Abstract
Background:
Data of musculoskeletal manifestations of tuberculosis (TB) are limited to case reports, series, or retrospective studies. Therefore, we conducted this study to create awareness among doctors about musculoskeletal manifestations of TB.
Materials and Methods:
This was a prospective observational study conducted at a referral TB Hospital in North India in September and October 2016. The aim of our study was to study musculoskeletal manifestations of TB. We included patients who had active TB as per the World Health Organization 2010 criteria. Patients with other chronic illnesses were excluded. A detailed history, examination, and appropriate investigations (blood, urine, serological, and radiological) of the 100 consecutive patients fulfilling the inclusion criteria were recorded.
Results:
The mean age of patients was 32.16 ± 12.93 years. Male-to-female ratio was 43:57. The mean duration of disease was 6.85 ± 8.83 months. Of the 100 patients, 60 (60%) had pulmonary TB. The mean duration of antitubercular therapy was 1.79 ± 1.34 months. Fibromyalgia was classified in 21 (21%) patients, polyarthralgia was seen in 9 (9%), Pott's spine in 7 (7%), osteomyelitis in 4 (4%), and scleritis in 2 (2%) patients. Uveitis, tenosynovitis, erythema induratum, subcutaneous abscess, and dactylitis were seen in 1 (1%) patient each. In 21 patients who had fibromyalgia, 11 developed fibromyalgia with the second episode of TB amounting to 60.75% patients.
Conclusion:
This is the first prospective study to look at the musculoskeletal manifestations of TB. Patients with active TB were found to have various rheumatological manifestations.
Keywords: Fibromyalgia, osteomyelitis, Poncet's, Pott's spine, rheumatology, Tuberculosis, uveitis
Introduction
Tuberculosis (TB) infection is a major public health problem around the world. In recent years, there has been a rise in the prevalence of TB in many parts of Europe due to migration of people from countries that are endemic with TB and various socioeconomic factors. The musculoskeletal system is involved in 1%–3% of the cases, and of these only 50% involve the extraspinal bones and soft tissues.
The association of TB and rheumatologic diseases is bidirectional.[1,2,3] In this association, Mycobacterium tuberculosis (MTB) can directly infect the musculoskeletal system. Further, patients with rheumatologic diseases are predisposed to develop TB due to the immunosuppressive state, the disease itself, or drug-induced immunosuppression.
Direct manifestations of TB musculoskeletal involvement include spondylitis, septic arthritis, osteomyelitis, myositis, bursitis, subcutaneous abscesses, or tenosynovitis.[3] Immunologic reactions such as reactive arthritis (Poncet's), erythema nodosum, erythema induratum, or secondary amyloidosis may also manifest as a tubercular rheumatism.[4,5,6,7] In addition, drugs used in the management of TB can also lead to arthropathy or tendinopathy, especially with the use of rifampin or fluoroquinolones,[8,9,10] drug-induced lupus (DILE) by isoniazid or rifampin,[11,12] and arthralgias and gout due to pyrazinamide.[13] Secondary fibromyalgia or chronic pain syndrome may be a manifestation of TB.
These rheumatological or musculoskeletal manifestations may be the presenting symptoms of TB. TB is a common illness in developing country like India, and if not detected at an early stage, it may lead to increased morbidity and mortality. Thus, it is important to have knowledge about these musculoskeletal manifestations for the treating doctors. Data of musculoskeletal manifestations of TB are limited to case reports, series, or retrospective study. To our knowledge, there is no prospective study addressing this issue. Therefore, we conducted this study to create awareness among doctors about musculoskeletal manifestations of TB.
Materials and Methods
It was a prospective observational study which was conducted at Rajan Babu Tuberculosis Hospital, Kingsway Camp, New Delhi, in the months of September and October 2016. Consecutive patients from outpatient and inpatient department of pulmonology were recruited irrespective of the duration of antitubercular therapy.
We included patients who were a confirmed case of active TB as per World Health Organization 2010 criteria.[14] Patients with chronic illness except TB were excluded.
Patients fulfilling the inclusion criteria were recruited for the study. A detailed history, examination, and appropriate investigations (blood, urine, and radiological) of the 100 consecutive patients fulfilling the inclusion criteria were recorded.
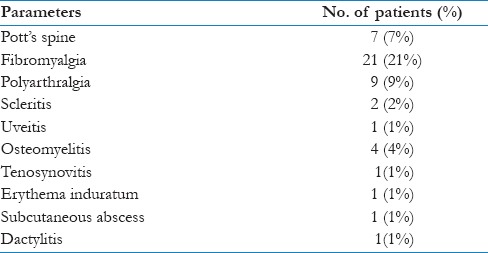
Musculoskeletal manifestations of TB which were looked at in patients are summarized in Table 1.
Table 1.
Musculoskeletal manifestations of tuberculosis

Diagnosis of Poncet's disease was made clinically by oligo or polyarticular involvement in the presence of TB.[15,16] The classification of fibromyalgia was made by American College of Rheumatology 1990[17] classification criteria for fibromyalgia.
The patient was classified as gout according to American College of Rheumatology–European League Against Rheumatism 2015 classification criteria for Gout.[18]
The patient was classified as DILE in the presence of lupus-like symptoms (commonly fever, musculoskeletal involvement, and serositis) which was temporally related to continuous drug exposure (>1 month) which resolves with cessation of the offending drug and the patient may have positive antinuclear antibody and anti-histone antibodies with negative antibodies to dsDNA.[19]
The diagnosis of the rest of musculoskeletal manifestations was clinical, microbiological, radiological, histopathological, joint aspiration, opthalmological, or serological depending on the manifestation.
Statistical analysis
Age and duration of disease are represented as mean ± standard deviation.
Results
The prospective study was carried out at Rajan Babu Tuberculosis Hospital. Consecutive patients who presented to the inpatient and outpatient department of respiratory and TB department were recruited. Those patients who fulfilled the inclusion and exclusion criteria were included in the study. The baseline characteristics of the study cohort are shown in Table 2. Many patients were found to have rheumatological manifestations. Table 3 shows rheumatological manifestations in patients with TB.
Table 2.
Baseline characteristic of the study group

Table 3.
Rheumatological manifestations in patients with tuberculosis (n=100)
Rheumatological manifestations such as septic arthritis, DILE, Poncet's arthritis, tendinopathy, amyloidosis, gout, erythema nodosum, and myositis were not seen in any patient.
Fibromyalgia was classified in 21 (21%) patients. Of these 21 patients, 11 patients developed fibromyalgia in patients with second episode of TB amounting to 60.75% patients developing fibromyalgia who had second episode of TB. Of these 21 patients of fibromyalgia, 12 were female.
Discussion
Our study is the first prospective study of its kind to look at rheumatological manifestations in patients with active TB. Fibromyalgia is the second most common rheumatic disease. The prevalence is from 2% to 8% of the population depending on the diagnostic criteria used.[20] Fibromyalgia may also occur with other chronic diseases such as osteoarthritis, rheumatoid arthritis, and lupus. Prevalence of fibromyalgia ranges from 10% to 30%[21] in patients with chronic rheumatic disorders. TB is a chronic infection. In our patients with active TB, fibromyalgia was seen in 21% of patients with 60.75% with second episode of TB developing fibromyalgia. There has been no study which has evaluated the incidence or prevalence of fibromyalgia in patients with TB.
Pott's spine is a common form of extrapulmonary TB. Around half the cases of skeletal TB are Pott's spine. In total, 1%–2% of total TB cases are attributable to Pott's disease.[22] In our cohort, Pott's spine was seen in 7% of patients with 2% having only Pott's spine and the remaining 5% having pulmonary TB with Pott's spine.
Polyarthralgia was observed in 9 (9%) of our study cohort. Arthralgia can be caused by antitubercular drugs as isoniazid[23] and pyrazinamide.[23] All our patients who developed polyarthralgia were on isoniazid or pyrazinamide.
Osteomyelitis was seen in 4 (4%) patients. Tubercular osteomyelitis occurs in 1%–2% of all cases of TB and 10% of all cases of extrapulmonary TB.[24]
Scleritis was seen in 2 (2%) of our patients. Donahue[25] found 1.4% ocular TB in 10,000 patients with primary pulmonary TB in the United States. In a study recently reported at Srilanka,[26] of the total of 2130 patients with TB, ocular TB was diagnosed in 23 patients among whom episcleritis and inflammatory scleral nodule were observed in 1 patient each.
Uveitis, dactylitis, tenosynovitis, subcutaneous abscess, and erythema induratum were seen in 1 (1%) each in patients with active TB.
However, a recent study from Japan by Wakabayashi et al.[27] showed an increasing frequency of tuberculous uveitis. Of 189 referred uveitis cases, 6.9% were found to have tuberculous uveitis. According to a study by Mercanti et al.,[28]7% of patients with uveitis in Italy had presumed tuberculous etiology. In India, where pulmonary TB is endemic, TB was the etiology of uveitis in 5.6%[16]–10.1%.[29]
Dactylitis was seen in 1 (1%) of our patient. As shown in studies, 7% of children with pulmonary TB may develop dactylitis.
In our study cohort, tubercular tenosynovitis was seen in 1 (1%) patient. Our patient developed tenosynovitis of the extensor tendons of right wrist.
Subcutaneous abscess and erythema induratum were seen in 1 (1%) patient, who developed breast abscess. The overall incidence of cutaneous TB among all forms of TB is approximately 1%–2%. The nodules are usually seen around the ankles.[30]
Limitation of our study: It was a single-center study with relatively small number of subjects. Patients with extrapulmonary TB were quite less when compared with pulmonary TB.
Conclusion
This is the first prospective study to look at musculoskeletal manifestations of TB. Patients with active TB were found to have secondary fibromyalgia (21%) and polyarthralgia (9%). Other manifestations that were seen were Pott's spine, dactylitis, scleritis, uveitis, tenosynovitis, erythema induratum, and subcutaneous abscess.
Financial support and sponsorship
It was a self funded project
Conflicts of interest
There are no conflicts of interest.
References
- 1.Rothschild BM, Martin LD, Lev G, Bercovier H, Bar-Gal GK, Greenblatt C, et al. Mycobacterium tuberculosis complex DNA from an extinct bison dated 17,000 years before the present. Clin Infect Dis. 2001;33:305–11. doi: 10.1086/321886. [DOI] [PubMed] [Google Scholar]
- 2.Santos AL, Roberts CA. A picture of tuberculosis in young Portuguese people in the early 20th century: A multidisciplinary study of the skeletal and historical evidence. Am J Phys Anthropol. 2001;115:38–49. doi: 10.1002/ajpa.1054. [DOI] [PubMed] [Google Scholar]
- 3.Kramer N, Rosenstein ED. Rheumatologic manifestations of tuberculosis. Bull Rheum Dis. 1997;46:5–8. [PubMed] [Google Scholar]
- 4.Southwood T, Gaston JSH. The molecular basis of Poncet's disease? Br J Rheumatol. 1990;29:491. doi: 10.1093/rheumatology/29.6.491. [DOI] [PubMed] [Google Scholar]
- 5.Chowdhary V, Aggarwal A, Misra R. Multifocal tuberculous dactylitis in an adult. J Clin Rheumatol. 2001;8:35–7. doi: 10.1097/00124743-200202000-00008. [DOI] [PubMed] [Google Scholar]
- 6.El-Hennawy AS, Goldstein M, Nicastri A. Renal amyloidosis secondary to tuberculosis of cecum. Nephron. 2002;92:708–10. doi: 10.1159/000064091. [DOI] [PubMed] [Google Scholar]
- 7.Khaliq Y, Zhanel GG. Fluoroquinolone-associated tendinopathy: A critical review of the literature. Clin Infect Dis. 2003;36:1404–10. doi: 10.1086/375078. [DOI] [PubMed] [Google Scholar]
- 8.Lipsky BA, Baker CA. Fluoroquinolone toxicity profiles: A review focusing on newer agents. Clin Infect Dis. 1999;28:352–64. doi: 10.1086/515104. [DOI] [PubMed] [Google Scholar]
- 9.Siegal FP, Eilbott D, Burger H, Gehan K, Davidson B, Kaell AT, et al. Dose-limiting toxicity of rifabutin in AIDS-related complex: Syndrome of arthralgia/arthritis. AIDS. 1990;4:433–41. doi: 10.1097/00002030-199005000-00009. [DOI] [PubMed] [Google Scholar]
- 10.Berning SE, Iseman M. Rifamycin-induced lupus syndrome. Lancet. 1997;349:1521–2. doi: 10.1016/S0140-6736(05)62102-2. [DOI] [PubMed] [Google Scholar]
- 11.Shakoor N, Michalska M, Harris CA, Block JA. Drug-induced systemic lupus erythematosus associated with etanercept therapy. Lancet. 2002;359:579–80. doi: 10.1016/S0140-6736(02)07714-0. [DOI] [PubMed] [Google Scholar]
- 12.Scott JT. Drug induced gout. Baillieres Clin Rheumatol. 1991;5:39–60. doi: 10.1016/s0950-3579(05)80295-x. [DOI] [PubMed] [Google Scholar]
- 13.Sanchez-Albisua I, Vidal ML, Joya-Verde G, del Castillo F, de Jose MI, Garcia-Hortelano J. Tolerance of pyrazinamide in short course chemotherapy for pulmonary tuberculosis in children. Pediatr Infect Dis J. 1997;16:760–3. doi: 10.1097/00006454-199708000-00006. [DOI] [PubMed] [Google Scholar]
- 14.WHO/HTM/TB/2009.420. 4th ed. Geneva: World Health Organization; 2010. World Health Organization. Treatment of Tuberculosis: Guidelines. [Google Scholar]
- 15.Abdulaziz S, Almoallim H, Ibrahim A, Samannodi M, Shabrawishi M, Meeralam Y, et al. Poncet's disease (reactive arthritis associated with tuberculosis): Retrospective case series and review of literature. Clin Rheumatol. 2012;31:1521–8. doi: 10.1007/s10067-012-2042-0. [DOI] [PubMed] [Google Scholar]
- 16.Garg S, Malaviya AN, Kapoor S, Rawat R, Agarwal D, Sharma A. Acute inflammatory ankle arthritis in northern India – Lofgren's syndrome or Poncet's disease? J Assoc Physicians India. 2011;59:87–90. [PubMed] [Google Scholar]
- 17.Wolfe F, Smythe HA, Yunus MB, Bennett RM, Bombardier C, Goldenberg DL, et al. The American College of Rheumatology 1990 criteria for the classification of fibromyalgia. 1990;33:160–72. doi: 10.1002/art.1780330203. [DOI] [PubMed] [Google Scholar]
- 18.Neogi T, Jansen TL, Dalbeth N, Fransen J, Schumacher HR, Berendsen D, et al. 2015 Gout classification criteria: An American College of Rheumatology/European League Against Rheumatism collaborative initiative. Ann Rheum Dis. 2015;74:1789–98. doi: 10.1136/annrheumdis-2015-208237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sarzi-Puttini P, Atzeni F, Capsoni F, Lubrano E, Doria A. Drug-induced lupus erythematosus. Autoimmunity. 2005;38:507–18. doi: 10.1080/08916930500285857. [DOI] [PubMed] [Google Scholar]
- 20.Vincent A, Lahr BD, Wolfe F, Clauw DJ, Whipple MO, Oh TH, et al. Prevalence of fibromyalgia: A population-based study in Olmsted County, Minnesota, utilizing the Rochester Epidemiology Project. Arthritis Care Res (Hoboken) 2013;65:786–92. doi: 10.1002/acr.21896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Phillips K, Clauw DJ. Central pain mechanisms in the rheumatic diseases: Future directions. Arthritis Rheum. 2013;65:291–302. doi: 10.1002/art.37739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Beek LA, van der Werf MJ, Richter C, Borgdorff MW. Extrapulmonary tuberculosis by nationality, The Netherlands, 1993-2001. Emerg Infect Dis. 2006;12:1375–82. doi: 10.3201/eid1209.050553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gholami K, Kamali E, Hajiabdolbagh MI, Shalviri G. Evaluation of anti-tuberculosis induced adverse reactions in hospitalized patients. Pharm Pract. 2006;4:134–8. [PMC free article] [PubMed] [Google Scholar]
- 24.Rieder HL, Snider DE, Jr, Cauthen GM. Extrapulmonary tuberculosis in the United States. Am Rev Respir Dis. 1990;141:347–51. doi: 10.1164/ajrccm/141.2.347. [DOI] [PubMed] [Google Scholar]
- 25.Donahue HC. Ophthalmologic experience in a tuberculosis sanatorium. Am J Ophthalmol. 1967;64:742–8. doi: 10.1016/0002-9394(67)92860-7. [DOI] [PubMed] [Google Scholar]
- 26.Yasaratne BMGD, Madegedara D, Senanayake NS, Senaratne T. A case series of symptomatic ocular tuberculosis and the response to anti-tubercular therapy. Ceylon Med J. 2010;55:1. doi: 10.4038/cmj.v55i1.1703. [DOI] [PubMed] [Google Scholar]
- 27.Wakabayashi T, Morimura Y, Miyamoto Y, Okada AA. Changing pattern of intraocular inflammatory disease in Japan. Ocul Immunol Inflamm. 2003;11:277–86. doi: 10.1076/ocii.11.4.277.18260. [DOI] [PubMed] [Google Scholar]
- 28.Mercanti A, Parolini B, Bonora A, Lequaglie Q, Tomazzoli L. Epidemiology of endogenous uveitis in north-eastern Italy: Analysis of 655 new cases. Acta Ophthalmol Scand. 2001;79:64–8. doi: 10.1034/j.1600-0420.2001.079001064.x. [DOI] [PubMed] [Google Scholar]
- 29.Salimpour R, Salimpour P. Picture of the month. Tuberculous dactylitis. Arch Pediatr Adolesc Med. 1997;151:851–2. doi: 10.1001/archpedi.1997.02170450101018. [DOI] [PubMed] [Google Scholar]
- 30.Kuramoto Y, Aiba S, Tagami H. Erythema induratum of bazin as a type of tuberculid. J Am Acad Dermatol. 1990;22:612–6. doi: 10.1016/0190-9622(90)70082-s. [DOI] [PubMed] [Google Scholar]


