Abstract
Purpose:
This systematic review aimed to evaluate retention failures in cement- and screw-retained fixed restorations on dental implants in partially edentulous arches.
Methods:
The relevant articles were retrieved from MEDLINE (PubMed), Cochrane Library, and EBSCO electronic databases for articles published from January 1995 to January 2016 and were restricted to randomized controlled trials and retrospective and prospective studies on human subjects that were reported in English. A further hand search was conducted on individual journals and reference list of the articles found. Reviewed studies which reported retention failures in fixed implant-supported prostheses using screw and cement retention mechanism. Information on the type and nature of restoration, as well as different luting cement, were also collected.
Results:
Thirty-three articles were finalized, 20 short-term clinical studies (up to 5 years) and 13 long-term studies (≥5 years). Out of 33 studies, 16 studies were included in meta-analysis, 8 in short-term and 8 in long-term studies. The results of the meta-analysis for short-term studies showed statistically significant difference between cement-retained and screw-retained prosthesis, with the forest plot favoring cement-retained prostheses (risk ratio [RR]: 0.26; confidence interval [CI]: 0.09–0.74; P < 0.0001; I2 = 79%). In long-term studies, the forest plot revealed statistically significant difference between both retention systems favoring cement-retained prostheses (RR: 0.31; CI: 0.13–0.76; P = 0.03; I2 = 56%).
Conclusion:
Analysis of the short- and long-term studies shows lesser retention failures with cement-retained prostheses when compared to screw-retained prostheses. Further, multicentric, high-quality randomized controlled studies with long-term observations and modified cementation protocols can yield higher grades of recommendation to avoid retention failures.
Keywords: Cement retained, fixed implant restorations, meta-analysis, retention loss, screw retained, systematic review, technical/mechanical complications
INTRODUCTION
Implant-fixed prostheses are very frequently used to rehabilitate partially and completely edentulous patients. Published data inscribe high- and long-term successful treatment outcomes and excellent patient acceptance. Research in implantology has for long been addressing survival of implants. Mechanical complications of components or prosthesis on implants with retention primarily as a factor have been addressed only to a minor extent. Mechanical stability of restorations fixed to implants is imperative for higher prognosis with good stability and reduced complications.[1,2,3]
Fixed implant-supported prostheses may be either screw or cement retained or a combination of both. However, both retention types have relative advantages and disadvantages and may have an influence on the frequency of technical and biologic complications. A complication in implant is defined in the Glossary of Oral and Maxillofacial Implants as “an unexpected deviation from the normal treatment outcome. It is generally classified as either technical or biological, e.g., surgical complication, hemorrhage, damage to the inferior alveolar nerve, infection, delayed wound healing, or lack of osseointegration.”[4] Mechanical and technical risks affecting these complications have been discussed in detail in literature which mention loss of retention, loosening of occlusal screw, loosening of the abutment, fracture of the abutment, fracture of the prosthesis, and chipping of veneering material as major technical reasons.[5,6,7] The performance of implant-supported reconstructions and the complication related to mechanical failures is well documented. A failure rate of 5.5%, 4.8%, and 5.7% has been reported for single crowns (SC), fixed partial dentures, and cantilevered prosthesis over implants at about 5-year observation period.[6]
Planning for prosthesis on implants is affected by factors such as esthetics, economics, and risk factors. Literature is abundant with narrative reviews on advantages and disadvantages of screw versus cement prosthetic retention. Vigolo et al. in 2012 in their 10-year randomized controlled trial showed similar clinical performance of screw- and cement-retained restorations.[8] In spite of these observations, decision-making for mode of retention has always been intriguing and left to the clinicians’ choice due to absence of evidence-based guidelines.
Screw-retained prosthesis is easily retrievable and possesses complete closure at margins. However, occlusal access holes for screws often disrupt occlusal form and also failure of ceramic veneer. Complex clinical and laboratory steps have also added to the total cost of screw-retained prosthesis. The screw used for retaining the prosthesis is often subjected to shear and tensile forces resulting in screw retention failure. To eliminate such disadvantages, cement retention protocols and all ceramic materials can be used. However, cement-retained prosthesis is difficult to retrieve and biologically weak due to difficulty in excess cement removal. Cement residues in the gingival collar remain as permanent etiological factor inducing soft-tissue inflammation in the implant gingival component. This issue to a certain extent has been addressed by the use of long collar, and customized abutments with the margins being positioned in self-cleansable areas have been suggested. Further, when implant abutments lack retention and resistance features of adequate height, surface area, and tapers or number of walls, cement-retained restorations often exhibit retention failures. Therefore, many a times, retention of prosthesis has often been directed to screw retention against cement-retained prosthesis.[9,10,11,12,13,14]
Although specific guidelines exists for when and how, screw- or cement-retained restorations in terms of retention should be used, final selection solely depends on clinician's expertise and patient's affordability. This is mainly due to lack of high level of evidence to make pertinent decisions on choosing the mechanism for prosthesis retention. Although randomized controlled trials and prospective and retrospective studies have been done concerning to the biological and technical complications, no systematic review has compared screw- and cement-retained implant prostheses in terms of retention failures alone. A systematic review by Ma and Fenton[15] in 2015 summarized the prosthodontic maintenance and complications in screw- and cement-retained implant-fixed prostheses. However, newer studies have been done evaluating success in implant prosthesis with loss of retention as a parameter after 2015. A more recent meta-analysis by Lemos et al.[16] in 2016 exists. However, their primary objective has been the evaluation of marginal bone loss in screw- and cement-retained prosthesis. Prosthodontic complications have been a secondary objective of the study. Further, none of these reviews have focused only on retention failures in cement- and screw-retained prostheses. Therefore, this systematic review along with a meta-analysis was planned to retrieve a detailed data pool from the published literature to consolidate data on retention as a factor affecting success in cement- and screw-retained implant-supported fixed restorations.
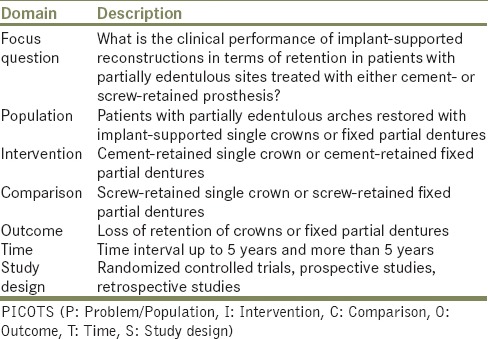
The PICOTS (P: Problem/Population, I: Intervention, C: Comparison, O: Outcome, T: Time, S: Study design) question framed was “What is the clinical performance in terms of retention of implant-supported restorations in patients with partially edentulous sites rehabilitated with either screw- or cement-retained prosthesis over a period up to 5 years and beyond 5 years?” The study design of interest was randomized controlled clinical studies and prospective and retrospective studies [Table 1].
Table 1.
PICOTS of the study
METHODS
This systematic review was structured according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines 2009.[17]
Search strategy
An electronic literature search was independently conducted by two investigators (J. J and S. S) from January 1995 to January 2016, using MEDLINE (PubMed), Cochrane Library, EBSCO databases for articles in English language published in journals of dentistry using following search terms: “dental implant AND screw retained AND cement retained prostheses;” “dental implant AND screw OR cement retained single crowns;” “dental implant AND screw OR cement retained fixed prosthesis;” “dental implant AND screw retained AND cement retained NOT completely edentulous arches;” “dental implant AND screw OR cement retained fixed partial denture;” “dental implant AND screw and cement retained AND mechanical complications;” “dental implant AND screw AND cement retained AND technical complications;” and “dental implant AND screw AND cement retained AND prosthetic complications.” The “related articles” option in the search engines was used. Related articles were identified from existing reviews and also from reference list of obtained studies. The following journals were also searched manually: Journal of Prosthetic Dentistry, Journal of Oral Rehabilitation, Clinical Implant Dentistry and Related Research, International Journal of Prosthodontics, International Journal of Oral and Maxillofacial Implants, International Journal of Oral and Maxillofacial Surgery, International Journal of Periodontics and Restorative Dentistry, Journal of Dental Research, Clinical Oral Implants Research, and Journal of Oral and Maxillofacial Surgery.
Selection of studies
The review process consisted of two parts. The first part aimed at primary screening of identified articles for applicability by reading their abstracts. Complete texts of those articles which were found relevant including those identified by the manual search were evaluated. Any variations in views between the investigators were assessed by a third investigator (R. S). The following set of inclusion and exclusion criteria was applied in the first review phase.
Inclusion criteria
The inclusion criteria of this study were as follows:
Studies with restorations in the form of fixed partial dentures (FPD) or SC on implants
Studies evaluating prosthesis given human participants
Studies with an observation time of at least 1-year postinsertion of definitive prosthesis
Studies designed as randomized controlled trials and nonrandomized retrospective and prospective studies clinical studies.
Exclusion criteria
The exclusion criteria of this study were as follows:
Implant studies on animals
In vitro or bench research studies including finite element analysis
Case series or case reports
Clinical studies which report of implant success on the basis of biological complications and/or no report on technical problems
Clinical studies with < 10 cement- or screw-retained restorations
Clinical studies were data on retention failures could not be obtained or extracted.
Data extraction and meta-analysis
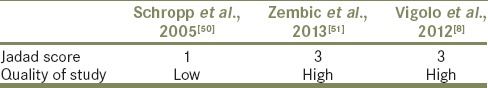
Data regarding loss of retention or retention failure reported in the selected studies were extracted (S. C and B. B) and verified (R. P and P. J). In cement retained, prosthesis which documented debonding/crown loosening and dislodgement purely due to cementation failure or decementation was only taken into consideration. Abutment screw loosening in cement-retained prosthesis was not regarded as retention failure as it is not directly due to failure of luting cement. For screw-retained prosthesis, retention loss due to occlusal/prosthetic/vertical/horizontal/abutment/prosthetic screw loosening was taken into consideration. Studies which had loss of retention or retention failure as their secondary outcome or studies in which data regarding retention failure was only mentioned but not analyzed were also included and data was extracted from them. The Newcastle–Ottawa scale (NOS) was used to assess the methodological quality of the included prospective and retrospective cohort and case–control studies [Table 2].[18] The Jadad scale was used for assessing randomized controlled trials [Table 3].[49] Meta-analysis was based on the Mantel-Haenszel and inverse variance methods. Dichotomous outcome measures of retention failures were presented as risk ratios (RRs) for the number of prosthesis reported in each study. Meta-analysis was performed using Review Manager version 5.3 software, Copenhagen (Nordic Cochrane Centre, The Cochrane Collaboration, 2014) to create forest plots. The I2 quantity was included to express the heterogeneity across the included studies, with 25% corresponding to low heterogeneity, 50% to moderate, and 75% to high.[52]
Table 2.
Quality assessment of the prospective and retrospective nonrandomized studies (Newcastle Ottawa scale)
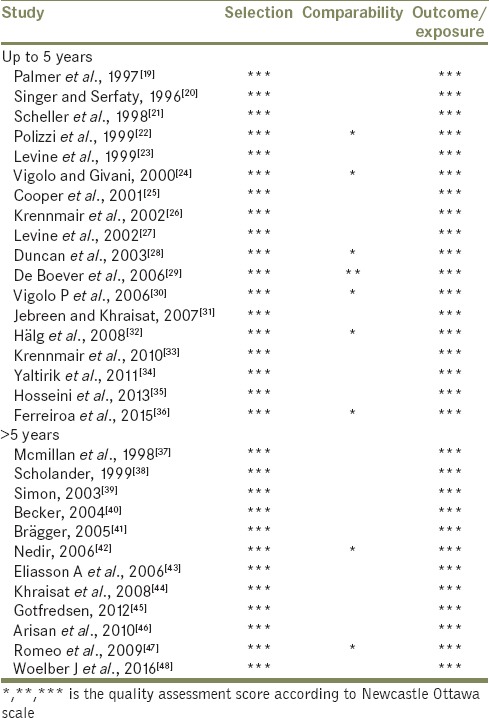
Table 3.
Quality assessment of the randomized controlled studies (Jadad scale)
RESULTS
The initial database search yielded 2029 references. Of these, 1450 were from EBSCO, 582 from PubMed/Medline, and 27 from the Cochrane Library. References if repeated were removed and 1229 studies remained. Inclusion and exclusion criteria were applied to research titles and summaries to yield 35 studies. After further hand searching of articles, 7 more were added. After full-text evaluation of total 42 articles, 9 articles were excluded and total 33 studies were selected, 20 short- and 13 long-term studies [Figure 1].
Figure 1.
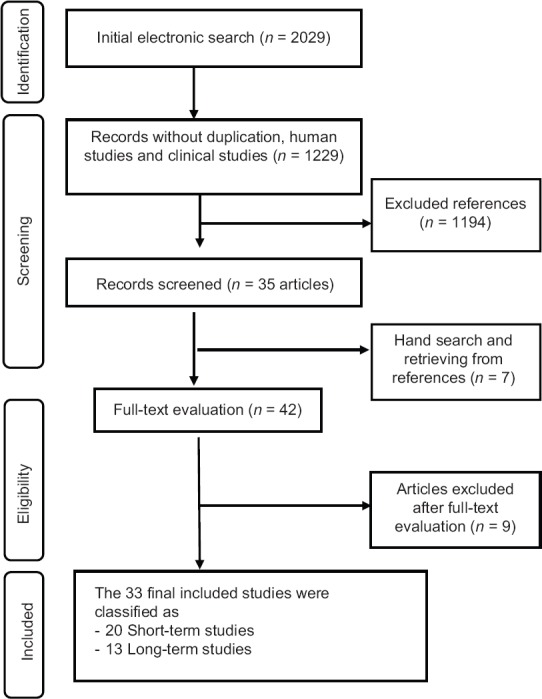
Flowchart of search strategy
The included studies were classified into four categories:
Studies evaluating failure of cement-retained prosthesis with observation period up to 5 years
Studies evaluating failure of screw-retained prosthesis with observation period up to 5 years
Studies evaluating failure of cement-retained prosthesis with observation period more than 5 years
Studies evaluating failure of screw-retained prosthesis with observation period more than 5 years.
Data of the final included studies were tabulated. Incidence of retention failures was obtained. In addition, information on design of study, number of participants, number of implants, mean period of observation, number and type of prosthesis, cement type with its complications, i.e., number of decementations/recementations, or number of occlusal or prosthetic screw loosening was obtained. All the excluded studies along with their reasoning have been mentioned in Table 4. Studies by Zembic et al.,[51] Gotfredsen,[45] and Vigolo et al.[8] were published at two different points of time but included results of the older publication in their recent report. These articles were included only once according to their most recent observation period. The extracted data are mentioned in Tables 5–8.
Table 4.
List of excluded articles with reasons for exclusion
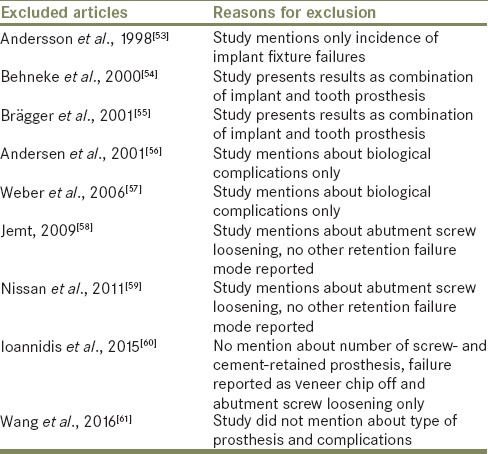
Table 5.
Study characteristics for cement-retained implant prosthesis up to 5 years
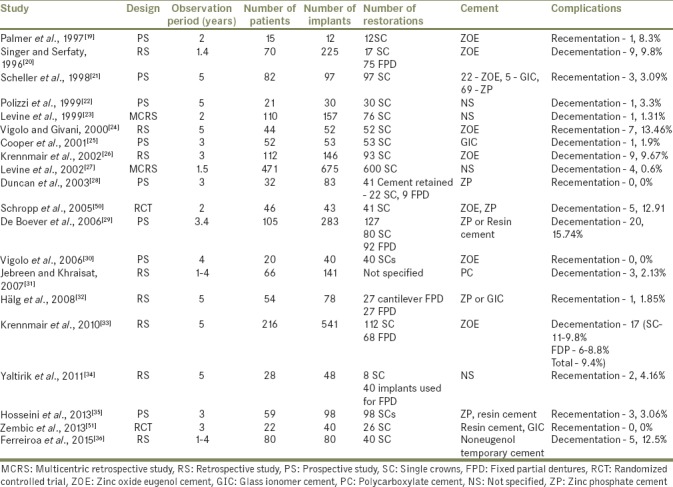
Table 8.
Study characteristics for screw-retained implant prosthesis >5 years
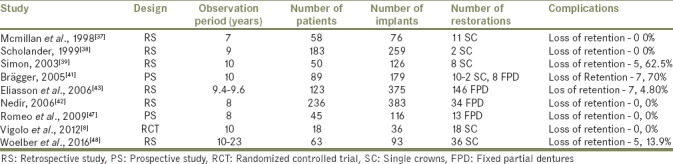
Table 6.
Study characteristics for cement-retained implant prosthesis >5 years
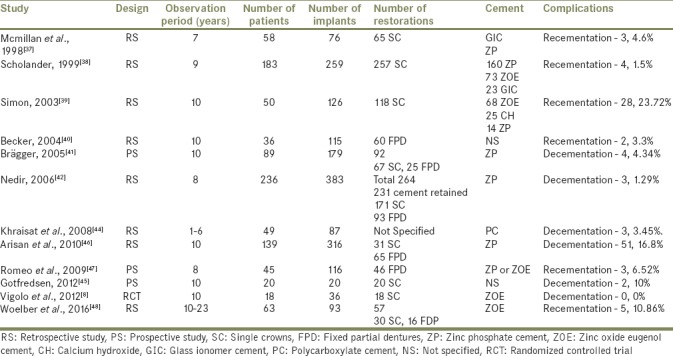
Table 7.
Study characteristics for screw-retained implant prosthesis up to 5 years
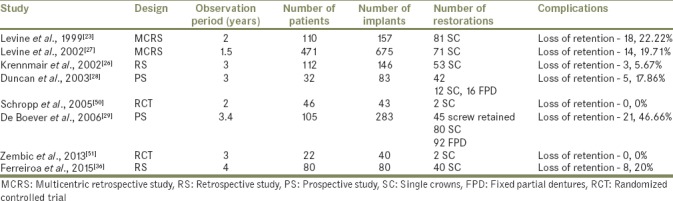
Short-term studies (up to 5 years)
The literature search revealed twenty studies.[19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,50,51] There were two randomized controlled trials,[50,51] eight prospective studies,[19,21,22,25,28,29,30,35] and ten retrospective studies.[20,23,24,26,27,31,32,33,34,36] Twelve studies had evaluated only cement-retained prosthesis,[19,20,21,22,24,25,30,31,32,33,34,35] whereas eight studies had evaluation of both cement- and screw-retained prosthesis.[23,26,27,28,29,36,50,51] Thirteen studies reported only SC,[19,21,22,23,24,25,26,27,30,35,36,50,51] whereas five studies reported both SC and fixed partial dentures.[20,28,29,30,34] One study did not clearly mention types of prosthesis,[31] and another study had reported of fixed dental prosthesis only.[32]
Conventional fixed partial denture provisional and definitive cement (zinc phosphate, glass ionomer, resin, and polycarboxylate cement) were used in nine studies.[21,25,28,29,31,32,35,50,51] One study had also used noneugenol temporary cement for cementation.[34] Provisional cement specifically zinc oxide eugenol were used in six studies.[19,20,24,26,30,33] Cement type was not mentioned in four studies.[22,23,27,34]
The complications, i.e., decementations in case of cement-retained restorations ranged from about 0% to 15.74% and screw loosening in case of screw-retained restorations ranged from 0% to 46.66%.
Long-term studies (more than 5 years)
The literature search revealed 13 studies with observation period more than 5 years (ranging from 6 to 23 years).[8,37,38,39,40,41,42,43,44,45,46,47,48] One study was randomized controlled trial,[8] three studies were prospective studies,[41,45,47] and nine studies were retrospective studies.[37,38,39,40,42,43,44,46,48] Four studies had evaluated only cement-retained prosthesis,[40,44,45,46] whereas eight studies had evaluated both cement- and screw-retained prosthesis.[8,37,38,39,41,42,47,48] One study had evaluated only screw-retained prosthesis.[43] Five studies reported only SC [8,37,38,39,45] and three studies reported only FPD,[40,43,47] whereas four studies reported of both SC and FPD.[41,42,46,48] In one study, the type of prosthesis was not clearly mentioned.[44] Conventional fixed partial denture provisional and definitive cement (zinc phosphate, glass ionomer polycarboxylate, and calcium hydroxide cement) were used in eight studies.[37,38,39,41,42,44,46,47] Zinc oxide eugenol temporary cement was used in two studies.[8,48] Two studies did not mention the cement type used.[40,45]
The complications, i.e., decementations in case of cement-retained restorations ranged from about 0% to 23.72% and screw loosening in case of screw-retained restorations ranged from 0% to 50%.
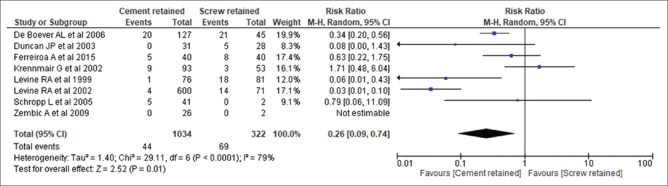
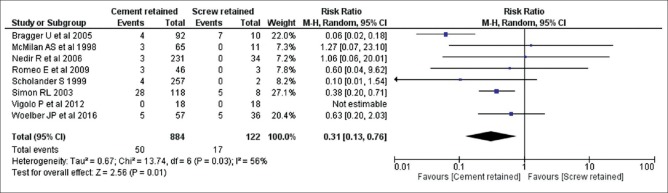
Meta-analysis
Since division was made as short- and long-term studies, and meta-analysis was performed separately for long- and short-term studies. Studies which were included were randomized controlled trials and prospective and retrospective studies. A random-effects model was used to evaluate the retention failure for short- and long-term studies. The results of the meta-analysis for short-term studies are presented in Figure 2. A 5-year meta-analysis showed a statistically significant difference between cement- and screw-retained prostheses, with the forest plot favoring cement-retained prostheses (RR: 0.26; CI: 0.09–0.74; P < 0.0001; I2 = 79%). In long-term studies [Figure 3], there was also a statistically significant difference between cement- and screw-retained prostheses, with the forest plot favoring cement-retained prostheses (RR: 0.31; CI: 0.13–0.76; P = 0.03; I2 = 56%).
Figure 2.
Forest plot showing comparison between failures in cement- and screw-retained prosthesis up to 5 years of observation period
Figure 3.
Forest plot showing comparison between failures in cement- and screw-retained prosthesis more than 5 years of observation period
DISCUSSION
The aim of this systematic review and meta-analysis was to evaluate short- and long-term prosthetic outcomes and complications in cement- and screw-retained implant prosthesis so as to determine which one is to be recommended for clinical application. This, in turn, can give valuable information on expected time when mechanical problems in cement- and screw-retained implant prosthesis. Studies included were divided into their observation time period into short-and long-term studies as this would be directly give idea of implant prognosis as well as the reasons for survival of the prosthesis during the entire period of service in the mouth.
The nonrandomized clinical studies were heterogeneous in number of participants, study designs, methods of outcome evaluation, and evaluation period. The multiple types of implants, their designs and components, edentulous site, restorative method, and material further added to the heterogeneity. Therefore, inferences of higher grades could not be made on the basis of these retrospective and prospective clinical studies. The heterogeneity was further compounded by the variety of implant systems and component being used, placement site, as well as implant restorative techniques and designs. Therefore, it was challenging to derive a clear inference from the included studies. There were three randomized controlled trials identified and included in this review of which two were of high quality on the Jadad scale and one was of low quality. Thus, there exists a need for more well-conducted randomized controlled studies on the evaluation of retention failures.
The systematic review was done with 33 studies in which 20 studies were included in short-term and 13 were included in long-term studies. The retention failure rate in short-term studies (<5 years) ranged from 0% to 15.74% for cement-retained prosthesis and 0% to 46.66% for screw-retained prosthesis. For long-term observation (more than 5 years), the retention failure rate ranged from 0% to 23.72% for cement-retained prosthesis and 0% to 50% for screw-retained prosthesis. Technical complications were reported more for FPDs, especially for cantilever FPDs than those for SCs. Weber and Sukotjo in 2007, from their systematic review, reported the prosthetic success rates of cement- and screw-retained implant-supported prosthesis for more than 6 years as 93.2% and 83.4%, respectively. It should be noted that this review reported success rate considering all technical complications, unlike the present systematic review which considered retention as the only criteria.[62]
Failures were more frequently observed with screw-retained crowns and FPDs compared to cemented SC and FPDs. The retention failure rate of restorations up to 5 years and more than 5 years for screw-retained restorations was comparably higher than that for cemented restorations.
The meta-analysis of the present systematic review was conducted to provide the best scientific evidence for clinicians regarding the clinical performance in terms of retention in screw- and cement-retained prosthesis according to the data collected in the included studies. The meta-analysis summarized all the outcomes extracted from the selected studies. Results of the meta-analysis up to 5 years for retention failure indicated that there was statistically significant difference between both the retention systems, favoring cement-retained prosthesis (P < 0.0001). Long-term studies, i.e., more than 5 years, showed a statistically significant difference between both retention systems favoring cement-retained prosthesis (P = 0.03). In terms of heterogeneity, the studies up to 5 years showed high heterogeneity (79%) than the studies having an observation period of more than 5 years (56%).
Ideally, adequate strength of the luting agent is required for retention of prosthesis yet should allow professional removal of restorations simple. However, literature regarding usage of ideal cement has revealed disagreements. Owing to varied cement, implants, components, and treatment protocols being used in different studies, a standardized cementation protocol was difficult to obtain. Most of the studies used zinc phosphate as definitive cement and zinc oxide eugenol as temporary cement. Of these, zinc phosphate luting agent can be advantageous as mechanical bonding of the cement and substructure exists. This benefits the clinician if the prosthesis has to be removed in case need arises. Zinc oxide eugenol on the other hand being temporary luting agent, guarantees easy removal. It can thus be assumed that cement that performs well a temporary luting agent for tooth-supported restorations may or may not be a definitive luting agent for implant-supported prosthesis. Hence, in this scenario, easy removal still remains a controversial issue. In addition, the implantologist should consider many other parameters of cement retention such as occlusal convergence of abutment, interarch space, abutment material, remaining walls of abutment, type of luting agent, and the definitive occlusion.[63] Abutment surface treatments of grooving and sandblasting may further improve retention of cementation prosthesis.[64]
In cement-retained prosthesis, the major disadvantage that has been reported is biological complication pertaining to excess cement leading to peri-implantitis and mechanical failure pertaining to retention loss. To overcome the problem of excess cement, there has been introduction of extraoral cementation techniques.[65] Further methods to maintain the patency of the abutment screw access hole should be employed, and cementing restorations to abutments extraorally to remove excess cement can further reduce biological complications related to residual cement in sulcular tissue. An attempt to ensure ease of prosthesis retrievability in cement-retained prosthesis is presented as an alternative retention protocol. The screw retrievable cement-retained prosthesis combines advantages of both screw and cement. Thus, this method can probably reduce the amount of prosthetic strain and implant stress.[66]
The failures in screw-retained prosthesis have been found to be higher than cement-retained restorations. Many reasons have been reported in literature for this failure. Fatigue, inadequate tightening torque, inadequate prosthesis fit, poorly machined components, vibrating micro-movement, and excessive loading are a few to mention.[67,68] Torque values often reduce after casting procedures are done. This along with casting micro-irregular rough surfaces at abutment implant contact surfaces further increases the misfit. This generates undue stress, changes in screw geometry, metal fatigue, and strain at the junctions eventually resulting in screw loosening.[69,70]
Cement-retained restorations ensure optimum esthetics, adequate occlusal morphologies, simple laboratory procedures, passive casting fits, and implant splinting if need.[71] Cement-retained prosthesis in both splinted and unsplinted conditions shows lesser strains around implant bone junctions which, in turn, shows lesser crestal resorption due to mechanical loads.[72] If cement-retained restorations are considered as treatment options, the clinician should weigh these pros and cons of the retention mode and other factors of retention as mentioned earlier because incidences of biomechanical risks and failures may lead to fabrication of new prosthesis which can increase the total cost. A progressive luting protocol can be followed which recommends use of cement in increasing order of their strengths until clinical success in retention is achieved.[73] In addition, minor modifications in the design of the restoration superstructure could make them easily retrievable.
Subgroup analysis by categorizing studies according to cement type, screw type, abutment type, or type of prosthesis could not be done. This probably explains the heterogeneity seen in the meta-analysis (high for up to 5-year observations and moderate for more than 5 years)
CONCLUSION
Within the limitation of this systematic review and meta-analysis the following conclusion can be made:
Cement-retained prosthesis shows less retention failures as compared to screw-retained prosthesis
However, the inferences made from this systematic review with meta-analysis should be carefully weighed before the clinical application of the scientific data because of the moderate-to-high level of heterogeneity seen in the meta-analysis and the nature of the majority of clinical studies involved being moderate on the level of evidence
Furthermore, long-term multicentric controlled, standardized studies with adequate data on cement/screw type, protocols of retention, and prosthetic type can aid in credible data for use in future systematic reviews.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Attard NJ, Zarb GA. Implant prosthodontic management of partially edentulous patients missing posterior teeth: The Toronto experience. J Prosthet Dent. 2003;89:352–9. doi: 10.1067/mpr.2003.91. [DOI] [PubMed] [Google Scholar]
- 2.Belser UC, Grütter L, Vailati F, Bornstein MM, Weber HP, Buser D, et al. Outcome evaluation of early placed maxillary anterior single-tooth implants using objective esthetic criteria: A cross-sectional, retrospective study in 45 patients with a 2- to 4-year follow-up using pink and white esthetic scores. J Periodontol. 2009;80:140–51. doi: 10.1902/jop.2009.080435. [DOI] [PubMed] [Google Scholar]
- 3.Jung RE, Zembic A, Pjetursson BE, Zwahlen M, Thoma DS. Systematic review of the survival rate and the incidence of biological, technical, and aesthetic complications of single crowns on implants reported in longitudinal studies with a mean follow-up of 5 years. Clin Oral Implants Res. 2012;23:2–21. doi: 10.1111/j.1600-0501.2012.02547.x. [DOI] [PubMed] [Google Scholar]
- 4.Laney WR, editor. Glossary of Oral and Maxillofacial Implants. Berlin: Quintessence; 2008. [DOI] [PubMed] [Google Scholar]
- 5.Sailer I, Mühlemann S, Zwahlen M, Hämmerle CH, Schneider D. Cemented and screw-retained implant reconstructions: A systematic review of the survival and complication rates. Clin Oral Implants Res. 2012;23(Suppl 6):163–201. doi: 10.1111/j.1600-0501.2012.02538.x. [DOI] [PubMed] [Google Scholar]
- 6.Wittneben JG, Millen C, Brägger U. Clinical performance of screw- versus cement-retained fixed implant-supported reconstructions – A systematic review. Int J Oral Maxillofac Implants. 2014;29(Suppl):84–98. doi: 10.11607/jomi.2014suppl.g2.1. [DOI] [PubMed] [Google Scholar]
- 7.Salvi GE, Brägger U. Mechanical and technical risks in implant therapy. Int J Oral Maxillofac Implants. 2009;24(Suppl):69–85. [PubMed] [Google Scholar]
- 8.Vigolo P, Mutinelli S, Givani A, Stellini E. Cemented versus screw-retained implant-supported single-tooth crowns: A 10-year randomised controlled trial. Eur J Oral Implantol. 2012;5:355–64. [PubMed] [Google Scholar]
- 9.Pauletto N, Lahiffe BJ, Walton JN. Complications associated with excess cement around crowns on osseointegrated implants: A clinical report. Int J Oral Maxillofac Implants. 1999;14:865–8. [PubMed] [Google Scholar]
- 10.Chee WW, Torbati A, Albouy JP. Retrievable cemented implant restorations. J Prosthodont. 1998;7:120–5. doi: 10.1111/j.1532-849x.1998.tb00191.x. [DOI] [PubMed] [Google Scholar]
- 11.Zarb GA, Schmitt A. The longitudinal clinical effectiveness of osseointegrated dental implants: The Toronto study. Part III: Problems and complications encountered. J Prosthet Dent. 1990;64:185–94. doi: 10.1016/0022-3913(90)90177-e. [DOI] [PubMed] [Google Scholar]
- 12.Keith SE, Miller BH, Woody RD, Higginbottom FL. Marginal discrepancy of screw-retained and cemented metal-ceramic crowns on implants abutments. Int J Oral Maxillofac Implants. 1999;14:369–78. [PubMed] [Google Scholar]
- 13.Okamoto M, Minagi S. Technique for removing a cemented superstructure from an implant abutment. J Prosthet Dent. 2002;87:241–2. doi: 10.1067/mpr.2002.119525. [DOI] [PubMed] [Google Scholar]
- 14.Emms M, Tredwin CJ, Setchell DJ, Moles DR. The effects of abutment wall height, platform size, and screw access channel filling method on resistance to dislodgement of cement-retained, implant-supported restorations. J Prosthodont. 2007;16:3–9. doi: 10.1111/j.1532-849X.2006.00150.x. [DOI] [PubMed] [Google Scholar]
- 15.Ma S, Fenton A. Screw- versus cement-retained implant prostheses: A systematic review of prosthodontic maintenance and complications. Int J Prosthodont. 2015;28:127–45. doi: 10.11607/ijp.3947. [DOI] [PubMed] [Google Scholar]
- 16.Lemos CA, de Souza Batista VE, Almeida DA, Santiago JF, Júnior, Verri FR, Pellizzer EP, et al. Evaluation of cement-retained versus screw-retained implant-supported restorations for marginal bone loss: A systematic review and meta-analysis. J Prosthet Dent. 2016;115:419–27. doi: 10.1016/j.prosdent.2015.08.026. [DOI] [PubMed] [Google Scholar]
- 17.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Int J Surg. 2010;8:336–41. doi: 10.1016/j.ijsu.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 18.Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomized studies in meta-analysis. [Last accessed on 2016 Apr 25]. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp .
- 19.Palmer RM, Smith BJ, Palmer PJ, Floyd PD. A prospective study of Astra single tooth implants. Clin Oral Implants Res. 1997;8:173–9. doi: 10.1034/j.1600-0501.1997.080303.x. [DOI] [PubMed] [Google Scholar]
- 20.Singer A, Serfaty V. Cement-retained implant-supported fixed partial dentures: A 6-month to 3-year follow-up. Int J Oral Maxillofac Implants. 1996;11:645–9. [PubMed] [Google Scholar]
- 21.Scheller H, Urgell JP, Kultje C, Klineberg I, Goldberg PV, Stevenson-Moore P, et al. A 5-year multicenter study on implant-supported single crown restorations. Int J Oral Maxillofac Implants. 1998;13:212–8. [PubMed] [Google Scholar]
- 22.Polizzi G, Fabbro S, Furri M, Herrmann I, Squarzoni S. Clinical application of narrow brånemark system implants for single-tooth restorations. Int J Oral Maxillofac Implants. 1999;14:496–503. [PubMed] [Google Scholar]
- 23.Levine RA, Clem DS, Wilson TG, Higgibottom F, Solnit G. Multicenter retrospective analysis of the ITI implant system used for single-tooth replacements: Results of loading for 2 or mare years. Int J Oral Maxillofac Implants. 1999;14:516–20. [PubMed] [Google Scholar]
- 24.Vigolo P, Givani A. Clinical evaluation of single-tooth mini-implant restorations: A five-year retrospective study. J Prosthet Dent. 2000;84:50–4. doi: 10.1067/mpr.2000.107674. [DOI] [PubMed] [Google Scholar]
- 25.Cooper L, Felton DA, Kugelberg CF, Ellner S, Chaffee N, Molina AL, et al. A multicenter 12-month evaluation of single-tooth implants restored 3 weeks after 1-stage surgery. International Journal of Oral and Maxillofacial Implants; 2001;16:182–92. [PubMed] [Google Scholar]
- 26.Krennmair G, Schmidinger S, Waldenberger O. Single-tooth replacement with the frialit-2 system: A retrospective clinical analysis of 146 implants. Int J Oral Maxillofac Implants. 2002;17:78–85. [PubMed] [Google Scholar]
- 27.Levine RA, Clem D, Beagle J, Ganeles J, Johnson P, Solnit G, et al. Multicenter retrospective analysis of the solid-screw ITI implant for posterior single-tooth replacements. Int J Oral Maxillofac Implants. 2002;17:550–6. [PubMed] [Google Scholar]
- 28.Duncan JP, Nazarova E, Vogiatzi T, Taylor TD. Prosthodontic complications in a prospective clinical trial of single-stage implants at 36 months. Int J Oral Maxillofac Implants. 2003;18:561–5. [PubMed] [Google Scholar]
- 29.De Boever AL, Keersmaekers K, Vanmaele G, Kerschbaum T, Theuniers G, De Boever JA. Prosthetic complications in fixed endosseous implant-borne reconstructions after an observations period of at least 40 months. J Oral Rehabil. 2006;33:833–9. doi: 10.1111/j.1365-2842.2006.01638.x. [DOI] [PubMed] [Google Scholar]
- 30.Vigolo P, Givani A, Majzoub Z, Cordioli G. A 4-Year Prospective Study to Assess Peri-Implant Hard and Soft Tissues Adjacent to Titanium Versus Gold-Alloy Abutments in Cemented Single Implant Crowns. J Prosthodont. 2006;15:250–6. doi: 10.1111/j.1532-849X.2006.00114.x. [DOI] [PubMed] [Google Scholar]
- 31.Jebreen SE, Khraisat A. Multicenter retrospective study of ITI implant-supported posterior partial prosthesis in Jordan. Clin Implant Dent Relat Res. 2007;9:89–93. doi: 10.1111/j.1708-8208.2007.00053.x. [DOI] [PubMed] [Google Scholar]
- 32.Hälg GA, Schmid J, Hämmerle CH. Bone level changes at implants supporting crowns or fixed partial dentures with or without cantilevers. Clin Oral Implants Res. 2008;19:983–90. doi: 10.1111/j.1600-0501.2008.01556.x. [DOI] [PubMed] [Google Scholar]
- 33.Krennmair G, Seemann R, Schmidinger S, Ewers R, Piehslinger E. Clinical outcome of root-shaped dental implants of various diameters: 5-year results. Int J Oral Maxillofac Implants. 2010;25:357–66. [PubMed] [Google Scholar]
- 34.Yaltirik M, Gökçen-Röhlig B, Ozer S, Evlioglu G. Clinical evaluation of small diameter straumann implants in partially edentulous patients: A 5-year retrospective study. J Dent (Tehran) 2011;8:75–80. [PMC free article] [PubMed] [Google Scholar]
- 35.Hosseini M, Worsaae N, Schiødt M, Gotfredsen K. A 3-year prospective study of implant-supported, single-tooth restorations of all-ceramic and metal-ceramic materials in patients with tooth agenesis. Clin Oral Implants Res. 2013;24:1078–87. doi: 10.1111/j.1600-0501.2012.02514.x. [DOI] [PubMed] [Google Scholar]
- 36.Ferreiroa A, Peñarrocha-Diago M, Pradíes G, Sola-Ruiz MF, Agustín-Panadero R. Cemented and screw-retained implant-supported single-tooth restorations in the molar mandibular region: A retrospective comparison study after an observation period of 1 to 4 years. J Clin Exp Dent. 2015;7:e89–94. doi: 10.4317/jced.51708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.McMillan AS, Allen PF, Bin Ismail I. A retrospective multicenter evaluation of single tooth implant experience at three centers in the United Kingdom. J Prosthet Dent. 1998;79:410–4. doi: 10.1016/s0022-3913(98)70154-4. [DOI] [PubMed] [Google Scholar]
- 38.Scholander S. A retrospective evaluation of 259 single-tooth replacements by the use of Brånemark implants. Int J Prosthodont. 1999;12:483–91. [PubMed] [Google Scholar]
- 39.Simon RL. Single implant-supported molar and premolar crowns: A ten-year retrospective clinical report. J Prosthet Dent. 2003;90:517–21. doi: 10.1016/j.prosdent.2003.08.025. [DOI] [PubMed] [Google Scholar]
- 40.Becker CM. Cantilever fixed prostheses utilizing dental implants: A 10-year retrospective analysis. Quintessence Int. 2004;35:437–41. [PubMed] [Google Scholar]
- 41.Brägger U, Karoussis I, Persson R, Pjetursson B, Salvi G, Lang N, et al. Technical and biological complications/failures with single crowns and fixed partial dentures on implants: A 10-year prospective cohort study. Clin Oral Implants Res. 2005;16:326–34. doi: 10.1111/j.1600-0501.2005.01105.x. [DOI] [PubMed] [Google Scholar]
- 42.Nedir R, Bischof M, Szmukler-Moncler S, Belser UC, Samson J. Prosthetic complications with dental implants: From an up-to-8-year experience in private practice. Int J Oral Maxillofac Implants. 2006;21:919–28. [PubMed] [Google Scholar]
- 43.Eliasson A, Eriksson T, Johansson A, Wennerberg A. Fixed partial prostheses supported by 2 or 3 implants: A retrospective study up to 18 years. Int J Oral Maxillofac implants. 2006;21:567–74. [PubMed] [Google Scholar]
- 44.Khraisat A, Jebreen SE, Baqain ZH, Smadi L, Bakaeen L, Abu-Hammad O, et al. Multicenter retrospective study of cement-retained implant-supported anterior partial prostheses: Success and restoration evaluation. Int J Oral Maxillofac Implants. 2008;23:705–8. [PubMed] [Google Scholar]
- 45.Gotfredsen K. A 10-year prospective study of single tooth implants placed in the anterior maxilla. Clin Implant Dent Relat Res. 2012;14:80–7. doi: 10.1111/j.1708-8208.2009.00231.x. [DOI] [PubMed] [Google Scholar]
- 46.Arisan V, Bölükbaşi N, Ersanli S, Ozdemir T. Evaluation of 316 narrow diameter implants followed for 5-10 years: A clinical and radiographic retrospective study. Clin Oral Implants Res. 2010;21:296–307. doi: 10.1111/j.1600-0501.2009.01840.x. [DOI] [PubMed] [Google Scholar]
- 47.Romeo E, Tomasi C, Finini I, Casentini P, Lops D. Implant-supported fixed cantilever prosthesis in partially edentulous jaws: A cohort prospective study. Clin Oral Implants Res. 2009;20:1278–85. doi: 10.1111/j.1600-0501.2009.01766.x. [DOI] [PubMed] [Google Scholar]
- 48.Woelber J, Ratka-Krueger P, Vach K, Frisch E. Decementation Rates and the Peri-Implant Tissue Status of Implant-Supported Fixed Restorations Retained via Zinc Oxide Cement: A Retrospective 10-23-Year Study. Clin Implant Dent Relat Res. 2016;18:917–25. doi: 10.1111/cid.12372. [DOI] [PubMed] [Google Scholar]
- 49.Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, et al. Assessing the quality of reports of randomized clinical trials: Is blinding necessary? Control Clin Trials. 1996;17:1–2. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- 50.Schropp L, Kostopoulos L, Wenzel A, Isidor F. Clinical and radiographic performance of delayed-immediate single-tooth implant placement associated with peri-implant bone defects. A 2-year prospective, controlled, randomized follow-up report. J Clin Periodontol. 2005;32(5):480–7. doi: 10.1111/j.1600-051X.2005.00699.x. [DOI] [PubMed] [Google Scholar]
- 51.Zembic A, Bösch A, Jung RE, Hämmerle CH, Sailer I. Five-year results of a randomized controlled clinical trial comparing zirconia and titanium abutments supporting single-implant crowns in canine and posterior regions. Clin Oral Implants Res. 2013 Apr 1;24:384–90. doi: 10.1111/clr.12044. [DOI] [PubMed] [Google Scholar]
- 52.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Andersson B, Odman P, Lindvall AM, Brånemark PI. Cemented single crowns on osseointegrated implants after 5 years: Results from a prospective study on CeraOne. Int J Prosthodont. 1998;11:212–8. [PubMed] [Google Scholar]
- 54.Behneke A, Behneke N, d’Hoedt B. The longitudinal clinica effectiveness of ITI solid-screw implants in partially edentulous patients: A 5-year follow-up report. Int J Oral Maxillofac Implants. 2000;15:633–45. [PubMed] [Google Scholar]
- 55.Brägger U, Aeschlimann S, Bürgin W, Hämmerle CH, Lang NP. Biological and technical complications and failures with fixed partial dentures (FPD) on implants and teeth after four to five years of function. Clin Oral Implants Res. 2001;12:26–34. doi: 10.1034/j.1600-0501.2001.012001026.x. [DOI] [PubMed] [Google Scholar]
- 56.Andersen E, Saxegaard E, Knutsen BM, Haanaes HR. A prospective clinical study evaluating the safety and effectiveness of narrow-diameter threaded implants in the anterior region of the maxilla. Int J Oral Maxillofac Implants. 2001;16:217–24. [PubMed] [Google Scholar]
- 57.Weber HP, Kim DM, Ng MW, Hwang JW, Fiorellini JP. Peri-implant soft-tissue health surrounding cement- and screw-retained implant restorations: A multi-center, 3-year prospective study. Clin Oral Implants Res. 2006;17:375–9. doi: 10.1111/j.1600-0501.2005.01232.x. [DOI] [PubMed] [Google Scholar]
- 58.Jemt T. Cemented CeraOne and porcelain fused to TiAdapt abutment single-implant crown restorations: A 10-year comparative follow-up study. Clin Implant Dent Relat Res. 2009;11:303–10. doi: 10.1111/j.1708-8208.2008.00120.x. [DOI] [PubMed] [Google Scholar]
- 59.Nissan J, Narobai D, Gross O, Ghelfan O, Chaushu G. Long-term outcome of cemented versus screw-retained implant-supported partial restorations. Int J Oral Maxillofac Implants. 2011;26:1102–7. [PubMed] [Google Scholar]
- 60.Ioannidis A, Gallucci GO, Jung RE, Borzangy S, Hämmerle CH, Benic GI. Titanium-zirconium narrow-diameter versus titanium regular-diameter implants for anterior and premolar single crowns: 3-year results of a randomized controlled clinical study. J Clin Periodontol. 2015;42:1060–70. doi: 10.1111/jcpe.12468. [DOI] [PubMed] [Google Scholar]
- 61.Wang JH, Judge R, Bailey D. A 5-year retrospective assay of implant treatments and complications in private practice: The restorative complications of single and short-span implant-supported fixed prostheses. Int J Prosthodont. 2016;29:435–44. doi: 10.11607/ijp.4794. [DOI] [PubMed] [Google Scholar]
- 62.Weber HP, Sukotjo C. Does the type of implant prosthesis affect outcomes in the partially edentulous patient? Int J Oral Maxillofac Implants. 2007;22:140–72. [PubMed] [Google Scholar]
- 63.Rosenstiel SF, Land MF, Crispin BJ. Dental luting agents: A review of the current literature. J Prosthet Dent. 1998;80:280–301. doi: 10.1016/s0022-3913(98)70128-3. [DOI] [PubMed] [Google Scholar]
- 64.Shrivastav M. Effect of surface treatments on the retention of implant-supported cement-retained bridge with short abutments: An in vitro comparative evaluation. J Indian Prosthodont Soc. 2018;18:154–60. doi: 10.4103/jips.jips_251_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Yuzbasioglu E. A modified technique for extraoral cementation of implant retained restorations for preventing excess cement around the margins. J Adv Prosthodont. 2014;6:146–9. doi: 10.4047/jap.2014.6.2.146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.AlHelal A, Kattadiyil MT, AlBader B, Clark JL. A protocol for screw-retrievable, cement-retained, implant-supported fixed partial dentures. Int J Prosthodont. 2017;30:577–80. doi: 10.11607/ijp.5321. [DOI] [PubMed] [Google Scholar]
- 67.Ha CY, Lim YJ, Kim MJ, Choi JH. The influence of abutment angulation on screw loosening of implants in the anterior maxilla. Int J Oral Maxillofac Implants. 2011;26:45–55. [PubMed] [Google Scholar]
- 68.Kim ES, Shin SY. Influence of the implant abutment types and the dynamic loading on initial screw loosening. J Adv Prosthodont. 2013;5:21–8. doi: 10.4047/jap.2013.5.1.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Barbosa GA, Bernardes SR, das Neves FD, Fernandes Neto AJ, de Mattos Mda G, Ribeiro RF, et al. Relation between implant/abutment vertical misfit and torque loss of abutment screws. Braz Dent J. 2008;19:358–63. doi: 10.1590/s0103-64402008000400013. [DOI] [PubMed] [Google Scholar]
- 70.Burguete RL, Johns RB, King T, Patterson EA. Tightening characteristics for screwed joints in osseointegrated dental implants. J Prosthet Dent. 1994;71:592–9. doi: 10.1016/0022-3913(94)90443-x. [DOI] [PubMed] [Google Scholar]
- 71.Ahmad M, Dhanasekar B, Aparna IN, Naim H. Replacement of missing anterior tooth using screw retained implant prosthesis in the esthetic zone: A case report with 3 years of follow up. J Indian Prosthodont Soc. 2014;14:297–300. doi: 10.1007/s13191-012-0188-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Rani I, Shetty J, Reddy V. A comparison of periimplant strain generated by different types of implant supported prostheses. J Indian Prosthodont Soc. 2017;17:142–8. doi: 10.4103/0972-4052.203195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Mansour A, Ercoli C, Graser G, Tallents R, Moss M. Comparative evaluation of casting retention using the ITI solid abutment with six cements. Clin Oral Implants Res. 2002;13:343–8. doi: 10.1034/j.1600-0501.2002.130401.x. [DOI] [PubMed] [Google Scholar]