Abstract
Objective
The aim of this study was to assess utilization pattern of surgical antibiotic prophylaxis in surgical wards of Dil Chora Referral Hospital.
Results
Prophylactic antibiotics were given in all surgical procedures. More than half of the participants 206(53.6%) were given Ceftriaxone while combination of Ceftriaxone and Metronidazole were used for 159(41.4%) patients. The most common procedure (88.3%), appendectomy, was managed with combination of Ceftriaxone and Metronidazole while the remaining was on Ceftriaxone. Hernia repair, another common procedure seen in this ward, was majorly managed by combination of Ceftriaxone and Metronidazole (60.7%) while the rest were on ceftriaxone alone. In general, inconsistence in antibiotic selection for different types of surgical procedures was seen. The surgical prophylactic antibiotics should be prescribed according to the international guidelines.
Electronic supplementary material
The online version of this article (10.1186/s13104-018-3629-6) contains supplementary material, which is available to authorized users.
Keywords: Surgical site infection, Surgical prophylaxis, Antibiotics
Introduction
Surgical site infection (SSI) is defined as a proliferation of pathogenic microorganisms which develops in an incision site either within the skin and subcutaneous fat (superficial) and muscular facial layers (deep) or in an organ or cavity within 30 days after operation [1]. SSI is one of major complication of surgical procedures and represents a significant burden with regard to patient’s morbidity, mortality and hospital costs [2].
Surgical antibiotic prophylaxis (SAP) is administration of short course of antimicrobial agent prior to surgery to prevent SSI [3, 4]. There is ample evidence on the effectiveness SAP for prevention of SSI for most of surgical procedures [5–8]. However, for optimum prophylaxis, SAP should be used appropriately by considering the possible pathogen, pharmacokinetic of the drug, timing and route of administration, patient and procedure related factors [9].
Despite the evidence of the effectiveness of the appropriate use of surgical antimicrobial prophylaxis, its use is often found to be inappropriate. Report indicates that between 30 and 90% of this antibiotics prophylaxis use is inappropriate [10, 11]. Inappropriate use specifically in the area of the antimicrobial selection, timing and the duration of the antimicrobial prophylaxis were commonly observed [12–14]. Inappropriate usage could leads to increased hospital costs, emergence of resistant microorganisms, and super-infections and increased adverse drug reaction [15].
In developing countries, antimicrobials expense share higher budget compared to the other drug category. Antibiotics are one of the commonly used drug category in surgical procedures. However, regardless of its widespread use, very little is known about how these antimicrobials are being used particularly for prophylaxis of SSI and there were no similar studies conducted before in Dilchora Referral Hospital (DCRH). Therefore, the aim of this study is to assess utilization pattern of surgical antibiotic prophylaxis in surgical wards in DCRH.
Main text
Methods
This study was conducted at DCRH, Dire Dawa city administration, which is 526 km East of the capital of Ethiopia, Addis Ababa from January 2017 to June 2017. DCRH, the only referral hospital in the city, provides general outpatient, inpatient and emergency services for more than 45,000 populations in Dire Dawa administrative city population and nearby communities. According to 2016 annual report of the hospital, about 611 surgical procedures were performed in this hospital.
Facility based retrospective cross sectional study design was used to assess the utilization pattern of SAP in surgical wards of DCRH. Medications records of all patients admitted in surgery ward and who underwent surgical procedures were included in the study. In order to avoid difficulty in distinguishing prolonged prophylaxis from post-operative infection treatment, all dirty/infected wounds and those patients who had receive therapeutic antibiotic before the surgical procedure were excluded from the study. In addition, the documents that do not contain relevant information were excluded from the study.
Sample size was determined by using single population formula considering the P value of 50%, CI of 95% and marginal error of 5% giving total sample size of 384. The patient cards were selected by using systematic random sampling technique using calculated K-value (total clients in past 5 years divided by sample size). The data extraction format was developed and pre-tested and subsequently modified to ensure that the data would provide valid information. All relevant data was retrieved from patient’s medical records. Details of patient’s record including age, sex, admission diagnosis, type of surgery, wound class, and details of antibiotic prophylaxis including antibiotic choice, administration route, dosage form, dose and duration was retrieved and recorded (Additional file 1).
In the processing of data, each recorded data from the study participant’s card was labeled on the study participant’s checklist then the information found from the checklist format were cross checked by the data collectors and pharmacists in DCRH. The processed data was analyzed by using SPSS version 20 for compilation, summarization and comparisons of the numbers. Then frequency and percentage of the findings was calculated against each variable and the total study subjects.
Results
Sociodemographic characteristics
A total of 384 patient cards were reviewed. The majority 159 (41.4%) of the patients were in age group of 31–65 years and just over half of the subjects 208 (51.2%) were male. Many of the subjects 228 (59.4%) were from urban areas and over one-third 148 (38.5%) had attended college and above while 115 (29.9%) were illiterate as shown in Table 1.
Table 1.
Socio-demographic characteristic of study participants assessed for surgical site infection prophylaxis in Dil Chora Referral Hospital, Eastern Ethiopia 2017 (n = 384)
| Variables | Number(%) |
|---|---|
| Age | |
| 1–10 | 35(9.1) |
| 11–30 | 153(39.8) |
| 31–65 | 159(41.4) |
| Above 65 | 37(9.6) |
| Sex | |
| Male | 208(54.2) |
| Female | 176(45.8) |
| Religion | |
| Orthodox | 153(39.8) |
| Muslim | 180(46.9) |
| Protestant | 51(13.3) |
| Residence | |
| Urban | 228(59.4) |
| Rural | 156(40.6) |
| Educational status | |
| Illiterate | 115(29.9) |
| Primary | 55(14.3) |
| Secondary | 66(17.2) |
| College and above | 148(38.5) |
Medical and surgical history of patients underwent surgery
Regarding the types of surgical procedure performed, appendectomy was leading procedure accounting about quarter (25.52%) of the procedure done in the ward followed by hernia repair (16.67%). Common procedures performed in DCRH are displayed in Fig. 1.
Fig. 1.
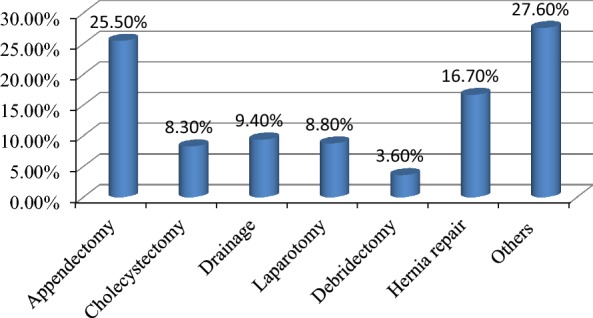
Type of surgical procedure Performed in Dil Chora Referral Hospital, Eastern Ethiopia, 2017 (n = 384). Others: Urology, head and neck, gynecology/obstetrics and vascular
Concerning the types of wound, a large number of subjects 279 (72.7%) had clean surgery followed by 82 (21.4%) clean contaminated wound. The contaminated wound type was accounted a few 23(5.9%). Preoperative length of stay were also reviewed and just over half of subjects 195(50.8%) had emergency surgery while the remaining went through elective surgery.
Surgical antibiotics usage
All patients were given prophylactic antibiotics. Concerning commonly employed antibiotics, only two agents were administered for all types of surgical procedures, Ceftriaxone and Metronidazole. More than half of the participants 206(53.6%) were given Ceftriaxone while combination of Ceftriaxone and Metronidazole were used for 159(41.4%) patients. The remaining subjects were managed with Metronidazole alone.
Regarding the selection of antibiotics for common procedures; most appendectomy procedures (88.3%) were given combination of Ceftriaxone and Metronidazole while the remaining was put on Ceftriaxone. Other common procedure seen in this ward, Hernia repair, was mainly managed by combination of Ceftriaxone and Metronidazole (60.7%) while the rest were put on ceftriaxone alone. In this ward, cholecystectomy was managed with different regimen; Metronidazole, combination of Ceftriaxone and Metronidazole and Ceftriaxone alone 49.3, 29.3 and 19.6% respectively (Fig. 2).
Fig. 2.
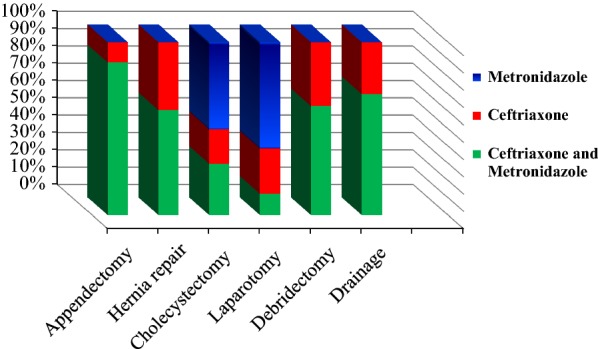
Type of surgical antibiotic prophylaxis used for commonly conducted surgical procedure in Dilchora Referral Hospital, 2017 (n = 384)
Concerning dosage and timing of administration of prophylactic antibiotics, a large number of patients 338 (88%) was given antibiotics 1 h before surgical procedures but the remaining were given just 30 min before the surgery. The majority 374(97.4%) of SAP was given as a single dose. Regarding the dose of ceftriaxone used in SAP, 1gm dose were used for 206(53.6%) patients, 2 gm were used for 30(7.5%). All patients who were put on Metronidazole were managed with 500 mg dose.
Discussion
The primary objective of this study was to assess pattern of antimicrobial usage for surgical site infection prophylaxis. In present study, all patients who went through surgical procedure were given prophylactic antibiotics. Ceftriaxone and Metronidazole were only agents prescribed for all types of surgery, ceftriaxone alone being given for more than half (53.6%) of the patients.
In this study, all patients who went through surgery have given prophylactic antibiotics. Although this is finding is in line with study done elsewhere [16–18] it indicates overutilization of antibiotics in this ward. This might show lack of awareness and compliance toward international and local guidelines among health care providers.
International guideline promote the use less costly and narrow spectrum antibiotics for prophylaxis [19]. Cefazolin is widely indicated as first choice for most of surgical procedure. In our study however, over half of subjects were managed by ceftriaxone. Although this study is in line with study done in Addis Ababa where 70% of procedures were managed by Ceftriaxone [20], it is in contrast to Iranian [21] and Sudanes [17] studies in which they reported Cefazolin and Cefuroxime as the most commonly used prophylactic agent respectively. This may be related to inaccessibility of antibiotics and noncompliance toward international guidelines.
In present study, combination (ceftriaxone and metronidazole) were indicated regularly (41.4%). Although similar finding was reported in other study [20], the routine use combination seems inappropriate as such regimen is recommended only for limited procedures where anaerobic bacteria coverage is required [19].
In this study, inconsistences in antibiotics selection were seen. Different antibiotics were used for similar procedure. For instance, appendectomy was managed through combination of Ceftriaxone and Metronidazole (88.3%) as well as Ceftriaxone alone. According to the guidelines, anaerobic coverage is needed for appendectomy such as cephalosporin with anaerobic activity (Cefotetan) or Metronidazole combined with Cefazolin [19]. This kind of inconsistence and deviation from guideline recommendation were also observed in other studies [18].
Regarding dosage and timing of administration prophylactic antibiotics, in current study most of subjects (88%) were given antibiotics from half an hour to 1 h before surgical procedures indicating compliance to guidelines recommendation. This is similar with the finding of this study where all antibiotic prophylaxis were given within 30–60 min before surgery [22].
Conclusion
It is concerning that in this ward all cases of surgical procedure were given antimicrobial prophylaxis either as single or combined forms. There was inappropriate antibiotic selection for different types of surgical procedure. The use of Ceftriaxone and combination of Ceftriaxone and Metronidazole for most procedure seems inappropriate.
Limitation of the study
The present study had limitation regarding its generalizability as it was not conducted in multicenter.
Additional file
Additional file 1. The data collection tool is attached as a Additional file. It is the data extraction format used to collect data from patient records.
Authors’ contributions
HT is principal author responsible for designing the study, data collection and analysis and interpretation of findings. YA responsible for conception of the research idea, participated in study design and authored the manuscript. Both authors read and approved the final manuscript.
Acknowledgements
We extend our heartfelt thanks to all directly and indirectly involved in this study and particularly DCRH surgical ward staffs. Our appreciation also goes to the data collectors who showed the utmost effort in acquiring appropriate information.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
The datasets are available from the corresponding author on reasonable request.
Consent to publish
Not applicable since there is no individual details in our result.
Ethics approval and consent to participate
The research protocol was reviewed and approved by the school delegate of Institutional Health Research Ethics Review Committee, Haramaya University. A formal permission letter was obtained from College of Health and Medical Sciences and submitted to DCRH to get permission for accessing patient records. The issue of assuring privacy and confidentiality was given more attention during the study by keeping the patient’s name anonymously and using identification number to refer each study participants.
Funding statement
The authors did not receive any fund for this research.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Abbreviations
- DCRH
Dil Chora Referral Hospital
- SAP
surgical antibiotics prophylaxis
- SSI
surgical site infection
Contributor Information
Yohanes Ayele, Email: yohanes.ayele16@gmail.com.
Henok Taye, Email: henokutaye@yahoo.com.
References
- 1.Horan TC, Gaynes RP, Martone WJ, Jarvis WR, Emori TG. CDC definitions of nosocomial surgical site infections, 1992; a modification of CDC definitions of surgical wound infections. Infection Control Hosp Epidemiol. 1992;1992(13):606–608. doi: 10.1017/S0195941700015241. [DOI] [PubMed] [Google Scholar]
- 2.Badia JM, Casey AL, Petrosillo N, Hudson PM, Mitchell SA, Crosby C. Impact of surgical site infection on healthcare costs and patient outcomes: a systematic review in six European countries. J Hosp Infect. 2017;96(1):1–15. doi: 10.1016/j.jhin.2017.03.004. [DOI] [PubMed] [Google Scholar]
- 3.Ierano C, Nankervis JAM, James R, Rajkhowa A, Peel T, Thursky K. Surgical antimicrobial prophylaxis. Aust Prescr. 2017;40(6):225–229. doi: 10.18773/austprescr.2017.073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Woods RK, Dellinger EP. Current guidelines for antibiotic prophylaxis of surgical wounds. Am Fam Physician. 1998;57(11):2731–2740. [PubMed] [Google Scholar]
- 5.Assessment SCoHT. Antibiotic Prophylaxis for Surgical Procedures: A Systematic Review (Summary and conclusions) [Internet]: SBU Yellow Report No. 200; 2010. https://www.ncbi.nlm.nih.gov/books/NBK448007/. Accessed 9 Apr 2018
- 6.Boonchan T, Wilasrusmee C, McEvoy M, Attia J, Thakkinstian A. Network meta-analysis of antibiotic prophylaxis for prevention of surgical-site infection after groin hernia surgery. Br J Surg. 2017;104(2):e106–e117. doi: 10.1002/bjs.10441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kasatpibal N, Nørgaard M, Sørensen HT, Schønheyder HC, Jamulitrat S, Chongsuvivatwong V. Risk of surgical site infection and efficacy of antibiotic prophylaxis: a cohort study of appendectomy patients in Thailand. BMC Infect Dis. 2006;6:111. doi: 10.1186/1471-2334-6-111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Waddell TK, Rotstein OD. Antimicrobial prophylaxis in surgery. Committee on Antimicrobial Agents, Canadian Infectious Disease Society. CMAJ. Can Med Assoc J. 1994;151(7):925–931. [PMC free article] [PubMed] [Google Scholar]
- 9.Burke JP. Maximizing appropriate antibiotic prophylaxis for surgical patients: an update from LDS Hospital, Salt Lake City. Clin Infect Dis. 2001;33(Supplement_2):S78–83. [DOI] [PubMed]
- 10.Bailly P, Lallemand S, Thouverez M, Talon D. Multicentre study on the appropriateness of surgical antibiotic prophylaxis. J Hosp Infect. 2001;49(2):135–138. doi: 10.1053/jhin.2001.1064. [DOI] [PubMed] [Google Scholar]
- 11.Pittalis S, Ferraro F, Piselli P, Ruscitti LE, Grilli E, Lanini S, et al. Appropriateness of surgical antimicrobial prophylaxis in the Latium region of Italy, 2008: a multicenter study. Surg Infect. 2013;14(4):381–384. doi: 10.1089/sur.2012.189. [DOI] [PubMed] [Google Scholar]
- 12.Ng RS, Chong CP. Surgeons’ adherence to guidelines for surgical antimicrobial prophylaxis—a review. Aust Med J. 2012;5(10):534–540. doi: 10.4066/AMJ.2012.1312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Napolitano F, Izzo MT, Di Giuseppe G, Angelillo IF, The Collaborative Working G Evaluation of the appropriate perioperative antibiotic prophylaxis in Italy. PLoS ONE. 2013;8(11):e79532. doi: 10.1371/journal.pone.0079532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mousavi S, Zamani E, Bahrami F. An audit of perioperative antimicrobial prophylaxis: compliance with the international guidelines. J Res Pharm Pract. 2017;6(2):126–129. doi: 10.4103/jrpp.JRPP_16_164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dellit TH, Owens RC, McGowan JE, Jr, Gerding DN, Weinstein RA, Burke JP, et al. Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America guidelines for developing an institutional program to enhance antimicrobial stewardship. Clin Infect Dis. 2007;44(2):159–177. doi: 10.1086/510393. [DOI] [PubMed] [Google Scholar]
- 16.Kaya S, Aktas S, Senbayrak S, Tekin R, Oztoprak N, Aksoy F, et al. An evaluation of surgical prophylaxis procedures in Turkey: a multi-center point prevalence study. Eurasian J Med. 2016;48(1):24–28. doi: 10.5152/eurasianjmed.2015.15222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Elbur AI, Ahmed Sayed Ahmed ElSayed, Mirghani Abd El Rahman Yousif, Abdel-Rahman ME. An audit of prophylactic surgical antibiotic use in a Sudanese Teaching Hospital. Int J Clin Pharm. 2012. [DOI] [PubMed]
- 18.Vessal G, Namazi S, Davarpanah MA, Foroughinia F. Evaluation of prophylactic antibiotic administration at the surgical ward of a major referral hospital, Islamic Republic of Iran. East Mediterr Health J. 2011;17(8):663–668. doi: 10.26719/2011.17.8.663. [DOI] [PubMed] [Google Scholar]
- 19.Bratzler DW, Dellinger EP, Olsen KM, Perl TM, Auwaerter PG, Bolon MK, et al. Clinical practice guidelines for antimicrobial prophylaxis in surgery. Am J Health Syst Pharm. 2013;70:195–283. doi: 10.2146/ajhp120568. [DOI] [PubMed] [Google Scholar]
- 20.Argaw NA, Shumbash KZ, Asfaw AA, Hawaze S. Assessment of surgical antimicrobial prophylaxis in Orthopaedics and Traumatology Surgical Unit of a Tertiary Care Teaching Hospital in Addis Ababa. BMC Res Notes. 2017;10(1):160. doi: 10.1186/s13104-017-2475-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Foroutan B, Foroutan R. Perioperative antibiotic prophylaxis in elective surgeries in Iran. Med J Islam Repub Iran. 2014;28:66. [PMC free article] [PubMed] [Google Scholar]
- 22.Afzal Khan AK, MirshAd PV, MohAMMed rAfiuddin rAshed GB. A study on the usage pattern of antimicrobial agents for the prevention of surgical site infections (SSIs) in a tertiary care teaching hospital. J Clin Diagn Res. 2013;7(4):671–4. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. The data collection tool is attached as a Additional file. It is the data extraction format used to collect data from patient records.
Data Availability Statement
The datasets are available from the corresponding author on reasonable request.


