Abstract
Primary stability in dental implants is an essential factor for achieving successful osseointegration. Surgical procedure and bone quality are among the most common factors that affect primary stability. It is also crucial to achieve high-insertion torque which is important for obtaining primary stability. Maintaining sufficient bone bulk and density is essential to achieve necessary bone-to-implant contact for obtaining a biomechanically stable implant. A new concept for osteotomy called osseodensification (OD) has been at the forefront of changes in surgical site preparation in implantology. This relatively new concept with universally compatible drills has been proposed to help in better osteotomy preparation, bone densification, and indirect sinus lift and also achieve bone expansion at different sites of varying bone densities. This procedure has also shown improvement in achieving better implant primary stability and better osteotomy than conventional implant drills. A systematic review was undertaken to analyze if OD procedure had any advantages over conventional osteotomy on bone density and primary stability. An electronic database search was conducted in PubMed using keywords such as “OD,” “implant primary stability,” “implant bone density,” and “implant osteotomy.” A total of 195 articles were collected and subjected to screening using inclusion and exclusion criteria. A literature review was done, following which it was seen that the use of versah drills for bone OD resulted in undersized osteotomy compared to conventional drills. It also resulted in improved bone density and increase in percentage bone volume and bone-to-implant contact, thereby improving implant stability.
Keywords: Implant stability, osseodensification, osteotomy
INTRODUCTION
Primary stability in implant placement is one of the most critical factors determining the outcome of implant therapy. The key factors in enhancing implant primary stability are bone density,[1,2] surgical protocol,[3] and implant thread type and geometry.[4] Primary stability is provided by the mechanical friction between the external implant surface and walls of the implant osteotomy. The insertion torque peak is directly related to implant primary stability and host bone density;[5] high-insertion torque could significantly increase the initial bone-to-implant contact percentage (%BIC) compared to implant inserted with low-insertion torque values.[6] Ottoni et al.[7] showed a reduction in failure rate of 20% in single-tooth implant restoration for every 9.8 N cm of torque increased.
Osseodensification (OD) is a new method of biomechanical bone preparation performed for dental implant placement. The procedure is characterized by low plastic deformation of bone that is created by rolling and sliding contact using a densifying bur that is fluted such that it densifies the bone with minimal heat elevation. OD, a bone nonextraction technique, was developed by Huwais 2013[8] and done using specially designed burs (Densah™ burs) that help densify bone [Figure 1] as they prepare an osteotomy.[9] These burs provide advantages of both osteotomes combining the speed along with improved tactile control of the drills during osteotomy. Standard drills excavate bone during implant osteotomy, while osteotomes tend to induce fractures of the trabeculae that requiring long remodeling time and delayed secondary implant stability. The Densah burs allow for bone preservation and condensation through compaction autografting during osteotomy preparation, thereby increasing the bone density in the peri-implant areas and improving the implant mechanical stability.[10] The bone-remodeling unit requires more than 12 weeks to repair the damaged area created by conventional drills that extract substantial amount of bone to let strains in the walls of osteotomy reach or go beyond the bone microdamage threshold. Hence, OD will help preserve bone bulk and increase density, thereby shortening the healing period.[11]
Figure 1.

Versah Kit with densification drills
Unlike traditional osteotomy, OD does not excavate bone but simultaneously compacts and autografts the particulate bone in an outward direction to create the osteotomy, thereby preserving vital bone tissue. This is achieved using specialized densifying burs [Figure 2]. When the specialized drill is used at high speed in an anticlockwise direction with steady external irrigation (Densifying Mode), the dense compact bone tissue is created along the osteotomy walls.[12] The pumping motion (in and out movement) creates a rate-dependent stress to produce a rate-dependent strain and allows saline solution pumping to gently pressurize the bone walls. This combination facilitates an increased bone plasticity and bone expansion [Figure 3]. Huwais demonstrated that OD helped ridge expansion while maintaining alveolar ridge integrity, thereby allowing implant placement in autogenous bone, also achieving adequate primary stability. OD helped in preserving bone bulk and shortened the waiting period to restorative phase.[13]
Figure 2.
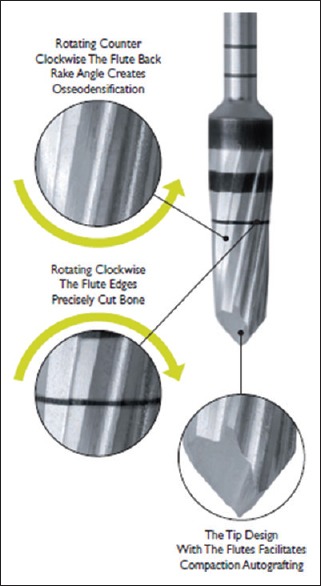
Role of densification Drills (image source: Versah LLC product catalogue, www.versah.com)
Figure 3.
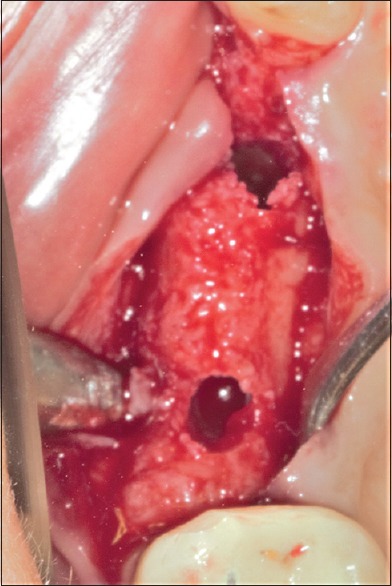
Osteotomy preparation using the densification drills
A systematic review was undertaken to analyze if OD procedure had any advantages over conventional osteotomy on bone density and primary stability. An electronic database search was conducted in PUBMED using keywords such asOD, implant primary stability, implant bone density, and implant osteotomy. An electronic database search in PUBMED was conducted for articles up to 2017 using MeSH and keywords such as “OD,” “implant primary stability,” “implant osteotomy,” and “implant bone density.” A total of 195 articles were identified and scrutinized for full-text articles, and after screening, finally, three full-text articles were selected for the review according to the inclusion criteria [Figure 4].
Figure 4.
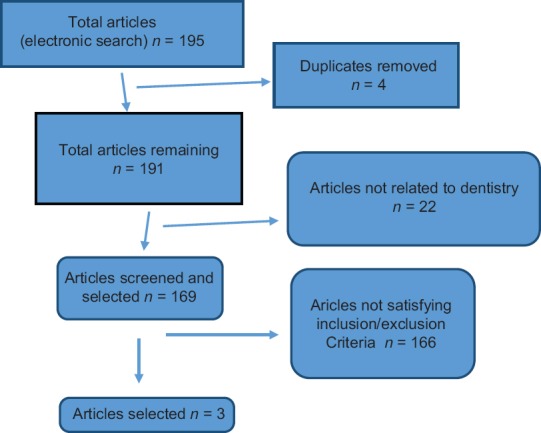
Diagram showing search results
Inclusion criteria
Only full-text articles were considered.
Implant site: Compact bone/cancellous bone
Implant stability: Primary stability/secondary stability
Drills: Osteotomy preparation with conventional drills/OD drills
Bone density: Bone volume percentage (%BV)/BIC.
Exclusion criteria
Case reports/case series
In vitro studies.
OSSEODENSIFICATION AND BONE DENSITY
The process of osseointegration leads to bone formation on the implant surface and contributes to implant secondary stability between bone and dental implant.
In areas of low bone density, such as maxillary posterior region, the insufficient bone available could affect the histomorphometric parameters such as %BIC and %BV negatively, thereby affecting primary and secondary implant stability. A layer of increased bone mineral density has been shown by imaging around the periphery of osteotomies using OD. The increase in bone density achieved by OD has shown to have a potentiating effect on secondary stability.
OSSEODENSIFICATION AND PRIMARY STABILITY
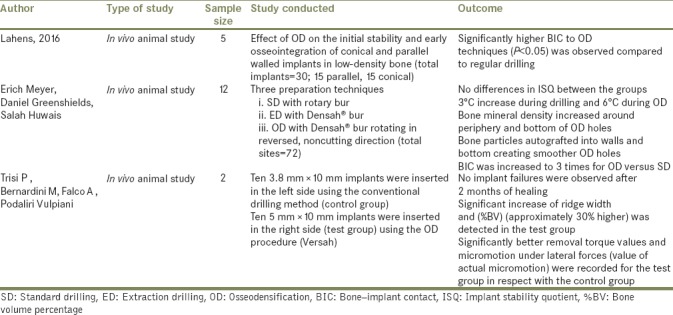
The implant primary stability is a crucial factor to achieve implant osseointegration.[14] High primary implant stability is critical in immediate loading protocols, and it was reported that an implant micromotion above 50–100 um potentiated peri-implant bone resorption or implant failures.[15,16,17] Trisi et al. in in vivo study found a statistically significant correlation between peri-implant bone density, insertion torque, and micromotion [Table 1]. A significant increase in insertion torque and a concomitant reduction in micromotion was noted with an increase in bone density values.[18] Berardini et al.[19] and Li et al.[20] in a review reported no significant difference in crestal bone resorption and failure rate between implants inserted with either high- or low-insertion torque values. They also demonstrated the ability of OD drills to increase the % of BV and % of BIC for dental implants inserted into poor density bone compared to conventional osteotomies, which may help in enhancing osseointegration,[21,22]
Table 1.
Table with relevant studies on osseodensification
Newer methods such as cutting torque resistance analysis developed by Johansson and Strid was also suggested as a tool to evaluate implant primary stability,[23] but nothing specific has been documented in the literature with regard to OD.
OSSEODENSIFICATION VERSUS CONVENTIONAL OSTEOTOMY
Biomechanical capabilities of implants are affected by various factors, which include implant macro/microgeometry, nanosurface modifications, and osteotomy techniques employed.[22,24] Standard drills used in implant site osteotomy excavate bone to facilitate implant placement. They produce effective cutting of bone but lack the design capability to create a precise circumferential osteotomy. Osteotomies, therefore, become elongated and elliptical due to the imprecise cutting of the drills. This leads to a reduction of torque during implant insertion, leading to poor primary stability and contributing to the potential for nonintegration of implant. Furthermore, osteotomies prepared in deficient bone may produce either buccal or lingual dehiscence, which results in a reduction of primary stability and necessitates an additional bone grafting adding to the total cost of treatment and increasing healing time.
Undersizing the implant site preparation[25,26] and using the osteotomes for bone condensation[27,28] are some of the surgical methods advised to increase primary stability in implants and % of BIC in poor density bone. Observations were also made of different healing patterns and peri-implant bone-remodeling models.[29,30,31] The alternative to implant drilling procedures in the posterior maxilla is the osteotome technique[27] that aims to compact the bone with the mechanical action of cylindrical instruments along the osteotomy walls. This procedure created trabecular fractures with debris, which caused an obstruction to the process of osseointegration.[32]
OD osteotomy diameters were found to be smaller than conventional osteotomies prepared with the same burs due to the springy nature and elastic strain of bone. This increased the percent of bone available at the implant site by about three times. Histomorphological analysis has demonstrated the presence of autogenous bone fragments in the osseodensified osteotomy sites, especially in the bone of low mineral density relative to regular drills.[33] These fragments acted as nucleating surfaces promoting new bone formation around the implants and providing greater bone density and better stability. Gil et al. found no statistically significant difference in bone-area-fraction occupancy as a result of drilling technique (P = 0.22).[34]
CONCLUSION
OD is a specialized procedure for osteotomy preparation that is inherently bone preserving. Unlike conventional osteotomy, it uses specialized high-speed densifying burs to prepare osteotomy and autograft bone in the phase of plastic deformation. This results in an expanded osteotomy with preserved and dense compacted bone tissue that helps maintain ridge integrity and allows implant placement with superior stability. Use of versah drills in OD led to the formation of undersized osteotomy when compared to conventional drills. It helped improve bone density and also increased the percent of BV and increased bone-to-implant contact, thereby improving implant stability. Current literature evidence is inadequate to draw any concrete conclusions, and more studies are recommended in this field.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Marquezan M, Osório A, Sant’Anna E, Souza MM, Maia L. Does bone mineral density influence the primary stability of dental implants? A systematic review. Clin Oral Implants Res. 2012;23:767–74. doi: 10.1111/j.1600-0501.2011.02228.x. [DOI] [PubMed] [Google Scholar]
- 2.Trisi P, De Benedittis S, Perfetti G, Berardi D. Primary stability, insertion torque and bone density of cylindric implant ad modum Branemark: Is there a relationship? An in vitro study. Clin Oral Implants Res. 2011;22:567–70. doi: 10.1111/j.1600-0501.2010.02036.x. [DOI] [PubMed] [Google Scholar]
- 3.Turkyilmaz I, Aksoy U, McGlumphy EA. Two alternative surgical techniques for enhancing primary implant stability in the posterior maxilla: A clinical study including bone density, insertion torque, and resonance frequency analysis data. Clin Implant Dent Relat Res. 2008;10:231–7. doi: 10.1111/j.1708-8208.2008.00084.x. [DOI] [PubMed] [Google Scholar]
- 4.Dos Santos MV, Elias CN, Cavalcanti Lima JH. The effects of superficial roughness and design on the primary stability of dental implants. Clin Implant Dent Relat Res. 2011;13:215–23. doi: 10.1111/j.1708-8208.2009.00202.x. [DOI] [PubMed] [Google Scholar]
- 5.Trisi P, Perfetti G, Baldoni E, Berardi D, Colagiovanni M, Scogna G, et al. Implant micromotion is related to peak insertion torque and bone density. Clin Oral Implants Res. 2009;20:467–71. doi: 10.1111/j.1600-0501.2008.01679.x. [DOI] [PubMed] [Google Scholar]
- 6.Capparé P, Vinci R, Di Stefano DA, Traini T, Pantaleo G, Gherlone EF, et al. Correlation between initial BIC and the insertion torque/depth integral recorded with an instantaneous torque-measuring implant motor: An in vivo study. Clin Implant Dent Relat Res. 2015;17(Suppl 2):e613–20. doi: 10.1111/cid.12294. [DOI] [PubMed] [Google Scholar]
- 7.Ottoni JM, Oliveira ZF, Mansini R, Cabral AM. Correlation between placement torque and survival of single-tooth implants. Int J Oral Maxillofac Implants. 2005;20:769–76. [PubMed] [Google Scholar]
- 8.Huwais S. Inventor; Fluted osteotome and surgical method for use. US Patent Application US2013/0004918; 3 January, 2013 [Google Scholar]
- 9.Huwais S. Autografting Osteotome. WO2014/077920. Geneva, Switzerland: World Intellectual Property Organization Publication; 2014. [Google Scholar]
- 10.Huwais S, Meyer E. Osseodensification: A novel approach in implant osteotomy preparation to increase primary stability, bone mineral density and bone to implant contact. Int J Oral Maxillofac Implants. 2016;32:27–36. doi: 10.11607/jomi.4817. [DOI] [PubMed] [Google Scholar]
- 11.Frost HM. A brief review for orthopedic surgeons: Fatigue damage (microdamage) in bone (its determinants and clinical implications) J Orthop Sci. 1998;3:272–81. doi: 10.1007/s007760050053. [DOI] [PubMed] [Google Scholar]
- 12.Meyer EG, Huwais S. Osseodensification is a Novel Implant Preparation Technique that Increases Implant Primary Stability by Compaction and Auto-Grafting Bone. San Francisco, CA: American Academy of Periodontology; 2014. [Google Scholar]
- 13.Huwais S. Enhancing implant stability with osseodensification: A two year follow up. Implant Pract. 2015;8:28–34. [Google Scholar]
- 14.Albrektsson T, Brånemark PI, Hansson HA, Lindström J. Osseointegrated titanium implants. Requirements for ensuring a long-lasting, direct bone-to-implant anchorage in man. Acta Orthop Scand. 1981;52:155–70. doi: 10.3109/17453678108991776. [DOI] [PubMed] [Google Scholar]
- 15.Søballe K, Brockstedt-Rasmussen H, Hansen ES, Bünger C. Hydroxyapatite coating modifies implant membrane formation. Controlled micromotion studied in dogs. Acta Orthop Scand. 1992;63:128–40. doi: 10.3109/17453679209154808. [DOI] [PubMed] [Google Scholar]
- 16.Søballe K, Hansen ES, Brockstedt-Rasmussen H, Bünger C. Hydroxyapatite coating converts fibrous tissue to bone around loaded implants. J Bone Joint Surg Br. 1993;75:270–8. doi: 10.1302/0301-620X.75B2.8444949. [DOI] [PubMed] [Google Scholar]
- 17.Szmukler-Moncler S, Salama H, Reingewirtz Y, Dubruille JH. Timing of loading and effect of micromotion on bone-dental implant interface: Review of experimental literature. J Biomed Mater Res. 1998;43:192–203. doi: 10.1002/(sici)1097-4636(199822)43:2<192::aid-jbm14>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- 18.Trisi P, Berardini M, Falco A, Podaliri Vulpiani M. Effect of implant thread geometry on secondary stability, bone density, and bone-to-implant contact: A biomechanical and histological analysis. Implant Dent. 2015;24:384–91. doi: 10.1097/ID.0000000000000269. [DOI] [PubMed] [Google Scholar]
- 19.Berardini M, Trisi P, Sinjari B, Rutjes AW, Caputi S. The effects of high insertion torque versus low insertion torque on marginal bone resorption and implant failure rates: A systematic review with meta-analyses. Implant Dent. 2016;25:532–40. doi: 10.1097/ID.0000000000000422. [DOI] [PubMed] [Google Scholar]
- 20.Li H, Liang Y, Zheng Q. Meta-analysis of correlations between marginal bone resorption and high insertion torque of dental implants. Int J Oral Maxillofac Implants. 2015;30:767–72. doi: 10.11607/jomi.3884. [DOI] [PubMed] [Google Scholar]
- 21.Trisi P, Berardini M, Falco A, Podaliri Vulpiani M. New osseodensification implant site preparation method to increase bone density in low-density bone: In vivo evaluation in sheep. Implant Dent. 2016;25:24–31. doi: 10.1097/ID.0000000000000358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lahens B, Neiva R, Tovar N, Alifarag AM, Jimbo R, Bonfante EA, et al. Biomechanical and histologic basis of osseodensification drilling for endosteal implant placement in low density bone. An experimental study in sheep. J Mech Behav Biomed Mater. 2016;63:56–65. doi: 10.1016/j.jmbbm.2016.06.007. [DOI] [PubMed] [Google Scholar]
- 23.Swami V, Vijayaraghavan V, Swami V. Current trends to measure implant stability. J Indian Prosthodont Soc. 2016;16:124–30. doi: 10.4103/0972-4052.176539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Coelho PG, Jimbo R. Osseointegration of metallic devices: Current trends based on implant hardware design. Arch Biochem Biophys. 2014;561:99–108. doi: 10.1016/j.abb.2014.06.033. [DOI] [PubMed] [Google Scholar]
- 25.Alghamdi H, Anand PS, Anil S. Undersized implant site preparation to enhance primary implant stability in poor bone density: A prospective clinical study. J Oral Maxillofac Surg. 2011;69:e506–12. doi: 10.1016/j.joms.2011.08.007. [DOI] [PubMed] [Google Scholar]
- 26.Degidi M, Daprile G, Piattelli A. Influence of underpreparation on primary stability of implants inserted in poor quality bone sites: An in vitro study. J Oral Maxillofac Surg. 2015;73:1084–8. doi: 10.1016/j.joms.2015.01.029. [DOI] [PubMed] [Google Scholar]
- 27.Summers RB. A new concept in maxillary implant surgery: The osteotome technique. Compendium. 1994;15:152. 154-6, 158. [PubMed] [Google Scholar]
- 28.Boustany CM, Reed H, Cunningham G, Richards M, Kanawati A. Effect of a modified stepped osteotomy on the primary stability of dental implants in low-density bone: A cadaver study. Int J Oral Maxillofac Implants. 2015;30:48–55. doi: 10.11607/jomi.3720. [DOI] [PubMed] [Google Scholar]
- 29.Campos FE, Gomes JB, Marin C, Teixeira HS, Suzuki M, Witek L, et al. Effect of drilling dimension on implant placement torque and early osseointegration stages: An experimental study in dogs. J Oral Maxillofac Surg. 2012;70:e43–50. doi: 10.1016/j.joms.2011.08.006. [DOI] [PubMed] [Google Scholar]
- 30.Coelho PG, Marin C, Teixeira HS, Campos FE, Gomes JB, Guastaldi F, et al. Biomechanical evaluation of undersized drilling on implant biomechanical stability at early implantation times. J Oral Maxillofac Surg. 2013;71:e69–75. doi: 10.1016/j.joms.2012.10.008. [DOI] [PubMed] [Google Scholar]
- 31.Munjal S, Munjal S, Hazari P, Mahajan H, Munjal A, Mehta DS, et al. Evaluation of specifically designed implants placed in the low-density jaw bones: A clinico-radiographical study. Contemp Clin Dent. 2015;6:40–3. doi: 10.4103/0976-237X.149290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Büchter A, Kleinheinz J, Wiesmann HP, Kersken J, Nienkemper M, Weyhrother HV, et al. Biological and biomechanical evaluation of bone remodelling and implant stability after using an osteotome technique. Clin Oral Implants Res. 2005;16:1–8. doi: 10.1111/j.1600-0501.2004.01081.x. [DOI] [PubMed] [Google Scholar]
- 33.Stavropoulos A, Nyengaard JR, Lang NP, Karring T. Immediate loading of single SLA implants: Drilling vs.osteotomes for the preparation of the implant site. Clin Oral Implants Res. 2008;19:55–65. doi: 10.1111/j.1600-0501.2007.01422.x. [DOI] [PubMed] [Google Scholar]
- 34.Gil LF, Sarendranath A, Neiva R, Marão HF, Tovar N, Bonfante EA, et al. Bone healing around dental implants: Simplified vs.conventional drilling protocols at speed of 400 rpm. Int J Oral Maxillofac Implants. 2017;32:329–36. doi: 10.11607/jomi.4802. [DOI] [PubMed] [Google Scholar]


