Abstract
Aim:
The aim of this study was to compare the adhesion of glass-ceramic overlays to tooth structure, under the effect of shear forces, using different bonding systems.
Materials and Methods:
Thirty healthy lower third molars were selected and randomly allocated into three groups (n = 10). Group 1: overlays bonded to tooth structure using Panavia V5 with immediate dentin sealing (IDS); Group 2: overlays bonded using Panavia V5 without IDS; and Group 3: overlays bonded using heated composite combined with a bonding agent with IDS. All the restorations were made of glass-ceramic (Suprinity, Vita). The restored teeth were then stored in distilled water for 7 days and at room temperature. Shear forces were applied using a universal testing machine. Load and displacement were recorded at intervals of 0.1 s. A statistical analysis was used to compare the groups.
Results:
The mean resistance to fractures ± standard deviation obtained for the Groups 1, 2, and 3 was, respectively, 15.7440 ± 2.13, 12.0750 ± 1.41, and 8.33364 ± 2.85 MPa. The analysis of variance was highly significant (P < 0.001) allowing us to reject the null hypothesis of equality between the three groups. Comparisons between pairs also provided significant results.
Conclusion:
Bonding using Panavia V5 with IDS showed a better resistance to shear forces when compared to other bonding techniques. The application of IDS increased the adhesion.
Keywords: Ceramic, immediate dentin sealing, overlay, shear forces
INTRODUCTION
The overlay is an indirect dental restoration, which can be considered as “the successor to the peripheral crown.” It can be made of ceramic or resin composite. It is a viable alternative to large direct resin composite and to a more invasive crown. Moreover, its use does not require any root anchorage through the placement of a root-retained post.[1]
Nowadays, adhesive dentistry has revolutionized our everyday practice. It has permitted a minimally invasive approach. In addition, it helped achieving improved esthetic, functional, and mechanical results.[2]
Progresses in adhesive dentistry along with computer-aided design/computer-aided manufacturing technologies and the use of newly bioactive materials have contributed to a better preservation of sound dental tissue.[2]
An optimal bonding is an absolute prerequisite for the realization of an overlay, insofar as it is subjected to strong occlusal forces and it has minimal mechanical retention. It is, therefore, necessary to investigate which adhesive system can best resist shear forces.[1]
There are different types of adhesive system available on the market, such as adhesive systems without adhesive capacity, which require the use of a bonding system, adhesive systems with adhesive capacity, and self-adhesive systems, which do not require any conditioning of the dental substrate, or preparation of the surfaces.
Immediate dentin sealing (IDS), which consists on applying a dental bonding agent in three steps (etching, primer, and bonding) (three-step etch and rinse) immediately after the preparation of the dentin (freshly cut dentin), is well known to improve the bond strength of indirect restorations.[3]
To the best knowledge of the authors, there is a lack of data concerning the shear bond strength of preheated resin composite used to bond indirect ceramic restorations.[4] Only a few have compared the preheated composite and the resin cement for luting of indirect restorations.[5]
The aim of this study is to compare the resistance to shear forces of overlays bonded with two adhesive systems without adhesive capacity: Panavia V5 (with and without IDS) and heated composite combined with a bonding agent (with IDS).
MATERIALS AND METHODS
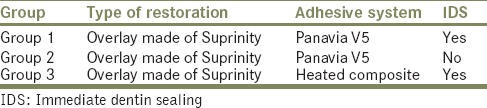
Thirty healthy lower third molars were extracted for reasons such as a lack of space, eruption issues, or the presence of a cyst. After extraction, the teeth were stored in a physiological saline solution and at room temperature for 7 days maximum. They were then randomly allocated to three groups (n = 10) [Table 1]. The agreement of the Ethics Committee of the Erasme Academic Hospital (Ref: P2017/231) was granted.
Table 1.
Teeth preparation following their group
Teeth preparation
The teeth have received a standardized dental preparation. Pits of 2.5 mm of depth are first prepared using a round diamond bur (green ring) with a head diameter of 2.5 mm (Dumont Instrument reference: 806314001; Brussels, Belgium), starting with the center of the buccal and lingual grooves, followed by the central groove mesially and distally and by the tip of the cuspids. The bur is penetrated in the tooth structure until full penetration of the cylinder of the bur. After preparation, the depths of the pits are checked using a periodontal probe. The bottoms of the grooves are marked with a pencil. All the grooves are then joined together using a diamond disc bur (green ring): occlusal reduction bur from Dumont Instrument (reference: 806314068; Brussels, Belgium) until disappearance of the pencil marks, to obtain a round and anatomical reduction. The same operator performed all the preparations. The preparations are nonretentive and present a “flat” configuration. The retention of the overlays will depend exclusively on the adhesive system. New burs were used for each tooth, and all the drillings are performed under water irrigation.
Immediate dentin sealing
IDS on 20 molars was performed (Groups 1 and 3) before bonding the overlays. A three-step adhesive system (three-step Etch-and-Rinse-OptiBond FL, Kerr Italia Srl, Scafati, Salerno, Italy) was applied following the manufacturer's instructions. A glycerine layer was then applied and followed by a polymerization for an extra 10 s.
Finally, the enamel periphery was re-prepared using a green ring chamfer diamond bur from Dumont Instruments (reference: 806314199).[1,2,3,6] No IDS was performed on the remaining 10 teeth (Group 2). The teeth were then kept in a physiological saline solution for 3 days at room temperature.
Impression and realization of the restorations
All the teeth were restored with an indirect restoration (overlay). Intraoral digital impressions were taken using the Trios® system (3Shape). A digital 3D model was prepared using the Cerec InLab software (Dentsply Sirona, Philadelphia, USA) [Figures 1 and 2]. All the overlays were milled in a 14 mm Suprinity block (VITA Zahnfabrik, Bad Säckingen, Deutschland). Finally, the restorations underwent crystallization in a ceramic oven (at a temperature up to 840°C).
Figure 1.
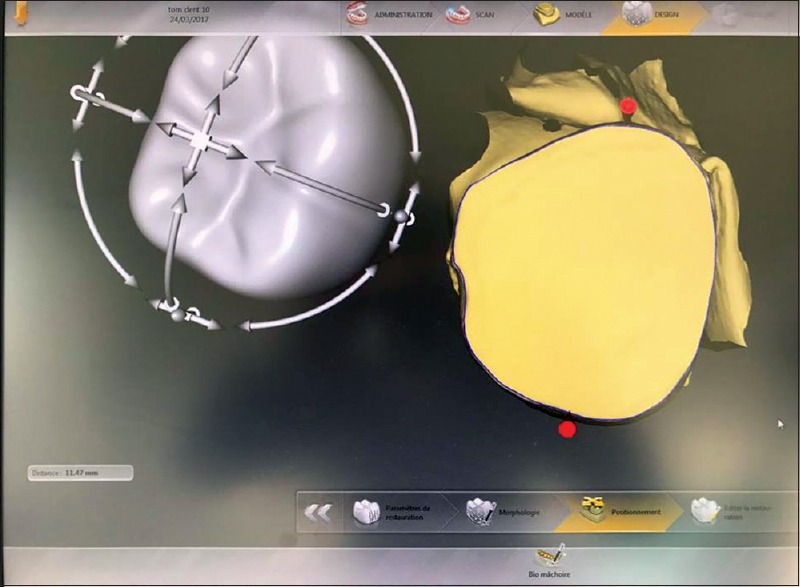
Illustration of the first step to realize a three-dimensional model, using Cerec InLab software
Figure 2.
Three-dimensional onlay model, validated before the milling
Bonding
-
Dental tissue treatment
-
Adhesive system Group 1 and Group 2 protocol:
- Treatment of the enamel: “Tooth primer” (20s) and air dried without polymerization
- Treatment of the dentin: Sandblasting with aluminum oxide (50 microns),[7] “tooth primer” (20s), and air dried.
-
Adhesive system Group 3 protocol
- Treatment of the dentin: Sandblasting using aluminum oxide (50 microns),[7] “tooth primer” (20s), and air dried
- Treatment of the enamel: Etching (37% phosphoric acid) for 30 s, rinse, and application of a bonding agent without polymerization.
-
Ceramic restoration treatment (similar for the three groups): Application of a 10% hydrofluoric acid (20s),[8,9] rinsing (20s), and air dried (20s). The overlays were then immersed in an ultrasonic distilled water bath for 3 min.[9] It is followed by the application of a silane in multiple layers and left untouched for a few minutes. They were then air dried and heated using a polymerization lamp.[10,11,12] Finally, a thin layer of bonding agent was applied without polymerization.[13]
-
Application of the adhesive system
- Group 1: Ten teeth, with IDS, were bonded using Panavia V5 (adhesive system without adhesive capacity; Kuraray Noritake Dental Inc., Okayama, Japan), which is applied under constant pressure. The excess of material was removed and polymerization for 1 min from the occlusal surface and then for 20 s per face. The polishing is performed using a fine grain diamond flame bur (red ring)
- Group 2: Ten teeth without IDS were bonded using Panavia V5, which is applied under constant pressure. The excess of material was removed and polymerization for 1 min from the occlusal surface and then for 20 s per face. The polishing is performed using a fine grain diamond flame bur (red ring)
- Group 3: Ten teeth, with IDS, were bonded using a heated resin composite (photopolymerizable composite compule tube heated at 60° for 15 min, with a Heater Ena Heat from Micerium SPA, Avegno GE, Italy). It is then applied on the tooth. A constant pressure is applied. The excess of material is removed. A polymerization is carried out for 1 min from the occlusal surface and then for 20 s per face. It is followed by a polishing, using a low diamond flame bur (red ring).[9]
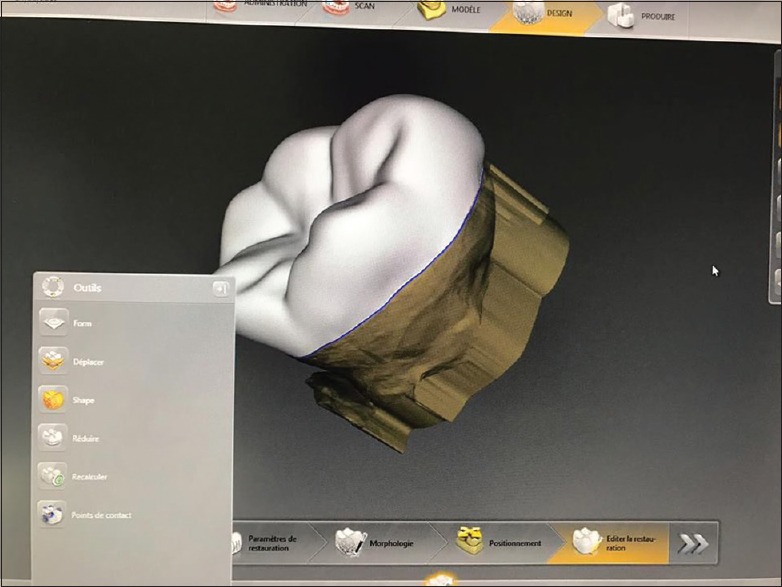
Shear test
The roots of each tooth were immersed in a resistant thermopolymerizable resin (Novodur resin, Novodent ETS; Eschen, Liechtenstein) with the tooth/overlay limits protruding by 2 mm beyond the resin support and then placed in a pot under a 2.5 bar pressure. Each tooth was placed in a device at 90° to the vertical plane [Figure 3]. The ceramic restorations were subjected to shear forces applied at 1 mm from the tooth/overlay limit using a universal testing machine [INSTRON 5585, Massachusetts, USA; Figure 4]. Forces were expressed in Newton and were applied until fracture which could be of different types:
Figure 3.
Schematic illustration of shear forces applied at 1 mm from the dentoprosthetic limit on the ceramic restoration through the INSTRON 5585 machine. Forces are applied vertically regarding to the tooth position
Figure 4.
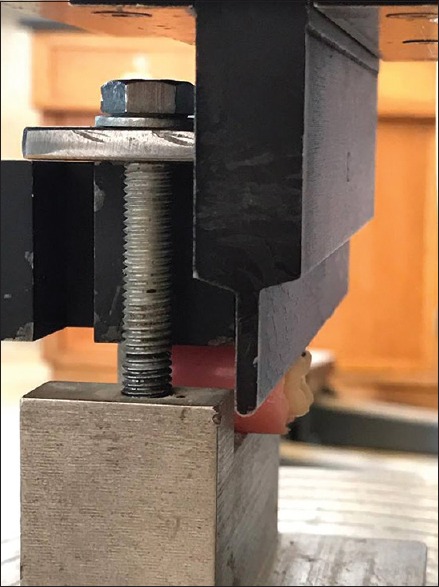
The INSTRON 5585 machine
Type 1: Adhesive fracture between the bonding agent and the dentin, between the bonding agent and the resin cement, or between the resin cement and the ceramic
Type 2: Cohesive fracture within the ceramic, within the resin cement, or within the dentin
Type 3: Cohesive and adhesive fracture
Type 4: Fracture of the support.
Our results were then converted into Megapascal (MPa), by dividing the load (in Newton) by the bonding surface (in mm2), which was previously measured using a dedicated software (ARCHICAD, Budapest, Hungary).
RESULTS
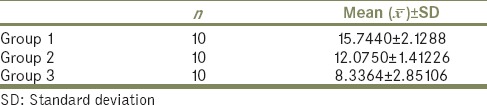
The shear bond strength of the different systems tested is shown in Table 2.
Table 2.
Shear forces results. With the mean (x̄) and the standard deviation for each group
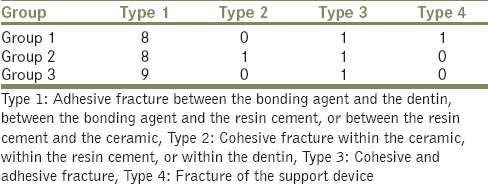
Examination of the fractured surfaces showed similar results between Groups 1, 2, and 3 [Table 3], where the most frequent fracture pattern observed was of “adhesive type” (Type 1). With the use of IDS, the adhesion was strong enough to induce fracture of the device used for the support of the samples (Type 4). Only Group 2 showed a cohesive fracture within the dentin.
Table 3.
Results showing the fractures for each group, with the type of fracture
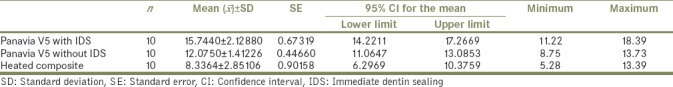
A descriptive statistical analysis was performed and is presented in Tables 3 and 4.
Table 4.
Paired comparisons between adhesive systems using a Kolmogorov-Smirnov test
A Kolmogorov–Smirnov test was performed, confirming that the data followed a normal distribution. The data were subjected to a statistical analysis of variance (ANOVA) with a 5% significance level. The ANOVA was highly significant (P < 0.001), so we could reject the null hypothesis of equality of the three mean shear bond strengths. The paired comparisons between the adhesive systems, using a Bonferroni test, also provided significant results. These results are shown in Table 5.
Table 5.
Paired comparisons between adhesive systems using a Bonferroni test
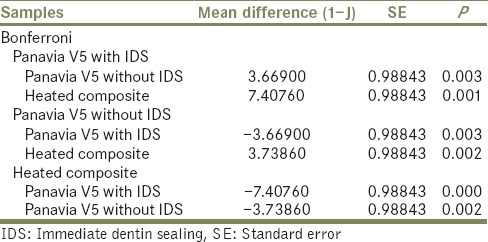
When comparing Panavia V5 with IDS and without IDS, the P value was 0.003 [Table 5]. The results were, therefore, significant. Panavia V5 with IDS exhibited a stronger adhesion with mean shear bond strength of 15.744 MPa against 12.075 MPa for the same system without IDS [Table 2].
When comparing Panavia V5 without the IDS with the heated composite, the P value was 0.002 [Table 5]. The results were, therefore, significant. The adhesion to Panavia V5 without IDS exhibited a stronger adhesion with a mean shear bond strength of 12.0750 MPa versus 8.333 MPa for the heated composite [Table 2].
When comparing Panavia V5 with IDS and heated composite obtained a P value inferior to 0.001 (P = 0.000) [Table 5]. The results were, therefore, highly significant. Panavia V5 with IDS had a shear bond strength of 15.7440 versus 8.333 MPa for the heated composite [Table 2].
Therefore, in the limit of our study, Panavia V5 with IDS exhibited the highest shear bond strength of 18.390 MPa and the highest mean of 15.744 [Table 2].
DISCUSSION
Overlays are indirect restorations with full cusp coverage. They are particularly indicated for the rehabilitation of heavily damaged teeth and are a viable alternative to the peripheral crown.
Overlays can be made of ceramic or composite. We chose in our study to use a glass-ceramic overlay (Suprinity, Vita). It consists of a glass matrix with alkaline ternary oxides and at least 30% by volume of crystalline fillers such as leucite. It contains also some lithium monosilicate and zirconia.
The adequate choice of material and of adhesive system is critical to achieve proper functional and esthetic results, along with a good marginal seal.
Since overlays do not have mechanical retention, an optimal bonding through a strict bonding protocol is of utmost importance. It consists first in the treatment of the intaglio surface of the glass-ceramic restoration using hydrofluoric acid for 20 s. It will influence the topography of the surface/interface and therefore the bonding strength of the ceramic.[13] It is followed by the application of a silane on the prosthesis intaglio surface. Many studies showed that heating it at 100°C increases its efficiency by eliminating water, alcohol, and other by-products from the silanized surface.[10,11,12]
At the level of the tooth, sandblasting forms micro-roughnesses, which can increase the bonding surface and therefore allows a better adhesion.[7,14] Furthermore, many studies showed that stronger bonding is achieved on enamel rather than on dentin.[15,16]
Since the early 90s, it has been well established by several authors[1,3,17,18,19] that the application of a resin coating on freshly cut dentin using a three-step etch-and-rinse system (IDS) protects the pulp by sealing the dentinal tubules, reduces bacterial leakage and dental sensitivity, avoids contamination by temporary cements[20] and space formation, allows the bonding agent and the adhesive layer to be polymerized in two steps,[1,21,22] and then avoids the collapse of the uncured dentin-resin during insertion of the restoration.[1,3,23,24] In our study, we agreed with the previous researches recommending to immediately seal the freshly cut dentin (IDS) to significantly improve bond strength.
The choice of an adequate adhesive system is another critical point.
There are three adhesive subclasses which are the adhesive systems without adhesive capacity that require the use of a bonding agent; the adhesive systems with adhesive capacity; and the self-adhesive systems that require no dental substrate preparation or surface preparation. The latter allows a simplification of the bonding protocol.
In our study, we have only tested an adhesive system without adhesive capacity (Panavia V5). It is a resin without reactive groups but also contains the 10-methacryloyloxydecyl dihydrogen phosphate (MDP) monomer, which is considered as one of the most effective functional monomers for dental adhesives. It is extremely effective on enamel, dentin, and metal alloys. Therefore, Panavia V5 is considered as a high-performing and resistant material for cementation to dental structures and metals.[25] If compared to self-adhesive systems, the Panavia V5 is showing higher adhesion performances.[16]
In addition to the subclasses of adhesive systems, there are also three types of polymerization mode: pure photopolymerization (such as for the heated composite) where the processing time is controlled by the clinician, chemical polymerization (where two components are mixed to initiate a reaction), and dual polymerization (chemical and photopolymerization such as for Panavia V5). For the chemical and dual polymerization, the working and setting times are no longer dependent on the clinician, which can make the insertion of the restoration and the removal of the excesses of material more difficult.
Even though the use of a photopolymerizable adhesive system requires the restorations to allow enough light transmission in order to obtain the maximum possible degree of conversion, this directly affects the mechanical properties, the bond strength on the substrate, as well as the esthetic results.[26]
The viscosity of the material has also to be taken into account. We observed in our study that the insertion of the overlays was more difficult with the heated composite, which is more viscous, than with Panavia V5. It is then recommended to use an ultrasonic tip when using heated composite. On the other hand, once the restoration was placed, it was more stable and the removal of the excesses was done more easily with the heated composite than with Panavia V5.
Whenever a proper bonding in an adequate environment (dry working area isolated under dental dam) can be achieved, the use of overlays is indicated.
To the best of our knowledge, our study is the first to compare the bonding of an indirect glass-ceramic restoration with the new Panavia V5 and a preheated resin composite.
Our results showed that Group 3 (heated composite combined with a bonding agent) exhibited lower bond strength when compared to Groups 1 and 2 (Panavia V5 with, and without IDS). These were not in accordance with a previous study by Sarr et al.,[27] where feldspathic ceramic blocks were bonded to dentin using composite cement. The authors obtained the highest μ-shear bond strength when using a two-step self-adhesive (Clearfil SE) combined with a restorative composite (Clearfil APX). This combination was, therefore, recommended by the authors in clinical situations where the restoration allows sufficient light transmission. Kameyama et al.[28] also observed higher microtensile bond strength (μ-TBS) when using a two-step self-etch adhesive combined with a light-cured resin composite compared to conventional dual-cure resin cement.
The differences observed in our research and other contradictory research may be due to the presence in the Panavia V5 of the MDP monomer. This monomer might contribute in the improvement of the bond strength.
More research is needed as results obtained in the study are contradictory.
Our results showed that the adhesive system with IDS (Group 1) showed a higher shear bond strength than the same system without IDS (Group 2). Our results are in accordance with the study of Okuda et al.,[17] where the authors evaluated the effect of a resin coating on μ-TBSs of indirect restorations to dentin using resin cement. The authors recommended applying a “resin coating” (Clearfil protect bond combined with a flowable resin composite [Protect Liner F]) on freshly cut dentin to prevent pulp irritation and to significantly increase the μ-TBS of indirect restorations to dentin (P < 0.05).
Islam et al.[18] also concluded that a resin coating with hybrid bond significantly improved the bonding of dentin resin cement to dentin in composite crown restorations (P < 0.05).
In another study, Jayasooriya et al.[29] showed that the application on a freshly cut dentin of a resin coating using a dentin bonding system combined with a flowable resin composite significantly improved μ-TBS of resin cement Panavia F to dentin in indirect restorations (P < 0.05), which is in accordance with our results.
Our study could have been improved by considering some points. The buccal temperature is higher than that of our test (23°C), which can modify certain properties of the materials. Overlays should have been dynamically aged by thermocycling, which would have mimicked the real conditions of the oral environment.
CONCLUSION
Glass-ceramic overlays can be a viable alternative to crowns for the restoration of heavily damaged teeth. Within the limits of our study, Panavia V5 with IDS showed the highest shear bond strength. Moreover, whenever bonding to dentin, we recommend the application of IDS, which significantly increases the shear bond strength. However, we cannot translate our findings into clinical reality. Long-term in vivo prospective studies are needed to confirm our findings.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Magne P. Immediate dentin sealing: A fundamental procedure for indirect bonded restorations. J Esthet Restor Dent. 2005;17:144–54. doi: 10.1111/j.1708-8240.2005.tb00103.x. [DOI] [PubMed] [Google Scholar]
- 2.Magne P, Knezevic A. Influence of overlay restorative materials and load cusps on the fatigue resistance of endodontically treated molars. Quintessence Int. 2009;40:729–37. [PubMed] [Google Scholar]
- 3.Magne P, So WS, Cascione D. Immediate dentin sealing supports delayed restoration placement. J Prosthet Dent. 2007;98:166–74. doi: 10.1016/S0022-3913(07)60052-3. [DOI] [PubMed] [Google Scholar]
- 4.Kramer MR, Edelhoff D, Stawarczyk B. Flexural strength of preheated resin composites and bonding properties to glass-ceramic and dentin. Materials (Basel) 2016;9:E83. doi: 10.3390/ma9020083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bortolotto T, Guillarme D, Gutemberg D, Veuthey JL, Krejci I. Composite resin vs. resin cement for luting of indirect restorations: Comparison of solubility and shrinkage behavior. Dent Mater J. 2013;32:834–8. doi: 10.4012/dmj.2013-153. [DOI] [PubMed] [Google Scholar]
- 6.Magne P, Douglas WH. Porcelain veneers: Dentin bonding optimization and biomimetic recovery of the crown. Int J Prosthodont. 1999;12:111–21. [PubMed] [Google Scholar]
- 7.Soares CJ, Giannini M, Oliveira MT, Paulillo LA, Martins LR. Effect of surface treatments of laboratory-fabricated composites on the microtensile bond strength to a luting resin cement. J Appl Oral Sci. 2004;12:45–50. doi: 10.1590/s1678-77572004000100009. [DOI] [PubMed] [Google Scholar]
- 8.Peumans M, Hikita K, De Munck J, Van Landuyt K, Poitevin A, Lambrechts P, et al. Effects of ceramic surface treatments on the bond strength of an adhesive luting agent to CAD-CAM ceramic. J Dent. 2007;35:282–8. doi: 10.1016/j.jdent.2006.09.006. [DOI] [PubMed] [Google Scholar]
- 9.Magne P, Schlichting LH, Maia HP, Baratieri LN. In vitro fatigue resistance of CAD/CAM composite resin and ceramic posterior occlusal veneers. J Prosthet Dent. 2010;104:149–57. doi: 10.1016/S0022-3913(10)60111-4. [DOI] [PubMed] [Google Scholar]
- 10.Abduljabbar T, AlQahtani MA, Jeaidi ZA, Vohra F. Influence of silane and heated silane on the bond strength of lithium disilicate ceramics – An in vitro study. Pak J Med Sci. 2016;32:550–4. doi: 10.12669/pjms.323.9851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.de Carvalho RF, Cotes C, Kimpara ET, Leite FP, Özcan M. Heat treatment of pre-hydrolyzed silane increases adhesion of phosphate monomer-based resin cement to glass ceramic. Braz Dent J. 2015;26:44–9. doi: 10.1590/0103-6440201300212. [DOI] [PubMed] [Google Scholar]
- 12.de Carvalho RF, Martins ME, de Queiroz JR, Leite FP, Ozcan M. Influence of silane heat treatment on bond strength of resin cement to a feldspathic ceramic. Dent Mater J. 2011;30:392–7. [PubMed] [Google Scholar]
- 13.Naves LZ, Soares CJ, Moraes RR, Gonçalves LS, Sinhoreti MA, Correr-Sobrinho L, et al. Surface/interface morphology and bond strength to glass ceramic etched for different periods. Oper Dent. 2010;35:420–7. doi: 10.2341/09-152-L. [DOI] [PubMed] [Google Scholar]
- 14.Santos MJ, Bapoo H, Rizkalla AS, Santos GC. Effect of dentin-cleaning techniques on the shear bond strength of self-adhesive resin luting cement to dentin. Oper Dent. 2011;36:512–20. doi: 10.2341/10-392-L. [DOI] [PubMed] [Google Scholar]
- 15.Naumova EA, Ernst S, Schaper K, Arnold WH, Piwowarczyk A. Adhesion of different resin cements to enamel and dentin. Dent Mater J. 2016;35:345–52. doi: 10.4012/dmj.2015-174. [DOI] [PubMed] [Google Scholar]
- 16.Öztürk E, Bolay Ş, Hickel R, Ilie N. Shear bond strength of porcelain laminate veneers to enamel, dentine and enamel-dentine complex bonded with different adhesive luting systems. J Dent. 2013;41:97–105. doi: 10.1016/j.jdent.2012.04.005. [DOI] [PubMed] [Google Scholar]
- 17.Okuda M, Nikaido T, Maruoka R, Foxton RM, Tagami J. Microtensile bond strengths to cavity floor dentin in indirect composite restorations using resin coating. J Esthet Restor Dent. 2007;19:38–46. doi: 10.1111/j.1708-8240.2006.00062.x. [DOI] [PubMed] [Google Scholar]
- 18.Islam MR, Takada T, Weerasinghe DS, Uzzaman MA, Foxton RM, Nikaido T, et al. Effect of resin coating on adhesion of composite crown restoration. Dent Mater J. 2006;25:272–9. doi: 10.4012/dmj.25.272. [DOI] [PubMed] [Google Scholar]
- 19.Nakabayashi N, Kojima K, Masuhara E. The promotion of adhesion by the infiltration of monomers into tooth substrates. J Biomed Mater Res. 1982;16:265–73. doi: 10.1002/jbm.820160307. [DOI] [PubMed] [Google Scholar]
- 20.Paul SJ, Schärer P. Effect of provisional cements on the bond strength of various adhesive bonding systems on dentine. J Oral Rehabil. 1997;24:8–14. doi: 10.1046/j.1365-2842.1997.00484.x. [DOI] [PubMed] [Google Scholar]
- 21.McCabe JF, Rusby S. Dentine bonding – The effect of pre-curing the bonding resin. Br Dent J. 1994;176:333–6. doi: 10.1038/sj.bdj.4808447. [DOI] [PubMed] [Google Scholar]
- 22.Frankenberger R, Sindel J, Krämer N, Petschelt A. Dentin bond strength and marginal adaptation: Direct composite resins vs.ceramic inlays. Oper Dent. 1999;24:147–55. [PubMed] [Google Scholar]
- 23.Dietschi D, Magne P, Holz J. Bonded to tooth ceramic restorations: In vitro evaluation of the efficiency and failure mode of two modern adhesives. Schweiz Monatsschr Zahnmed. 1995;105:299–305. [PubMed] [Google Scholar]
- 24.Dietschi D, Herzfeld D. In vitro evaluation of marginal and internal adaptation of class II resin composite restorations after thermal and occlusal stressing. Eur J Oral Sci. 1998;106:1033–42. doi: 10.1046/j.0909-8836.1998.eos106609.x. [DOI] [PubMed] [Google Scholar]
- 25.Yoshihara K, Nagaoka N, Okihara T, Kuroboshi M, Hayakawa S, Maruo Y, et al. Functional monomer impurity affects adhesive performance. Dent Mater. 2015;31:1493–501. doi: 10.1016/j.dental.2015.09.019. [DOI] [PubMed] [Google Scholar]
- 26.De Souza G, Braga RR, Cesar PF, Lopes GC. Correlation between clinical performance and degree of conversion of resin cements: A literature review. J Appl Oral Sci. 2015;23:358–68. doi: 10.1590/1678-775720140524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sarr M, Mine A, De Munck J, Cardoso MV, Kane AW, Vreven J, et al. Immediate bonding effectiveness of contemporary composite cements to dentin. Clin Oral Investig. 2010;14:569–77. doi: 10.1007/s00784-009-0327-8. [DOI] [PubMed] [Google Scholar]
- 28.Kameyama A, Bonroy K, Elsen C, Lührs AK, Suyama Y, Peumans M, et al. Luting of CAD/CAM ceramic inlays: Direct composite versus dual-cure luting cement. Biomed Mater Eng. 2015;25:279–88. doi: 10.3233/BME-151274. [DOI] [PubMed] [Google Scholar]
- 29.Jayasooriya PR, Pereira PN, Nikaido T, Tagami J. Efficacy of a resin coating on bond strengths of resin cement to dentin. J Esthet Restor Dent. 2003;15:105–13. doi: 10.1111/j.1708-8240.2003.tb00325.x. [DOI] [PubMed] [Google Scholar]


