Abstract
Lomentospora prolificans is a rare cause of vertebral osteomyelitis. We report a case of L. prolificans thoracic vertebral osteomyelitis with spinal epidural abscess in a patient without apparent immunodeficiency. Clinical manifestations and radiographic findings could not distinguish from other etiologic agents. Treatment is also challenging because L. prolificans is usually resistant to antifungal agents. The patient underwent surgical debridement and has been receiving a prolonged combination of antifungal therapy to prevent an infection relapse.
Keywords: Lomentospora prolificans, Vertebral osteomyelitis, Spinal epidural abscess, Immunocompetent patient
1. Introduction
Lomentospora prolificans (formerly known as Scedosporium prolificans) is filamentous fungus predominantly found in natural sources. L. prolificans can be transmitted to humans through inhalation of fungal particles, causing fungal colonization, localized pulmonary infection, or dissemination to distant organs [1]. The fungus can also be transmitted via direct inoculation following penetrating trauma or previous surgery rendering skin, soft tissue and osteoarticular infections. The disseminated infection is usually reported among patients with immunodeficiency conditions. In Thailand, L. prolificans infection had been reported in a patient who had prolonged neutropenia following chemotherapy for acute myeloid leukemia; the patient presented with a disseminated infection including pansinusitis, cutaneous hemorrhagic bulla, and multiple pulmonary nodules [2]. Vertebral osteomyelitis from L. prolificans is an uncommon infection and has been rarely reported. We report a case of L. prolificans vertebral osteomyelitis of the 8th (T8) and 9th (T9) thoracic spines with spinal epidural abscess in a patient without apparent immunodeficiency status.
(This work was presented in part at the 8th Trends in Medical Mycology (TIMM) Meeting, October 6–9, 2017 in Belgrade, Serbia.)
2. Case
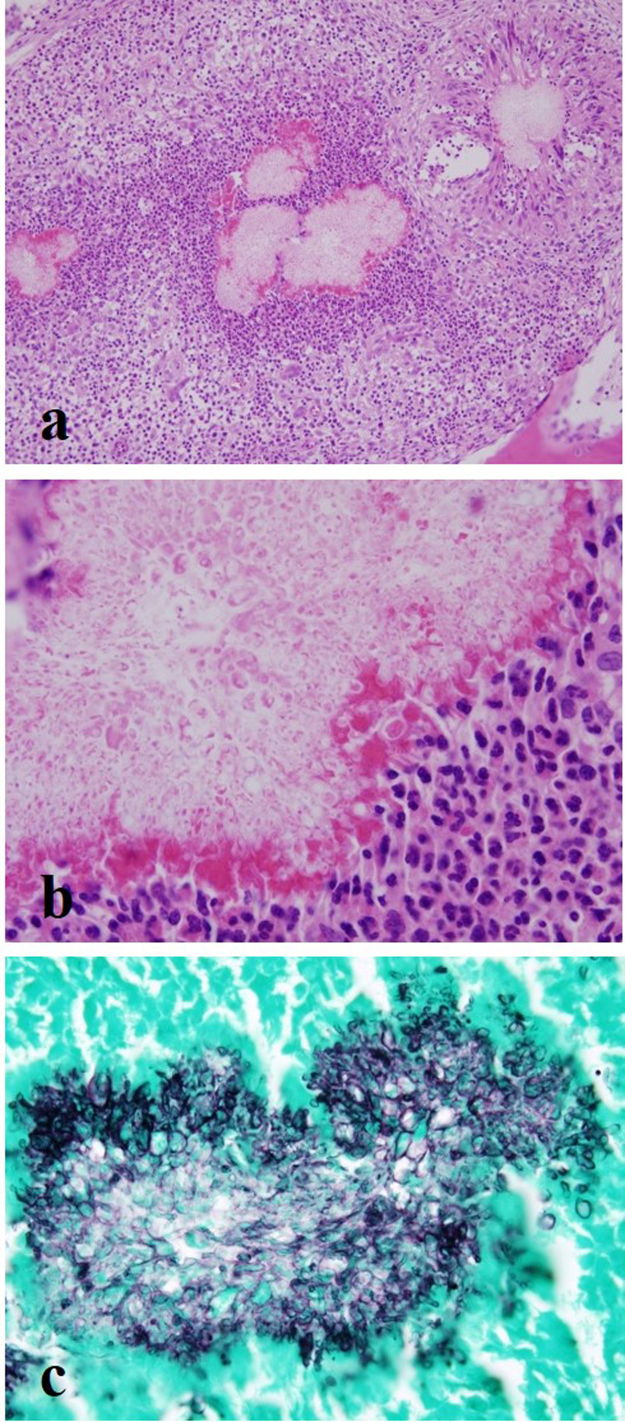
A 57-year-old Thai woman who was previously healthy presented with chronic progressive mid-thoracic back pain for 3 months. The pain caused the patient restricted to do daily activities. She was afebrile, but her weight decreased 8 kg in 3 months. She denied taking herbal medicines, illicit drugs, or corticosteroids. She had no previous surgery or back injury. She was hospitalized on 22 January 2017 (Day 0). Physical findings demonstrated tenderness over the mid-thoracic spines, hypertonia and hyperreflexia of the right lower extremities. Other examinations were unremarkable. Blood chemistries were in normal range. Anti-HIV testing was negative. Magnetic resonance imaging (MRI) of the thoracolumbar (TL) spines revealed destruction of the T8 and T9 vertebral bodies, pedicles and posterior elements, resulting T8 and T9 myelopathy, including spinal epidural abscess formation (Fig. 1). Three days after admission (Day +3), a T8 and T9 laminectomy found necrotic tissues and 3-mL pus located in the epidural space. The pathologic findings showed Splendore-Hoeppli phenomenon in pyogranulomatous reaction, and Gomori methenamine silver (GMS) staining highlighted groups of septate fungal hyphae (Fig. 2). Pus cultures grew black pigmented mold, later internal transcribed spacer (ITS) gene sequencing identified L. prolificans. Antifungal susceptibility testing showed MICs (μg/mL) of amphotericin B of 8, 5-flucytosine of > 64, fluconazole of > 256, itraconazole of > 16, voriconazole of 4, posaconazole of > 8, caspofungin of 8, micafungin of > 8 and anidulafungin of 4. Voriconazole 400 mg/day and terbinafine 500 mg/day were prescribed after ascertaining the fungal culture (Day + 12). An immunological testing panel including anti-interferon-gamma autoantibody, interferon-gamma receptor, interleukin 12 receptor, CD4 level, and CD8 level found no abnormality. A high resolution computed tomography (HRCT) of the chest did not identify contiguous pulmonary or mediastinal infectious foci causing the vertebral infection. The patient complied well with antifungal therapy, and voriconazole concentrations ranged from 1.5 to 2.0 μg/mL.
Fig. 1.
A: The MRI of TL spines demonstrated bony destruction of T8 and T9 vertebral bodies and posterior elements, causing myelopathy at T8–T9 levels with spinal epidural abscess formation. B: The follow-up MRI after the 6-month therapy demonstrated new and more progressive vertebral osteomyelitis at the T6, T7 and T10 spines, and circumferential soft tissue thickening with heterogeneous enhancement in epidural space, causing spinal canal stenosis.
Fig. 2.
A: Fungal colony with Splendore-Hoeppli phenomenon in pyogranulomatous reaction (HE 20 × magnification). B: High magnification revealed club shape eosinophilic material at the periphery of the fungal colony (HE 100 × oil immersion). C: Septate fungal hyphae were highlighted in GMS stain (GMS 100 × oil immersion).
Following the 6-month antifungal therapy (Day +180), her back pain gradually resolved, but an MRI revealed new and more progressive vertebral osteomyelitis at the T6, T7 and T10 spines, and circumferential soft tissue thickening with heterogeneous enhancement in the epidural space, causing spinal canal stenosis (Fig. 1b). The dose of voriconazole was raised to 600 mg/day. The voriconazole concentrations ranged from 1.8 to 2.6 μg/mL following the incremental dose. Her back pain was in complete remission. The patient has continued the long-term combination antifungal therapy without serious complications.
3. Discussion
Vertebral osteomyelitis caused by fungal infection is rare, but the incidence has been increasing over the past several decades. Aspergillus spp. (38%) and Candida spp. (23%) are the two common etiologies of fungal vertebral osteomyelitis, for which recent surgery, organ transplant recipient, and malignancy are the risk factors [3]. The presented case had an unclear portal of infection, and had no previous injury or surgery of the spine. Inhalation of fungal spores can lead to pulmonary infection and occasionally causes metastatic infection to distant organs [1]. An HRCT of the chest was performed to evaluate if there was a pulmonary focus of infection causing direct invasion to the adjacent vertebra or dissemination to the distant vertebra. However, it revealed no radiographic findings suggestive of a pulmonary fungal infection.
Vertebral osteomyelitis and/or spinal epidural abscess caused by L. prolificans has been rarely reported in previous literature, as shown at Table 1 [4], [5], [6]. The previous case reports had risk factors or identified routes of infection, such as stem cell transplant, previous colonization, recent spine surgery, and previous spinal anesthesia [4], [5], [6]. All but one had back pain as a presenting manifestation. The duration of the presenting symptoms from all case reports tended to be chronic and slowly progressive from the onset. Fever was the presenting symptom in only one patient, who developed spondylodiscitis of the affected sites following L5-S1 intervertebral disc herniation surgery [5]. The infectious foci were mostly located in the lower thoracic or lumbrosacral regions. However, the clinical manifestations and radiographic findings of L. prolificans vertebral osteomyelitis cannot be distinguished from other etiologic agents, such as bacteria, mycobacteria, and other fungi.
Table 1.
Summary of case reports with vertebral osteomyelitis and/or epidural abscess spinal epidural abscess due to L. prolificans infection.
| Case, | Age (yrs.)/sex | Predisposing conditions | Presenting symptoms | Infectious foci | Radiographic findings | Pathological findings | Antifungal | Treatments | Outcomes |
|---|---|---|---|---|---|---|---|---|---|
| country (Year) | MICs (μg/mL) | ||||||||
| 1, | 53/F | MM, autologous HSCT, previous | LBP and weakness of right leg | L, S | L2, L3, L5 and S1 vertebral osteomyelitis with intervertebral discitis | Acute inflammatory | ABD 8 | - Oral VORI, TBF | Partial recoverya |
| Australia | ITRA > 16 | ||||||||
| (2003)5 | L. prolificans rhinosinusitis | reaction | VORI 2 | - Laminectomy | |||||
| 2, | 62/F | Previous spine surgery 5 months | Fever and LBP | L, S | L5 and S1 vertebral osteomyelitis with intervertebral discitis | n/a | ABD 16 | - Oral VORI | Complete recovery |
| Spain | ITRA 8 | - Debridement and | |||||||
| (2009)4 | 1 month | VORI 8 | arthrodesis | ||||||
| 3, | 35/M | Previous spinal epidural anesthesia 15 yrs | Progressive weakness of lower limbs 6 yrs | T | Spinal epidural abscess | Chronic inflammation and fungal hyphae | n/a | - IV and oral VORI | Relapseb |
| Brazil | at T9 and T10 levels | - Laminectomy and | |||||||
| (2009)6 | drainage | ||||||||
| The present | 57/F | – | Mid thoracic back pain 3 months | T | T8-T9 vertebral osteomyelitis and spinal epidural abscess | Granulomatous inflammation, Splendore-Hoeppli reaction, and fungal hyphae | ABD 8 | - Oral VORI, TBF | Ongoing treatment |
| case, | ITRA > 16 | - Laminectomy and | |||||||
| Thailand | VORI 4 | removal of | |||||||
| (2017) | POSA > 8 | abscess |
Abbreviations: ABD, amphotericin B deoxycholate; F, female; HSCT, haematopoetic stem cell transplantation; ITRA, itraconazole; IV, intravenous; L, lumbar, LBP, low back pain; MICs, minimal inhibitory concentrations; MM, multiple myeloma; n/a, not available; POSA, posaconazole; S, sacrum; T, thoracic; TBF, terbinafine; VORI, voriconazole; yrs, years.
Recovery of neurological deficits, but LBP and radiographic findings has been unchanged.
Relapse following discontinuation of antifungal therapy for 3 months.
Diagnosis of this condition comprises a tissue biopsy sent for histopathological examinations and fungal cultures. From the presented case, the pathological section demonstrated pyogranulomatous inflammation with Splendore-Hoeppli reaction, which is not specific for fungal infection [7]. Tissue for fungal culture is required for diagnosis of invasive fungal infection. In our case, the fungal culture identified colonies of dematiaceous mold, which demonstrated single-celled conidia on elongated conidiophores under microscopic examination. The colony and microscopic structures cannot differentiate between Lomentospora spp. and Scedosporium spp. Thus, the ITS gene sequencing was used for species identification of the isolate in this case. Occasionally, species identification is crucial because virulence and antifungal susceptibility may vary among different species [8]. L. prolificans mostly demonstrates reduced in vitro antifungal susceptibility, and is associated with more invasive infections and higher mortality compared to S. apiospermum [1], [9], [10]. From Table 1, the isolates from the previous and the presented cases exhibited higher MICs to amphotericin B and itraconazole than voriconazole. A previous study demonstrated L. prolificans had moderate to high MICs to several antifungals agents, such as amphotericin B, conventional azoles, flucytosine, and echinocandins [1].
The optimal management of L. prolificans vertebral osteomyelitis remains inconclusive. Successful treatment generally requires adequate resection of infected foci and long-term antifungal therapy. Adequate surgical debridement is associated with favorable outcomes, particularly in localized or osteoarticular infections [11]. According to Table 1, all patients underwent surgical debridement combined with prolonged voriconazole therapy. Voriconazole has a relatively greater in vitro activity, and it can penetrate well into bone and the central nervous system [1]. Of 4 cases, 2 received a combination of antifungal agents. A combination of terbinafine and voriconazole or itraconazole showed a synergistic effect against L. prolificans isolates [12], in which both agents inhibited an ergosterol synthesis of fungal cell wall at different sites of action [11]. Anecdotal data showed the combined voriconazole and terbinafine was used to treat a patient who had L. prolificans osteoarticular infection of the left ankle successfully [13]. However, the opitmal dosing regimen and duration of antifungal therapy are still unknown. The presented case has been receiving a prolonged combination of voriconazole and terbinafine to prevent a relapse of infection without serious adverse reactions.
In conclusion, L. prolificans is a rare cause of fungal vertebral osteomyelitis. Clinical manifestations and radiographic findings cannot distinguish from other etiologic agents. A high index of suspicion, pathological examination, and fungal culture are required for diagnosis. Antifungal susceptibility testing may assist in choosing the appropriate antifungal regimen. Adequate surgical removal of the infected focus and long-term antifungal therapy are required to achieve a successful outcome.
Acknowledgements
The authors would like to acknowledge neurosurgeons at Siriraj Hospital for management of the patient; the staff of the Mycology Laboratory Unit, Department of Microbiology, for providing the microbiological data; and the staff of the Department of Pathology for providing the pathological data.
Acknowledgments
Conflict of interest
There are no conflicts of interest.
This study did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
References
- 1.Cortez K.J., Roilides E., Quiroz-Telles F., Meletiadis J., Antachopoulos C., Knudsen T. Infections caused by Scedosporium spp. Clin. Microbiol. Rev. 2008;21:157–197. doi: 10.1128/CMR.00039-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Damronglerd P., Phuphuakrat A., Santanirand P., Sungkanuparph S. Disseminated Scedosporium prolificans infection in a patient with acute myeloid leukemia and prolonged febrile neutropenia. J. Infect. Dis. Antimicrob. Agents. 2014;31:101–105. [Google Scholar]
- 3.Ganesh D., Gottlieb J., Chan S., Martinez O., Eismont F. Fungal infections of the spine. Spine (Phila. Pa 1976) 2015;40:E719–E728. doi: 10.1097/BRS.0000000000000903. [DOI] [PubMed] [Google Scholar]
- 4.Garcia-Vidal C., Cabellos C., Ayats J., Font F., Ferran E., Fernandez-Viladrich P. Fungal postoperative spondylodiscitis due to Scedosporium prolificans. Spine J. 2009;9:e1–e7. doi: 10.1016/j.spinee.2009.03.012. [DOI] [PubMed] [Google Scholar]
- 5.Howden B.P., Slavin M.A., Schwarer A.P., Mijch A.M. Successful control of disseminated Scedosporium prolificans infection with a combination of voriconazole and terbinafine. Eur. J. Clin. Microbiol. Infect. Dis. 2003;22:111–113. doi: 10.1007/s10096-002-0877-z. [DOI] [PubMed] [Google Scholar]
- 6.Carod-Artal F.J., Ferreira-Coral L., Mauro-Couto J., Gomes E., de Agassiz-Vasques M. Chronic spinal epidural abscess caused by Scedosporium prolificans in an immunocompetent patient. Spine (Phila. Pa 1976) 2009;34:E330–E332. doi: 10.1097/BRS.0b013e31819964eb. [DOI] [PubMed] [Google Scholar]
- 7.Hussein M.R. Mucocutaneous Splendore-Hoeppli phenomenon. J. Cutan. Pathol. 2008;35:979–988. doi: 10.1111/j.1600-0560.2008.01045.x. [DOI] [PubMed] [Google Scholar]
- 8.Wang H., Wan Z., Li R., Lu Q., Yu J. Molecular identification and susceptibility of clinically relevant Scedosporium spp. in China. Biomed. Res. Int. 2015;2015:109656. doi: 10.1155/2015/109656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Troke P., Aguirrebengoa K., Arteaga C., Ellis D., Heath C.H., Lutsar I. Global Scedosporium study Group.treatment of scedosporiosis with voriconazole: clinical experience with 107 patients. Antimicrob. Agents Chemother. 2008;52:1743–1750. doi: 10.1128/AAC.01388-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cooley L., Spelman D., Thursky K., Slavin M. Infection with Scedosporium apiospermum and S. prolificans, Australia. Emerg. Infect. Dis. 2007;13:1170–1177. doi: 10.3201/eid1308.060576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Panackal A.A., Marr K.A. Scedosporium/Pseudallescheria infections. Semin. Respir. Crit. Care Med. 2004;25:171–187. doi: 10.1055/s-2004-824901. [DOI] [PubMed] [Google Scholar]
- 12.Meletiadis J., Mouton J.W., Rodriguez-Tudela J.L., Meis J.F., Verweij P.E. In vitro interaction of terbinafine with itraconazole against clinical isolates of Scedosporium prolificans. Antimicrob. Agents Chemother. 2000;44:470–472. doi: 10.1128/aac.44.2.470-472.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gosbell I.B., Toumasatos V., Yong J., Kuo R.S., Ellis D.H., Perrie R.C. Cure of orthopaedic infection with Scedosporium prolificans, using voriconazole plus terbinafine, without the need for radical surgery. Mycoses. 2003;46:233–236. doi: 10.1046/j.1439-0507.2003.00878.x. [DOI] [PubMed] [Google Scholar]