Abstract
Epiploic appendagitis is a rare cause of acute abdomen that often manifests with acute onset of pain in the left or right lower quadrant. Its symptoms can mimic and be mistaken for acute diverticulitis, appendicitis, or omental infarction. In this case report, we discuss a 65-year-old woman who presented with sharp right upper and lower quadrant abdominal pain, for which she had an emergent abdominal computed tomography (CT) scan. On CT images, epiploic appendagitis will appear as oval lesions with a central area of fat attenuation, accompanied by surrounding inflammation. Ultrasound and magnetic resonance imaging are more often used to evaluate acute abdominal pain in the pediatric and obstetric populations, so the respective findings of acute epiploic appendagitis must be recognized in those examinations as well. Despite the rarity of the condition and its common omission from differential diagnoses, the ability to recognize and diagnose epiploic appendagitis from its imaging is important for radiologists, especially considering its potential complications. If not diagnosed correctly, epiploic appendagitis can result in unnecessary hospital admission and patient workup, antibiotic use, dietary restrictions, and perhaps even unnecessary surgery. In this case, the diagnosis of epiploic appendagitis using CT allowed the patient to avoid surgery and other invasive treatment, and the patient was eventually discharged on conservative medical management.
Keywords: Epiploic appendagitis, Acute abdomen, Computed tomography
Case summary
A 65-year-old woman presented to our emergency department (ED) with a sharp, right-sided flank pain that had started the day before her presentation. The patient reported a medical history of fatty liver and elevated liver function tests, as well as a history of unspecified liver nodules in the past that were biopsied elsewhere. She denied trauma to the area, fever, chills, nausea, vomiting, dysuria, hematuria, and any history of renal colic. Review of systems was otherwise negative.
Physical examination of the patient was performed in the ED and revealed an otherwise well-appearing patient. Abdominal examination revealed a nondistended abdomen with tenderness in the right upper and lower quadrant. There was no guarding, rebound, pulsatile, or palpable mass, or costovertebral angle tenderness. Physical examination was otherwise unremarkable. The patient was placed on observation status, and laboratory and diagnostic tests were ordered. The patient was given an intravenous (IV) bolus of 250 mL of normal saline solution followed by 125 mL/h IV normal saline solution, and Toradol (Roche Pharmaceuticals, Switzerland) 15 mg IV for pain control. Laboratory results obtained in the ED showed aspartate aminotransferase of 57 and alanine aminotransferase of 79.
Imaging findings and diagnosis
An abdominopelvic computed tomography (CT) with IV contrast performed at the hospital revealed infiltration of the fat adjacent to the right colon, just inferior to the right lobe of the liver (Fig. 1). This finding was on the antimesenteric margin of the colon and contained a central lucency consistent with epiploic appendagitis (Fig. 2). The appendix was normal in morphology and there was no bowel obstruction or abscess formation. In addition to the patient's epiploic appendagitis, there was also CT evidence of mild hepatomegaly with diffuse fatty infiltration of the liver, colonic diverticulosis without CT evidence of diverticulitis, mild atherosclerotic changes seen in the abdominal aorta, and a right hip prosthesis.
Fig. 1.
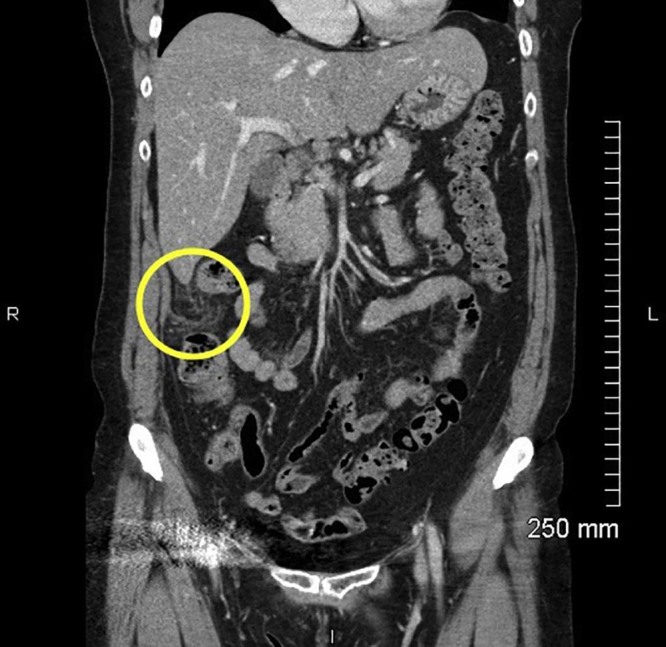
Five-millimeter coronal sections were reconstructed from 5-mm helically acquired axial sections by the technologist on the computed tomography scanner. On coronal view, there is infiltration of the fat adjacent to the right colon, just inferior to the right lobe of the liver.
Fig. 2.

Axial view shows the epiploic appendagitis located on the antimesenteric margin of the colon with a central lucent area of fat attenuation and surrounding induration.
The observation discharge examination revealed improvement in the patient's symptoms and physical examination. The last recorded vital signs showed temperature of 98.3°F, blood pressure of 127/86 mm Hg, pulse of 73 beats/min, respiratory rate of 18 breaths/min, and pulse oximetry of 98% on room air. The patient was instructed to follow up with her primary care doctor within 2 days for further evaluation. A prescription for ibuprofen was written, and the patient was discharged.
Discussion
Acute epiploic appendagitis is a benign, self-limiting inflammation of the appendices epiploicae. These epiploic (or omental) appendages are peritoneal outpouchings composed of adipose tissue and blood vessels that arise from the serosa, parallel to the taenia coli of the colon. Each epiploic appendage is connected by a vascular stalk that contains a branch of the circular artery and vein that supply the underlying area of colon [1]. Epiploic appendages are typically 0.5-5 cm in length, with the largest ones located near the sigmoid colon [2]. Normal epiploic appendages are not typically seen on CT imaging, unless they are inflamed, surrounded by intraperitoneal fluid (eg, ascites or hemoperitoneum), or calcified [3]. The most common sites of acute epiploic appendagitis are the sigmoid colon, the descending colon, and the right hemicolon [2]. During an episode of acute epiploic appendagitis, torsion of the appendages causes vascular or venous occlusion, which can result in ischemia, thrombosis, or infarction. Besides torsion, epiploic appendagitis can also be caused by hernia incarceration or intestinal obstruction [2].
Epiploic appendagitis is mostly seen during the fourth to fifth decades of life, and is more common in men. It is frequently associated with colonic diverticula, obesity, strenuous exercise, and hernias [2].
Epiploic appendagitis is a rare cause of acute abdomen that often manifests with acute onset of pain in the left or right lower quadrant [2]. Its symptoms can mimic and be mistaken for acute diverticulitis, but patients with epiploic appendagitis are usually afebrile, without leukocytosis, nausea, or vomiting [1]. Epiploic appendagitis can also be mistaken for appendicitis or omental infarction.
Before CT imaging was available, epiploic appendagitis was most commonly diagnosed during surgery, and it was not until 1986 that the CT features for the condition were even described [4]. Definitive diagnosis is most commonly made by contrast CT imaging, but ultrasound and magnetic resonance imaging (MRI) can also be used. On CT images, epiploic appendagitis will appear as oval lesions with a central area of fat attenuation, accompanied by surrounding inflammation [2]. The inflammation may cause secondary thickening of the parietal peritoneum, and the colon wall may be inflamed as well [2]. Although the patient's clinical symptoms usually resolve within 2 weeks, CT findings can last for as long as 6 months after the episode, showing some residual soft tissue attenuation [2]. With regard to alternative imaging modalities, ultrasound and MRI are more often used to evaluate acute abdominal pain in the pediatric and obstetric populations, so the respective findings of acute epiploic appendagitis must be recognized in those examinations as well [5]. On ultrasound imaging of the point of maximal tenderness, epiploic appendagitis will appear as an oval, noncompressible mass with no central blood flow depicted on color Doppler [6]. The hyperechoic mass will usually be surrounded by a hypoechoic peripheral ring [7]. Additionally, ultrasound can be used to evaluate the presence of a central dot-shaped, hyperdense focus, which suggests a thrombosed vein [3]. Although MRI is rarely used for diagnosis, T1- and T2-weighted images will show a focal lesion that has the signal intensity of fat. Additionally, contrast-enhanced T1-weighted images show an enhancing rim around the oval fatty lesion [2]. Complications of epiploic appendagitis include adhesions, abscess formation, peritonitis, bowel obstruction, intussusception, or intraperitoneal loose body [2].
In the majority of patients, epiploic appendagitis is self-resolving, with pain control being the only treatment modality. Oral anti-inflammatory medication is usually prescribed for 4-7 days, and antibiotics are not often indicated. Surgery is reserved for patients whose symptoms fail to improve with conservative management, or patients who develop complications that cannot be managed nonoperatively. In this case, the inflamed appendage would be ligated and resected [8].
Conclusion
Despite the rarity of the condition and its common omission from differential diagnoses, the ability to recognize and diagnose epiploic appendagitis using various imaging modalities is important for radiologists and other health care providers, especially considering its potential complications. If not diagnosed correctly, epiploic appendagitis can result in unnecessary hospital admission and patient workup, antibiotic use, dietary restrictions, and perhaps even unnecessary surgery.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
References
- 1.Ryen C. Epiploic appendagitis in a female patient with situs ambiguous abnormality. J Radiol Case Rep. 2009;3(8):30–34. doi: 10.3941/jrcr.v3i8.282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Singh A.K., Gervais D.A., Hahn P.F., Sagar P., Mueller P.R., Novelline R.A. Acute epiploic appendagitis and its mimics. Radiographics. 2005;25(6):1521–1534. doi: 10.1148/rg.256055030. [DOI] [PubMed] [Google Scholar]
- 3.Kani K.K., Moshiri M., Bhargava P., Kolokythas O. Extrahepatic, nonneoplastic, fat-containing lesions of the abdominopelvic cavity: spectrum of lesions, significance, and typical appearance on multidetector computed tomography. Curr Probl Diagn Radiol. 2012;41(2):56–72. doi: 10.1067/j.cpradiol.2011.07.005. [DOI] [PubMed] [Google Scholar]
- 4.Danielson K., Chernin M.M., Amberg J.R., Goff S., Durham J.R. Epiploic appendicitis: CT characteristics. J Comput Assist Tomogr. 1986;10(1):142–143. doi: 10.1097/00004728-198601000-00032. [DOI] [PubMed] [Google Scholar]
- 5.Eberhardt S.C., Strickland C.D., Epstein K.N. Radiology of epiploic appendages: acute appendagitis, post-infarcted appendages, and imaging natural history. Abdom Radiol (NY) 2016;41(8):1653–1665. doi: 10.1007/s00261-016-0757-0. [DOI] [PubMed] [Google Scholar]
- 6.Mollà E., Ripollés T., Martínez M., Morote V., Roselló-Sastre E. Primary epiploic appendagitis: US and CT findings. Eur Radiol. 1998;8:435. doi: 10.1007/s003300050408. [DOI] [PubMed] [Google Scholar]
- 7.Nadida D., Amal A., Ines M., Makram M., Amira M, Leila B.F. Acute epiploic appendagitis: radiologic and clinical features of 12 patients. Int J Surg Case Rep. 2016;28:219–222. doi: 10.1016/j.ijscr.2016.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Patel V.G., Rao A., Williams R., Srinivasan R., Fortson J.K., Weaver W.L. Cecal epiploic appendagitis: a diagnostic and therapeutic dilemma. Am Surg. 2007;73(8):828–830. [PubMed] [Google Scholar]


