Abstract
Background:
Accredited social health activist (ASHA) has the pivotal role to play in the whole design and strategy of national rural health mission (NRHM). The performance of ASHA is, therefore, critical for the success of NRHM and hence of the health improvement strategy of the government of India.
Objectives:
(1) To evaluate the knowledge and performance of ASHA. (2) To assess the factors affecting these two attributes of ASHA.
Methods:
Ten ASHAs were randomly selected from each of the eight administrative blocks of Anand District. Thus, a total of 80 ASHAs participated in the study. Knowledge of ASHAs was assessed by computing knowledge score which included 15 questions, while the performance was assessed through performance score which included 17 indicators. Each ASHA was ranked “Poor,” “Average,” and “Good” based on the performance score.
Results:
Out of 80 ASHAs, 49 (61%) were in the age group of 30–40 years. Majority of ASHAs(68%) belonged to other backward class (OBC). 73 (91%) ASHAs had education up to at least secondary level. 65 (81%) ASHAs were working for more than 4 years. About 84% of ASHAs had knowledge score between 12 and 15. Nearly 51% of ASHAs ranked average in performance, while 49% ranked poor. None of the ASHAs ranked good. Knowledge score and performance ranks were not associated with age, caste, education, and duration of service of ASHAs. Performance ranks were found to be significantly associated only with time lapse since the last training received.
Conclusion:
To strengthen the grass root cader of ASHAs, their evaluation should be conducted regularly. Additional refresher training should be provided to ASHAs with low knowledge and performance scores so that the engagement of rural community with the health system can be improved.
Keywords: Accredited social health activist, evaluation, knowledge, performance
Introduction
India is the 2nd largest populous country in the world after China with a population of 1210 million[1] and an equal volume of public health problems. About 69% of the country's population lives in rural areas which comprise almost three-quarters of the population.
However, in these areas, utilization of basic health services has remained poor though there has been an increase in the public expenditure on the provision of primary health care. To meet this challenge, a new band of community-based functionaries, named as accredited social health activist (ASHA) was proposed under national rural health mission (NRHM), an ambitious initiative of the central government of India, to fulfil its promise on inclusive growth. ASHA has the pivotal role to play in the whole design and strategy of this mission. She acts as a link between the community and the rural health system.[2] She is the first port of call for any health-related demands of deprived sections of the population, especially women and children, who find it difficult to access health services.[2] She also acts as a promoter of good health practices, health educator, and a counselor for women in reproductive age group. The performance of ASHA is, therefore, critical for the success of NRHM and hence of the health improvement strategy of Government of India. Developing and utilizing the potentials of ASHAs require assessment of their knowledge and functions, knowing their deficiencies and difficulties in service provision and how these can be corrected so that their efficiency is augmented. The present study is an attempt to evaluate their knowledge and performance related to their role as a link worker and to assess the factors affecting these two attributes.
Materials and Methods
A community-based cross-sectional study was conducted among ASHAs working in Anand District of Gujarat. Ten ASHAs were randomly selected from each of the eight administrative blocks of the district to have equal representation from all blocks. Thus, a total of 80 ASHAs participated in the study. After seeking a written informed consent, relevant sociodemographic information was collected from the participants through pretested structured questionnaire. Knowledge of ASHAs was assessed by computing knowledge score which included 15 questions related to antenatal care, common illnesses, immunization, mosquito breeding, and other health aspects. For each correct response, a score of one was given. Thus, an ASHA can score maximum of 15 and minimum of zero. While performance was assessed through performance score which included 17 indicators, such as blood smear preparation, referral services, sputum collection, provision of “Directly Observed Treatment Short (DOTS)” course to tuberculosis patients, motivating rural community for sanitary latrines, and their participation in governmental programs. For each indicator, ranges for “Poor,” “Average,” and “Good” work were set in quantifiable figures. The scores of 1, 2, and 3 were assigned for the “Poor,” “Average,” and “Good” performance, respectively. All the scores were summed up to reach a final score, which would be minimum of 17 and maximum of 51. Again, each ASHA was ranked “Poor,” “Average” and “Good” based on this final performance score.
Data collecte0d was analyzed using (Stata 14.2, StataCorp LLC, Texas, USA) software. Proportions and percentages were computed for categorical data. Statistical significance was tested using χ2 test, Fisher's exact test, t-test, and analysis of variance.
The study was approved by the Human Research Ethics Committee of H M Patel Center for Medical Care and Education.
Results
Mean age of 80 ASHAs who participated in our study was 32.3 years ± 5.9, with 49 (61%) in the age group of 30–40 years. 54 (68%) ASHAs belonged to other backward class (OBC), and 77 (96.3%) were married. Most of them (90%) were working as homemaker. Moreover, 73 (91%) ASHAs had education up to at least 8th standard, and 65 (81%) were working for more than 4 years. Only 6% of ASHAs had monthly household income of <1000 rupees. While 47 (58.8%) ASHAs received 1000–2000 Rs as monthly incentive, 2 (2.5%) received incentive <500 Rs, and 3 (3.8%) received incentive more than 2500 Rs. The majority (74%) of the ASHAs had beneficiary population of 1000–1500. 9 (11%) ASHAs spent <3 h for their work, while 20 (25%) worked 3–5 h, and 52 (64%) for more than 5 h.
All ASHAs, except one, had received modular training. Out of these 79 ASHAs, 54 (68%) received it within 6 months of the interview, while rest 25 (32%) beyond 6 months. Mean knowledge score achieved by the participants was 12.8 ± 1.5, with a range of 9–15. 67 (84%) ASHAs got knowledge score more than 11. Age, caste, education, period of service, and time lapse since last training were not found to be associated with knowledge score (P > 0.05). Regarding performance assessment, 51% of ASHAs ranked average in performance while 49% ranked poor. None of the ASHAs ranked good. Only time lapse since the last training was found to be significantly related to the performance of ASHAs (P < 0.05).
Discussion
The study evaluated ASHAs from different blocks of Anand District for their knowledge and work performance. Knowledge and work performance as dependent variables were also correlated with a number of different independent socioeconomic and demographic variables.
As per the guidelines of NRHM for ASHA, she should be primarily a woman resident of the village, preferably in the age group of 25–45 years.[2] In our study, only 7 (8.8%) ASHAs had age outside this range, 2 (2.5%) below 25 years and 5 (6.3%) above 45 years. Thirty-two (40%) ASHAs were in age group of 25–35 years. An eight states study by the national health systems resource center (NHSRC) showed that in all states, about 60% of ASHAs were in 24–35 years age group, except in Kerala where only 35% belonged to this age group.[3] In Rajasthan and Jharkhand, the remaining were mainly in the 20–24 years age group, whereas in Kerala, Assam, Orissa, Bihar, and West Bengal the majority of the remainder were above 36 years of age.[3] A study conducted by State Institute of Health and Family Welfare (SIHFW), Lucknow in Uttar Pradesh found that 66.7% ASHAs were between the age group of 25 and 34 years.[4] Shrivastava and Shrivastava have reported that 48% of ASHAs were below the age of 25 years in their Maharashtra based study with a range of 17–34 years.[5] In a study conducted in Gujarat, the mean age of ASHAs was found to be 27.8 years with 35% of them having age <25 years.[6]
In our study, the majority of ASHAs (68%) were from OBC and only 10% belonged to general category. While 16% ASHAs were from scheduled castes (SC) and 6% from scheduled tribes (ST). A study done in Nagaland revealed that all ASHAs included in the study were from ST.[7] This notable difference between the two states may be due to socioeconomic variations. On the contrary, SIHFW study found that as much as 35% ASHAs came from general category, 40% from OBC, 23% from SC, and only 2% from ST.[4] A study conducted in Cuttack, Orissa, the caste composition revealed that the ASHAs from SC and ST together constitute more than half of the total sample, while those belonging to general castes and OBC were 26% and 21%, respectively.[8] In a study done in Rajasthan, 18% ASHAs belonged to SC, 14% to ST, and 38% to OBC.[9]
As per the guidelines of NRHM, ASHA should be married, widowed, or divorced.[2] In our study, 96% ASHAs were married, while rest were either widow or divorcee. However, in Nagaland study, as high as 12% ASHAs were unmarried.[7] Similarly, in Chhattisgarh, 9% ASHAs were not married.[10] Another Gujarat based study found 90% ASHAs to be married.[6]
NRHM guideline directs that ASHA worker should be a literate woman with formal education up to the eighth standard.[11] This norm may be relaxed only if a suitable person with this qualification is not available.[11] Studies conducted in different states have noted a significant variation in educational status of ASHAs across the country. In this study, only 9% of ASHAs had education lower than 8th standard. Rest 91% were educated up to 8th standard and above. About 10% of ASHAs were Graduate. In NHSRC study, 27% of ASHAs in Jharkhand, 37% of ASHAs in Orissa, 25% in Andhra Pradesh, and 11% in Bihar were found to be educated lower than 8th standard.[3] This proportion was further higher in tribal districts of these states. Thus, comparatively, ASHAs in our study were better educated. Similarly, a study done in Nagaland revealed that only 23% ASHAs were having education qualification lesser than 8th class.[7] However, a Karnataka study showed completion of 8 years of schooling in 90% of ASHAs, a proportion comparable with that of our study.[12] While in another four-state study, 28% ASHAs were educated below 8th grade in Chhattisgarh, and only 2% in Rajasthan, UP and Bihar each.[10] Shrivastava and Shrivastava found that 46% of the ASHAs were educated up to the secondary school level.[5] Similarly, a Gujarat-based study found 70% of ASHAs having secondary level of education.[6]
In our study, 58% of ASHAs had monthly household income of more than 3000 rupees, 36% between 1000 and 3000 rupees, and only 6% <1000 rupees. The figures for Karnataka study were 24%, 59%, and 17%, respectively.[12] As per the NHSRC study, ASHAs in Kerala, Orissa and Jharkhand were the poorest with household income <1000 per month in 65%, 35%, and 22% of families.[3]
ASHA is an honorary volunteer, not receiving any salary. However, she is incentivized for various health activities she conducts. Most of the states have performance-based payment. In states such as West Bengal and Rajasthan, ASHAs receive a fixed amount of 800 and 950 rupees, respectively.[3] In our study, only 3% of ASHAs were receiving <500 rupees as incentive. While 26% received 500–1000 rupees and the majority (71%) received more than 1000 rupees as an average monthly incentive. In Kerala, 24% ASHAs were getting <500 rupees, 56% between 500 and 1000 rupees, and 20% more than 1000 rupees/month.[3] While, on the one hand, 64% ASHAs were monthly paid more than 1000 rupees in Orissa, on the other hand, 27% ASHAs in Jharkhand and 20% in Bihar were getting <50 rupees as monthly incentive.[3] In AP, this incentive was <500 rupees in 57% ASHAs, and 500–1000 rupees in 43% ASHAs.[3] None of the ASHAs got more than 1000 rupees as monthly incentive.
As per NRHM norm, one ASHA will cater a population of 1000 rural people.[11] This norm can be relaxed depending on local conditions such as geographically remote, tribal, hilly or desert areas.[11] In our study, the majority (79%) of the ASHAs catered to the needs of more than 1000 population. Only 21% ASHAs had a beneficiary population of 500–1000. NHSRC study found that about 36% to 64% of ASHAs served 500–1000 population in all the states included in the study.[3] While, 60% ASHAs in WB, 44% in Orissa and Rajasthan, 42% in Kerala, 38% in Assam, 34% in Bihar, 28% in Jharkhand and 26% in AP served over 1000 population.[3] In Nagaland, 40% ASHAs covered a population of more than 1000.[7]
It is envisaged that ASHA will work only about 2–3 h per day, on 4 days/week, with a flexible work schedule.[11] In our study, 64% ASHAs worked for more than 5 h/day, 5 days a week, making it a total of more than 25 h/week, followed by 25% ASHAs who worked for 15–25 h/week, and rest 11% worked for <15 h/week. The study done by Bajpai and Dholakia revealed that, on an average, ASHAs worked for 26–28 h/week in Chhattisgarh, Rajasthan, UP, and Bihar.[10] On the contrary, in Nagaland, 45% ASHAs worked about 1–2 h daily, followed by another 21% working for 2–3 h/day.[7]
Effective training of ASHA is crucial for enhancing her role as health facilitator, health-care provider and social activist. After selection, ASHA undergoes induction modular training for 23 days intended to provide the necessary knowledge and skills to fulfil her responsibilities.
In our study, except one, all the ASHAs had taken induction training completing all the five modules. One who did not receive training was newly recruited. However, the four state study revealed that states such as Bihar, Assam, and Rajasthan have not covered 100% ASHAs, but have covered 90% or more as far as modular training is concerned.[10] These states considerably lag behind the ASHA training for module 2 onward. Similarly, NHSRC study found that 90% of ASHAs had received complete 23 days-induction training in West Bengal, 52% in Kerala, and 46% in Orissa.[3] While in Jharkhand, 46% of ASHAs had received 11 to 15 days training and 50% received <10 days training.[3]
In this study, the mean knowledge score of ASHAs was 12.8, with the majority (84%) of them scoring more than 11. In a study done in Varanasi, the mean knowledge score was found to be 2.11 on a 3-point Likert scale, with 25% ASHAs ranking poor, 39% ranking average, and 36% ranking good.[13] In our study, all ASHAs gave the correct response to the questions about “age of vaccination for the Bacille Calmette Guerin(BCG),” “treatment of snake bite,” and “exclusive breastfeeding” period. The questions wrongly answered by most of the ASHAs were about “common causes of diarrhea” and “timings of Tetanus Toxoid(TT) vaccine in the antenatal woman” for which the wrong responses were given by 75% and 44% ASHAs, respectively. In another study conducted in Rajasthan, the mean knowledge score obtained by ASHAs was found to be 8.1 out of maximum possible nine.[14] Most of the ASHAs gave incorrect answers for questions related to environmental sanitation in this study. Similarly, in Nagaland study, knowledge of ASHAs about breastfeeding and family planning was found to be good compared to that of immunization and management of diarrhea.[7] In four state study, ASHAs from Chhattisgarh obtained highest knowledge scores, while those from Bihar were the poorest achievers.[10] In Bihar, 54% of ASHAs obtained failing scores (below 70%) compared to 19% in Chhattisgarh, 23% in Rajasthan, and 33% in UP.[10] Only 5% of ASHAs from Chhattisgarh, 1% from Rajasthan, and none from the remaining two states scored above 90%.[10] A study done in Gujarat reported the mean knowledge score of the ASHAs to be 16.7 out of 34.[15] However, in this study, the investigators assessed only the knowledge about home-based newborn care. In the study done by Shrivastava and Shrivastava, all of the ASHAs were found to have correct knowledge about advising women regarding institutional deliveries, postnatal check-ups, and exclusive breastfeeding.[5] However, this study reported a poor knowledge in about 20%–40% ASHAs regarding immunization and care of child with diarrhea and respiratory tract infections. In contrast to this, Swain et al. observed that 81% of ASHAs had correct knowledge about counseling on antenatal and postnatal care, breastfeeding and immunization.[16] In another study done in Gujarat, 70% of ASHAs had poor knowledge about breastfeeding and immunization, while 86% of ASHAs had incorrect knowledge regarding newborn care.[6]
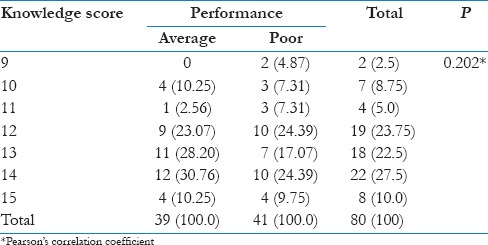
The study did not find any association of knowledge score with age, caste, education, duration of service of ASHAs, and time lapse since the last training received [Table 1]. Similarly, the performance ranks were not associated with age, caste, education, size of population served by the ASHAs, and duration of service of ASHAs [Table 2]. Study done in Varanasi noted a significant association of caste, education as well as the size of service population with performance scores of ASHAs.[13] However, in this study, performance ranks were found to be significantly associated with time lapse since the last training received [Table 2]. This emphasizes the importance of periodic refresher training of ASHAs for improving their performance. Mony and Raju also felt the need of training of ASHAs in their study done in Karnataka to fulfil the objectives of the program.[17] A study done by Kohli et al. reported a poor performance by ASHAs regarding antenatal care and referral services.[18] They too recommended identification of reasons for such performance and skill-based training to improve it. Moreover, in our study, no correlation was observed between knowledge scores and performance scores achieved by ASHAs, as depicted in Table 3.
Table 1.
Distribution of Accredited Social Health Activists according to background characteristics and knowledge scores
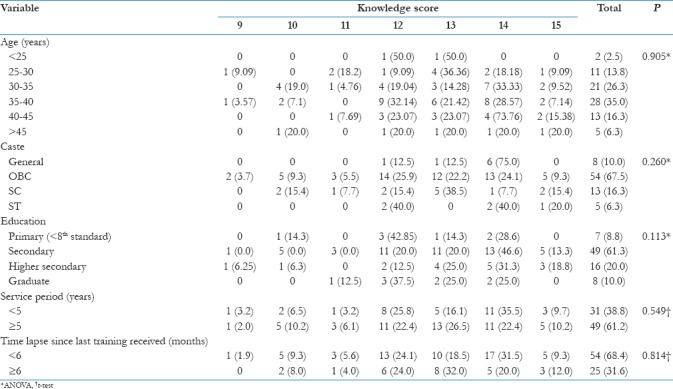
Table 2.
Distribution of Accredited Social Health Activists according to background characteristics and performance ranks
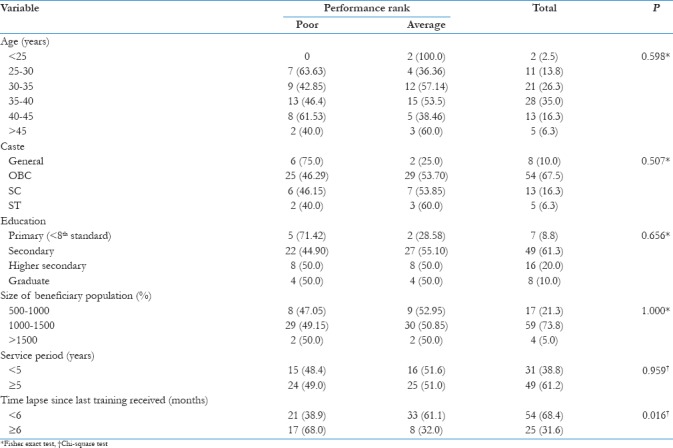
Table 3.
Correlation between knowledge and performance scores
Conclusion
Evaluation of ASHAs should be conducted regularly to strengthen this grassroot level cader of link workers and social activists. Additional refresher training should be provided to ASHAs with low knowledge and performance scores so that the engagement of rural community with the health system can be improved. Further qualitative studies can be conducted to understand the reasons for the difference in performances of ASHAs who have undergone similar kind of training.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.New Delhi: Government of India; [Last accessed on 2017 May 02]. Office of Registrar General & Census Commissioner, Ministry of Home Affairs. Available from: http://www.censusindia.gov.in/2011-prov-results/paper2/data_files/india/Rural_Urban_2011.pdf . [Google Scholar]
- 2.National Health Mission. About Accredited Social Health Activist (ASHA). Ministry of Health and Family Welfare, Government of India. [Last accessed on 2017 May 02]. Available from: http://www.nrhm.gov.in/communitisation/asha/about-asha.html .
- 3.New Delhi: National Institute of Health and Family Welfare; 2010-2011. [Last accessed on 2017 May 02]. National Health Systems Resource Centre. ASHA. Which Way Forward? Evaluation of ASHA Programme. Available from: http://www.nhsrcindia.org/index.php?option=com_content&view=article&id=286 . [Google Scholar]
- 4.Lucknow, Uttar Pradesh State Institute of Health & Family Welfare; 2007-2008. [Last accessed on 2017 May 04]. State Institute of Health & Family Welfare. Assessment of the functioning of ASHA under NRHM in Uttar Pradesh. Available from: http://www.nihfw.org/doc/RAHI.I%20Reports/Lucknow/LUKNOW.pdf . [Google Scholar]
- 5.Shrivastava SR, Shrivastava PS. Evaluation of trained accredited social health activist (ASHA) workers regarding their knowledge, attitude and practices about child health. Rural Remote Health. 2012;12:2099. [PubMed] [Google Scholar]
- 6.Mahyavanshi DK, Patel MG, Kartha G, Purani SK, Nagar SS. A cross sectional study of the knowledge, attitude and practice of ASHA workers regarding child health (under five years of age) in Surendranagar district. Healthline. 2011;2:50. [Google Scholar]
- 7.Regional Resource Centre for North Eastern States, Ministry of Health and Family Welfare, Government of India. ASHA Evaluation Nagaland. 2012. [Last accessed on 2017 May 02]. Available from: http://www.rrcnes.gov.in/study_report/ASHA%20Evaluation_Nagaland_Report.pdf .
- 8.National Institute of Applied Human Research and Development, Cuttack, Orissa. Rapid Appraisal of Functioning of ASHA under NRHM in Cuttack, Orrisa. 2007-2008. [Last accessed on 2017 May 04]. Available from: http://www.nihfw.org/doc/RAHI.I%20Reports/Cuttack/CUTTACK.pdf .
- 9.Centre for Operations Research and Training, Vadodara. Assessment of ASHA and Janani Suraksha Yojana in Rajasthan. 2007. [Last accessed on 2017 May 04]. Available from: http://www.cortindia.in/RP%5CRP.2007-0302.pdf .
- 10.Bajpai N, Dholakia RH. Improving the Performance of Accredited Social Health Activists in India. Working Paper No. South Asia, Columbia University: Columbia Global Centers; May. 2011. [Last accessed on 2017 May 02]. Available from: http://www.globalcenters.columbia.edu/files/cgc/pictures/Improving_the_Performance_of_ASHAs_in_India_CGCSA_Working_Paper_1.pdf .
- 11.National Health Mission. State Health Society, Health and Family Welfare Department. Government of Gujarat. Guidelines on Accredited Social Health Activists (ASHA) [Last accessed on 2017 May 04]. Available from: https://www.nrhm.gujarat.gov.in/images/pdf/ASHA_Guidelines.pdf .
- 12.Fathima FN, Raju M, Varadharajan KS, Krishnamurthy A, Ananthkumar SR, Mony PK, et al. Assessment of ‘accredited social health activists’-a national community health volunteer scheme in Karnataka state, India. J Health Popul Nutr. 2015;33:137–45. [PMC free article] [PubMed] [Google Scholar]
- 13.Mohapatra A, Mohapatra SC. Intraorganizational human resource auditing of ASHAs in Harahua block of Varanasi. J Public Health Epidemiol. 2013;5:237–42. [Google Scholar]
- 14.National Institute of Health and Family Welfare. Assessment of Performance Based Incentive System for ASHA Sahyogini in Udaipur District, Rajasthan. Udaipur, Rajasthan: R.N.T. Medical College. [Last accessed on 2017 May 02]. Available from: http://www.nihfw.org/pdf/RAHI-II%20Reports/UDAIPUR.pdf .
- 15.Bansal SC, Nimbalkar SM, Shah NA, Shrivastav RS, Phatak AG. Evaluation of knowledge and skills of home based newborn care among accredited social health activists (ASHA) Indian Pediatr. 2016;53:689–91. doi: 10.1007/s13312-016-0911-3. [DOI] [PubMed] [Google Scholar]
- 16.Swain S, Swain P, Nair KS, Dhar N, Gupta S, Nandan D. A rapid appraisal of functioning of ASHA under NRHM in Orissa. Health Popul Perspect Issues. 2008;31:73–9. [Google Scholar]
- 17.Mony P, Raju M. Evaluation of ASHA programme in Karnataka under the national Rural health mission. BMC Proc. 2012;6(Suppl 5):12. [Google Scholar]
- 18.Kohli C, Kishore J, Sharma S, Nayak H. Knowledge and practice of accredited social health activists for maternal healthcare delivery in Delhi. J Family Med Prim Care. 2015;4:359–63. doi: 10.4103/2249-4863.161317. [DOI] [PMC free article] [PubMed] [Google Scholar]


