Abstract
Background
The Kidney Awareness Registry and Education (KARE) trial examined the impact of a multilevel intervention on blood pressure control among patients with chronic kidney disease (CKD) in a public health care delivery system. KARE consisted of a clinic-based intervention (a primary care CKD registry with point-of-care provider notifications and quarterly feedback related to CKD management) and a patient-directed intervention [a CKD self-management support (CKD-SMS) program that included low literacy educational materials, automated telephone-administered self-management modules and telephone health coaching]. We explored the acceptability of these interventions among end users.
Methods
At trial conclusion, we surveyed 39 primary care providers (PCPs) to identify preferences about components of the clinic intervention, conducted two focus groups among non-PCP staff to elicit in-depth attitudes and experiences with operationalizing the team-based CKD registry, and conducted eight focus groups with English- and Spanish-speaking patients to hear about their experiences with the CKD-SMS program. Focus group transcripts were analyzed using thematic analysis. Self-reported participation and data from the automated telephone program were used to evaluate patient engagement.
Results
Most PCPs (94%) believed that the point-of-care notifications benefited clinic workflow and agreed that quarterly feedback enhanced their ability to identify (89.5%) and manage (73.7%) CKD. Staff confirmed usefulness of point-of-care notifications. Patients suggested the automated telephone system was impersonal, though easy to use; that frequent automated calls were helpful to reinforce self-management behaviors; and that telephone health coaching was convenient. Nearly 40% of patients completed >80% of automated phone calls, 95% participated in calls with their health coach and 77% created at least one action plan.
Conclusions
A CKD registry is acceptable to primary care health care teams and has potential to enhance identification and management of CKD in primary care. Low-income patients appreciated and engaged with a telephone-based CKD-SMS program, demonstrating its potential for increasing awareness and health engagement among populations with CKD within a public health care delivery system.
Keywords: acceptability, awareness, chronic kidney disease, CKD, registry, safety-net, self-management support
Introduction
Chronic kidney disease (CKD) affects more than 10% of the US population and is a pressing public health problem [1, 2]. Despite this, awareness of CKD among those with the disease remains very low, with studies reporting that <10% of individuals with CKD are aware of their disease [3, 4]. Among providers, awareness of CKD management guidelines is also suboptimal [4]. Low patient and provider awareness of CKD likely limit the delivery of, and adherence to, evidence-based CKD care, thus impeding efforts to slow CKD progression and negatively affecting health outcomes. There is a clear need for solutions that sustainably enhance the detection and management of CKD at the primary care level, which may also offer a critical vantage point for narrowing known disparities in CKD outcomes and care delivery [5].
The Kidney Awareness Registry and Education (KARE) study is a 2 × 2 randomized controlled trial (ClinicalTrials.gov: NCT01530958) that aimed to improve blood pressure control through enhanced patient and provider awareness of CKD. KARE examined the impact of a multilevel intervention consisting of a primary care CKD registry and a CKD self-management support (CKD-SMS) program [6]. At the primary care level, a team-based patient CKD registry supported the identification and management of individuals with CKD and uncontrolled blood pressure. The CKD registry was comprised of an ‘in-reach’ element (e.g. point-of-care notifications) and an ‘out-reach’ component (e.g. quarterly feedback reports), and built on prior CKD registry efforts [7–9]. At the patient level, the comprehensive, telephone-based CKD-SMS program encouraged patients to engage in their health care and adopt healthy behaviors. The self-management support program included low literacy written educational materials, automated telephone administered self-management modules and telephone health coaching, and was based on previous self-management support initiatives [10–14]. The KARE trial took place within a public health care delivery system and enrolled a low-income patient population that was linguistically and racially diverse.
While registries and self-management support programs have independently been shown to improve uptake of health knowledge and disease self-management among patients with various chronic diseases [13, 14], much less is known about their potential to affect change within the CKD population, or their acceptability within a public health care delivery system. Few CKD studies have involved the primary care setting and even fewer have targeted a diverse, lower-income population. Examining the acceptability of the provider-level and patient-level KARE interventions could offer valuable insight into key facilitators of implementing similar interventions among health systems and populations that shoulder a high burden of chronic disease. The objectives of this study were thus: (i) to explore the acceptability of a primary care CKD registry with both ‘in-reach’ and ‘out-reach’ among health care teams in clinics in a public health care delivery system; (ii) to investigate patient opinions and beliefs about the CKD-SMS program; and (iii) to determine factors that could facilitate the sustainable implementation of both a CKD primary care registry and a CKD-SMS program within a public health care delivery system.
Materials and methods
Study design, setting and participants
KARE was a non-blinded, randomized controlled trial with a 2 × 2 factorial design implemented in two primary care clinics within a public health care delivery system. Provider teams, consisting of primary care providers (PCPs), nurses, nurse practitioners, medical assistants and behaviorists were randomized to receive either the primary care CKD registry or usual care. Patients were subsequently randomized to participate in a CKD-SMS program or usual care. Details of the KARE study protocol, including an evaluation of educational materials used in the CKD-SMS, have been previously reported [6, 15]. For this mixed-methods study examining acceptability of the multilevel intervention using surveys, focus groups and interviews, only members of the primary care clinic teams randomized to receive the KARE registry and patients randomized to receive the CKD-SMS program were eligible for participation.
Study procedures
PCP survey
Acceptability of the clinic-level intervention was assessed among study teams in the intervention arm; eligible PCPs were asked to complete a survey at the end of the 12-month study that elicited preferences toward the ‘in-reach’ and ‘out-reach’ components of the primary care CKD registry in a quantitative fashion to facilitate comparisons. The survey also asked whether or not providers agreed that point-of-care alerts and quarterly feedback patient lists had changed their ability to identify and deliver CKD care using 5-point Likert scales and whether they had altered their interactions with patients and/or clinic staff. PCP surveys were distributed via e-mail, mailboxes and were handed out in-person.
Clinic staff focus groups
Two focus groups with non-PCP clinic staff were organized between June and October 2015. Focus groups were chosen instead of one-on-one interviews to elicit in-depth attitudes and experiences with operationalizing the team-based CKD registry and to promote shared conversation. Focus groups were held in a clinic conference room and were facilitated by three members of the research team who had received training in facilitation, including a health coach and two study investigators (A.V., K.L.). Facilitators used a focus group guide designed to encourage staff to discuss their attitudes and experiences, using open-ended questions informed by social cognitive theory [16], which describes a dynamic process of how personal factors, environmental variables and human behavior reciprocally exert influence on each other to enable behavior change and posits that individuals with self-efficacy can enact behavior change, even when faced with obstacles (Supplementary data A). Participants provided written consent to participate.
Patient focus groups
Eight focus groups with English- and Spanish-speaking patients who had been randomized to participate in the CKD-SMS program were organized between June and October 2015. Participants were recruited by telephone, provided written consent for participation and completed brief demographic surveys on the day of focus group facilitation. Patient focus groups were conducted in community clinic conference rooms, ranged in size from two to six participants, and lasted between 1 and 2 h. They were facilitated by three members of the research team who were trained in facilitation, including a KARE health coach and two study investigators (A.V., K.L). They used a focus group guide informed by social cognitive theory that encouraged patients to draw upon their personal experiences with the three different components of the CKD-SMS intervention: low-literacy, language-concordant written patient education materials; bimonthly, language-concordant automated telephone self-management calls; and telephone health coaching (Supplementary data B).
Patient engagement data
Self-reported patient engagement with each component of the CKD-SMS program and socio-demographic data were collected during standardized research calls for all patients randomized to the intervention (n = 74). Additional data from the automated telephone self-management program identified the number of patients with an average call completion rate above 80% throughout the course of the 50-week program; these patients were a priori determined to be ‘high utilizers’ of the automated portion of the CKD-SMS program. Records from health coaching calls were reviewed to identify the number of patients who developed at least one action plan during the study’s duration.
Analysis
All focus groups were audio-recorded and professionally transcribed. Spanish focus group transcripts were professionally translated and transcribed into English prior to the coding process. No field notes taken during the focus groups contributed to the analysis. Transcripts were analyzed using thematic analysis with an iterative and collaborative process, drawing themes from the primary data rather than relying an a priori conceptual model [17]. Three investigators (K.L., A.N. and A.S.) independently coded one transcript for each language group and agreed upon initial codes. Only one of these individuals was involved in focus group facilitation, thus minimizing the impact of facilitator–participant interactions on the analytic process. They used the preliminary codebook to independently analyze another subset of transcripts, and then compared independent coding results, resolved inconsistencies through adjustment of the codebook and developed a set of specific code definitions. The remaining transcripts were independently coded by two of the three investigators who had done the initial coding. Any discrepancies in coding were resolved by consensus. As additional concepts emerged, team members collaboratively modified the codebook. After analyzing all of the transcripts, the analytic team felt that thematic saturation was achieved among the non-PCP staff and patient focus groups.
PCP survey data and patient engagement data were analyzed using StataSE Version 14 (StataCorp, College Station, Texas, USA). PCP responses were categorized into binary variables that reflected agreement and complete agreement with statements about the different registry components. Chi-squared tests were used to evaluate potential differences in PCP responses by clinic site (academic versus community).
Ethics
The study was approved by the UCSF Committee on Human Research (Protocol number 11-07399) and participant anonymity was preserved. No patient or provider names were included in the focus group audio recordings or the accompanying transcripts. Focus group participants agreed to maintain confidentiality of other participants during the formal consent process. PCP surveys were anonymous unless individuals willingly provided their names for subsequent contact.
Results
Characteristics of study participants
A total of 21 (54%) PCPs randomized to the registry arm responded to the survey. A majority (81%) of the registry PCPs worked in the academic training clinic and most (61.9%) were female. PCP respondents had a varied amount of clinical experience and included diverse provider types: 25% (n = 5) were trainees, 55% (n = 11) were attending providers and 20% (n = 4) were nurse practitioners (Table 1).
Table 1.
Characteristics of study participants
| Participant characteristics | PCP | Non-PCP clinic staff | Patients randomized to CKD-SMS | Focus group patient participants |
|---|---|---|---|---|
| (n = 21) | (n = 8) | (n = 74) | (n = 26) | |
| n (%) | n (%) | n (%) | n (%) | |
| Clinic | ||||
| Academic training clinic | 17 (81.0) | 6 (75.0) | 48 (64.9) | 20 (76.9) |
| Community clinic | 4 (19.0) | 2 (25.0) | 26 (35.1) | 6 (23.1) |
| Female | 13 (61.9) | 7 (87.5) | 39 (52.7) | 12 (46.2) |
| Race/ethnicity | ||||
| White | 9 (42.9) | 0 (0.0) | 7 (9.6) | 3 (11.5) |
| Asian | 6 (28.6) | 3 (37.5) | 11 (15.1) | 0 (0.0) |
| Black | 1 (4.8) | 0 (0.0) | 30 (41.1) | 9 (34.6) |
| Hispanic | 4 (19.0) | 5 (62.5) | 25 (34.3) | 14 (53.8) |
| Other | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| More than one race | 1 (4.8) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Non-English language | – | – | 27 (36.5) | 15 (60.0) |
| Age | ||||
| 20–44 years | – | – | 14 (18.9) | 5 (19.2) |
| 45–64 years | – | – | 48 (64.9) | 15 (57.7) |
| 65+ years | – | – | 12 (16.2) | 6 (23.1) |
| Provider type or clinic rolea | ||||
| Trainee | 5 (25.0) | – | – | – |
| Attending provider | 11 (55.0) | – | – | – |
| Nurse practitioner | 4 (20.0) | – | – | – |
| Medical assistant | – | 7 (100.0) | – | – |
| Other (e.g. health worker, etc.) | – | 0 (0.0) | – | – |
| Years of experience after degree | ||||
| <5 years | 7 (33.3) | – | – | – |
| 5–15 years | 7 (33.3) | – | – | – |
| ≥16 years | 7 (33.3) | – | – | – |
One PCP and one staff member did not answer this question, resulting in denominators of n = 20 and n = 7.
A total of eight (42%) of the non-PCP clinic staff randomized to the registry participated in a focus group. While registry team members served various roles on the health care team (e.g. health workers, panel managers, nurses), all of the registry focus group attendees were medical assistants. They were racially/ethnically diverse, with 37.5% self-identifying as Asian and 62.5% self-identifying as Hispanic (Table 1). The majority (75%) of the non-PCP clinic staff focus group participants were from the academic training clinic.
Of the 74 patients randomized to receive the CKD-SMS program and from whom engagement data were obtained, 26 (35%) participated in a focus group. Similar to the overall KARE study population and the population randomized to receive CKD-SMS, focus group patients were racially/ethnically diverse, with 53.9% (n = 14) self-identifying as Hispanic, 34.6% (n = 9) self-identifying as Black and 11.5% (n = 3) self-identifying as White. A majority (76.9%) of patient focus group participants received care from the academic training clinic and most (60%) spoke Spanish as their primary language (Table 1).
PCP attitudes toward the primary care CKD registry
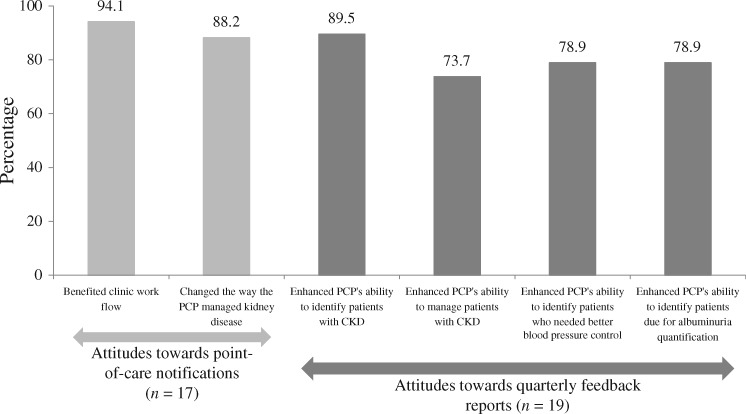
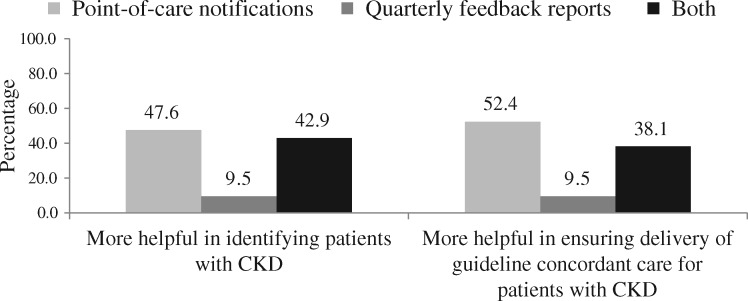
Most (94.1%) PCPs believed that the ‘in-reach’ component of the registry, with point-of-care notifications, benefited clinic workflow and 88.2% reported that these notifications influenced the way in which they managed CKD (Figure 1). PCP respondents also reported positive attitudes toward the ‘out-reach’ component of the registry, consisting of quarterly feedback, with a majority stating it enhanced their ability to identify patients who had CKD, needed better blood pressure control or were due for albuminuria quantification (89.5%, 78.9% and 78.9%, respectively). In addition, 73.7% reported that the quarterly feedback reports enhanced their ability to manage patients with CKD. When asked to compare the two different registry components, a majority of PCPs stated that the point-of-care notifications were more helpful than the quarterly feedback reports, though similar numbers reported that having both types of notifications were helpful in identifying CKD and supporting the delivery of guideline-concordant care (Figure 2). Responses were similar among PCPs from the two different clinics (data not shown).
Fig. 1.
PCP attitudes toward the CKD registry.
Fig. 2.
PCP attitudes toward the registry components.
Non-PCP clinic staff attitudes toward the primary care CKD registry
Theme 1: CKD registries can aid health care teams in delivering guideline-concordant CKD care
Non-PCP clinic staff acknowledged the benefits of a primary care CKD registry. They stated that the point-of-care alerts reminded the health care team members to check for overdue diagnostic tests (i.e. albumin:creatinine ratio), allowing them to deliver better care to patients with CKD.
I think it reminded a lot of the providers what they needed to do, including us… So when we had time to actually do it, those orders would be carried out. (Participant #1)
It was really good for early detection for kidney disease 'cause we all know people who have chronic kidney disease on dialysis but I think it’s so nice to catch it early on and educate the patient, see if they have some options and maybe try and control it. (Participant #3)
Theme 2: Suggestions for promoting registry uptake in a public health care delivery health system
Non-PCP clinic staff believed that there were several factors that would promote registry uptake. Specifically, they mentioned that better communication among the providers within each health care team would help avoid duplication of services and streamline activities.
[The registry] was a reminder… It’s like I need to do my homework, just sometimes I end up doing [the providers’] homework many times. (Participant #4)
They also stated that a smaller workload would allow them to take advantage of the ‘in-reach’ component of the registry (e.g. the point-of-care alerts) in a more sustainable way.
We don’t really actually review [the alerts] anymore… that’s one thing that … we’ve taken off our plate in order to accommodate other stuff that has been put on our plate. (Participant #8)
Patient attitudes toward the CKD-SMS program
Theme 1. Patients appreciated a language-concordant CKD-SMS program
Patients voiced appreciation for the low-literacy patient education materials and the educational benefits of the CKD-SMS program overall. Participants mentioned that throughout the course of the program, they had learned how to take better care of their kidneys and how to eat a healthier diet. For the most part, patients found the automated telephone calls to be informative and reported that the calls helped to reinforce the importance of various health behaviors such as remembering to take their medication and doing more physical activity. This was particularly true among Spanish-speaking participants, who emphasized the benefit of receiving new information from the CKD-SMS program and voiced an appreciation for the written educational materials more than their English-speaking counterparts.
Those questions are giving you information so you don’t feel they are long. You feel the call is informative. [Spanish (S.) #1]
I felt like it worked 'cause it managed to beat some things into my head that people have been trying for a long time. [English (E.) #1]
Theme 2: Patients generally agreed that the automated calls were easy to understand, practical and convenient, though some patients felt that the automated calls were impersonal
To press the numbers and to make the call. It was easy. (S. #5)
The way they explained it was very nice because it seemed as if we were having a conversation. It was easy to understand for any of us. At any educational level. (S. #3)
Those patients that did not appreciate the automated nature of the telephone calls expressed a preference for more personal interaction and the health coaching component of the CKD-SMS program.
Talking to the [telephone]; it's impersonal and if you have a question right then, then you can't get a response. (E. #1)
And I think you could learn more from people if you can offer them a back and forth, you know, a real confidant. (E. #2)
Theme 3: Patients universally enjoyed their health coaches, appreciating their accessibility as well as the support that they provided
Patients mentioned that their health coaches were very helpful because they followed up with solutions and connected patients with various community resources.
I didn’t feel I was talking to someone from the hospital related to the illness I suffer, I felt like she was my friend, she was someone I could talk to and clarify any doubts I could have. (S. #3)
I enjoyed it because each time you had any questions, they were always available and they always found a solution or an answer for you… (E. #7)
Theme 4: System enhancements may improve patient experience with the CKD-SMS program and increase uptake of health knowledge and behaviors
Focus group participants requested that educational materials include more dietary advice. They also expressed a shared desire for the automated phone calls to provide the user with options to repeat prompts and confirm responses. Finally, they mentioned that the calls would be most useful if they could be delivered on a weekly basis, rather than the 50-week program structure that they had received, which involved weekly calls for the first 4 weeks followed by a biweekly call for the remainder of the program.
I would like for the calls to be weekly because –, it just keeps it on your mind then, because when you get older we have a tendency to kind of forget things and you go oh, we discussed something really, really important and then the following couple days it goes right out of your mind. (E. #1)
Patients voiced mixed opinions when asked about their option of a reminder text to alert users to the time of their automated call and provide information for calling into the system. One reservation expressed by focus group participants was that patients did not always have a phone plan that accommodates text messages. Participants voiced no desire to include video-conferencing functionality.
Theme 5: Despite voicing appreciation for their health coaches, there was disagreement among participants about the merits of in-person versus telephone health coaching
Those participants that voiced a preference for in-person health coaching believed that the in-person interaction would make them feel even more comfortable, thus providing a better environment for their questions to be answered.
People that do okay over the phone with questions but I'd rather do it in-person… you know I've got to see the person who I'm talking to and get more time to understand what you're talking about. (E. #10)
And the more we talk face to face, the more comfortable we get in talking with each other. So again, through that aspect you stand to learn more as well. (E. #2)
My questions are better asked in person. (E. #4)
Other participants expressed a preference for the telephone health coaching because of the convenience it offered. One English speaker in particular stated the following:
It was very convenient. You know, if I missed a call, I could call them back… I could call them back even if it was the next day. So it was very convenient for me, rather than going out and transportation and all of that. (E. #7)
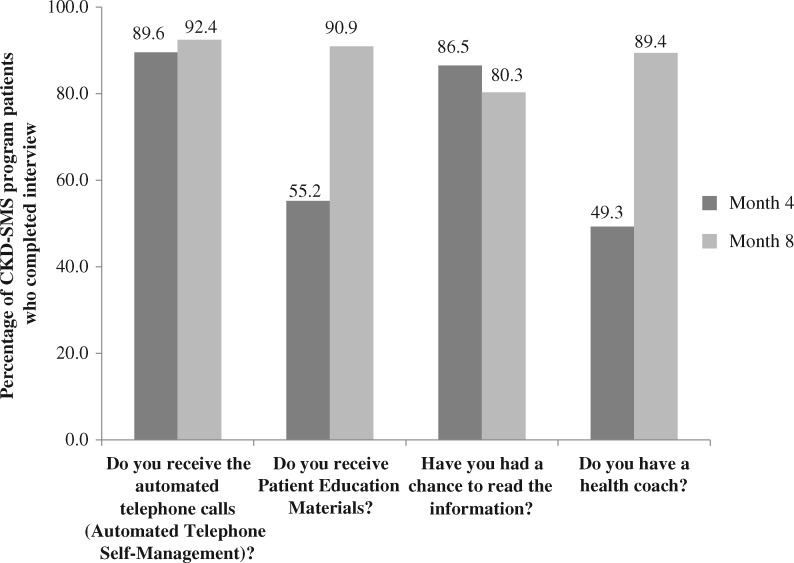
Patient engagement with the CKD-SMS program
Over 90% of patients completed the month 4 research calls and 89% completed the month 8 research calls, providing ample data about engagement with the CKD-SMS program. Self-reported participation with each component self-management support program ranged from 49% to 92% and increased throughout the program duration (Figure 3). A majority of patients who reported having read the education materials gave them an 8 or higher on a 1–10 scale in terms of readability and helpfulness (88% and 85%, respectively). Nearly 40% of the 74 CKD-SMS program participants were high utilizers of the automated portion of the CKD-SMS system, with an average automated-phone call completion rate >80%. Additionally, over 95% of CKD-SMS participants participated in phone calls with their health coaches. The most common topics discussed during the health coaching phone calls were physical activity, diet, blood pressure control and medication adherence. A majority (77%) of CKD-SMS participants created at least one action plan with his/her health coach over the course of the study intervention. The most frequent action plan themes were increasing physical activity, improving diet and enhancing patient–provider communication.
Fig. 3.
Self-reported patient engagement with the CKD-SMS program.
Discussion
Using a mixed-methods approach with quantitative and qualitative methods, we demonstrated high acceptability of both KARE interventions among PCPs, other primary care medical staff and patients. Our approach was multifaceted, using various types of acceptability data. The Theoretical Framework of Acceptability for health care system interventions proposed by Sekhon et al. provides a useful context for interpreting and organizing these different data [18]. This framework is beneficial for the evaluation of multi-level, complex interventions because it breaks acceptability into seven different constructs, each of which emerge from a validated theory. The four framework constructs most relevant to our acceptability analysis are: affective attitude, self-efficacy, ethicality and perceived effectiveness. When evaluated together, these constructs provide a holistic view of the KARE interventions’ acceptability and the likelihood that they can be incorporated into routine practice.
Affective attitude and self-efficacy
Affective attitude refers to how an individual feels about an intervention and self-efficacy is defined by a participant’s confidence that he/she can participate in the intervention. In our study, PCPs and their team members demonstrated positive attitudes toward both the ‘in-reach’ and ‘out-reach’ components of the CKD registry and voiced confidence that the registry enhanced their ability to manage kidney disease in a public health care delivery system. These findings support a growing body of evidence suggesting that registries are effective at enhancing provider self-efficacy of chronic disease management at the population level. Prior registries with ‘in-reach’ and/or ‘out-reach’ components have also been shown to successfully enhance the delivery of guideline-concordant care for populations with hypertension and diabetes [19–21]. Our acceptability results demonstrate that a CKD registry comprised of both components has a similar potential to help health care providers more confidently identify and manage CKD in the primary care setting. A prior study identified that a key facilitator to implementing a primary care CKD registry was the inclusion of roles for non-PCP staff due to the increased workload introduced by the registry [8]. It is, therefore, particularly notable that both the PCPs and the non-PCP health care team members in the KARE study reported positive attitudes toward the CKD registry, reinforcing the benefit of sharing the workload burden that a registry may introduce.
Patients reported positive beliefs about the CKD-SMS program and noted that it provided helpful health knowledge and management strategies. While prior studies have demonstrated that health coaching interventions and automated communication programs are effective methods for improving patient awareness and management of hypertension and diabetes, including those who receive medical care in a public health care delivery system, this study is one of the first to examine these types of interventions within the CKD context [10, 11, 13]. The positive attitudes that patients had toward all three components of the CKD-SMS program demonstrate the desire of CKD patients to receive additional education, knowledge and support.
Ethicality
Ethicality is the extent to which an intervention has good fit with an individual’s value system. Focus group data from the non-physician primary care staff demonstrated that the CKD registry was aligned with primary care team goals and enhanced the opportunity for team-based care delivery. Patient participation data illustrated high levels of patient engagement with all components of the CKD-SMS program. This is important because patient populations within the public health care delivery system, which are disproportionately comprised of individuals with minority or immigrant status and individuals who live in economically disadvantaged communities, tend to be less engaged in health care, resulting in poorer health outcomes [22, 23]. Increasing health awareness and engagement among these populations is, therefore, an important public health strategy to curb the complications associated with chronic diseases. Our results suggest that a phone-based self-management support program may provide a critical vantage point for increasing CKD awareness and activating health engagement in racially and linguistically diverse populations within a public health care delivery system. This conclusion is further supported by previous studies that have shown mobile health technology to offer an untapped potential for engaging vulnerable populations in chronic disease management [22, 24]. The high levels of self-reported patient engagement with the patient education materials also suggest that language-concordant, low-literacy education pamphlets offer another key method for increasing health awareness to ‘hard-to-reach’, populations. This is consistent with prior studies that identified that low-literacy education materials for diabetes, CKD and congestive heart failure were associated with higher usability ratings than materials with higher literacy levels [15, 25–27].
Perceived effectiveness
Perceived effectiveness is the extent to which an intervention is perceived as likely to achieve its purpose. Our study results indicate the majority of patients and providers were satisfied with their respective intervention and believed in its efficacy. Importantly, however, several key suggestions emerged from focus groups about how the interventions could be strengthened to further enhance effectiveness. For example, PCPs noted that the registry and the electronic health record should be integrated to ensure the accuracy and usefulness of point-of-care patient alerts, as well as facilitate enhanced provider team user experience. Additionally, adequate clinic staffing and provider teamwork should be prioritized to more effectively align use of the registry with clinic workflow. Patient participants identified several facilitators to improve engagement and efficacy, including increasing the frequency of automated CKD-SMS phone calls and providing additional support to educate and assist patients to successfully interface with the self-management support system. Some patient participants voiced a preference for telephone health coaching because of its convenience; others voiced a preference for the personal touch inherent to in-person health coaching. It is quite possible that the observed difference in participant attitudes toward health-coaching modalities is informed by demographic factors such as patient age and health conditions, such as mobility status. For example, it is possible that patients who are less mobile would find telephone health-coaching to be preferable to in-person coaching because patients can do it within their own homes; in contrast, older patients who are less mobile may be less comfortable with technology and might prefer in-person health-coaching. Future self-management support interventions may want to include both coaching options to optimize patient-centeredness. Lastly, linkage between the provider-level and patient-level interventions is key for sustainability. One way to do this is by leveraging the electronic health record for more frequent and optimal communication among providers and health coaches.
Evaluating KARE’s interventions within each of these constructs is critical, since evidence suggests that high provider and patient satisfaction are essential to the successful implementation of CKD interventions [28, 29]. Additionally, behavioral interventions with high patient acceptability have been associated with better clinical outcomes than those that do not garner high patient satisfaction [18, 30, 31]. While acceptability is gaining recognition as a necessary consideration for the design and implementation of effective health care system interventions, few studies in the USA have comprehensively examined this construct [18]. Our article addresses this gap and serves as a model that can be employed during evaluations of future chronic disease interventions.
Additionally, our acceptability findings are important because CKD is a pressing public health concern, with large challenges related to low patient and provider awareness of CKD [4] as well as existing ethnic/racial and socioeconomic disparities associated with CKD clinical outcomes and quality of care delivery [32]. The positive end-user comments and high engagement and satisfaction levels among providers and patients within this setting speak to the potential of programs that improve CKD knowledge within vulnerable populations and their health care providers. Previous studies have demonstrated that CKD discussions during primary care encounters are lacking [33]. A team-based primary care CKD registry may offer a valuable and acceptable way to improve provider awareness and detection of CKD. In turn, this could lead to more CKD discussions with patients during primary care encounters, thus reinforcing CKD knowledge that patients may gain through self-management support programs.
Limitations of this study include a small sample size and a moderately low survey completion rate among PCPs and focus group participation rate among patients. Nonresponse bias may have thus influenced the positive perception of the interventions reported by PCPs and patients. However, a review of physician survey response behaviors found that nonresponse bias may not be an important factor contributing to the validity of physician surveys [34]. Additionally, while the findings suggest that a primary care CKD registry and CKD-SMS program are acceptable within a public health care delivery system, it is not clear whether the same outcomes would be observed in other types of health care settings. Also, a few constructs from Sekhon’s theoretical framework were not available for our analysis, including burden, intervention coherence and opportunity costs. Future acceptability studies may want to include these variables in their evaluation.
Conclusion
Overall, we demonstrate that a primary care CKD registry is acceptable to health care teams that work in a public health care delivery system and has the potential to improve CKD identification and management efforts at the population level. Additionally, a language-concordant CKD-SMS program is well-received by diverse, low-income patients, suggesting a great potential for programs that leverage similar combinations of automated communication, low-literacy patient education materials and telephone health coaching, to improve this population’s engagement with health. Multi-component CKD-SMS programs could serve as a key tool for activating populations within a public health care delivery system that often experience poor health outcomes, perhaps leading to increased patient awareness of CKD, better health outcomes and reduced health care costs. Finally, the demonstrated feasibility of KARE’s provider-level and patient-level interventions suggest great potential in the use of technology in multilevel interventions to improve awareness and care delivery in public health care systems. Given the significant disparities that exist in CKD, future initiatives should continue to investigate the ways in which technology can be successfully harnessed to provide better care and outcomes within the primary care settings that serve the most vulnerable.
Funding
The KARE study was funded by grant numbers R01DK104130, R34DK093992 and K23DK094850, all from the National Institute of Diabetes and Digestive and Kidney Disease, Bethesda, MD, USA. The funding body had no role in the design of the study, or in the collection, analysis and interpretation of data.
Conflict of interest statement
None declared.
Supplementary data
Supplementary data are available at ckj online.
Supplementary Material
References
- 1. Murphy D, McCulloch CE, Lin F. et al. Trends in prevalence of chronic kidney disease in the United States. Ann Intern Med 2016; 165: 473–481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Coresh J, Selvin E, Stevens LA. et al. Prevalence of chronic kidney disease in the United States. JAMA 2007; 298: 2038–2047 [DOI] [PubMed] [Google Scholar]
- 3. Tuot DS, Plantinga LC, Hsu C-Y. et al. Chronic kidney disease awareness among individuals with clinical markers of kidney dysfunction. Clin J Am Soc Nephrol 2011; 6: 1838–1844 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Plantinga LC, Tuot DS, Powe NR.. Awareness of chronic kidney disease among patients and providers. Adv Chronic Kidney Dis 2010; 17: 225–236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Greer RC, Ameling JM, Cavanaugh KL. et al. Specialist and primary care physicians' views on barriers to adequate preparation of patients for renal replacement therapy: a qualitative study. BMC Nephrol 2015; 16: 37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Tuot DS, Velasquez A, McCulloch CE.. The Kidney Awareness Registry and Education (KARE) study: protocol of a randomized controlled trial to enhance provider and patient engagement with chronic kidney disease. BMC Nephrol 2015; 16: 166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Navaneethan SD, Jolly SE, Schold JD. et al. Development and validation of an electronic health record-based chronic kidney disease registry. Clin J Am Soc Nephrol 2011; 6: 40–49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. McBride D, Dohan D, Handley MA. et al. Developing a CKD registry in primary care: provider attitudes and input. Am J Kidney Dis 2014; 63: 577–583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Drawz PE, Miller RT, Singh S. et al. Impact of a chronic kidney disease registry and provider education on guideline adherence–a cluster randomized controlled trial. BMC Med Inform Decis Mak 2012; 12: 62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Dennis SM, Harris M, Lloyd J. et al. Do people with existing chronic conditions benefit from telephone coaching? A rapid review. Aust Health Rev 2013; 37: 381–388 [DOI] [PubMed] [Google Scholar]
- 11. Thom DH, Willard-Grace R, Hessler D. et al. The impact of health coaching on medication adherence in patients with poorly controlled diabetes, hypertension, and/or hyperlipidemia: a randomized controlled trial. J Am Board Fam Med 2015; 28: 38–45 [DOI] [PubMed] [Google Scholar]
- 12. Halladay JR, DeWalt DA, Wise A. et al. More extensive implementation of the chronic care model is associated with better lipid control in diabetes. J Am Board Fam Med 2014; 27: 34–41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Willard-Grace R, Chen EH, Hessler D.. Health coaching by medical assistants to improve control of diabetes, hypertension, and hyperlipidemia in low-income patients: a randomized controlled trial. Ann Fam Med 2015; 13: 130–138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Posadzki P, Mastellos N, Ryan R. et al. Automated telephone communication systems for preventive healthcare and management of long-term conditions. Cochrane Database Syst Rev 2016; 12: CD009921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Tuot DS, Davis E, Velasquez A. et al. Assessment of printed patient-educational materials for chronic kidney disease. Am J Nephrol 2013; 38: 184–194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Painter JE, Borba CP, Hynes M. et al. The use of theory in health behavior research from 2000 to 2005: a systematic review. Ann Behav Med 2008; 35: 358–362 [DOI] [PubMed] [Google Scholar]
- 17. Glaser BG, Strauss AL.. The Discovery of Grounded Theory: Strategies for Qualitative Research. Chicago, IL: Aldine Pub. Co., 1967 [Google Scholar]
- 18. Sekhon M, Cartwright M, Francis JJ.. Acceptability of healthcare interventions: an overview of reviews and development of a theoretical framework. BMC Health Serv Res 2017; 17: 88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Peterson KA, Radosevich DM, O'Connor PJ. et al. Improving diabetes care in practice: findings from the TRANSLATE trial. Diabetes Care 2008; 31: 2238–2243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Grant RW, Hamrick HE, Sullivan CM. et al. Impact of population management with direct physician feedback on care of patients with type 2 diabetes. Diabetes Care 2003; 26: 2275–2280 [DOI] [PubMed] [Google Scholar]
- 21. Jaffe MG, Lee GA, Young JD. et al. Improved blood pressure control associated with a large-scale hypertension program. JAMA 2013; 310: 699–705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Sigler BE. Investigating the perceptions of care coordinators on using behavior theory-based mobile health technology with medicaid populations: a grounded theory study. JMIR Mhealth Uhealth 2017; 5: e36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Lewin ME, SH A.. America's Health Care Safety Net: Intact But Endangered. Washington, DC: Institute of Medicine, 2000 [Google Scholar]
- 24. Broderick A, Haque F.. Mobile health and patient engagement in the safety net: a survey of community health centers and clinics. Issue Brief (Commonw Fund) 2015; 9: 1–9 [PubMed] [Google Scholar]
- 25. Hill-Briggs F, Renosky R, Lazo M. et al. Development and pilot evaluation of literacy-adapted diabetes and CVD education in urban, diabetic African Americans. J Gen Intern Med 2008; 23: 1491–1494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Wallace AS, Seligman HK, Davis TC. et al. Literacy-appropriate educational materials and brief counseling improve diabetes self-management. Patient Educ Couns 2009; 75: 328–333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Hill-Briggs F, Smith AS.. Evaluation of diabetes and cardiovascular disease print patient education materials for use with low-health literate populations. Diabetes Care 2008; 31: 667–671 [DOI] [PubMed] [Google Scholar]
- 28. Tsang JY, Blakeman T, Hegarty J. et al. Understanding the implementation of interventions to improve the management of chronic kidney disease in primary care: a rapid realist review. Implement Sci 2016; 11: 47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Davy C, Bleasel J, Liu H. et al. Factors influencing the implementation of chronic care models: a systematic literature review. BMC Fam Pract 2015; 16: 102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Hommel KA, Hente E, Herzer M. et al. Telehealth behavioral treatment for medication nonadherence: a pilot and feasibility study. Eur J Gastroenterol Hepatol 2013; 25: 469–473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Fisher P, McCarney R, Hasford C. et al. Evaluation of specific and non-specific effects in homeopathy: feasibility study for a randomised trial. Homeopathy 2006; 95: 215–222 [DOI] [PubMed] [Google Scholar]
- 32. Tuot DS, Grubbs V.. Chronic kidney disease care in the US safety net. Adv Chronic Kidney Dis 2015; 22: 66–73 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Greer RC, Cooper LA, Crews DC. et al. Quality of patient-physician discussions about CKD in primary care: a cross-sectional study. Am J Kidney Dis 2011; 57: 583–591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Kellerman SE, Herold J.. Physician response to surveys. A review of the literature. Am J Prev Med 2001; 20: 61–67 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.