Abstract
Objectives
Cardiovascular diseaseand heart failure (CHF) are leading causes of death in systemic lupus erythematosus (SLE). The underlying mechanisms for increased CHF in SLE are unclear but myocardial inflammation and lupus myocarditis (LM) may play a role. We propose that 18F-fluorodeoxyglucose–positron emission tomography (18F-FDG–PET)/CT can help diagnose LM.
Methods
This report describes eight patients with presumed LM; five patients were evaluated due to active cardiorespiratory symptoms and three patients were participating in a pilot study to determine the prevalence of subclinical myocarditis in SLE. Clinical characteristics, laboratory and cardiac testing including electrocardiography (ECG), transthoracic echocardiogram (TTE), coronary artery evaluation as well as 18F-FDG–PET/CT imaging are discussed.
Results
Four patients were African American and the others were Hispanic. Half presented with chest pain; 37% had dyspnoea and 25% were asymptomatic. The median SLE Disease Activity Index (SLEDAI-2K) was 5 (2–18) and SLICC Damage Index (SDI) 0.5 (0–5). The median troponin level was 0.08 ng/mL (0–0.9). The most common ECG findings were non-specific ST-T wave abnormalities (n=5). Fifty per cent of the patients had a decreased ejection fraction on TTE and all patients had diffuse myocardial FDG uptake on 18F-FDG–PET/CT consistent with myocardial inflammation.
Conclusion
This case series is the first to describe the use of 18F-FDG–PET/CT in the diagnosis of LM and discuss the clinical characteristics and cardiac findings of eight patients with LM supporting the role for cardiac 18F-FDG–PET/CT in its diagnosis.
Introduction
Systemic lupus erythematosus (SLE) is an autoimmune disease characterised by autoantibody-mediated systemic injury resulting in heterogeneous manifestations. Throughout the course of the disease, cardiac involvement occurs in over 50% of patients with SLE1–3 and every structure of the heart can be affected. Notably, cardiovascular disease (CVD) has become the leading cause of death in SLE.4 Epidemiological studies estimate a 2–9-fold increased risk of cardiovascular events in patients with lupusof all age groups with an increased prevalence of myocardial infarction, stroke and heart failure compared with the general population.5–8 Importantly, the excess in CVD seen in SLE is only partially accounted for by traditional CVD risk factors and SLE itself is an independent risk factor for CVD.9–13
Although the underlying mechanisms leading to CVD in lupus remain unclear, persistent systemic and local inflammation are the main proposed contributing factors.14–18 Lupus myocarditis (LM) is a recognised complication of SLE with a prevalence reported to be as high as 57% based on postmortem studies,19–21 and a 10% mortality described in case series at 3-year follow-up.22 However, the diagnosis of myocarditis in SLE remains challenging in clinical practice. LM is currently diagnosed clinically, supported by abnormalities noted on electrocardiograms (ECG) and transthoracic echocardiograms (TTE). As ECG and TTE findings are not sensitive or specific for myocarditis, the accuracy of this diagnosis is limited. Endomyocardial biopsies are considered the gold standard for diagnosing myocarditis, yet they are not routinely performed due to the related risk of the invasive procedure and associated potential sampling error. Furthermore, the sensitivity and specificity of the procedure in LM is unknown.23–25 As such, non-invasive imaging techniques to diagnose, characterise and provide prognostic data for LM have become a research priority.26 To date, studies using non-invasive imaging such as cardiac MRI (cMRI) have suggested that clinical diagnostic criteria for LM underdiagnose cases and that many patients with SLE have subclinical myocardial inflammation.27 28
Positron emission tomography (PET)/CT has emerged as a novel imaging modality for active inflammation, currently being evaluated in several rheumatic diseases.29–32 The ability of FDG to accumulate in inflammatory cells has made it a useful tool in measuring inflammation, and in particular in sarcoid myocarditis 18F-FDG–PET/CT is a more sensitive diagnostic test than cMRI.33–37 Given the lack of data on 18F-FDG–PET/CT imaging in the evaluation of myocardial inflammation in SLE, we describe eight patients with active myocardial inflammation on 18F-FDG–PET/CT scanning consistent with LM.
Methods
Patients
Eight patients with SLE are described in this case series. Five patients were diagnosed during their admission at Columbia University Medical Center, June 2014–March 2016 for cardiorespiratory symptoms. The remaining three patients were diagnosed as part of a pilot study of 10 participants to identify the prevalence of myocarditis in patients with SLE without clinical CVD. All patients were 18 years of age or older and met the 1997 American College of Rheumatology (ACR) classification criteria for SLE.38 The study was approved by the Columbia University Institution Review Board.
Outcome measure
18F-FDG PET/CT Myocardial uptake. Imaging was performed on an MCT 64 PET/CT scanner (Siemens Medical Solutions USA, Knoxville, Tennessee, USA). A low-dose CT transmission scan (120 kV, 25 mA) was obtained for attenuation correction of PET data. All patients were on a carbohydrate-free diet for 24 hours. Patients were injected with 10±0.1 mCi of 18F-FDG intravenously using an antecubital or dorsal forearm catheter. A list mode 3D PET scan was acquired for 10 min following a 90 min uptake period post-18F-FDG injection. Non-gated attenuation-corrected images were reconstructed yielding 3 mm effective resolution. Corridor 4DM software was used to visually assess myocardial 18FDG uptake as well as semiautomatically quantify mean radiotracer uptake in the myocardium. Quantification of inflammation by 18F-FDG PET/CT involved measurement of standardised uptake values (SUV) in the myocardium.
Clinical covariates
Demographics, comorbidities and smoking history were self-reported and collected from questionnaires and patient interview. Hypertension was defined as a systolic BP of ≥140 mm Hg, diastolic BP of ≥90 mm Hg at the time of the evaluation or antihypertensive medication use. Diabetes was defined as glycated haemoglobin (HbA1c) greater than 6.4% or use of diabetes medications. All medications were documented from patient interview and medical records. SLE disease duration was defined as the duration in years from the date of physician diagnosis. SLE disease activity was calculated using the Systemic Lupus Erythematosus Disease Activity Index 2000 (SLEDAI-2K).39 Disease damage was determined by the calculation of the Systemic Lupus International Collaborating Clinics (SLICC) damage index for SLE (SDI).40
Coronary artery disease (CAD)
In four patients, CAD was evaluated by the Agatston coronary artery calcium score.41 The remaining four patients underwent cardiac catheterisation.
Electrocardiography (ECG)
Twelve-lead ECGs (25 mm/s paper speed and 10 mm/mV amplitude) were performed and interpreted by board-certified cardiologists.
Transthoracic echocardiogram (TTE)
TTEs were performed by trained registered cardiac sonographers using conventional GE machines with commercially available software. End-diastolic and end-systolic frames, five anatomical landmarks (septal, lateral, anterior and inferior mitral annulus and apex of the left ventricle (LV)) were manually identified, and a semiautomated endocardial border detection was performed, followed by LV endocardium tracking throughout the cardiac cycle. LV end-diastolic and end-systolic volumes were indexed by body surface area. Doppler, 3-D echocardiography and contrast agents were used at the discretion of the sonographer. A normal ejection fraction (EF) was defined as >50%.
Laboratory covariates
Autoantibodies including antinuclear antibodies, anti-SSA/Ro, anti-SSB/La, anti-ds-DNA, anti-Smith, anti-RNP, antiphospholipid antibodies and other pertinent laboratories including complement levels (C3, C4), erythrocyte sedimentation rate (ESR), high-sensitivity C reactive protein, troponin and pro-beta-natriuretic peptide (pro-BNP) levels, were performed at the clinical laboratory at New York Presbyterian Hospital and the Core Laboratory of the Columbia University Irving Institute for Clinical and Translation Research.
Results
Patientscharacteristics
Patient demographics, clinical and SLE characteristics and supportive tests are depicted in table 1. Fifty per cent of the patients were Hispanic and 50% were African American. Six were women (75%). The mean age of the patients was 43 years and mean disease duration was 11 years. One patient had both diabetes and hypertension. One patient was a current smoker, two patients were prior smokers and five were never smokers. Five of the patients had major organ involvement: four had a diagnosis of lupus nephritis, one of which was active at the time of the diagnosis of myocarditis; one had neuropsychiatric lupus (NPSLE) in the past. None of the patients had antiphospholipid antibody syndrome.
Table 1.
Patient characteristics and case description
| Cardiac symptoms | ||||||
| Demographics | CVD risk factors | SLE characteristics | Laboratory data | ECG, echo and coronary evaluation (CAC or catheterisation) | Cardiac FDG PET findings | Treatment and follow -up (f/u) |
| 32-year-old male Hispanic | No symptoms Never smoker |
SLE × 5 years h/o NPSLE SLEDAI-2K=1 SDI=0 ANA, SSA, SSB, DNA on HCQ | C3—87; C4—28; DNA—25; ESR—11 CRP—3.5; Trop<0.01; Pro-BNP—NA | ECG—sinus tachycardia; Echo—EF 56%; CAC—17 | Diffuse FDG myocardial uptake | Prednisone 1 mg/kg, MMF 3 g/day 6-month f/u echo: EF 60% |
| 31-year-old female Hispanic | Chest pain, palpitations Former smoker |
SLE × 11 years h/o LN SLEDAI-2K=4 SDI=0 ANA, SSA, SSB, DNA on HCQ | C3—91; C4—14; DNA—9.9; ESR—7; CRP—0.4; Trop<0.01; Pro-BNP—41 | ECG—sinus tachycardia, RBBB; Echo—EF 60%; CAC—0 | Diffuse FDG myocardial uptake | Prednisone 1mg/kg, MMF 3 g/day 6-month f/u echo: EF 60% |
| 55-year-old female African American | Chest pain Former smoker, h/o lupus pericarditis |
SLE × 16 years h/o LN SLEDAI-2K=9 SDI=1 ANA, DNA on HCQ | C3—71; C4—10.5; DNA—38.8; ESR—6; CRP—85; Trop<0.01; Pro-BNP—820 | ECG—sinus tachycardia, non-specific ST-T changes; Echo—EF 20%, pericardial effusion, valvular abnormalities; Catheterisation—non-obstructive CAD | Diffuse FDG myocardial uptake | Methylprednisolone 1 g/day ×3 days, then prednisone 1 mg/kg Other—Metoprolol, carvedilol, valsartan 8-month f/u echo: EF 60% |
| 67-year-old male African American | Shortness of breath Never smoker, HTN, DM |
SLE × 20 years SLEDAI-2K=2 SDI=5 ANA, SSA on HCQ | C3—91; C4—26; DNA— <6.0; ESR— 596; CRP—19.6; Trop<0.01; Pro-BNP—NA | ECG—non-specific ST-T changes, RBBB; Echo—EF 30%, global hypokinesis, LV dilatation; Catheterisation—angiographically normal coronary arteries | Diffuse FDG myocardial uptake | Prednisone 1 mg/kg, MMF 3 g/day Other- carvedilol, amlodipine, valsartan, rosuvastatin, aspirin 13-month f/u cardiac FDG PET: EF 35%, diffuse FDG myocardial uptake decreased by 3 SUV units |
| 35-year-old female Hispanic | No symptoms Never smoker |
SLE x 2 years SLEDAI-2K=2 SDI=0 ANA, SSA, DNA on HCQ | C3—140; C4—33; DNA—60.7; ESR—29; CRP—2.6; Trop<0.01; Pro-BNP—NA | ECG—sinus tachycardia; Echo—EF 55%; CAC—0 | Diffuse FDG myocardial uptake | Prednisone 1 mg/kg, MMF 3 g/day 5-month f/u cardiac FDG PET: No FDG uptake. EF 62% |
| 47-year-old female African American | Shortness of breath Never smoker |
SLE × 17 years h/o LN SLEDAI-2K=18 SDI=2 ANA, DNA, Sm, RNP On HCQ | C3—62; C4—11; DNA—192.8; ESR—25; CRP—0.3; Trop<0.01; Pro-BNP—10235 | ECG—non-specific ST-T changes; Echo—EF 20%, global hypokinesis, left atrial enlargement; Catheterisation—angiographically normal coronary arteries | Diffuse FDG myocardial uptake | Prednisone 1 mg/kg, MMF 3 g/day. Other—carvedilol, nifedipine, aspirin, atorvastatin. Lost to follow-up |
| 37-year-old female African American | Chest pain Never smoker |
SLE × 9 years h/o LN SLEDAI-2K=12 SDI=2 ANA, DNA, Sm, RNP On HCQ | C3—52; C4—0; DNA—1098.2; ESR—52; CRP—12; Trop—0.75; Pro-BNP—NA | ECG—non-specific ST-T changes; Echo—EF 40%, wall motion abnormality, pericardial effusion; Catheterisation—mid LAD 70% occlusion and 100% D1 occlusion | Diffuse FDG myocardial uptake | Prednisone 1mg/kg, Cyclophosphamide 500mg/m2 intravenous monthly Other—carvedilol, hydralazine, isosorbide mononitrate, aspirin, atorvastatin 6-month f/u echo: EF 50%, impaired LV relaxation. No wall motion abnormality |
| 42-year-old female Hispanic | Chest pain Current smoker |
SLE × 7 years SLEDAI-2K=6 SDI=0 ANA, SSA, SSB, DNA, Sm On HCQ | C3—82; C4—12; DNA—130.1; ESR—77; CRP—0.6; Trop<0.01; Pro-BNP—NA | ECG—sinus tachycardia, non-specific ST-T changes; Echo—EF 50%, pericardial effusion, valvular abnormality; CAC—0 | Diffuse FDG myocardial uptake | Prednisone 1 mg/kg, MMF 3 g/day Other—metoprolol, atorvastatin 6-month f/u echo: EF 55%, impaired LV relaxation |
Reference values: DNA≤24.9 IU/mL; C3 (80–162 mg/dL); C4 (14–47 mg/dL); ESR (0–20 mm/hour); CRP (<10 mg/L); Troponin<0.01 ng/mL; pro-BNP<178 pg/mL.
ANA, antinuclear antibody; CAC, coronary artery calcium; CAD, coronary artery disease; CRP, C reactive protein; CVD, cardiovascular disease; D1, first diagonal branch. DNA, anti-ds-DNA antibody; ECG, electrocardiogram; Echo, echocardiogram; EF, ejection fraction; ESR, erythrosedimentation rate; FDG PET, fluorodeoxyglucose positron emission tomography; HCQ, hydroxychloroquine; h/o, history of; LAD, left anterior descending artery; LN, lupus nephritis; LV, left ventricle; MMF, mycophenolate mofetil; NA, not available; NPSLE, neuropsychiatric SLE; pro-BNP, pro-beta natriuretic peptide; RBBB, right bundle branch block; RNP, anti-ribonucleoprotein antibody; SDI, Systemic Lupus International Collaborating Clinics (SLICC) damage index for SLE; SLE, systemic lupus erythematosus; SLEDAI-2K, SLE Disease Activity Index 2000; Sm, anti-Smith antibody; SSA, anti-SSA antibody; SSB, anti-SSB antibody; SUV, standardised uptake values; Trop, troponin.
Clinicalpresentation
Four patients complained of chest pain, one of dyspnoea, one had both chest pain and dyspnoea and two did not have any cardiac or respiratory symptoms. Five patients were diagnosed at the time of admission for acute lupus flare and cardiac symptoms; the other three were participants in a study to evaluate the prevalence of subclinical myocarditis and on further questioning one patient acknowledged shortness of breath (table 1).
Disease activity and pertinentlaboratories
The median SLEDAI-2K was 5 (2–18) and the SLICC SDI score was 0.5 (0–5). Median C3 level was 84 (64–91) and C4 was 13 (11–27). ESR was elevated in six patients with a median level of 27 (8–52) and an elevated high-sensitivity CRP was noted in five patients with a median of 3 (0.5–17). Troponin and pro-BNP levels were significantly elevated in one patient (table 1).
Cardiac testing
The most common ECG findings were non-specific ST-T wave abnormalities (n=5) and sinus tachycardia (n=5). Right bundle branch block (n=2) and left atrial dilatation (n=1) were also noted. On TTE, half of the patients had a decreased EF. The mean EF was 41% (20%–60%). Three patients had pericardial effusions and two patients had global hypokinesis. Three of the four patients evaluated by Agatston coronary artery calcium scoring had a measurement of 0; the remaining patient had a score of 17, not clinically significant for atherosclerosis. The other four patients underwent coronary artery catheterisation: three had angiographically normal coronary arteries and one had 70% stenosis of the left anterior descending artery and 100% occlusion of the first diagonal branch (D1); the latter was diagnosed with a non-ST elevation myocardial infarction (NSTEMI) in addition to active myocarditis. However, the contribution of the D1 branch occlusion versus the active myocarditis to the troponin elevation and depressed EF could not be accurately ascertained (table 1). One patient had an endomyocardial biopsy that showed non-specific changes: preserved myocardial fibres with mild hypertrophic changes and increased cellular organelles consistent with non-specific mild myocardial hypertrophy.
On 18F-FDG–PET/CT imaging, all patients had diffuse myocardial uptake consistent with diffuse inflammation and suggestive of a diagnosis of myocarditis, including the patient with a concomitant NSTEMI (figure 1).
Figure 1.
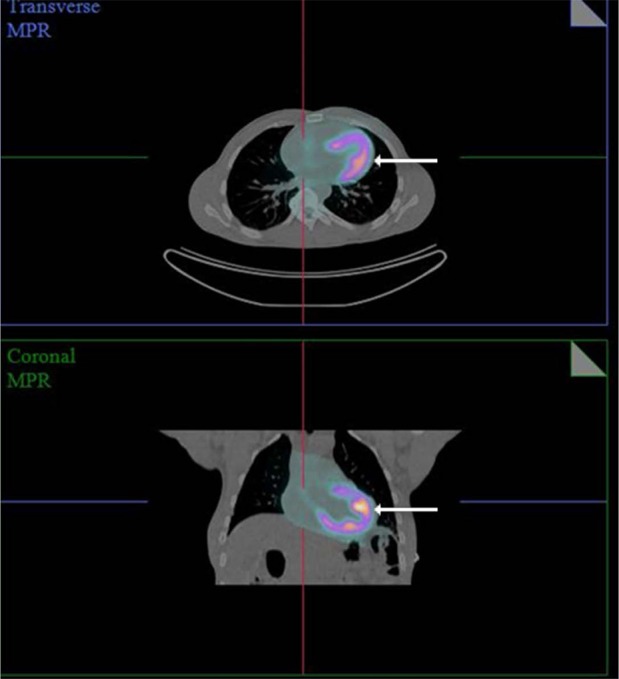
18F-fluorodeoxyglucose positron emission tomography/CT showing diffuse myocardial FDG uptake (arrows) on a transverse and coronal view in a patient with SLE described in this series. FDG, fluorodeoxyglucose; SLE, systemic lupus erythematosus.
Treatment
All patients were treated with high-dose steroids (1 mg/kg of prednisone). One patient also received 3 days of pulse solumedrol intravenous (1000 mg). All patients were treated with immunosuppressive therapy: 7/8 with mycophenolate mofetil with a goal dose of 3 g per day in divided doses; 1/8 with cyclophosphamide at 500 mg/m2 intravenous monthly due to coexisting lupus nephritis which had been previously non-responsive to mycophenolate mofetil (table 1).
Follow up
Two patients had follow-up 18F-FDG–PET/CT imaging: one had no myocardial uptake after 5 months, while the other showed persistent diffuse uptake/inflammation but with decrease in FDG uptake by an SUV factor of 3 at 13 months. Five had a follow-up TTE within 6–8 months: mean EF was 57% (range 50%–60%) and all had normal wall motion. Two of these five patients had impaired LV relaxation of unclear significance (present on initial TTE). One patient was lost to follow-up (table 1).
Discussion
This case series describes eight patients with 18F-FDG–PET/CT myocardial uptake suggestive of LM. The clinical presentation and characteristics of our patients with LM were non-specific and variable, emphasising the need for additional sensitive testing for LM and supporting a role for cardiac 18F-FDG–PET/CT for the early diagnosis and prompt treatment of this condition.
CVD is the leading cause of death in SLE.4 It has been estimated that patients with SLE aged 35–44 have a greater than 50-fold increased relative risk of myocardial infarction compared with age matched controls, and that in general, patients with SLE have up to a 7–10-fold greater relative risk of angina, myocardial infarction and stroke.8 10 13 42 This excess in cardiovascular risk is not fully explained by the increase in traditional risk factors, suggesting that SLE-specific factors play a central role.12
The increased cardiovascular risk in SLE is considered multifactorial and potentiated by a combination of systemic and local inflammation.14–18 In idiopathic subclinical myocarditis, local inflammation and endothelial activation lead to microvascular disease and dysfunction, promoting accelerated atherosclerosis.43 While LM is a recognised complication of SLE, its true prevalence is unknown as its diagnosis remains challenging. A recent case series of 29 patients with LM reported a 10% mortality at 3-year follow-up, stressing the importance of recognising and treating this lupus manifestation. 22 Currently, LM is diagnosed based on clinical suspicion, abnormalities of ECG and echocardiograms44–47 and lack of an alternative diagnosis. Zawadowski et al46 described 24 patients with LM and similar to our findings, the most common ECG abnormalities were non-specific ST changes (70%) and sinus tachycardia (63%), while 78% had a reduced EF on TTE. However, these findings are non-specific for LM. Although endomyocardial biopsy is considered the gold standard, its use in LM is unclear and it has been noted to have poor sensitivity and specificity. Sampling error and interventional risk often outweigh the benefits of the procedure23 25 resulting in ambiguity in both the diagnosis and treatment of this condition.
A recent interest has emerged in investigating the utility of non-invasive imaging techniques to further characterise myocarditis in lupus. Refined imaging modalities are more sensitive and inform on cardiac morphology and function and help assist in prognostication.24 26 Two recent studies have assessed the cMRI findings of patients with lupusin association with disease activity. Mavrogeni et al studied patients with active SLE without specific cardiovascular complaints and compared their findings to a commonly used clinical criteria for the diagnosis of acute myocarditis. While 5/20 patients with SLE fulfilled clinical criteria for myocarditis, cMRI was found to be positive in 16/20. Interestingly, of those with cMRI-proven myocarditis who underwent endomyocardial biopsy, only 3/7 had positive immunohistology.27 In addition, Zhang et al compared patients with inactive SLE (SLEDAI <3) with healthy controls using T2 time values on T2 cMRI mapping sequences,28 which have been shown to detect myocardial oedema and have high sensitivity and specificity for acute inflammation detection (94 and 97%, respectively).24 Despite being clinically quiescent, the SLE group was found to have T2 times significantly higher than controls suggesting the occurrence of subclinical myocarditis in patients with clinically inactive SLE with preserved myocardial contractility.28 Our study reflects Zhang’s findings in that our case series includes patients with SLE without cardiac symptoms that were found to have active myocardial uptake on FDG PET. While data on treating subclinical myocarditis are lacking, the two patients in our series without active cardiac symptoms were treated with steroids and immunosuppressants based on the acknowledgement of the borderline normal EFs, expert opinion and patient preference. Although the clinical implications of subclinical myocarditis in lupus remain unknown, these findings raise awareness for the need of additional identifiers of patients with SLE at risk for development of myocarditis as well as longitudinal follow up to evaluate its prognosis and associated risk for the development of cardiovascular events.
The use of 18F-FDG–PET/CT in cardiovascular inflammatory diseases has been best described in the setting of sarcoidosis. Comparable to LM, cardiac sarcoid involvement can be subclinical and have non-specific findings on ECG and echocardiogram.48 49 In cardiac sarcoidosis, FDG-PET has been shown to have equivalent or higher sensitivity to delayed enhancement cMRI in detecting active lesions.50 By targeting the increased glucose uptake of infiltrating granulocytes and tissue macrophages, FDG PET/CT has been shown to delineate inflammation with high sensitivity. Hence, the myocardial FDG uptake of the patients described in this series is likely to represent cardiac inflammation. Additional advantages of 18F-FDG–PET/CT imaging include its feasibility for patients with renal dysfunction and metal implants and having shorter time-frames than MRI studies. Furthermore, 18F-FDG–PET/CT provides quantitative measures of inflammation in the form of SUV that allow objective interval change assessments.51
To our knowledge, this is the first case series of lupus myocardial inflammation diagnosed by 18F-FDG–PET/CT scanning. Limitations include the small sample size, lack of pathological confirmation and lack of follow-up 18F-FDG PET/CT for all cases.
In conclusion, we describe a case series of patients with lupus with myocardial 18F-FDG–PET/CT uptake consistent with LM. Observational studies are needed to evaluate the sensitivity, specificity and overall clinical impact of this imaging modality in LM.
Footnotes
Contributors: All authors contributed to all phases of the manuscript writing.
Funding: Funding for this project was provided in part by the Rheumatology Research Foundation Scientist Development Award CU13-2392 (LGP).
Competing interests: None declared.
Patient consent: Not required.
Ethics approval: Columbia University.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data statement: All available data can be obtained by contacting the corresponding author.
References
- 1. D’Cruz D, Khamashta M, Hughes GRV. Cardiovascular manifestation of systemic lupus erythematosus Lupus erythematosus. Philadelphia: Lippincott Williams & Wilkins, 2001. [Google Scholar]
- 2. Doria A, Iaccarino L, Sarzi-Puttini P, et al. . Cardiac involvement in systemic lupus erythematosus. Lupus 2005;14:683–6. 10.1191/0961203305lu2200oa [DOI] [PubMed] [Google Scholar]
- 3. Moder KG, Miller TD, Tazelaar HD. Cardiac involvement in systemic lupus erythematosus. Mayo Clin Proc 1999;74:275–84. 10.4065/74.3.275 [DOI] [PubMed] [Google Scholar]
- 4. Knight JS, Kaplan MJ. Cardiovascular disease in lupus: insights and updates. Curr Opin Rheumatol 2013;25:597–605. 10.1097/BOR.0b013e328363eba3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bartels CM, Buhr KA, Goldberg JW, et al. . Mortality and cardiovascular burden of systemic lupus erythematosus in a US population-based cohort. J Rheumatol 2014;41:680–7. 10.3899/jrheum.130874 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bengtsson C, Ohman ML, Nived O, et al. . Cardiovascular event in systemic lupus erythematosus in northern Sweden: incidence and predictors in a 7-year follow-up study. Lupus 2012;21:452–9. 10.1177/0961203311425524 [DOI] [PubMed] [Google Scholar]
- 7. Hak AE, Karlson EW, Feskanich D, et al. . Systemic lupus erythematosus and the risk of cardiovascular disease: results from the nurses' health study. Arthritis Rheum 2009;61:1396–402. 10.1002/art.24537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Hesselvig JH, Ahlehoff O, Dreyer L, et al. . Cutaneous lupus erythematosus and systemic lupus erythematosus are associated with clinically significant cardiovascular risk: a Danish nationwide cohort study. Lupus 2017;26:1–6. 10.1177/0961203316651739 [DOI] [PubMed] [Google Scholar]
- 9. Westerweel PE, Luyten RK, Koomans HA, et al. . Premature atherosclerotic cardiovascular disease in systemic lupus erythematosus. Arthritis Rheum 2007;56:1384–96. 10.1002/art.22568 [DOI] [PubMed] [Google Scholar]
- 10. Manzi S, Meilahn EN, Rairie JE, et al. . Age-specific incidence rates of myocardial infarction and angina in women with systemic lupus erythematosus: comparison with the Framingham Study. Am J Epidemiol 1997;145:408–15. 10.1093/oxfordjournals.aje.a009122 [DOI] [PubMed] [Google Scholar]
- 11. Roman MJ, Shanker BA, Davis A, et al. . Prevalence and correlates of accelerated atherosclerosis in systemic lupus erythematosus. N Engl J Med 2003;349:2399–406. 10.1056/NEJMoa035471 [DOI] [PubMed] [Google Scholar]
- 12. Esdaile JM, Abrahamowicz M, Grodzicky T, et al. . Traditional Framingham risk factors fail to fully account for accelerated atherosclerosis in systemic lupus erythematosus. Arthritis Rheum 2001;44:2331–7. [DOI] [PubMed] [Google Scholar]
- 13. Bessant R, Hingorani A, Patel L, et al. . Risk of coronary heart disease and stroke in a large British cohort of patients with systemic lupus erythematosus. Rheumatology 2004;43:924–9. 10.1093/rheumatology/keh213 [DOI] [PubMed] [Google Scholar]
- 14. Hong J, Maron DJ, Shirai T, Weyand C, et al. . Accelerated atherosclerosis in patients with chronic inflammatory rheumatologic conditions. Int J Clin Rheumtol 2015;10:365–81. 10.2217/ijr.15.33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Shoenfeld Y, Gerli R, Doria A, et al. . Accelerated atherosclerosis in autoimmune rheumatic diseases. Circulation 2005;112:3337–47. 10.1161/CIRCULATIONAHA.104.507996 [DOI] [PubMed] [Google Scholar]
- 16. Willerson JT, Ridker P. Inflammation as a cardiovascular risk factor. Circulation 2004;109(21_suppl_1):II-2–0. 10.1161/01.CIR.0000129535.04194.38 [DOI] [PubMed] [Google Scholar]
- 17. Frostegård J. Atherosclerosis in patients with autoimmune disorders. Arterioscler Thromb Vasc Biol 2005;25:1776–85. 10.1161/01.ATV.0000174800.78362.ec [DOI] [PubMed] [Google Scholar]
- 18. Hansson GK, Hermansson A. The immune system in atherosclerosis. Nat Immunol 2011;12:204–12. 10.1038/ni.2001 [DOI] [PubMed] [Google Scholar]
- 19. Bulkley BH, Roberts WC. The heart in systemic lupus erythematosus and the changes induced in it by corticosteroid therapy. A study of 36 necropsy patients. Am J Med 1975;58:243–64. 10.1016/0002-9343(75)90575-6 [DOI] [PubMed] [Google Scholar]
- 20. Bidani AK, Roberts JL, Schwartz MM, Lewis E, et al. . Immunopathology of cardiac lesions in fatal systemic lupus erythematosus. Am J Med 1980;69:849–58. 10.1016/S0002-9343(80)80010-6 [DOI] [PubMed] [Google Scholar]
- 21. Roberts WC, High ST. The heart in systemic lupus erythematosus. Curr Probl Cardiol 1999;24:1–56. 10.1016/S0146-2806(99)90019-1 [DOI] [PubMed] [Google Scholar]
- 22. Thomas G, Cohen Aubart F, Chiche L, Amoura Z, et al. . Lupus myocarditis: initial presentation and longterm outcomes in a multicentric series of 29 patients. J Rheumatol 2017;44:24–32. 10.3899/jrheum.160493 [DOI] [PubMed] [Google Scholar]
- 23. Wijetunga M, Rockson S. Myocarditis in systemic lupus erythematosus. Am J Med 2002;113:419–23. 10.1016/S0002-9343(02)01223-8 [DOI] [PubMed] [Google Scholar]
- 24. Greulich S, Ferreira VM, Dall'Armellina E, Mahrholdt H, et al. . Myocardial inflammation-are we there yet? Curr Cardiovasc Imaging Rep 2015;8:6 10.1007/s12410-015-9320-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Cooper LT, Baughman KL, Feldman AM, et al. . The role of endomyocardial biopsy in the management of cardiovascular disease: a scientific statement from the American Heart Association, the American College of Cardiology, and the European Society of Cardiology. Endorsed by the heart failure society of America and the heart failure association of the european society of cardiology. J Am Coll Cardiol 2007;50:1914–31. 10.1016/j.jacc.2007.09.008 [DOI] [PubMed] [Google Scholar]
- 26. Bohkari S. FDG-PET is a superior tool in the diagnosis and management of cardiac sarcoid. American college of cardiology expert review. http://www.acc.org/latest-in-cardiology/articles/2017/04/10/08/43/fdg-pet-is-a-superior-tool
- 27. Mavrogeni S, Bratis K, Markussis V, et al. . The diagnostic role of cardiac magnetic resonance imaging in detecting myocardial inflammation in systemic lupus erythematosus. Differentiation from viral myocarditis. Lupus 2013;22:34–43. 10.1177/0961203312462265 [DOI] [PubMed] [Google Scholar]
- 28. Zhang Y, Corona-Villalobos CP, Kiani AN, Petri M, et al. . Myocardial T2 mapping by cardiovascular magnetic resonance reveals subclinical myocardial inflammation in patients with systemic lupus erythematosus. Int J Cardiovasc Imaging 2015;31:389–97. 10.1007/s10554-014-0560-3 [DOI] [PubMed] [Google Scholar]
- 29. Morgenstern R, Amigues I, Giles JT, et al. . Coronary artery inflammation in rheumatoid arthritis using fluorine-18 fluorodeoxyglucose positron emission tomography. J Clin Rheumatol 2017;23:454–5. 10.1097/RHU.0000000000000603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Geraldino-Pardilla L, Zartoshti A, Ozbek AB, et al. . Arterial inflammation detected with 18 F-Fluorodeoxyglucose-positron emission tomography in rheumatoid arthritis. Arthritis Rheumatol 2018;70:30–9. 10.1002/art.40345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Glaudemans AW, de Vries EF, Galli F, et al. . The use of (18)F-FDG-PET/CT for diagnosis and treatment monitoring of inflammatory and infectious diseases. Clin Dev Immunol 2013;2013:623036 10.1155/2013/623036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Yamashita H, Kubota K, Mimori A. Clinical value of whole-body PET/CT in patients with active rheumatic diseases. Arthritis Res Ther 2014;16:423 10.1186/s13075-014-0423-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Yamagishi H, Shirai N, Takagi M, et al. . Identification of cardiac sarcoidosis with (13)N-NH(3)/(18)F-FDG PET. J Nucl Med 2003;44:1030–6. [PubMed] [Google Scholar]
- 34. Juneau D, Erthal F, Alzahrani A, Chow BJ, et al. . Systemic and inflammatory disorders involving the heart: the role of PET imaging. Q J Nucl Med Mol Imaging 2016;60:383–96. [PubMed] [Google Scholar]
- 35. Okumura W, Iwasaki T, Toyama T, et al. . Usefulness of fasting 18F-FDG PET in identification of cardiac sarcoidosis. J Nucl Med 2004;45:1989–98. [PubMed] [Google Scholar]
- 36. Ohira H, Tsujino I, Ishimaru S, et al. . Myocardial imaging with 18F-fluoro-2-deoxyglucose positron emission tomography and magnetic resonance imaging in sarcoidosis. Eur J Nucl Med Mol Imaging 2008;35:933–41. 10.1007/s00259-007-0650-8 [DOI] [PubMed] [Google Scholar]
- 37. Mehta D, Lubitz SA, Frankel Z, et al. . Cardiac involvement in patients with sarcoidosis: diagnostic and prognostic value of outpatient testing. Chest 2008;133:1426–35. 10.1378/chest.07-2784 [DOI] [PubMed] [Google Scholar]
- 38. Hochberg MC. Updating the American college of rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis & Rheumatism 1997;40:1725 10.1002/art.1780400928 [DOI] [PubMed] [Google Scholar]
- 39. Gladman DD, Ibañez D, Urowitz MB. Systemic lupus erythematosus disease activity index 2000. J Rheumatol 2002;29:288–91. [PubMed] [Google Scholar]
- 40. Gladman DD, Urowitz MB, Goldsmith CH, Sturfelt G, et al. . The reliability of the systemic lupus international collaborating clinics/american college of rheumatology damage index in patients with systemic lupus erythematosus. Arthritis Rheum 1997;40:809–13. 10.1002/art.1780400506 [DOI] [PubMed] [Google Scholar]
- 41. Agatston AS, Janowitz WR, Hildner FJ, Detrano R, et al. . Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol 1990;15:827–32. 10.1016/0735-1097(90)90282-T [DOI] [PubMed] [Google Scholar]
- 42. Aviña-Zubieta JA, To F, Vostretsova K, et al. . Risk of myocardial infarction and stroke in newly diagnosed systemic lupus erythematosus: a general population-based study. Arthritis Care Res 2017;69:849–56. 10.1002/acr.23018 [DOI] [PubMed] [Google Scholar]
- 43. Schwartz T, Diederichsen LP, Lundberg IE, et al. . Cardiac involvement in adult and juvenile idiopathic inflammatory myopathies. RMD Open 2016;2:e000291 10.1136/rmdopen-2016-000291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Law WG, Thong BY, Lian TY, et al. . Acute lupus myocarditis: clinical features and outcome of an oriental case series. Lupus 2005;14:827–31. 10.1191/0961203305lu2228oa [DOI] [PubMed] [Google Scholar]
- 45. Apte M, McGwin G, Vilá LM, et al. . Associated factors and impact of myocarditis in patients with SLE from LUMINA, a multiethnic US cohort (LV). [corrected]. Rheumatology 2008;47:362–7. 10.1093/rheumatology/kem371 [DOI] [PubMed] [Google Scholar]
- 46. Zawadowski GM, Klarich KW, Moder KG, et al. . A contemporary case series of lupus myocarditis. Lupus 2012;21:1378–84. 10.1177/0961203312456752 [DOI] [PubMed] [Google Scholar]
- 47. Zhang L, Zhu YL, Li MT, et al. . Lupus myocarditis: a case-control study from China. Chin Med J 2015;128:2588–94. 10.4103/0366-6999.166029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. James OG, Christensen JD, Wong TZ, et al. . Utility of FDG PET/CT in inflammatory cardiovascular disease. Radiographics 2011;31:1271–86. 10.1148/rg.315105222 [DOI] [PubMed] [Google Scholar]
- 49. Brigden W, Bywaters EGL, Lessof MH, et al. . The heart in systemic lupus erythematosus. Heart 1960;22:1–16. 10.1136/hrt.22.1.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Blankstein R, Osborne M, Naya M, et al. . Cardiac positron emission tomography enhances prognostic assessments of patients with suspected cardiac sarcoidosis. J Am Coll Cardiol 2014;63:329–36. 10.1016/j.jacc.2013.09.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Skali H, Schulman AR, Dorbala S. 18F-FDG PET/CT for the assessment of myocardial sarcoidosis. Curr Cardiol Rep 2013;15:352–70. 10.1007/s11886-013-0370-6 [DOI] [PMC free article] [PubMed] [Google Scholar]


