Abstract
Background
Malaria is a major public health problem in Myanmar with reported artemisinin resistance. Myanmar promotes the use of insecticide-treated nets (ITNs) through the free delivery of long-lasting insecticide nets (LLINs) with target coverage of at least 80% in moderate and high-risk areas by 2014. Migrant people are at greater risk of malaria. They have significant barriers to health care services for febrile illness and malaria. Thus, a community-based survey was conducted among the migrant population to assess the ownership and utilization of bed nets (ITN/LLINs) for malaria.
Methods
The study analyzed secondary data from a community-based malaria survey conducted in 2014 among migrant population in 30 randomly selected townships out of 52 Regional Artemisinin Resistance Initiative (RAI) townships. In each township, five migrant sites were randomly selected (total of 150 migrant sites). A total of 3933 households (approximately 125 households from each township) were selected.
Results
Of 3923 households assessed, 97% had access to at least one bed net (any type), but only half had access to ITN/LLINs. Only 24% of households had adequate ITN/LLIN access (at least one ITN/LLIN per two persons). In terms of household utilization, 94.3% slept under a bed net (any type) the previous night. Only 43.4% slept under an ITN/LLIN. ITN/LLIN utilization in children under 5 years and pregnant women (high-malaria risk groups) was 45.3 and 46.6%, respectively. Of all nets, 31.3% had holes or had already undergone repairs. In terms of insecticide treatment status, 52.9% of bed nets were untreated and 35.9% of ITNs had not been treated with insecticide for more than a year.
Conclusion
This study highlights poor access and high utilization of ITN/LLINs among migrant population, particularly among children and pregnant women. It highlights the need for improving bed net coverage and access to ITN/LLINs through bed net distributions and/or social marketing with the focus on migrant population and targeting of households with children and pregnant women.
Keywords: Malaria, ITN/LLINs, MARC area, Bed net ownership, Migrant
Background
Despite global decline in malaria morbidity and mortality in the last decade, malaria is still one of the major public health problems in Myanmar with two thirds of its population at risk of getting the disease [1]. There is growing evidence of artemisinin resistance in parts of The Greater Mekong Sub-region (GMS), known as the epicenter of multidrug-resistant Plasmodium falciparum, especially in eastern Myanmar along with Cambodia and Vietnam. A gradual decline in the therapeutic efficacy of common artemisinin-based combination therapy (ACT) [2] and the evidence of artemisinin resistance in certain pockets of Myanmar [3] led to the Myanmar Artemisinin Resistance Containment (MARC) strategy by World Health Organization (WHO) [4].
The strategy focused on the mobile migrant populations, with a major emphasis on improving access to vector control measures including personal protection, malaria diagnosis, antimalarial drugs, and treatment in order to prevent or delay the spread of artemisinin resistance [4]. In 2014, Regional Artemisinin Initiative (RAI) project was initiated by the Global Fund in 52 selected townships from the MARC areas with suspected artemisinin resistance.
The use of insecticide-treated bed nets (ITNs) is one of the most effective forms of vector control. The WHO Global Malaria Programme has recommended full coverage of long-lasting insecticidal nets (LLINs)/ITNs for malaria prevention [5]. Myanmar also promotes the use of bed nets (ITNs) through the free delivery of LLINs and free treatment of mosquito nets already in use before the start of the peak transmission season. The goal is that at least 80% of people in moderate and high-risk areas are protected by ITNs/LLINs [6]. Previous studies among the general population in Myanmar or among selected migrant groups such as the rubber plantation workers have shown the poor utilization of ITN/LLINs [7, 8].
Migration poses new challenges for health systems. In Myanmar, migrant people are at greater risk of malaria because of their nature of work and proximity to places such as forest, rubber plantation, oil, and mine working places [9]. They temporarily stay in remote areas and have significant barriers to preventive, diagnostic, and treatment services for febrile illness and malaria [7]. Of particular importance is malaria among mobile occupational migrants on international borders, particularly the Myanmar-Thai border where there is a serious threat to ACT effectiveness due to resistance. The 2008 World Health Assembly adopted the resolution on the health of migrants, calling on member states “to promote migrant-sensitive health policies.” Healthy migrants contribute to the positive sustainable development and improve the public health outcomes.
In line with this, a community-based survey was conducted among migrant population in the RAI project areas of Myanmar in 2015. This study aimed to assess the ownership of, access to, and utilization of bed nets (LLIN/ITNs) in RAI areas of Myanmar.
Methods
Study design
A cross-sectional study design involving analysis of secondary data from community-based malaria survey conducted among migrant population in 2014.
Study setting
General setting
The Republic of the Union of Myanmar has an estimated population of 51 million inhabitants of whom 70% live in rural areas. The country is bordered by Bangladesh, India, China, Laos and Thailand in the North and East, the Bay of Bengal in the west, and in the south by the Andaman Sea. It is divided administratively, into the capital territory (Nay Pyi Taw Council Territory) and seven states and seven regions. There are 74 districts with 330 townships.
Specific setting
Malaria is endemic in 291 out of the 330 townships in Myanmar. The country constitutes of high transmission (> 1 case per 1000 population), low transmission (0–1 case per 1000 population), and malaria-free areas (zero cases) represented by 16, 44, and 40% of the total population, respectively [10]. Malaria remains a public health problem due to climatic and ecological changes, population migration, and ecological development activities such as mining, forestry, and development of multidrug resistance Plasmodium falciparum parasite.
Areas are categorized into tiers 1, 2, and 3 according to the evidence and level of artemisinin resistance. Tier 1 areas is where there is credible evidence of artemisinin resistance; tier 2 is where there is a significant inflow of people from tier 1, including those areas immediately bordering tier 1; and tier 3 is where there is no evidence of artemisinin resistance and limited contact with tier 1 areas. There are 31 townships in tier 1, 21 in tier 2, and 258 in tier 3. In 2014, RAI project was initiated by the Global Fund which covered 52 townships from tier 1 and tier 2. The study areas were selected from these RAI project areas (tiers 1 and 2).
Free distribution of ITNs/LLINs in areas of high-malaria transmission is one of the key interventions for malaria elimination in Myanmar. This is done mainly by the National Malaria Control Program (NMCP) and other partners yearly. Although ITN/LLIN is internationally recommended, other bed-net types including cotton, nylon, and lace are available in local markets.
Community-based survey among the migrant population
A nation-wide community-based survey was conducted jointly by the Department of Medical Research (DMR) and NMCP in 2014 to understand the knowledge, attitude, and health-seeking behavior towards malaria and the ownership and utilization of ITNs among the migrant population in the selected townships of RAI areas. A total of 3933 households in 125 migrant sites located in 30 townships were covered.
Data source
Data variables related to the study objectives were obtained from the community-based survey described above. The survey database is available with the Ministry of Health and Sports, Myanmar.
Study area and population
The survey was carried out in the townships supported by the RAI project which is a Global Fund Grant to avert the spread of artemisinin resistance in the Greater Mekong Sub-region (GMS).
The study population included migrant population residing in the selected townships. However, those who temporarily stay in the deep forest in the selected townships were not enrolled in this study for potential security concerns. The study population (migrant population) was defined as a migrant person who is a male or female at any age who temporarily lives in the selected townships and not registered as a native villager in the village census. Exclusion criteria includes a person who has no intention to stay overnight in the selected area. Household was defined as all persons living under one roof and consuming food cooked from the same kitchen.
Sampling and sample size
Out of 52 townships in RAI areas, 30 were selected randomly. A sampling frame of all migrant sites was available from a migrant mapping exercise done by NMCP staff. In each township, five migrant sites were randomly selected (total of 150 migrant sites). A total of 3933 households (approximately 125 households from each township) were selected. The number of households to be interviewed was based on the probability proportionate to the size of the site. Kawthaung, being a large township, 300 households were selected. A list of households in each site was also available from a baseline census of migrants done prior to the survey. In each site, the households were systematically selected from a list of households (Fig. 1).
Fig. 1.
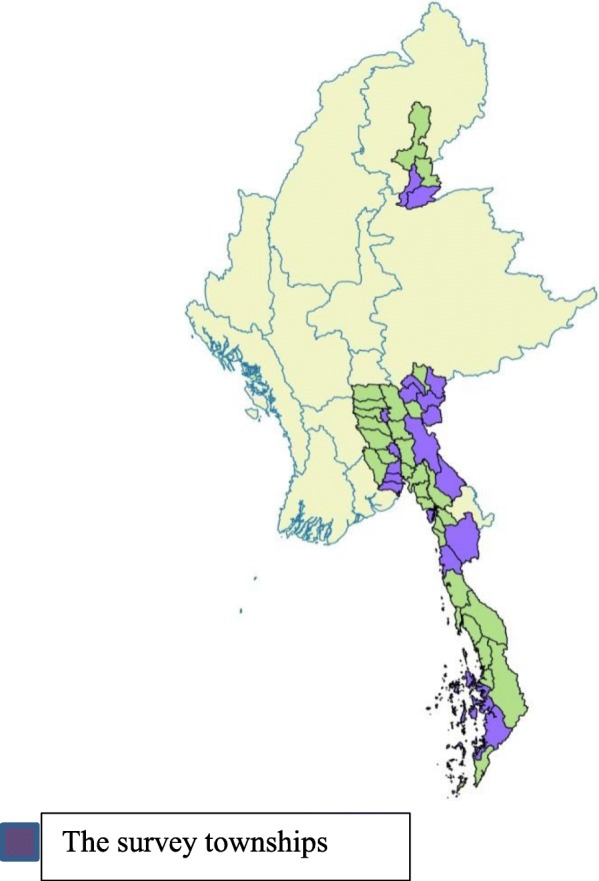
The map showing the survey townships among RAI project townships
Data validation and statistical analysis
Survey data used for this analysis were double entered and validated using EpiData Entry software (version 3.1, EpiData Association, Odense, Denmark). A descriptive analysis was performed wherein proportions were used to summarize categorical variables related to the ownership and use of bed nets. The ownership of bed nets at household level was assessed using two indicators, (a) % of households with at least one ITN/LLIN and (b) % of households with ITN/LLIN per two household members [1]. Indicators for assessing bed net utilization included the total number and proportion of household members who slept under an ITN/LLIN during the previous night. Information on the physical condition of bed nets was also gathered including material type, presence, or absence of holes and the hole size. Binomial logistic regression was used to determine the factors associated with the ownership of sufficient ITN/LLINs among the migrant population.
The indicators were calculated following the guidelines in the Household Survey Indicators for Malaria Control [11].
The proportion of households with at least one ITN/LLIN (number of households surveyed with at least one ITN/LLIN)/(total number of households surveyed)
The proportion of households with at least one ITN/LLIN for every two people (number of households with at least one ITN/LLIN for every two people)/(total number of households surveyed)
The proportion of population with access to an ITN/LLIN within their household (total number of individuals who could sleep under an ITN/LLIN if each ITN/LLIN in the household is used by two people)/(total number of individuals who spent the previous night in surveyed households)
The proportion of population that slept under an ITN/LLIN the previous night (number of individuals who slept under an ITN/LLIN the previous night)/(total number of individuals who spent the previous night in surveyed households)
Results
Characteristics of the study population and their household characteristics
Out of a total of 3933 households included in the survey, 3923 (99.8%) households completed the interview. There were a total of 14,331 members in these households. Nearly 52% of them were males and the majority (65%) belonged to the age group 15–59 years (Table 1).
Table 1.
Demographic characteristics of migrant population in RAI project areas of Myanmar, 2014
| Demographic characteristics | Total n = 14,331 n (%) |
|---|---|
| Households accessed | 3923 |
| Household members | 14,331 |
| Gendera | |
| Male | 7487 (52.3) |
| Female | 6829 (47.7) |
| Age group (years)a | |
| < 5 | 1519 (11.2) |
| 5–14 | 2755 (20.3) |
| 15–49 | 7922 (58.4) |
| 50–59 | 936 (6.9) |
| ≥ 60 | 431 (3.2) |
| Household size (n = 3923) | |
| 1–2 | 1185 (30.2) |
| 3–5 | 2091 (53.3) |
| ≥ 6 | 647 (16.5) |
RAI Regional Artemisinin Resistance Initiative
aMissing data omitted
About half of the participants lived under a barrack. Nearly three fourths of the population migrated in search of work and nearly two-thirds were unsure of their duration of stay in the present location (Table 2).
Table 2.
Characteristics and migration dynamics of migrant population in RAI project areas of Myanmar, 2014
| Characteristics | Percentage |
|---|---|
| House ownership | N = 3913 |
| Own | 1659 (42.4) |
| Tenant | 163 (4.2) |
| Bar rack | 1985 (50.7) |
| Do not know | 3 (0.1) |
| Others | 103 (2.6) |
| Reason for moving here | N = 3917 |
| To work | 2940 (75.1) |
| To find job | 780 (19.9) |
| To live here | 122 (3.1) |
| Visiting relatives/with spouse | 239 (6.1) |
| Other | 63 (1.6) |
| Intention to stay | N = 3912 |
| Less than 4 weeks | 90 (2.3) |
| One month to 3 months | 231 (5.9) |
| 3 months to 6 months | 318 (8.1) |
| 6 months to 1 year | 234 (6.0) |
| More than 1 year | 585 (15.0) |
| Not sure | 2454 (62.7) |
| Next place to move | N = 3910 |
| Home | 1686 (43.1) |
| Other work place | 401 (10.3) |
| Do not know | 1623 (41.5) |
| Other | 200 (5.1) |
Household ownership, access, and utilization of bed nets
Table 3 shows the household ownership, access, and utilization of bed nets among the migrant population in RAI areas. Almost all (95%) households had at least one bed net per household and, about half (51%) had at least one ITN/LLINs. However, less than one fourth (24%) of all households had sufficient ITN/LLIN, i.e., one ITN/LLINs per two persons.
Table 3.
Household ownership and utilization of bed nets among migrant population in RAI project areas of Myanmar, 2014
| Characteristics | n (%) |
|---|---|
| Household ownership of bed nets | |
| Total number of households | 3923 |
| At least one net per household (any type) | 3742 (95.5) |
| At least one ITN/LLIN per household | 1998 (50.9) |
| One net per two people (any type) | 2608 (66.5) |
| One ITN/LLIN per two people | 935 (23.8) |
| Access and utilization of ITN/LLIN | |
| Total number of household membersa | 13,592 |
| % of population with access to any bed net | 11,558 (85.0) |
| % of population with access to ITN/LLIN | 5723 (42.1) |
| % of population slept under an ITN/LLIN | 4799 (35.3) |
| % of population slept under an ITN/LLIN in those who have access to LLIN/ITN | 83.9% |
ITN=Insecticide treated net, LLIN = Long Lasting Insecticide Net
aIncludes individuals who slept in the household the previous night
Among the household members who slept last night (13592), only 42% had access to ITN/LLINs and only 35% used ITN/LLINs (Table 3). This result shows that high utilization of ITN/LLINs among those who had access to ITN/LLINs.
The proportion of children under 5 years (n = 1519) who slept under an ITN/LLIN the previous night was 45.3% while among pregnant women (n-178), this was 46.6% (data not tabulated).
Characteristics of the bed nets including their physical condition
Table 4 shows the characteristics of available bed nets at the household level. Less than half (41%) of all bed nets were ITN/LLINs. The main sources of LLINs were government (63.3%) and NGO’s (32.1%) (table not shown). Around 58% of the bed nets were 2-person size. Of all nets, 31.3% had holes or had already undergone repairs. In terms of insecticide treatment status, an estimated 52.9% were untreated and 38.9% of ITNs had not been treated for more than a year.
Table 4.
Characteristics of bed nets in households among migrant population in RAI project areas of Myanmar, 2014
| Characteristics | Total |
|---|---|
| Total bed nets | n = 6990 n (%) |
| Bed net type | |
| Non-LLIN | 4121 (58.9) |
| LLIN | 2869 (41.0) |
| Bed net size | 6967 |
| One person size | 675 (9.7) |
| One and half person size | 352 (5.1) |
| Two persons size | 4037 (57.9) |
| Family size | 1903 (27.3) |
| Bed net condition | 6943 |
| Good (no holes) | 4769 (68.7) |
| Repaired (no holes) | 578 (8.3) |
| Holes | 1596 (23.0) |
| Insecticide treatment status | 6922 |
| Untreated | 3647 (52.7) |
| LLIN | 2869 (41.5) |
| ITN | 406 (5.9) |
| Time since last insecticide treatment | 387 |
| Less than 6 months | 62 (16.0) |
| 6 months to 1 year | 186 (48.1) |
| > 1 year | 139 (35.9) |
ITN insecticide-treated net, LLIN long-lasting insecticide net
Missing and do not know categories omitted
Source of information on ITNs
Regarding the source of information on ITNs, health personnel including private providers were the major informers to the migrant workers (72.4%) followed by leaflets/brochures (8.5%), friends/family members/neighbors (8.2%), and posters (5.6%) (table not shown).
Table 5 shows the factors associated with the ownership of sufficient ITN/LLINs among the migrant population. The associated factors with the ownership of sufficient ITN/LLINs among migrants were state/region, household size, duration of residence since last time, and their intention to stay in the current place.
Table 5.
Factors associated with ownership of sufficient ITN/LLINs among the migrant population in RAI project areas of Myanmar, 2014
| Characteristics | Total | Sufficient ITN/LLIN | Crude OR (95% CI) | p value | Adjusted OR (95% CI) | p value |
|---|---|---|---|---|---|---|
| N | n (%) | |||||
| Tier | ||||||
| Tier 2 | 1737 | 302 (17.4) | 1 | 1 | ||
| Tier 1 | 2186 | 633 (29.0) | 1.9 (1.6–2.3) | < 0.001 | 1.0 (0.6–1.6) | 0.996 |
| Education | ||||||
| Illiterate | 346 | 68 (19.7) | 1 | 1 | ||
| Read and write/primary | 2900 | 713 (24.6) | 1.3 (1.0–1.8) | 0.043 | 1.1 (0.8–1.5) | 0.482 |
| Secondary school | 277 | 52 (18.8) | 0.9 (0.6–1.4) | 0.782 | 0.8 (0.5–1.3) | 0.443 |
| High school and above | 392 | 100 (25.5) | 1.4 (1.0–2.0) | 0.059 | 1.2 (0.8–1.8) | 0.372 |
| Occupation | ||||||
| Daily wage laborer | 1775 | 455 (25.6) | 1 | 1 | ||
| Agriculture/animal husbandry | 1026 | 208 (20.3) | 0.7 (0.6–0.9) | 0.001 | 0.8 (0.7–1) | 0.074 |
| Stone mining work/brick | 473 | 98 (20.7) | 0.8 (0.6–1.0) | 0.028 | 1.0 (0.8–1.4) | 0.94 |
| Other | 627 | 171 (27.3) | 1.1(0.9–1.3) | 0.422 | 1.0 (0.8–1.3) | 0.825 |
| State/region | ||||||
| Tanintharyi | 1175 | 309 (26.3) | 1 | 1 | ||
| Kachin | 242 | 18 (7.4) | 0.2 (0.1–0.4) | < 0.001 | 0.2 (0.1–0.3) | < 0.001* |
| Bago | 1119 | 286 (25.6) | 0.96 (0.8–1.2) | 0.686 | 0.9 (0.6–1.4) | 0.619 |
| Kayah | 251 | 15 (6.0) | 0.2 (0.1–0.3) | < 0.001 | 0.2 (0.1–0.3) | < 0.001* |
| Mon | 886 | 293 (33.1) | 1.4 (1.1–1.7) | 0.001 | 1.0 (0.8–1.3) | 0.917 |
| Kayin | 250 | 14 (5.6) | 0.2 (0.1–0.3) | < 0.001 | 0.2 (0.02–0.1) | < 0.001* |
| Number of household members | ||||||
| More than 6 | 647 | 71 (11.0) | 1 | 1 | ||
| 3–5 | 2091 | 448 (21.4) | 2.2 (1.7–2.9) | < 0.001 | 2.4 (1.8–3.2) | < 0.001* |
| 1–2 | 1185 | 416 (35.1) | 4.4 (3.3–5.8) | < 0.001 | 8.6 (6.2–11.6) | < 0.001* |
| Duration of residence since last time | ||||||
| 0–12 months | 1872 | 302 (16.1) | 1 | 1 | ||
| 13–24 months | 580 | 179 (30.9) | 2.3 (1.9–2.9) | < 0.001 | 2.4 (1.9–3.1) | < 0.001* |
| 25–36 months | 515 | 159 (30.9) | 2.3 (1.9–2.9) | < 0.001 | 2.4 (1.9–3.2) | < 0.001* |
| > 36 months | 705 | 251 (35.6) | 2.9 (2.4–3.5) | < 0.001 | 3.1 (2.4–4.1) | < 0.001* |
| Intention to stay | ||||||
| 0–6 months | 639 | 83 (13.0) | 1 | 1 | ||
| 6 months–1 year | 234 | 45 (19.2) | 1.6 (1.1–2.4) | 0.022 | 1.6 (1.0–2.4) | 0.044* |
| > 1 year | 585 | 146 (25.0) | 2.2 (1.7–3.0) | < 0.001 | 1.5 (1.0–2.0) | 0.031* |
| Not sure | 2454 | 657 (26.8) | 2.4 (1.9–3.1) | < 0.001 | 1.5 (1.2–2.0) | 0.003* |
*represents significant
Discussion
This is the first community-based study assessing access and utilization of bed nets among different types of migrant population in the Regional Artemisinin Resistance Initiative (RAI) project areas in Myanmar. The present study showed nearly 95% of households had access to bed net of any type, whereas only around half of all households had ITN/LLINs. About 35.3% of households actually slept under an ITN/LLIN last night. Thus, the study reports poor access to ITN/LLIN though utilization is high among those who have access to bed nets.
The major strengths of the study were that data were obtained from a large survey among migrant population in RAI areas, the response rate was high, the interviewers were well trained and supervised, and the subject is an identified national operational research priority. Data quality was ensured through double data entry and validation using EpiData entry software. We also adhered to STROBE guidelines for the reporting of observational studies [12].
The study had some limitations as well. The study did not explore the reasons as to why people do not use bed nets despite possessing them. Further qualitative studies are required to understand the reasons for the same.
The study findings have a number of policy and practice implications. Firstly, only half of the households had access to ITN/LLINs, which is the recommended type of bed net. This is much lower than the desired target of 80%. Migrant population is one of the most vulnerable with high risk for malaria due to their socio-cultural practices and occupation. This suggests the need for urgent attention and community distribution of ITN/LLINs to address the shortage of ITN/LLIN coverage in this vulnerable group. Among the vulnerable mobile population, only about one-third slept under an ITN/LLIN last night which is a matter of concern and warrants urgent attention.
Another large community-based survey in non-MARC areas of Myanmar showed that nearly 58% of households had access to at least one ITN/LLIN, only 24% had one ITN/LLIN per two people and about one-third of people slept under an ITN/LLIN [13]. These figures are similar to those obtained in the present study. This probably points to the fact that apart from the migrant population, there is also poor ownership and utilization of ITN/LLINs in the general population as well.
A study in Kachin region of Myanmar showed high coverage and usage rates of bed nets. The authors ascribed the success to the GFATM rounds for the China Malaria Programme, which distributed free LLINs through Health Poverty Action (HPA) in the region in the past 5 years (2008–2013) ensuring equity through active community participation [8]. Similarly, a report on several African countries showed high-utilization rates in areas with good access [14]. Another study in Myanmar among a small sample of migrant plantation workers reported high coverage, but low utilization of ITNs [7]. Previous studies in various African countries have reported low coverage/ownership and poor utilization of bed nets [15–18]. Few other studies have reported high coverage/ownership but poor utilization of bed nets [19–21]. Matovu et al. also highlighted pro-rich inequalities in ownership of ITNs which were much more pronounced in rural areas [18]. Thus, giving special attention to the poorest and the most vulnerable populations such as the migrants is essential to ensure universal access to ITN/LLINs.
Secondly, it was noted that mass media including television, radio, and newspapers have little role in disseminating information among these migrant workers. This might probably be due to their low-education level and poor socio-economic status leading to lack of access to health education messages through mass media such as radio, TV channels, and press media [7]. This has important implications while designing health promotion campaigns for this vulnerable group.
Thirdly, although the rates of ITN/LLIN use was higher among the children and pregnant women than the general population, only less than half of them (who constitute the high-risk groups for malaria) slept under an ITN/LLIN last night. Since malaria-related morbidity and mortality is highest in these groups [22], more focus and prioritization is mandated to ensure 100% coverage and utilization in these vulnerable subgroups. Studies in different settings have shown poor ownership and use of ITNs/LLINs among pregnant women [23–25] and under-five children [18]. However, in another study in Kachin region of Myanmar, children and pregnant females had higher use rate of ITNs/LLINs [8]. This was probably because of the health behavior and education interventions by the Chinese GFATM Malaria Programme. Under this program, children and pregnant females were prioritized and 390 sessions of community health education were delivered to promote the use of bed nets [8]. This suggests the need for increasing public awareness through community-based activities.
Fourthly, although the study reported poor access to ITNLLIN, there was high utilization of ITN/LLINs among those who had access to it. This shows a positive behavior towards usage of nets, thus pointing to the fact that access to bed-nets is the key barrier to its utilization. The NMCP should direct its resources towards better coverage of ITN/LLIN distribution.
Finally, the majority of available ITNs were either untreated or not treated for more than a year which makes it less effective than treated nets. This pushes the need for LLINs or continuous distribution of LLINs especially for the vulnerable groups, one such group being the migrants in RAI areas.
Conclusions
The study highlights poor ownership, access to, and utilization of ITN/LLINs among migrant population in RAI areas. But high utilization of ITN/LLINs among those who had access to ITN/LLINs in RAI areas indicates that the need of priority attention should be given to improving the LLIN distribution for migrant populations through effective delivery channels.
Acknowledgements
We would like to thank National Malaria Control Program (NMCP) for allowing the usage of this database. We also would like to express our gratitude to Global funds for giving fund for data collection.
Availability of data and material
Data are not available in public domain because they are currently being analyzed in related papers. However, data are available with the corresponding author (TMM) and will be made accessible on request at the following e-mail: themgmg.dr@gmail.com.
Funding
The data collection for this study was funded by the Global Fund.
Abbreviations
- ACT
Artemisinin-based combination therapy
- DMR
Department of Medical Research
- GMS
Greater Mekong Sub-region
- HPA
Health Poverty Action
- ITN
Insecticide-treated nets
- LLIN
Long-lasting insecticide nets
- MARC
Myanmar Artemisinin Resistance Containment
- MOHS
Ministry of Health and Sports
- NMCP
National Malaria Control Program
- RAI
Regional Artemisinin Resistance Initiative
- STROBE
The Strengthening the Reporting of Observational Studies in Epidemiology
- WHO
World Health Organization
Authors’ contributions
The work was conceived and designed by TMM, JPT, KTW, and TO. The field study and data entry were performed by TMM, SMO, and AT, and data analysis was done by TMM, SMO, and JPT. TMM, JPT, and KTW contributed to writing the paper. All authors read and approved the final manuscript.
Ethics approval
Ethics approval for the community-based survey used for this secondary analysis was already obtained from the Ethics Review Committee, Department of Medical Research, Myanmar. Ethics approval was also received from The Union Ethics Advisory Group (International Union against Tuberculosis and Lung Disease, Paris, France) (EAG number 104/16). We used secondary data, and therefore, informed consent was waived off by the ethical committee.
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.World Health Organization . Myanmar Artemisinin Resistance Containment Surveys: draft report. Myanmar: World Health Organization; 2012. [Google Scholar]
- 2.Cui L, Yan G, Sattabongkot J, Cao Y, Chen B, Chen X, et al. Malaria in the Greater Mekong Subregion: heterogeneity and complexity. Acta Trop. 2012;121:227–239. doi: 10.1016/j.actatropica.2011.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kyaw MP, Nyunt MH, Chit K, Aye MM, Aye KH, Aye MM, et al. Reduced susceptibility of plasmodium falciparum to artesunate in southern Myanmar. PLoS One. 2013;8:e57689. doi: 10.1371/journal.pone.0057689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Strategic Framework for Artemisinin Resistance Containment in Myanmar (MARC) 2011–2015. 2011.
- 5.World Health Organization. Achieving and maintaining universal coverage with long-lasting insecticidal nets for malaria control.
- 6.Ministry of Health . Union of Myanmar: National Strategic Plan Malaria Control Myanmar 2010–2015. Yangon: Ministry of Health; 2009. [Google Scholar]
- 7.Nyunt MH, Aye KM, Kyaw MP, Kyaw TT, Hlaing T, Oo K, et al. Challenges in universal coverage and utilization of insecticide-treated bed nets in migrant plantation workers in Myanmar. Malar J. 2014;13:211. doi: 10.1186/1475-2875-13-211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liu H, Xu J, Guo X, Havumaki J, Lin Y, Yu G, et al. Coverage, use and maintenance of bed nets and related influence factors in Kachin Special Region II, northeastern Myanmar. Malar J. 2015;14:212. doi: 10.1186/s12936-015-0727-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wai KT, Kyaw MP, Oo T, Zaw P, Nyunt MH, Thida M, et al. Spatial distribution, work patterns, and perception towards malaria interventions among temporary mobile/migrant workers in artemisinin resistance containment zone. BMC Public Health. 2014;14:463. doi: 10.1186/1471-2458-14-463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.World Health Organization . World Malaria Report 2015. Geneva: World Health Organization; 2015. [Google Scholar]
- 11.Florey L, Herrera S, Kilian A, Noor A, Carvajal L, Choi M, et al. Household survey indicators for malaria control. 2013. [Google Scholar]
- 12.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Bull World Health Organ. 2007;85:867–872. doi: 10.2471/BLT.07.045120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Maung TM, Oo T, Wai KT, Hlaing T, Owiti P, Kumar B, et al. Assessment of household ownership of bed nets in areas with and without artemisinin resistance containment measures in Myanmar. Infect Dis Poverty. 2018;7(1):19. doi: 10.1186/s40249-018-0399-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Koenker H, Ricotta E, Olapeju B. Insecticide-treated nets (ITN) access and use report. Baltimore, MD. PMI | VectorWorks Project, Johns Hopkins Center for Communication Programs. 2018.
- 15.Batisso E, Habte T, Tesfaye G, Getachew D, Tekalegne A, Kilian A, et al. A stitch in time: a cross-sectional survey looking at long lasting insecticide-treated bed net ownership, utilization and attrition in SNNPR. Ethiopia Malar J. 2012;11:183. doi: 10.1186/1475-2875-11-183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Biadgilign S, Reda A, Kedir H. Determinants of ownership and utilization of insecticide-treated bed nets for malaria control in eastern Ethiopia. J Trop Med. 2012;2012:235015. doi: 10.1155/2012/235015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Watiro AH, Awoke W. Insecticide-treated net ownership and utilization and factors that influence their use in Itang, Gambella region, Ethiopia: cross-sectional study. Risk Manag Healthc Policy. 2016;9:101–112. doi: 10.2147/RMHP.S104311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Matovu F, Goodman C, Wiseman V, Mwengee W. How equitable is bed net ownership and utilisation in Tanzania? A practical application of the principles of horizontal and vertical equity. Malar J. 2009;8:109. doi: 10.1186/1475-2875-8-109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stevens ER, Aldridge A, Degbey Y, Pignandi A, Dorkenoo MA, Hugelen-Padin J. Evaluation of the 2011 long-lasting, insecticide-treated net distribution for universal coverage in Togo. Malar J. 2013;12:162. doi: 10.1186/1475-2875-12-162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bennett A, Smith SJ, Yambasu S, Jambai A, Alemu W, Kabano A, et al. Household possession and use of insecticide-treated mosquito nets in Sierra Leone 6 months after a national mass-distribution campaign. PLoS One. 2012;7:e37927. doi: 10.1371/journal.pone.0037927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kateera F, Ingabire CM, Hakizimana E, Rulisa A, Karinda P, Grobusch MP, et al. Long-lasting insecticidal net source, ownership and use in the context of universal coverage: a household survey in eastern Rwanda. Malar J. 2015;14:390. doi: 10.1186/s12936-015-0915-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schantz-Dunn J, Nour NM. Malaria and pregnancy: a global health perspective. Rev Obstet Gynecol. 2009;2:186–192. [PMC free article] [PubMed] [Google Scholar]
- 23.Fuge TG, Ayanto SY, Gurmamo FL. Assessment of knowledge, attitude and practice about malaria and ITNs utilization among pregnant women in Shashogo District, Southern Ethiopia. Malar J. 2015;14:235. doi: 10.1186/s12936-015-0755-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pettifor A, Taylor E, Nku D, Duvall S, Tabala M, Meshnick S, et al. Bed net ownership, use and perceptions among women seeking antenatal care in Kinshasa, Democratic Republic of the Congo (DRC): opportunities for improved maternal and child health. BMC Public Health. 2008;8:331. doi: 10.1186/1471-2458-8-331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wagbatsoma VA, Aigbe EE. ITN utilization among pregnant women attending ANC in Etsako West Lga, Edo State, Nigeria. Niger J Clin Pract. 2010;13:144–148. [PubMed] [Google Scholar]


