic in North India. Arch Sex Behav. 1998;27:309–14. doi: 10.1023/a:1018607303203. [DOI] [PubMed] [Google Scholar]
- 29.Kant S, Misra P, Gupta S, Goswami K, Krishnan A, Nongkynrih B, et al. The Ballabgarh health and demographic surveillance system (CRHSP-AIIMS) Int J Epidemiol. 2013;42:758–68. doi: 10.1093/ije/dyt055. [DOI] [PubMed] [Google Scholar]
- 30.WHO. International Classification of Diseases. World Health Organization. [Last accessed on 2017 Mar 31]. Available from: http://www.who.int/classifications/icd/en/
- 31.Hyde Z, Flicker L, Hankey GJ, Almeida OP, McCaul KA, Chubb SA, et al. Prevalence and predictors of sexual problems in men aged 75-95 years: A population-based study. J Sex Med. 2012;9:442–53. doi: 10.1111/j.1743-6109.2011.02565.x. [DOI] [PubMed] [Google Scholar]
- 32.Moreira ED, Jr, Hartmann U, Glasser DB, Gingell C GSSAB Investigators Group. A population survey of sexual activity, sexual dysfunction and associated help-seeking behavior in middle-aged and older adults in Germany. Eur J Med Res. 2005;10:434–43. [PubMed] [Google Scholar]


