Abstract
Background:
The estimated incidence of TB in India was approximately 28,00,000 as per the Global TB report 2017. This accounts for a quarter of the world's TB (Tb) cases. National strategic plan, is a programme which aims at the elimination of Tb by 2018. The programme is crafted in line with other health sector strategies and global efforts, such as the draft National Health Policy 2015, World Health Organization's (WHO) End TB Strategy and the Sustainable Development Goals (SDGs) of the United Nations (UN). Key strategies under National Strategic plan: Private sector engagement, active case finding, drug resistant Tb case management, addressing social determinants including nutrition, robust surveillance system, community engagement and multisectoral approach.
Methods:
In March 2018, India Tb report was released by RNTCP. An analysis of the report is done in the research article, an attempt to take forward end Tb strategy.
Result:
According to The India Tb report, 85% of new TB cases were detected, nationwide, where as 90% of new cases were detected in Hyderabad, during the same time period. Tuberculosis (Tb) notification rate (per 100 000 population), in India is 138, where as in Hyderabad district of Telengana it is 100. Both Public and private sector Tb case notification rate, of Hyderabad district was less than that of India (90,10). 6% of Tb cases were paediatric cases both Hyderabad and Nationwide. HIV status was known in 66% cases, in India and 67% in Hyderabad district of Telengana.
Keywords: Revised National Tuberculosis Control Program, tuberculosis Hyderabad, tuberculosis report
Introduction
One fifty years ago, Virchow recognised tuberculosis(Tb) a social disease. Since then, Koch's discovery of the bacillus and the discovery of streptomycin and other antimicrobials provided humankind with a means to both diagnose and treat tuberculosis. Tuberculosis is a major public health problem even after 20 years of its declaration as a global public health emergency by World Health Organization WHO. India continues to have the highest number of tuberculosis (Tb) cases in the world, according to the Global Tuberculosis Report 2017 released by World Health Organization (WHO). In 2016, there were an estimated 10.4 million new TB cases worldwide. Seven countries accounted for 64% of the total burden, with India having the maximum number of Tb patients followed by Indonesia, China, Philippines, Pakistan, Nigeria and South Africa, it. In India, an estimated 27.9 lakh patients were suffering from tuberculosis in 2016 and up to 4.23 lakh patients were estimated to have died during the year.
According to the report, Multidrug-resistant TB (MDR-TB) remains a public health crisis and a health security threat. WHO estimates that worldwide, there were 600,000 new TB cases with resistance to rifampicin—the most effective first-line drug, of which 490,000 had MDR-TB. Almost half of these cases were in India, China and the Russian Federation. The report highlighted that underreporting and under diagnosis of TB cases continue to be a challenge, especially in countries with large unregulated private sectors and weak health systems, including India.
Of the estimated 10.4 million new cases, only 6.3 million were detected and officially notified in 2016, leaving a gap of 4.1 million. India, Indonesia and Nigeria accounted for almost half of this global gap. Only one in five MDR-TB cases was started on treatment. India and China accounted for 39% of the global gap. Treatment success remains low, at 54% globally.
Tuberculosis (TB) disease kills 1.5 million per year and remains a major global health problem. Many low and middle income countries are unlikely to meet the Millennium Development Goals for reduction of TB disease prevalence and mortality. This is due in part to poorer people experiencing inequitable healthcare provision and access and suffering a disproportionate burden of morbidity and mortality from TB disease. Poverty increases TB risk and TB exacerbates poverty, affecting the most economically productive age group.
To bring down the TB burden in India, Revised National Tuberculosis Control Programme (RNTCP) is an on-going Centrally Sponsored Scheme, being implemented under the umbrella of National Health Mission. The programme was initiated from 1997, covered entire country in 2006.
RNTCP has now entered into an ambitious national strategic plan, aimed at providing - Universal access for quality diagnosis and treatment for all tuberculosis patients in the community with the target of “Reaching the Unreached”.
Objectives
To estimate the burden of the disease TB both pulmonary and extrapulmonary TB in Hyderabad district
To analyze the notification and TB treatment initiation in Nationwide
To estimate the proportion of Pediatrics’ TB and TB HIV-positive cases in Hyderabad and India.
Methods
It is estimated that about 40% of the Indian population is infected with TB bacteria, the vast majority of whom have TB rather than TB disease [Tables 1–4].
Table 1.
The World Health Organisation (WHO) TB statistics for India for 2016
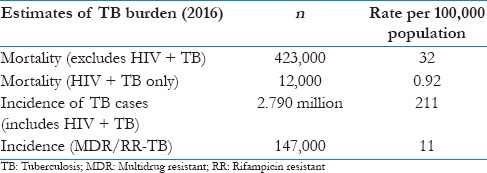
Table 4.
Paediatrics cases and HIV status
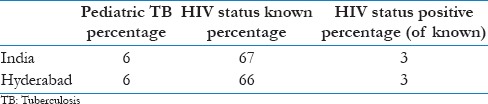
Table 2.
Site of disease pulmonary TB case and treatment initiated
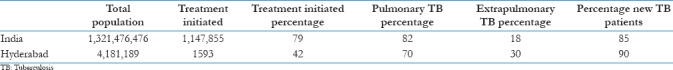
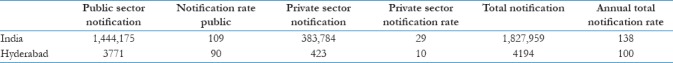
Table 3.
Tb notification rate
Most of the National TB statistics for India are collected by the government RNTCP which was launched in 1996, and then expanded across the country. In these studies, analysis of National TB report, released by RNTCP in March 2018, is done.
Results
National Tuberculosis Statistics India
India is the country with the highest burden of TB. The WHO TB statistics for India for 2016 give an estimated incidence figure of 2.79 million cases of TB for India. TB incidence is the number of new cases of active TB disease during a certain time period (usually a year).
Site of disease pulmonary tuberculosis case
Patient with TB of the lungs (with or without involvement of any extrapulmonary locations).[9] Extrapulmonary TB case – patient with TB of any organ other than the lungs, such as pleura, lymph nodes, intestines, genitourinary tract, skin, bones and joints, and meninges of the brain, diagnosed with microbiological, histological, radiological, or strong clinical evidence. According to the report, 79% cases, treatment was initiated, whereas only 42% cases, TB treatment was initiated in Hyderabad district. It is reported in Hyderabad treatment initiation for treatment initiated for pulmonary TB is 70%, which is less than the treatment initiated for India (82%).
Patient type
New tuberculosis case – a patient who has never been treated with anti-TB drugs or has been treated with anti-TB drugs for <1 month from any source recurrent TB case – patient who has been treated for TB in the past and has been declared successfully treated (cured/treatment completed) at the end of their treatment regimen.[10,11] Treatment change – patient returning after interruption or patients put on a new treatment regimen and due to failure of the current treatment regimen. About 85% of new TB cases were detected nationwide, whereas 90% of new cases were detected in Hyderabad, during the same time period.
Tuberculosis notification rate
Number of new and relapse TB cases notified in a given year, per 100,000 population. The term “notification” means that TB is diagnosed in a patient and is reported within the national surveillance system and then on to the WHO.[12] TB notification rate (per 100,000 population) in India is 138, whereas in Hyderabad district of Telangana, it is 100, in 2017. Both public and private sector TB case notification rate of Hyderabad district was less than (90, 10) that of India.
Pediatrics cases proportion and HIV status of cases
Children (age 0–14 years)[13] presenting with signs and symptoms suggestive of TB to any of the public or private health, Xpert testing was done, and cases were diagnosed. Facilities and specimens (sputum and nonsputum) were collected at the respective health facilities and transported to a centralized laboratory in each city for microscopy and Xpert testing. Nearly 6% of TB cases were pediatric cases both from Hyderabad and nationwide.
The risk of developing TB is estimated to be between 16 and 27 times greater in people living with HIV, than among those without HIV infection.[14] HIV status was known in 66% cases, in India and 67% in Hyderabad district of Telangana.
Discussion
Annual TB Report provides an update on progress of TB control activities, information on newer initiatives, policies, and guidelines developed in 2017. RNTCP is an on-going Centrally Sponsored Scheme, being implemented under the umbrella of the National Health Mission. The program was initiated from 1997, covered the entire country in 2006. The program, since then, has achieved global benchmark of case detection and treatment success and achieved millennium development goals in 2015 of halting and reversing the incidence of TB. The major initiatives taken in 2017 are expansion of daily regimen for treatment of TB across the country, scale-up of bedaquiline, conditional approval of delamanid, release of guidelines on programmatic management of drug-resistant TB (PMDT) in India, National Training of Trainers guidelines on PMDT, and introduction of medication event reminder monitor system boxes.[15] The cost-effective system is specifically designed to be used with blister-packaged TB medications, incorporates visual and audible reminders of both daily dosing and refill, compiles detailed dosing histories, and transmits these data to digital health systems to support enhanced adherence counseling and guide differentiated care.
To ensure proper TB diagnosis and case management, reduce TB transmission, and address the problems of emergence of spread of drug resistant-TB, it is essential to have complete information of all TB cases. Therefore, the Government of India declared TB a notifiable disease on May 7, 2012. All public and private health providers shall notify TB cases diagnosed and/or treated by them to the nodal officers for TB notification.[16]
Worldwide, TB disease is one of the leading causes of death among people with HIV.[17] Infection with both HIV and TB is called HIV/TB coinfection. Latent TB is more likely to advance to TB disease in people with HIV than in people without HIV. TB disease may also cause HIV to worsen.
Conclusion
While intense scientific and clinical research efforts into novel diagnostic, therapeutic, and preventative interventions have focused on TB in adults, childhood TB has been relatively neglected. However, children are particularly vulnerable to severe disease and death following infection,[18] and those with latent infection become the reservoir of disease reactivation in adulthood, fuelling the future epidemic. Hence TB notification, treatment is an integral component of TB control in India.[19]
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
I acknowledge the support of Department faculties, for facilitating the analysis.
References
- 1.Raviglione M, Krech R. Tuberculosis: Still a social disease. Int J Tuberc Lung Dis. 2011;15(Suppl 2):6–8. doi: 10.5588/ijtld.11.0158. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization. TB: A Global Emergency. WHO Report on TB Epidemic. Geneva: World Health Organization; 1994. [Last accessed on 2018 June 28]. Available from: http://www.who.int/tb/publications/1994/en/ [Google Scholar]
- 3. [Last accessed on 2018 June 28]. Available from: http://www.who.int/tb/publications/global_report/gtbr2017_annex4.pdf .
- 4. [Last accessed on 2018 June 28]. Available from: http://www.iammdelhi.com/wp-content/uploads/2017/10/Guidelines-for-PMDT-in-India-2017-Draft-050317.pdf .
- 5.World Health Organization. World Health Organization Global Tuberculosis Report 2014. World Health Organization. 2014 [Google Scholar]
- 6.Lönnroth K, Jaramillo E, Williams BG, Dye C, Raviglione M. Drivers of tuberculosis epidemics: The role of risk factors and social determinants. Soc Sci Med. 2009;68:2240–6. doi: 10.1016/j.socscimed.2009.03.041. [DOI] [PubMed] [Google Scholar]
- 7.Solar O, Irwin A. Action on the Social Determinants Social Determinants of Health Discussion Paper 2 a Conceptual Framework for Action on the Social Determinants of Health. World Health Organization. 2010 [Google Scholar]
- 8.Strategic Vision for TB Control for the Country up to 2015 Goals and Objectives for TB Control in India up to 2015. [Last accessed on 2018 June 28]. Available from: https://tbcindia.gov.in/
- 9.Chaudhuri AD. Recent changes in technical and operational guidelines for tuberculosis control programme in India – 2016: A paradigm shift in tuberculosis control. The Journal of Association of Chest Physician. 2017;5:1–9. [Google Scholar]
- 10.Treatment of Tuberculosis: Guidelines. 4th ed. Geneva: World Health Organization; 2010. [PubMed] [Google Scholar]
- 11. [Last accessed on 2018 June 28]. Available from: www.icmr.nic.in/guidelines/TB/
- 12.World Health Statistics 2018: Monitoring health for the SDGs. [Last accessed on 2018 June 28]. Available from: http://www.who.int/healthinfo/indicators/2015/chi_2015_45_tb_notification.pdf .
- 13.Raizada N, Khaparde SD, Salhotra VS, Rao R, Kalra A, Swaminathan S, et al. Accelerating access to quality TB care for pediatric TB cases through better diagnostic strategy in four major cities of India. PLoS One. 2018;13:e0193194. doi: 10.1371/journal.pone.0193194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pawlowski A, Jansson M, Sköld M, Rottenberg ME, Källenius G. Tuberculosis and HIV co-infection. PLoS Pathog. 2012;8:e1002464. doi: 10.1371/journal.ppat.1002464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liu X, Blaschke T, Thomas B, De Geest S, Jiang S, Gao Y, et al. Usability of a medication event reminder monitor system (MERM) by providers and patients to improve adherence in the management of tuberculosis. Int J Environ Res Public Health. 2017;14:pii: E1115. doi: 10.3390/ijerph14101115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. [Last accessed on 2018 June 28]. Available from: http://www.who.int/healthinfo/en/
- 17.Crook AM, Turkova A, Musiime V, Bwakura-Dangarembizi M, Bakeera-Kitaka S, Nahirya-Ntege P, et al. Tuberculosis incidence is high in HIV-infected African children but is reduced by co-trimoxazole and time on antiretroviral therapy. BMC Med. 2016;14:50. doi: 10.1186/s12916-016-0593-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tsai KS, Chang HL, Chien ST, Chen KL, Chen KH, Mai MH, et al. Childhood tuberculosis: Epidemiology, diagnosis, treatment, and vaccination. Pediatr Neonatol. 2013;54:295–302. doi: 10.1016/j.pedneo.2013.01.019. [DOI] [PubMed] [Google Scholar]
- 19.Newton SM, Brent AJ, Anderson S, Whittaker E, Kampmann B. Paediatric tuberculosis. Lancet Infect Dis. 2008;8:498–510. doi: 10.1016/S1473-3099(08)70182-8. [DOI] [PMC free article] [PubMed] [Google Scholar]


