Abstract
Context:
Probiotics have been prescribed to old aged patients’ invariably with or without complete dentures for improving their digestive process. It is mentioned that probiotics do have an effect in increasing the amount of saliva in the oral cavity. Therefore, this study was planned to evaluate the amount and pH of saliva after using probiotics for 60 days in completely edentulous patients.
Aim:
This study aims to evaluate the amount and pH of saliva of edentulous patients before and after using probiotics.
Settings and Design:
The interventional prospective study was conducted at the department of prosthodontics of the institute.
Methods:
The study was conducted on edentulous patients. The whole unstimulated and stimulated saliva was collected at baseline and amount, and pH was measured. Then, each patient was given probiotic capsules reaching 3.3 × 107 CFU/g to consume daily once for 60 days. Saliva was recollected from patients, and its amount and pH was calculated and compared with baseline.
Statistical Analysis Used:
STATAIC-13.
Results:
On comparison of saliva before and after consuming probiotics, there was an increase in the mean unstimulated and stimulated saliva from baseline to that after 60 days, the difference being 0.406 and 0.433, respectively. The difference was statistically significant with P < 0.001. The mean pH at baseline was 7.818 ± 0.231 which increased after 60 days to 7.825 ± 0.189, the difference being 0.007.
Conclusion:
This study concluded that probiotics increase the amount of saliva of completely edentulous patients and so it can be helpful in patients suffering from xerostomia/hyposalivation.
Keywords: Edentulous patients, hyposalivation, probiotics, saliva, xerostomia
INTRODUCTION
Saliva is a composite fluid consisting of electrolytes, glycoproteins, and enzymes that lubricates and keeps the mucosa hygienic, protects it from distress, aids in digestion and also provides sensation of taste. The prevalence of adequate quality and quantity of saliva becomes even more mandatory in completely edentulous patients. The wetting mechanism of saliva helps create adhesion, cohesion and surface tension in between dentures and mucosa thus leading to increase in the retention of the prosthesis.[1] There may be detrimental effect on denture stability and retention if there is any amendment in salivary flow or characteristics.[2,3] Saliva also plays a profound role in decreasing stomatitis of prosthetic etiology which is found in significant number of complete and partial denture wearers.[4]
The term probiotic, meaning “for life,” is derived from the Greek language. According to the WHO/FAO report (2002), probiotics are “Live microorganisms which, when administered in adequate amounts, confer a health benefit on the host.” The definition reflects that probiotic micro-organisms are living and execute health benefits.[5,6]
In the past few years, probiotics have also been investigated from an oral health perspective, and their use has shown promising results with respect to the control of chronic conditions, such as dental caries, periodontitis, halitosis, and candidial infections.7 Control of biofilm formation on voice prosthesis has also been documented.[8] It has been proved in animal studies that probiotics affect the composition of saliva, such as altering the concentrations of mucins and immunoglobulins.[9] Probiotics help in patients suffering from hyposalivation, which was the secondary finding of this study.[7]
It has also been noted and commented that probiotics can also efficiently lessen the risk of xerostomia.[10,11] However, still, there is no research carried out to confirm these findings in edentulous patients.
Hence, the null hypothesis proposed is that probiotics do not have any effect on the amount of saliva and the current study is carried out to evaluate the effect of probiotics on saliva of edentulous patients over a period of 2 months. This study will provide a baseline data regarding the use of probiotics in increasing the amount of saliva and pH in edentulous patients which in turn will contribute to better denture retention and thus may help in the treatment of dry mouth problems in denture wearers.
MATERIALS AND METHODS
This interventional prospective study was done on a group of completely edentulous patients visiting the department of prosthodontics. The study was carried out for 2 months on 29 patients (males – 21 and females – 8) selected on the basis of the following inclusion criteria: completely edentulous patients with the age of 60 years or above, patients who were not suffering from any chronic debilitating disease or not on any kind of medication, absence of any kind of oral pathology, and patients who understand and were willing to be a part of these studies. The patients who did not give informed consent or were not willing to be a part of this study were excluded from the study.
The materials/equipment used were Probiotics capsules ((1) Mitushi Pharma; L-130/2268, Parishram Nagar Part-1, Krishnanagar, Naroda, Ahmedabad, Gujarat 382346. (2) Rajvi Enterprise; c-203, Supath-2, Near old Vadaj bus stop, Ashram Rd, Old Wadaj, Ahmedabad, Gujarat 380013) and saliva collection kit which included beaker, gauze piece, weighing scale, and pH meter. The probiotic strains used in the study were Lactobacillus rhamnosus GG-HS111, Lactobacillus Acidophilus-HS101, and Bifidobacterium bifidum. These strains will be combined in powder form in equal amount in a power of 108 CFU (3.3 × 107 CFU of each) per capsule and dispensed to the patient [Figure 1].
Figure 1.
Probiotic capsules containing Lactobacillus rhamnosus GG-HS111, Lactobacillus acidophilus-HS101, and Bifidobacterium bifidum
Prior Institutional Ethical Approval was obtained. Before this study was conducted, participants were informed about the study background and procedures before they signed the written informed consent form. The oral and dental status of the participants was examined, and a detailed history was taken at 0 week (baseline). The saliva was collected using the following two methods:
Whole unstimulated saliva production: The patient sat quietly, without talking or chewing, and spit any saliva that accumulates in the floor of the mouth into a preweighed beaker. This Test was done for 5 min. An unstimulated flow rate of below 0.1 ml/min was considered to indicate hyposalivation
Whole stimulated saliva production: The patient was asked to chew a preweighed gauze for 5 min, following which the accumulated saliva was measured, by spitting the wet gauze piece along with saliva into a preweighed beaker. A stimulated flow rate of 0.8 ml/min was considered to indicate hyposalivation.
This is a well-known recommended method of saliva collection.[9] Other methods that can be used for saliva collection are passive drool method and SalivaBio Oral Swab.
After sample collection, the amount of saliva was measured in Grams on a weighing scale and pH was calculated using a pH meter. After this, each patient was given 60 probiotic capsules which they were supposed to consume daily once between morning 9–11 am with water for 60 days. During those 60 days, a regular follow-up was kept to monitor the consumption of probiotic capsules by the patients on daily basis.
After 60 days of the interventional period, the patients were recalled. Out of 29 patients, four patients dropped out. The reason for the withdrawal from the study was moving out and health issues. The patients were told to refrain themselves from eating, drinking (except water), and smoking 1 h before the investigation. Saliva was collected from the rest of the 25 patients, and its amount and pH was calculated using the above-mentioned method, and the amount of saliva was compared with that of the baseline.
Ethics
Ethical approval from the University Ethics Committee was obtained. The proper information regarding the purpose of the study was given to the patients, and an informed consent form was made to be filled by each of the patients.
Statistical analysis
Data were analyzed using STATAIC-13. Mean and standard deviation (SD) was measured using descriptive analysis. Statistical significance of differences between means was analyzed using paired t-test. All the data were expressed as mean ± SD. The accepted level of statistical significance was P < 0.05.
RESULTS
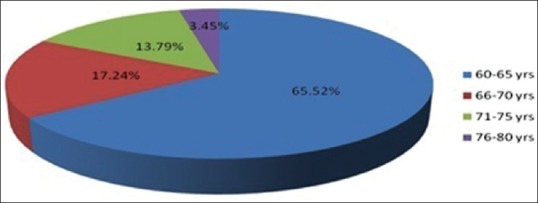
In this 60 days intervention, the amount of saliva obtained at baseline and after 60 days and its pH was obtained and compared. “Table 1” and [Figure 2] shows the descriptive statistics of age groups of the patients enrolled for the study. “Table 2” describes the frequency distribution before and after 60 days for the whole stimulated, unstimulated saliva and pH.
Table 1.
Descriptive statistics
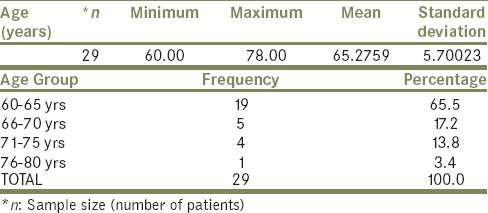
Figure 2.
Age group distribution chart
Table 2.
Frequency Distribution

According to the statistical analysis performed using paired t-test, the mean unstimulated saliva at baseline was 0.815 ± 0.628 which increased after 60 days to 1.222 ± 0.617, the difference being 0.406 as observed in “Table 3”. The difference is statistically significant with P < 0.001. The mean stimulated saliva at baseline was 2.033 ± 0.575 which increased after 60 days to 2.466 ± 0.616, the difference being 0.433 which is statistically significant with P < 0.001 as observed in “Table 4”. The mean pH at baseline was 7.818 ± 0.231 which increased after 60 days to 7.825 ± 0.189, the difference being 0.007 as observed in “Table 5”. All the three comparisons are reflected in Data chart [Figure 3].
Table 3.
Paired t-Test: Whole Unstimulated Saliva
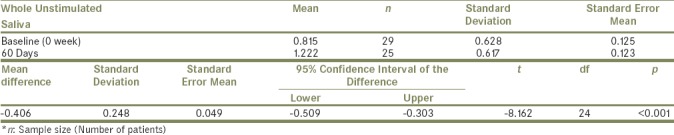
Table 4.
Paired t-Test: Whole Stimulated Saliva
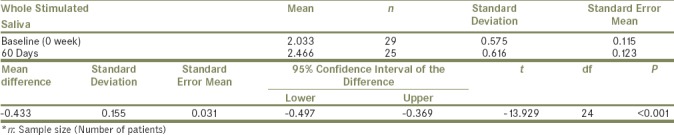
Table 5.
Paired t-Test: pH Level
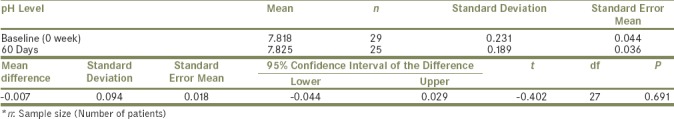
Figure 3.
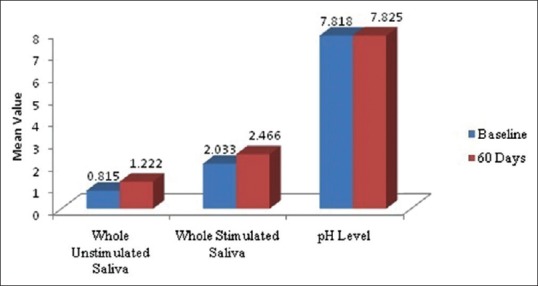
Data comparison chart
DISCUSSION
We carried out this study to evaluate the effect of probiotics on the amount of saliva in edentulous patients. Accordingly, 29 edentulous patients were selected, and their saliva samples were collected, and the amount of saliva and its pH was measured at baseline. Then, they were given 60 capsules each containing three different strains of probiotics (Lactobacillus rhamnosus GG-HS111, Lactobacillus Acidophilus-HS101, and Bifidobacterium bifidum) which they were supposed to consume during 60 days. The regular communication was maintained with the patients on ingestion of probiotic capsules. After an interventional period, the patients were recalled, and their saliva samples were collected and measured. The sample measurements were compared with that of the baseline data and analyzed.
The study found that supplementation of three strains of probiotics has an effect on the amount of saliva. It was observed that the amount of saliva significantly increased compared to the baseline whereas no significant change in pH was observed.
The results of this study are in accordance with the secondary findings of a study done be Hataka.[9] The study was carried out with a primary aim of using probiotics to reduce the prevalence of oral candida in elderly patients. It was found during the research that the amount of saliva also increased along with a reduction in oral Candida. Since there are no similar studies carried out before to assess the effect of probiotics on amount of saliva therefore there is no literature available related to the study.
The findings of this study would be a baseline for further researches to be carried out on patients suffering from xerostomia.
The The exact mechanism of this increase is not known, but it has been mentioned in a study that probiotics might somehow influence the composition of saliva, such as the concentrations of mucins and salivary immunoglobulins, as has been shown in animals[12] and in vivo studies,[13] thereby affecting the nature and amount of saliva secreted.[9] In addition, probiotics are observed to induce hormonal secretion.[5] It has also been found that there is increased milk production in animals on the intake of probiotics.[14,15] This shows that probiotics do play a role in increasing the fluid production in the body. Probiotics can alter the epithelial cell of parotid glands to produce more beta adhesion-2 in saliva.[16] From this, it can be anticipated that probiotics possess the ability to alter the epithelial cells of saliva producing glands like parotid thereby increasing the secretion of saliva. Further research is necessary to confirm the precise mechanism of action.
One of the major efforts in such interventional studies is to make sure that the patients regularly take the dose of probiotic prescribed at home on the daily basis. In this study, an attempt was made to contact the patients and encourage them to take probiotics regularly. Furthermore, this study was carried out for a short period of 2 months. Therefore, a similar study can be planned for a longer period and on greater number of patients.
Thus, the null hypothesis is proved wrong, and it can be concluded that probiotics do have an effect in increasing the amount of saliva in edentulous patients.
The results of the study were statistically significant proving that probiotics do have an effect on the amount of saliva of completely edentulous patients and can become a boon for patients suffering from xerostomia and hyposalivation. The data on probiotic effects in the mouth are accumulating, but the exact molecular mechanisms of their action are still unclear and should be probed to make these benevolent bacteria useful for mankind.
CONCLUSION
Within the limitations of the study it can be concluded that probiotics can increase the amount of saliva in completely edentulous patients and therefore can be judiciously utilized in patients suffering from xerostomia/hyposalivation.
Financial support and sponsorship
This research is a “Short Term Studentship” award project (STS 2015-02122) granted by the Indian Council of Medical Research. The authors gratefully acknowledge the stipend Rs. 10,000/- sanctioned to Ms. Urvi Sanghvi as an award prize.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors gratefully acknowledge the Indian Council of Medical Research for approving this research “Short Term Studentship” (STS 2015-02122). The authors also acknowledge the infrastructural support provided by the department in the study.
REFERENCES
- 1.Turner M, Jahangiri L, Ship JA. Hyposalivation, xerostomia and the complete denture: A systematic review. J Am Dent Assoc. 2008;139:146–50. doi: 10.14219/jada.archive.2008.0129. [DOI] [PubMed] [Google Scholar]
- 2.Sachdeva S, Noor R, Mallick R, Perwez E. Role of saliva in complete denture: An overview. Ann Dent Spec. 2014;2:51–4. [Google Scholar]
- 3.Niedermeier WH, Krämer R. Saliva and dentures. J Prosthet Dent. 1992;67:211–6. doi: 10.1016/0022-3913(92)90455-j. [DOI] [PubMed] [Google Scholar]
- 4.Albanese S, Villani G. Saliva: An important factor in retention of complete denture. Arch Stomatol (Napoli) 1989;30:329–36. [PubMed] [Google Scholar]
- 5.Stamatova I, Meurman JH. Probiotics: Health benefits in the mouth. Am J Dent. 2009;22:329–38. [PubMed] [Google Scholar]
- 6.Haukioja A. Probiotics and oral health. Eur J Dent. 2010;4:348–55. [PMC free article] [PubMed] [Google Scholar]
- 7.Pradeep K, Kuttappa MA, Prasana KR. Probiotics and oral health: An update. SADJ. 2014;69:20–4. [PubMed] [Google Scholar]
- 8.Reddy JJ, Sampathkumar N, Aradhya S. Probiotics in dentistry: Review of the current status. Rev Clí Pesq Odontol. 2010;6:261–7. [Google Scholar]
- 9.Hatakka K, Ahola AJ, Yli-Knuuttila H, Richardson M, Poussa T, Meurman JH, et al. Probiotics reduce the prevalence of oral candida in the elderly – A randomized controlled trial. J Dent Res. 2007;86:125–30. doi: 10.1177/154405910708600204. [DOI] [PubMed] [Google Scholar]
- 10.Ramchandran S, Vijayabala S, Raj KS D. Probiotics the promising future – A review. SEAJCRR. 2013;2:98–105. [Google Scholar]
- 11.Singh K, Kallali B, Kumar A, Thaker V. Probiotics: A review. Asian Pac J Trop Biomed. 2011;1:S287–90. [Google Scholar]
- 12.Negretti F, Casetta P, Clerici-Bagozzi D, Marini A. Researches on the intestinal and systemic immune-responses after oral treatments with Lactobacillus GG in rabbit. Dev Phisiopath Clin. 1997;7:15–21. [Google Scholar]
- 13.Mack DR, Ahrne S, Hyde L, Wei S, Hollingsworth MA. Extracellular MUC3 mucin secretion follows adherence of Lactobacillus strains to intestinal epithelial cells in vitro. Gut. 2003;52:827–33. doi: 10.1136/gut.52.6.827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kritas SK, Govaris A, Christodoulopoulos G, Burriel AR. Effect of bacillus licheniformis and Bacillus subtilis supplementation of ewe's feed on sheep milk production and young lamb mortality. J Vet Med A Physiol Pathol Clin Med. 2006;53:170–3. doi: 10.1111/j.1439-0442.2006.00815.x. [DOI] [PubMed] [Google Scholar]
- 15.Sun P, Wang JQ, Deng LF. Effects of bacillus subtilis natto on milk production, rumen fermentation and ruminal microbiome of dairy cows. Animal. 2013;7:216–22. doi: 10.1017/S1751731112001188. [DOI] [PubMed] [Google Scholar]
- 16.Kusumaningsih T, Subijanto MS, Indrawati R, Devijanti RR. The level of beta defensin-2 in saliva and its expression in parotid gland epithelial cells after probiotic (Lactobacillus reuteri) induction to inhibit Streptococcus mutans in caries. Eur J Dent. 2016;10:556–60. doi: 10.4103/1305-7456.195161. [DOI] [PMC free article] [PubMed] [Google Scholar]


